Académique Documents
Professionnel Documents
Culture Documents
Clin Infect Dis. 2003 Saravolatz 40 5
Transféré par
Rahul SoniCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Clin Infect Dis. 2003 Saravolatz 40 5
Transféré par
Rahul SoniDroits d'auteur :
Formats disponibles
40 CID 2003:36 (1 January) Saravolatz et al.
M A J O R A R T I C L E
Broad-Range Bacterial Polymerase
Chain Reaction for Early Detection
of Bacterial Meningitis
Louis D. Saravolatz,
1,2
Odette Manzor,
1
Nancy VanderVelde,
1
Joan Pawlak,
1
and Bradley Belian
1
1
Department of Medicine, Molecular Biology Research Laboratory, St. John Hospital and Medical Center, and
2
Wayne State University School
of Medicine, Detroit, Michigan
The diagnosis of bacterial meningitis often depends on isolation of bacteria on culture, which may take 24
48 h. DNA amplication techniques could provide rapid diagnosis, which would guide the clinician in anti-
microbial therapy decisions. This study determined the clinical utility of polymerase chain reaction (PCR) for
the diagnosis of meningitis with use of a broad range of bacterial primers. Seventy-four cerebrospinal uid
specimens obtained from 70 patients were subjected to PCR with use of primers derived from conserved
regions of the bacterial 16S RNA gene. The test characteristics for the broad-range bacterial PCR were as
follows: sensitivity, 100%; specicity, 98.2%; positive predictive value, 94.4%; and negative predictive value,
100%. Broad-range bacterial PCR may be useful for excluding the diagnosis of meningitis, and the results
may inuence the decision to initiate or discontinue antimicrobial therapy.
The incidence of bacterial meningitis in the United States
is 35 cases per 100,000 persons per year, with a mor-
tality rate of 6%26%, leading to 12000 deaths yearly
[1]. Morbidity and mortality rates are even higher in
developing countries. Rapid diagnosis and treatment are
critical, because permanent neurological sequelae (such
as hearing loss, mental retardation, seizures, and behav-
ioral changes) may occur in up to one-half of survivors.
Classic clinical signs, which are present in 80% of
patients, include headache, fever, meningismus, and
cerebral dysfunction. However, among neonates and
elderly persons, only subtle signs, such as lethargy and
irritability, may herald the onset of meningitis [1]. Anti-
biotic treatment is empirically initiated on the basis of
clinical ndings. The diagnosis of meningitis depends
Received 5 July 2002; accepted 30 September 2002; electronically published
12 December 2002.
Reprints or correspondence: Dr. Louis D. Saravolatz, Dept. of Medicine, St. John
Hospital and Medical Center, 22201 Moross Rd., Ste. 80, Detroit, MI 48236
(louis.saravolatz@stjohn.org).
Clinical Infectious Diseases 2003; 36:405
2003 by the Infectious Diseases Society of America. All rights reserved.
1058-4838/2003/3601-0007$15.00
on results of culture of blood and CSF samples and the
ndings of microscopic and chemical analysis of CSF
specimens. Denitive therapy is guided by the results
of culture, which may take 2428 h to obtain; antibiotic
susceptibility testing may require an additional 24 h
[2]. Thus, the information needed for specic anti-
microbial therapy is unavailable for the rst 48 h.
During the rst few days of illness in which a di-
agnosis of bacterial meningitis is entertained, the pa-
tient, family, and clinician may all experience a high
level of anxiety. In addition, prophylaxis may be used
if meningococcal meningitis is suspected. These con-
siderations emphasize the need for a rapid and accurate
diagnostic test for bacterial meningitis.
PCR amplication of bacterial DNA is a potential
method for rapid detection of bacterial meningitis [3].
