Académique Documents
Professionnel Documents
Culture Documents
1791 Full
Transféré par
zingioTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
1791 Full
Transféré par
zingioDroits d'auteur :
Formats disponibles
Risk of Glaucoma after Pediatric Cataract Surgery
Birgitte Haargaard,
1,2
Christian Ritz,
1
Anna Oudin,
1
Jan Wohlfahrt,
1
John Thygesen,
3
Thomas Olsen,
4
and Mads Melbye
1
PURPOSE. To determine the risk of glaucoma after surgery for
pediatric cataract and to evaluate risk factors for glaucoma.
METHODS. A population-based cohort of all children in Denmark
aged 0 to 17 years during the period 1977 to 2001, who
underwent surgery for pediatric cataract, was established by
retrospective chart review. Glaucoma cases were dened as
those in which glaucoma surgery (trabeculectomy and/or di-
ode laser transscleral cyclophotocoagulation) was performed
and/or permanent medical therapy prescribed after cataract
surgery.
RESULTS. Of 946 eyes (595 patients) undergoing pediatric cat-
aract surgery, 72 eyes (48 patients) had subsequent develop-
ment of glaucoma. Early surgery (9 months of age) was
associated with a 7.2-fold increased risk of glaucoma compared
with late surgery (9 months of age). Ten years after cataract
surgery, glaucoma developed in 31.9% (95% condence inter-
val [CI], 24.441.1) of children undergoing surgery before 9
months of age compared with 4.1% (95% CI, 2.4 to 6.8) of
children aged 9 months at the time of surgery. Glaucoma
cases continued to occur more than 10 years after cataract
surgery. After adjustment for age at surgery, no other risk
factor appeared important.
CONCLUSIONS. The risk of glaucoma after surgery for pediatric
cataract is substantial and particularly high for those below 9
months of age at the time of surgery. Because the increased risk
persists for many years after surgery, careful continuous mon-
itoring for glaucoma is mandatory. (Invest Ophthalmol Vis Sci.
2008;49:17911796) DOI:10.1167/iovs.07-1156
O
ne of the most severe complications after surgery for
congenital cataract is glaucoma. However, reported inci-
dences of glaucoma after congenital cataract surgery vary.
Because of differences in study population, criteria for diagno-
sis of glaucoma, and length of follow-up period, the frequen-
cies of postoperative glaucoma have been reported to be be-
tween 8% and 59%.
111
Similarly, several risk factors (e.g.,
surgery at a very early age
1214
microcornea,
47,15
nuclear
cataract morphology,
6,7,12,15
surgical technique,
6
and surgery
for secondary cataract
6,14
) have been suggested to be associ-
ated with glaucoma after cataract surgery, but with other
reports not being able to nd one or more of these associa-
tions.
4,8,12,15,16
Furthermore, some studies nd primary in-
traocular lens implantation to be protective against glauco-
ma,
1719
but others do not.
16,2023
The uncertainties between
previously reported studies are perhaps because most studies
have been based on smaller sample sizes. Previous larger re-
ports on risk factors for glaucoma have been on selected
groups of aphakic children,
6,11
and have found age at surgery,
small corneas, surgery for secondary cataract and primary sur-
gery with posterior capsulotomy-anterior vitrectomy to be risk
factors for development of glaucoma.
We took advantage of the national registration of pediatric
cataract surgery in Denmark to establish a population-based
cohort of all children who underwent surgery for pediatric
cataract from 1977 to 2005. Our objective was to investigate
the risk of glaucoma after surgery according to cataract etiol-
ogy, surgical technique, surgery for secondary cataract, cata-
ract morphology, other ocular anomalies, age at surgery, and
time since surgery.
METHODS
Ascertainment of Cases
Since 1977 all discharge diagnoses and surgical procedures of patients
admitted to public hospitals have been registered in the Danish Na-
tional Register of Patients (NRP). Since 1995 outpatients have also been
registered. Based on the information in NRP we established a cohort of
all children from birth to 17 years and diagnosed with pediatric cata-
ract during the period 1977 to 2001. We subsequently contacted all
relevant hospitals and were able to retrieve and review the childrens
medical records. Additional case information was obtained from the
consultant ophthalmologists who provided care when needed. Cata-
racts were classied by etiology, and those caused by trauma (n
patients
466), or considered to be due to acquired systemic (e.g., diabetes)
or acquired ocular disease (e.g., uveitis; n
patients
258) were exclud-
ed.