This technique has been used to identify such organ-
isms as penicillin-resistant Streptococcus pneumoniae [2,
4], Neisseria meningitidis [5], group B streptococci [6],
Listeria monocytogenes [7], and Mycobacterium tuber-
culosis [8] with use of species-specic primers. In this
study, we selected a broad-range primer that could de-
tect most if not at all bacterial pathogens submitted to
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
PCR for Bacterial Meningitis CID 2003:36 (1 January) 41
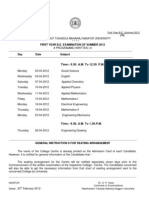
Figure 1. Results of broad-range bacterial PCR with use of CSF samples in a study of bacterial meningitis. Lanes CJ, Results of broad-range
bacterial PCR with use of CSF samples obtained from patients with microbiological evidence of bacterial meningitis (i.e., positive results of either
culture or Gram staining). Positive PCR result is 241-bp product. Lane A, molecular size standard; lane B, source of nonbacterial DNA (human placenta,
serving as negative control); lane K, product of broad-range bacterial PCR for Streptococcus pneumoniae ATCC (American Type Culture Collection)
49619, serving as positive control.
a microbiology laboratory. The usefulness of this diagnostic test
would be to determine whether empirical antimicrobial therapy
should or should not be administered and thus potentially
eliminate unnecessary administration of antimicrobial therapy
to some patients. In view of the lack of specic information
on antimicrobial susceptibility, the test would not replace con-
ventional culture and susceptibility testing. Our purpose was
to determine the utility of a broad-range bacterial PCR (BRB-
PCR) as a rapid diagnostic technique for detection of bacterial
meningitis and to delineate test characteristics, including sen-
sitivity, specicity, positive predictive value, and negative pre-
dictive value.
METHODS
Specimen collection. CSF samples were obtained via lumbar
puncture or from CSF shunts and were submitted for routine
microbiology, chemistry, and hematology testing. Gram stain-
ing was performed with a cytocentrifuge specimen. CSF spec-
imens were inoculated onto blood agar, chocolate agar, and
enriched broth. The remaining CSF sample was stored at 70C
for subsequent batch analysis at the Department of Medicine
Molecular Biology Research Laboratory, St. John Hospital and
Medical Center (Detroit, Michigan). Seventy-four samples were
available for analysis.
DNA amplication techniques. CSF specimens stored at
70C were thawed and briey spun in a microcentrifuge. A
15-mL aliquot of the supernatant was transferred to a sterile
microcentrifuge tube and boiled for 10 min. Five microliters
of the boiled sample was used as the template for the PCR
reaction [2].
PCR reactions were done with use of a primer sequence
derived from highly conserved regions of the bacterial 16S RNA
gene (5
-GGAGGAAGGTGGGGATGACG -3
and 5
-ATGGTG-
TGACGGGCGGTGTG-3
) [9, 10]. This primer is known as a
universal primer because of its ability to amplify a 241-bp
product from any bacterial species.
A master mix solution consisting of 0.4 mM of each primer,
2.5 mM of MgCl, 1 PCR buffer, 200 mM of deoxynucleoside
triphosphates, and 1.25 U of Taq DNA polymerase (Stoffel
fragment) was used. The PCR mixture was placed in a thermo-
cycler (model 9600; Perkin Elmer) for 25 cycles. The parameters
were as follows: denaturation for 30 s at 95C, annealing for
30 s at 50C, and extending for 30 s at 70C. Twenty microliters
of the PCR reaction was loaded onto a 2% agarose gel con-
taining ethidium bromide (0.5 mg/mL).
Presence of a 241-bp band was considered to be a positive
result (gure 1). The reliability of the PCR assay for the 241-
bp band was previously established by other investigators; thus,
it was not necessary to sequence the PCR product [911]. When
used with S. pneumoniae ATCC (American Type Culture Col-
lection) 49619, the detection limit of this test was !3.25 cfu/
mL, as determined by serial dilution. Negative controls included
with each run were human placental DNA, PCR reagents only,
and a CSF sample that was known to be culture negative and
that lacked any WBCs. The positive control was a CSF sample
spiked with S. pneumoniae ATCC 49619. Samples were also
examined for PCR inhibitors and/or degradation of DNA. This
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
42 CID 2003:36 (1 January) Saravolatz et al.
was achieved by spiking negative specimens with S. pneumoniae
ATCC 49619 in the reaction tube before retesting. We did this
to ensure that the potential for false-negative assay results would
be minimized.
Patient characteristics. Medical records were reviewed for
data regarding age, associated illnesses, total duration of anti-
microbial therapy, outcome, systemic WBC count, results of
Gram staining and culture of CSF, and CSF WBC count. On
the basis of culture and Gram staining results and CSF WBC
counts, patients were divided into 3 groups. The no-infection
group consisted of patients who had no cellular or microbio-
logical evidence of infection (i.e., no WBCs in the CSF, no
organisms seen on direct microscopic evaluation of a Gram
stain, and negative culture results); the CSF WBCpositive
group included patients who did not have microbiological ev-
idence of infection, as determined by negative results of Gram
staining and culture, but who had a cellular response in CSF
(WBC count, 1100 cells/mm
3
); and the infected group con-
sisted of patients with microbiological evidence of infection, as
determined by a positive result of either culture or Gram stain-
ing of CSF specimens.
Test effectiveness. Sensitivity, specicity, positive predictive
value, and negative predictive value were determined on the
basis of standard denitions [12]. The 95% CIs for sensitivity,
specicity, and positive and negative predictive values were cal-
culated according to the method of Newcombe [13].
RESULTS
The demographic characteristics, associated illnesses, CSF and
systemic WBC count, and data regarding antimicrobial therapy
and culture results for the 3 study groups are summarized
in table 1. As expected, patients in the infected group had higher
systemic and CSF WBC counts, a higher risk of associated
illnesses, and a longer mean duration (SD) of treatment
( days) than did either of the other groups (CSF 20.9 41.7
WBCpositive group, days; no-infection group, 2.0 1.5
days). Microbiological ndings for the 17 specimens 1.0 1.8
obtained from the infected patients are shown in table 2. The
high rate of isolation of Staphylococcus epidermidis is consistent
with the presence of neurosurgically implanted devices. Two
patients had positive results of Gram staining but negative re-
sults of culture. The PCR assay was positive in all 17 cases. In
the no-infection group, there were no positive results of BRB-
PCR tests. In the CSF WBCpositive group, there was only 1
positive BRB-PCR assay result (2.7%). This sample that tested
positive had been obtained from a patient who had a prior
specimen in the infected group. Therefore, PCR detected CSF
infection in this sample, whereas culture and Gram staining
did not. In the analysis of test characteristics, the positive result
in the CSF WBCpositive group was considered to be falsely
positive. Results of the BRB-PCR assay and microbiological
techniques are compared in table 3.
The sensitivity of the BRB-PCR compared with microbio-
logical techniques was 100% (95% CI, 81.6%100%; 17 of 17
samples that tested positive with use of microbiological tech-
niques had positive BRB-PCR results); the specicity was 98.2%
(95% CI, 90.7%99.7%; 56 of 57 samples that tested negative
with use of microbiological techniques had negative BRB-PCR
results); the positive predictive value was 94.4% (95% CI,
74.2%99.7%; 17 of 18 samples with positive BRB-PCR results
also tested positive with use of microbiological techniques);
and the negative predictive value was 100% (95% CI, 93.6%
100%; 56 of 56 samples with negative BRB-PCR results also
tested negative with use of microbiological techniques).
DISCUSSION
The morbidity and mortality associated with bacterial men-
ingitis make this a dreaded illness for both physicians and pa-
tients. Faster accurate diagnosis of bacterial meningitis would
alleviate much of the worry associated with suspicion of this
disease. The BRB-PCR assay appears to hold promise for this
application. The BRB-PCR result may also inuence the initial
empirical choice of antimicrobial therapy. Because the negative
predictive value was 100%, if the results are negative, the cli-
nician may either not prescribe antimicrobials or, if treatment
has already begun, elect to discontinue antibiotic treatment.
This may lead to a reduced duration of antimicrobial exposure
for patients who show a WBC response in CSF before nal
culture results are available. In addition, BRB-PCR results may
be helpful for treatment of patient contacts to trace menin-
gococcal exposure. If a patient suspected of having bacterial
meningitis due to N. meningitidis has a negative BRB-PCR
result, the contacts can be assured that prophylaxis is not
needed. In addition, CSF ndings in patients with nonbacterial
infections or noninfectious diseases may result in the admin-
istration of unnecessary antimicrobial therapy. These consid-
erations are represented by patients in the CSF WBCpositive
group in our study. Antibiotic therapy could be avoided for
such patients, and the clinicians could focus diagnostic studies
on nonbacterial entities.
Antimicrobial therapy reduces the yield of cultures, but it
probably does not affect PCR results. For example, after the
initiation of parenteral antibiotic therapy, the isolation of me-
ningococci from blood culture decreases from 50% to !5% [5].
BRB-PCR should not require the presence of large numbers of
organisms, and it may detect fastidious, slow-growing, or non-
viable organisms [14, 15].