24,25
The nal cohort consisted only of those who underwent
cataract surgery during the period 1977 to 2005. For the present
analysis cases reported with aniridia (n 13), congenital rubella (n
17), and Lowes syndrome (n 1) were excluded, because these
diseases are independently associated with glaucoma. Cases with per-
sistent fetal vasculature (PFV) and microcornea were included for the
purpose of studying the risk of these conditions with the development
of glaucoma. Microcornea was dened as 2 standard deviations below
the mean corneal diameter, according to postconceptional age and
otherwise as 10 mm in diameter.
26,27
The cases were classied according to etiology and clinical char-
acteristics. The main etiological groups were idiopathic, hereditary,
and familial, associated with syndromes and chromosomal anomalies,
and associated with intrauterine infection.
25
Clinically, the cases were
divided by laterality (unilateral or bilateral cataracts) and into groups
including isolated cataracts and cataracts associated with additional
anomalies (ocular dysmorphology and/or systemic anomalies denoted
cataract plus). Data on cataract morphology were grouped into nuclear/
zonular and other (non-nuclear).
In the rst categorization, cataract surgery was divided into three
groups: (1) Cataract surgery by lensectomy using either a suction
From the
1
Department of Epidemiology Research, Statens Serum
Institut, Copenhagen, Denmark; the
2
Department of Ophthalmology,
Glostrup University Hospital, Copenhagen, Denmark; the
3
Department
of Ophthalmology, Rigshospitalet, University Hospital of Copenhagen,
Copenhagen, Denmark; and the
4
Department of Ophthalmology, Aar-
hus University Hospital, Aarhus, Denmark.
Supported by the Carl and Nicoline Larsen Foundation.
Submitted for publication September 5, 2007; revised December
29, 2007; accepted March 24, 2008.
Disclosure: B. Haargaard, None; C. Ritz, None; A. Oudin, None;
J. Wohlfahrt, None; J. Thygesen, None; T. Olsen, None; M. Melbye,
None
Presented in part at the 37th annual meeting of the Nordic Con-
ference of Ophthalmology (NOK 37), Copenhagen, Denmark, June
2006.
The publication costs of this article were defrayed in part by page
charge payment. This article must therefore be marked advertise-
ment in accordance with 18 U.S.C. 1734 solely to indicate this fact.
Corresponding author: Birgitte Haargaard, Department of Epide-
miology Research, Statens Serum Institut, Artillerivej 5, DK-2300
Copenhagen, Denmark; bgd@ssi.dk;birgitte@haargaard.dk.
Investigative Ophthalmology & Visual Science, May 2008, Vol. 49, No. 5
Copyright Association for Research in Vision and Ophthalmology 1791
irrigation technique or phacoemulsication with or without posterior
capsulorrhexis or capsulotomy; (2) cataract surgery by lensectomy by
either the suctionirrigation technique or phacoemulsication with
posterior capsulorrhexis and anterior vitrectomy; and (3) unspecied.
We made another categorization to investigate whether the risk of
glaucoma is associated with a break in the posterior capsule and
thereby a risk of vitreous in the anterior chamber and trabecular
meshwork.
28
Accordingly, the second categorization consisted of
lensectomy leaving an intact posterior capsule and lensectomy with a
break in the posterior capsule or posterior capsulorrhexis, both at the
primary surgery.
The use of intraocular pressure (IOP) as the sole indicator of
glaucoma is probably not sufcient, especially in young children, in
whom, for example, myopic shift or increased optic disc cupping may
be the rst sign of glaucoma.
29
We therefore dened glaucomatous
eyes as eyes that the consultant decided required permanent medical
therapy and/or surgical therapy (trabeculectomy and/or diode laser
transscleral cyclophotocoagulation). Eyes with transient elevation of
IOP that could be controlled with an iridectomy or anterior vitrectomy
were not dened as cases of secondary glaucoma.
We excluded cataract cases that did not have a postoperative
measurement of IOP, because a postoperative measurement of IOP
was taken as a proxy for a glaucoma evaluation, and without a glau-
coma evaluation the cases could not be classied as glaucoma or
nonglaucoma cases.