Three cases in this study that suggest that BRB-PCR may be
more sensitive than standard culture and Gram staining are
summarized. For patient 1, a specimen obtained on 28 October
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
PCR for Bacterial Meningitis CID 2003:36 (1 January) 43
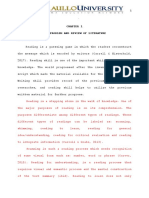
Table 1. Characteristics of patients and CSF specimens in a study of broad-range
bacterial PCR for early detection of bacterial meningitis.
Characteristic
Patients with
no infection
(n p 20)
CSF WBC
positive
patients
(n p 37)
Infected
patients
(n p 17)
Age, years
Mean SD 25.6 21.9 17.1 16.1 22.1 18.6
Range 0.0879 0.0855 0.0865
Associated condition or risk
factor, no. of patients
Diabetes mellitus 1 0 2
HIV infection 0 0 1
Alcohol abuse 2 0 2
Malignancy 0 1 1
Neurosurgery 2 3 5
WBC count, cells/mm
3
Mean SD 7200 2200 11,200 4300 15,800 7280
Range 250011,400 500025,400 440031,900
CSF leukocyte count, cells/mm
3
Mean SD 0 377 319 6703 14,726
Range 1002004 19262,250
Differential, mean % SD
Neutrophils 56 28 71 23
Lymphocytes 27 27 18 21
Monocytes 19 21 7 5
CSF protein level, mean
mg/L SD 61 76 88 59 391 600
CSF glucose level, mean
mg/L SD 64 13 58 11 52 22
Receipt of antibiotics before lumbar
puncture, no. of patients 1 5 5
Total duration of antibiotic
therapy, days
Mean SD 1.0 1.8 2.0 1.5 20.9 41.7
Range 06 04 0123
Outcome, no. of patients
Death 1 0 2
Discharge from hospital while
receiving antibiotic therapy 0 1 4
1999 had positive results of BRB-PCR, positive results of Gram
staining (which revealed rare gram-negative bacilli), and neg-
ative results of culture. The patient received intermittent anti-
microbial therapy, including therapy administered 3 days be-
fore the patient underwent lumbar puncture. Specimens
obtained on 9 and 23 October 1999 and on 1 November 1999
had positive results of BRB-PCR, culture, and Gram staining.
Samples obtained from patient 2 before admission to the hos-
pital had positive results of BRB-PCR and Gram staining, but
the results of culture were negative, and the patient received
antimicrobials before admission. Samples obtained from pa-
tient 3 had positive results of Gram staining, culture, and BRB-
PCR. However, a new CSF sample was obtained 24 h later; the
results of culture were negative, but BRB-PCR results were
positive.
These 3 cases support the view that BRB-PCR is a sensitive
method that does not depend on the presence of viable or-
ganisms, making it more applicable in cases in which the patient
has received prior antibiotic treatment. In a study similar to
ours, Dicuonzo et al. [16] described 4 patients with negative
culture results but no specic amplicon identied by the probes
studied. That study did not evaluate clinical parameters that
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
44 CID 2003:36 (1 January) Saravolatz et al.
Table 2. Microbiological ndings for patients
with microbiological evidence of infection, as de-
termined by positive results of culture or Gram
staining.
Results of culture
No. of patients
Positive
culture
results
Positive
results
of Gram
staining
Positive
Staphylococcus epidermidis 5 2
Streptococcus pneumoniae 2 2
Group B streptococci 2 2
Klebsiella pneumoniae 3 3
Enterobacter cloacae 1 0
Enterobacter aerogenes 1 0
Neisseria meningitidis 1 0
Negative
Gram-positive cocci
on Gram stain 0 1
Gram-negative rods
on Gram stain 0 1
Total 15 11
Table 3. Comparison of microbiological
ndings and broad-range bacterial PCR (BRB-
PCR) results for CSF specimens obtained from
patients who are suspected of having bacte-
rial meningitis.
BRB-PCR
result
Result of
microbiological tests
a
Total Positive Negative
Positive 17 1 18
Negative 0 56 56
Total 17 57 74
a
Microscopic evaluation of Gram stain or culture
isolation.
could explain the results but suggested that there were possibly
nosocomial pathogens that would not be detected by the probes
used, including Streptococcus species, N. meningitidis, Haemo-
philus inuenzae, and M. tuberculosis. In yet another study that
examined bacteremia in patients with fever and neutropenia,
18 patients who had been receiving antibiotics at the time that
blood samples were obtained for culture had bacterial DNA
detected in the blood, as determined by 16S RNA gene am-
plication [17]. As in our study, the authors suggested that
PCR of bacterial DNA may augment but not replace culture
as a detection method. In addition, only 11 of the 18 patients
who had positive PCR results in our study (table 3) also had
positive results of Gram staining. Thus, conventional direct
microscopy still has insufcient sensitivity for the diagnosis of
meningitis.