Permission to receive data from the national registries was obtained
from the Danish Data Protection Agency (2000-41-0285). The study
was approved by the Scientic-Ethical Committees for Copenhagen
and Frederiksberg (KF) 01-253/00), and it adhered to the tenets of the
Declaration of Helsinki.
Statistical Analyses
All analyses were based on eyes as the unit. The rate ratios (RRs) of
glaucoma after surgery of pediatric cataract according to age at surgery
and various characteristics were estimated by a Cox proportional
hazards regression model (the Proc Phreg feature of SAS statistical
software; SAS, Cary, NC). Time at risk (i.e., follow-up time) was dened
for each eye as the time from surgery until glaucoma diagnosis, last
measurement of IOP, emigration, or death, whichever came rst. Time
of glaucoma diagnosis was dened as the interval midpoint between
time of last measurement without glaucoma and rst with glau-
coma. In two additional sensitivity analyses, time of glaucoma diag-
nosis was dened as time of last measurement without glaucoma and
time of rst measurement with glaucoma, respectively. Adjustment
for age at surgery was performed by including age in the regression
model with the following categories (in months): 0 to 1, 1 to 2, 2 to
3, 3 to 4, 4 to 5, 5 to 6, 6 to 9, 9 to 12, 12 to 15, 15 to
18, 18 to 21, 21 to 24, 24 to 36, 36 to 48, 48 to 60, 60 to
72, 72 to 84, and 84. Adjustment for correlation between eyes
was obtained using robust standard errors,
30
resulting in slightly wider
condence intervals on estimated RRs. In the Cox proportional hazards
model proportional hazards are assumed over time. That the hazards
were proportional over time since surgery was supported by the fact
that there were no effect modications by time since surgery (see the
Results section). Proportion of children without glaucoma at a given
time after surgery was estimated by Kaplan-Meier estimates (Proc
Liftest; SAS).
RESULTS
Overall, 202 patients with a validated diagnosis of pediatric
cataract did not undergo cataract surgery, most because the
cataract was not visually signicant. These patients were not
included in the analyses. None of them was registered with
glaucoma surgery or received any antiglaucoma medical treat-
ment, and almost half of the cases had a registration of a normal
IOP measurement. In most of the nonsurgical cases, repeated
examinations by ophthalmologists had not revealed glaucoma.
Of 697 eligible patients with pediatric cataract and surgery,
we subsequently excluded surgically treated eyes that lacked
any postoperative measurement of IOP, as IOP was used as a
proxy for an evaluation of glaucoma. A total 946 eyes (595
patients: 306 males, and 289 females) remained in the study.
Bilateral lensectomy was performed in 351 patients (702 eyes),
and 244 patients had unilateral cataract surgery, 62 patients of
the latter group having bilateral cataract. The median follow-up
time since surgery was 4.2 years (25% quartile, 0.67 years; 75%
quartile, 9.7 years).
Secondary glaucoma developed in 72 (48 patients) of the
946 eyes that had had cataract surgery. Bilateral glaucoma was
present in 24 patients. The median time interval between
surgery and glaucoma diagnosis was 6.6 years (25% quartile,
1.1 years; 75% quartile, 10.7 years).
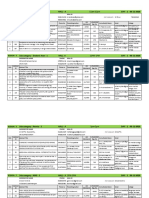
Table 1 gives the number of surgically treated and subse-
quently glaucomatous eyes and median follow-up time by age
at surgery. The risk of glaucoma after cataract surgery was
highly dependent on age at surgery (P 0.001). Compared
with children who underwent surgery at an age of 2 years or
more, the RR of glaucoma was increased between 5.8- and
9.4-fold among children undergoing surgery within the rst 8
months of life (Table 1). During the rst 8 months of age, the
risk of glaucoma did not vary signicantly by age at surgery.
Table 2 presents the cumulative risk of glaucoma by years
since surgery, according to whether children had had cataract
surgery before or after 9 months of age.