One advantage of using CSF specimens for BRB-PCR is that
CSF specimens obtained from uninfected persons are normally
sterile, and there is not the problem of bacterial colonization
that confuses PCR results, which occurs with samples from
other body sites, such as the respiratory tract. The ability to
distinguish infection from colonization remains a challenge in
the interpretation of results of tests that use samples other than
CSF specimens.
Our study further extends the recent observation made by
Rantakokko-Jalava et al. [18], who studied 253 CSF specimens
and found that 15 had positive PCR results and 32 had positive
culture results. Their study reported a sensitivity of 63.2% and
a specicity of 99.6%. This important work had numerous
controls for false-negative results, but it still reported a sensi-
tivity lower than that found in our study.
A limitation of our study is that, by its nature, BRB-PCR
does not use specic bacterial primers. If initial BRB-PCR tests
yield positive results, a subsequent PCR could be done with
primers specic for the most-common bacterial agents to con-
rm the diagnosis. Another option would be a multiplex ap-
proach, in which several primers are used to note the presence
of bacteria by BRB-PCR as well as specic pathogens, such as
S. pneumoniae and N. meningitidis. The limitation to this ap-
proach is that a large number of primers would have to be
used to detect all of the strains shown in table 2. Also, there
would still remain the need to perform antimicrobial suscep-
tibility testing on isolates recovered from culture. Because only
74 specimens were examined in this study, additional research-
ers and centers should also critically evaluate BRB-PCRmethod
before it is adopted widely.
In this study, BRB-PCR demonstrated excellent diagnostic
test characteristics, with high sensitivity (100%), specicity
(98.2%), positive predictive value (94.4%), and negative pre-
dictive value (100%). These results are based on a microbio-
logical standard: a positive result of culture or Gram staining.
Our results compare favorably with the results of a study by
Kotilainen et al. [9], which evaluated patients with meningitis
and found a sensitivity of 94% and specicity of 96%. In con-
trast, our study used 25 cycles of amplication (resulting in
improved sensitivity) and was applied to a greater variety of
bacterial species. Recently, Lu et al. [19] evaluated a universal-
primer PCR on 150 CSF samples with only 13 positive culture
results and found a sensitivity of 92.3%, which is comparable
to the results of our study. Our study extends the observations
with a universal-primer PCR and evaluated results in relation
to antimicrobial therapy, which could lead to negative culture
results but positive BRB-PCR results. There is the potential for
overuse of antibiotics if samples that yield positive BRB-PCR
results and negative culture results dictate therapy, because we
do not know how long bacterial genomic material persists in
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
PCR for Bacterial Meningitis CID 2003:36 (1 January) 45
the CSF after the initiation of therapy. Nonetheless, we believe
that BRB-PCR may be useful for excluding the diagnosis of
bacterial meningitis and may assist in the decision to discon-
tinue antibiotic therapy. If the BRB-PCR yields positive results,
the clinicians decision to administer antimicrobial therapy is
supported. If the results are negative, the clinician could con-
sider alternative diagnoses sooner.
BRB-PCR is a promising screening test for the diagnosis of
bacterial meningitis that may be performed in 2 h. Because of
the need for antimicrobial susceptibility testing, it should be
considered as an adjunct to culture and antimicrobial suscep-
tibility testing. BRB-PCR deserves further examination to es-
tablish reliability and reproducibility before it becomes a widely
used test for the rapid diagnosis of bacterial meningitis.
Acknowledgments
We thank Ruth Moore, for reviewing the manuscript, and
Patricia Schultz, for manuscript preparation.
References
1. Scheld WM. Bacterial meningitis, brain abscess, and other suppurative
intracranial infections. In: Fauci A, ed. Harrisons principles of internal
medicine. New York: McGraw-Hill, 1988:241962.
2. DuPlessis M, Smith A, Klugman K. Rapid detection of penicillin re-
sistant Streptococcus pneumoniae in cerebrospinal uid by a seminested
PCR strategy. J Clin Microbiol 1998; 36:4537.