We further investigated the inuence of surgical proce-
dures, cataract presentation, and cataract etiology on the sub-
sequent risk of glaucoma. Table 3 gives the RRs of developing
glaucoma according to type of surgery, surgery for secondary
cataract, other ocular anomalies, cataract etiology, clinical
TABLE 1. Number of Surgical Eyes and Subsequently Glaucomatous Eyes, Median Follow-up Time, and RR Stratied by Age at Surgery and Time
since Cataract Surgery
Age at Surgery
(mo)
Surgical
Eyes (n)
Glaucomatous
Eyes, n (%)
Median Follow-up
Time (y)
10-y risk
(95% CI) RR (95% CI)
01* 39 10 (26) 6.2 30.5 (15.055.7) 9.4 (3.624.1)
2 30 5 (17) 3.6 22.9 (8.354.0) 5.8 (2.116.1)
35 116 25 (22) 5.5 34.4 (23.848.0) 7.8 (3.915.7)
68 52 12 (23) 4.4 34.4 (19.655.7) 8.5 (3.520.5)
911 30 1 (3) 7.9 0 0.92 (0.126.86)
1223 59 4 (7) 6.5 8.1 (2.524.2) 2.0 (0.646.3)
24 620 15 (2) 2.9 3.7 (2.16.7) 1
08 237 52 (22) 5.3 31.9 (24.441.1) 7.2 (4.112.5)
9 709 20 (3) 3.8 4.1 (2.46.8) 1
* Includes the rst 8 weeks of life. Seven subjects underwent surgery during the rst 4 weeks of life, and glaucoma developed in one.
1792 Haargaard et al. IOVS, May 2008, Vol. 49, No. 5
manifestation of the cataract, laterality, implantation of intraoc-
ular lens, and cataract morphology. The unadjusted risk of
glaucoma was lower in eyes who had a primary intraocular lens
implantation and higher in eyes having had surgery by lensec-
tomy with posterior capsulorrhexis and anterior vitrectomy, in
eyes where the posterior capsule was not left intact, in eyes
with preoperative nystagmus, and in eyes with cataract asso-
ciated with other ocular and/or systemic disease (cataract
plus). However, none of these variables remained signicantly
associated with glaucoma after adjustment for age at surgery.
Further stratication by age at surgery (before and at or after
9 months of age) revealed effect modications by age at surgery
for laterality and for microcornea. In eyes of children aged 9
months or more at surgery, there was a higher risk of glaucoma
associated with having unilateral cataract (P
effect modication
0.03) and microcornea (P
effect modication
0.0001); however, the
majority (77%) of patients with unilateral cataract underwent
surgery at more than 9 months of age, whereas the majority (71%)
of eyes with microcornea underwent surgery at less than 9
months. The RRs of the variables given in Table 3 did not differ
depending on time since surgery (5 years, data not shown).
In subsequent analyses with adjustment for age at surgery, we
tested whether cataract surgery by pars plana lensectomy and
vitrectomy differed in glaucoma risk from other types of surgery,
but found that they had similar rate ratios (RR
pars plana versus other
0.75; 95% CI, 0.202.76). Moreover, there was no difference in
the glaucoma risk between right and left eyes (RR
left versus right
0.98; 95% CI, 0.721.33), between sexes (RR
boy versus girl
0.85;
95%CI, 0.471.54), or according to the surgical experience of the
ophthalmologist (RR 50 vs. 50 surgeries 0.62; 95% CI,
0.341.15).
Time of glaucoma diagnosis is not necessarily the same as
the time of debut. We therefore used the midpoint between
cataract surgery or last normal measurement of IOP until glau-
coma was rst registered as an approximation of the time of
debut. Additional sensitivity analyses using right and left end-
points instead of midpoints revealed that the conclusions
drawn were not dependent on this approximation.
In addition to the 946 surgical eyes included in the analyses,
there were 91 patients (134 eyes) for whom we had a date of
latest visit to an ophthalmologist but no postoperative mea-
surement of IOP, and 11 patients (14 eyes) with no record of
a postoperative visit to an ophthalmologist. As a sensitivity
analysis, we added these patients as follows: the rst group was
assigned a follow-up time equal to the time of the latest visit,
and the latter group was assigned the median follow-up time
for eyes operated on in the same 5-year calendar period. In-
cluding these eyes in the analyses and assuming that none of
them developed glaucoma gave very similar results. Compared
with eyes in children that were 9 months of age or older at
surgery, the rate of glaucoma was 7.85-fold (4.5113.66)
higher in children with age at surgery less than 9 months. The
cumulative risk estimates after 10 years in this analysis were
29.2% (95% CI, 22.2%37.8%) for those with an age at cataract
surgery of less than 9 months compared with 3.4% (95% CI,
2.0%5.7%) for those with an age at surgery of 9 months or
more.