3. Eisenstein BI. The polymerase chain reaction. N Engl J Med 1990; 322:
17883.
4. Dagan R, Shriker O, Hazan I, et al. Prospective study to determine
clinical relevance of detection of pneumococcal DNAin sera of children
by PCR. J Clin Microbiol 1998; 36:66973.
5. Ni H, Knight A, Cartwright K, Palmer W, McFadden J. Polymerase
chain reaction for diagnosis of meningococcal meningitis. Lancet
1992; 340:14324.
6. Bergeron MG, Danbing KE, Menard C, et al. Rapid detection of group
B streptococci in pregnant women at delivery. N Engl J Med 2000;
343:1759.
7. Jaton K, Sahli R, Billie J. Development of polymerase chain reaction
assays for detection of Listeria monocytogenes in clinical cerebrospinal
uid samples. J Clin Microbiol 1992; 30:19316.
8. Lorino G, Lilli D, Rivanera D, et al. Polymerase chain reaction, with
sequencing, as a diagnostic tool in culture-negative bacterial meningitis.
Clin Microbiol Infect 1999; 5:926.
9. Kotilainen P, Jalava J, Meurman C, et al. Diagnosis of meningococcal
meningitis by broad-range bacterial PCR with cerebrospinal uid. J
Clin Microbiol 1998; 36:22059.
10. Martineau F, Picard F, Roy P, Oullette M, Bergeron M. Species-specic
and ubiquitous DNA-based assays for rapid identication of Staphy-
lococcus epidermidis. J Clin Microbiol 1998; 36:288893.
11. Forbes B, Sahm DR, Weissfeld AS. Diagnostic microbiology. 10th ed.
St. Louis: Mosby, 1998:196.
12. Dawson B, Trapp RG. Basic and clinical biostatistics. 3rd ed. New York:
Lange Medical Books, 2001:2659.
13. Newcombe RG. Two-sided condence intervals for the single propor-
tion: comparison of seven methods. Stat Med 1998; 17:85772.
14. Rudolph KM, Parkinson AJ, Black CM, Mayer LW. Evaluation of poly-
merase chain reaction for diagnosis of pneumococcal pneumonia. J
Clin Microbiol 1993; 31:26616.
15. Zhang TD, Isaccman DJ, Wadowsky RM, Rydquist-White J, Post JC,
Ehrlich CD. Detection of Streptococcus pneumoniae in whole blood by
PCR. J Clin Microbiol 1995; 33:596601.
16. Dicuonzo G, Lorino G, Lilli D, et al. Use of oligoprobes on amplied
DNA in the diagnosis of bacterial meningitis. Eur J Clin Microbiol
Infect Dis 1999; 18:3527.
17. Ley BE, Linton OJ, Bennett BM, Foot ABM, Miller MR. Detection of
bacteremia in patients with fever and neutropenia using 16S rRNA
gene amplication by polymerase chain reaction. Eur J Clin Microbiol
Infect Dis 1998; 17:24753.
18. Rantakokko-Jalava K, Nikkart S, Jalava J, et al. Direct amplication of
rRNA genes in diagnosis of bacterial infections. J Clin Microbiol
2000; 38:329.
19. Lu J, Perng CL, Lee ST, Wan CC. Use of PCR with universal primer
and restriction endonuclease digestion for detection and identication
of common bacterial pathogens in cerebrospinal uid. J Clin Microbiol
2000; 38:207680.
b
y
g
u
e
s
t
o
n
J
u
n
e
3
,
2
0
1
4
h
t
t
p
:
/
/
c
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
Vous aimerez peut-être aussi
- Rtmnu Mechanical Engineering SyllabusDocument85 pagesRtmnu Mechanical Engineering SyllabusShobit JainPas encore d'évaluation
- Music Grades Fee Sheet UK 2011Document1 pageMusic Grades Fee Sheet UK 2011Sai TejaPas encore d'évaluation
- BEI Exam Summer 2012Document1 pageBEI Exam Summer 2012Rahul SoniPas encore d'évaluation
- B.SC Part-I Examination Summer 2012Document1 pageB.SC Part-I Examination Summer 2012Rahul SoniPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Total English Placement TestDocument6 pagesTotal English Placement TestKaterina PapakonstantinouPas encore d'évaluation
- English Grammar Book-Final - 2-5-21Document42 pagesEnglish Grammar Book-Final - 2-5-21Manav GaurPas encore d'évaluation
- IM4PBDocument518 pagesIM4PBJagdish HathiPas encore d'évaluation
- Girls, Gangs and Crime-The Profile of The Female OffenderDocument16 pagesGirls, Gangs and Crime-The Profile of The Female OffenderLiLiThBLaCkPas encore d'évaluation
- Kutub PDFDocument12 pagesKutub PDFMs RawatPas encore d'évaluation
- NLS Arabic and French Issue R12.1.3Document7 pagesNLS Arabic and French Issue R12.1.3Anil RawatPas encore d'évaluation
- Sentence Structure TypesDocument44 pagesSentence Structure TypesGanak SahniPas encore d'évaluation
- Jean Faber and Gilson A. Giraldi - Quantum Models For Artifcial Neural NetworkDocument8 pagesJean Faber and Gilson A. Giraldi - Quantum Models For Artifcial Neural Networkdcsi3Pas encore d'évaluation
- DisasterDocument10 pagesDisasterMixsz LlhAdy100% (1)
- Problems and Answer Key: - 1 (A) 70 (B) 97 (C) 127 (D) 159 (E) 729 2Document9 pagesProblems and Answer Key: - 1 (A) 70 (B) 97 (C) 127 (D) 159 (E) 729 2alice24134Pas encore d'évaluation
- 2 Cor 37Document2 pages2 Cor 37M. Div ChoudhrayPas encore d'évaluation
- 11 Rabino v. Cruz 222 SCRA 493Document4 pages11 Rabino v. Cruz 222 SCRA 493Joshua Janine LugtuPas encore d'évaluation
- Minimalism of InformationDocument125 pagesMinimalism of InformationRastko VukovicPas encore d'évaluation
- 11.1. Complete The Sentences. Use One of These Verbs in The Past SimpleDocument4 pages11.1. Complete The Sentences. Use One of These Verbs in The Past SimpleSebastián Valencia Moreno0% (1)
- 330A 2018docDocument20 pages330A 2018docDavid MendozaPas encore d'évaluation
- Azeem English Magazine Vol. 22 Issue 01Document68 pagesAzeem English Magazine Vol. 22 Issue 01Raheel Asghar100% (1)
- IA Feedback Template RevisedDocument1 pageIA Feedback Template RevisedtyrramPas encore d'évaluation
- Comparison of Ftir Apodization Functions Using Modeled and Measured Spectral DataDocument4 pagesComparison of Ftir Apodization Functions Using Modeled and Measured Spectral Dataገዛኽኝ ሱፋPas encore d'évaluation
- DLL Gen Math Ems AnnuitiesDocument13 pagesDLL Gen Math Ems AnnuitiesFreyy Agad Maligot0% (1)
- Progress Test 01Document6 pagesProgress Test 01lethuha1988100% (2)
- CBR Bahasa Inggris Fisika Kelompok 1Document9 pagesCBR Bahasa Inggris Fisika Kelompok 1Ryan SianiparPas encore d'évaluation
- Prose: Jooprencess E. PonoDocument11 pagesProse: Jooprencess E. Ponoaye plazaPas encore d'évaluation
- Past Simple PDFDocument4 pagesPast Simple PDFderlinPas encore d'évaluation
- Quantitative Option Strategies: Marco Avellaneda G63.2936.001 Spring Semester 2009Document29 pagesQuantitative Option Strategies: Marco Avellaneda G63.2936.001 Spring Semester 2009Adi MPas encore d'évaluation
- Science - G8 - Q1 - Week 4Document48 pagesScience - G8 - Q1 - Week 4Angelito MadesPas encore d'évaluation
- Reading Comprehension TextsDocument15 pagesReading Comprehension TextsCMRotaruPas encore d'évaluation
- Government vs. AlburalDocument2 pagesGovernment vs. Alburalpoppy2890100% (2)
- CHAPTER 1 Final OkDocument43 pagesCHAPTER 1 Final Okroneldayo62Pas encore d'évaluation
- Culture Shock Refers To The Feelings of Confusion and Uncertainty That You Experience When You Come Into Contact With A New CultureDocument13 pagesCulture Shock Refers To The Feelings of Confusion and Uncertainty That You Experience When You Come Into Contact With A New CultureRetno WulanPas encore d'évaluation