DISCUSSION
Based on a large population-based cohort of all children who
had undergone surgery for pediatric cataract, we found age at
surgery (9 months) to be the only important factor for sub-
sequent risk of glaucoma among several potential risk factors.
Ten years after cataract surgery, 31.9% (95% CI, 24.441.1) of
the children who underwent surgery before 9 months of age
had developed glaucoma compared with 4.1% (95% CI, 2.4
6.8) of children who were older at time of surgery. None of the
children with pediatric cataract who never underwent surgery
had subsequent development of glaucoma.
The study had several strengths, including its large size and
its population-based cohort design. Based on mandatory na-
tional registration, we were able to retrieve all children with a
diagnosis of pediatric cataract and over many years to follow
these children with respect to glaucoma development. We
thereby avoided signicant problems with selection bias and
differential misclassication. Previously published larger stud-
ies on glaucoma after pediatric cataract surgery based the
denition of glaucoma on IOP.
6,11
There is a risk that in lower
age groups this denition may lead to an underestimation of
glaucoma because IOP in infancy is not always increased in
glaucoma; rather, there is often an increased cupping of the
optic disc and/or an extraordinary decrease in hyperopia,
29
in
older age groups a possible overestimation depending on the
method of measurement, but also when central corneal thick-
ness, for example, is not taken into consideration. In fact, it has
been suggested that children who had lensectomy with or
without IOL implantation have a higher corneal thickness mea-
surement and thereby the IOP measurement may be articially
elevated.
31
Because of the retrospective nature of our study,
we chose to rely on the consultants diagnosis of glaucoma
(i.e., their decision to start surgical and/or long-term medical
treatment for glaucoma) to avoid the risk of misclassication.
Furthermore, we chose to exclude cases that did not have a
postoperative measurement of IOP, because we made the
assumption that measuring the IOP was an indication of glau-
coma evaluation. Children without any postoperative glau-
coma evaluation could neither be categorized as glaucoma
cases or nonglaucoma cases. However, measuring IOP may
indicate suspicion of glaucoma or that the surgeon recognized
that the patient was in a high-risk group. We therefore per-
formed additional analyses, where we also included children
without any postoperative glaucoma evaluation and as a worst-
case scenario assumed that none of them had ever had glau-
coma. As the results of these analyses were similar to the main
results, we do not think that exclusion of children without any
postoperative glaucoma evaluation has biased our results.
Age at surgery as a risk factor for glaucoma after pediatric
cataract surgery has been investigated in previous studies and
the following age periods have been suggested to be associated
with the highest risk of glaucoma: 2 weeks of life,
15
the rst
few months of life,
12,13
9 months of age,
6
1 year of
age
4,11,14
and 15 months of age.
3
In our study, the risk of
glaucoma was signicantly lower when having surgery at the
age of 9 months. We were not able to nd any difference in
risk during the rst 8 months of life, which is comparable to
TABLE 2. Risk of Glaucoma by Time since Surgery According to Age
at Surgery
Time since
Surgery
Age at Surgery
08 Months 9 Months
1 year 5.4 (3.29.6) 0.7 (0.31.9)
2 years 7.5 (4.712.0) 1.1 (0.52.5)
3 years 8.1 (5.12.7) 1.6 (0.83.2)
4 years 9.3 (6.112.7) 1.6 (0.83.2)
5 years 12.7 (8.718.6) 1.8 (1.65.0)
6 years 18.8 (13.525.8) 1.8 (1.65.0)
7 years 21.4 (15.628.8) 3.2 (1.85.5)
8 years 26.2 (19.634.4) 3.6 (2.16.1)
9 years 31.9 (24.441.1) 4.1 (2.46.8)
10 years 31.9 (24.441.1) 4.1 (2.46.8)
Data are the RRs of glaucoma (95% CI).
IOVS, May 2008, Vol. 49, No. 5 Glaucoma after Pediatric Cataract Surgery 1793
previous ndings.
6,11
Vishwanath et al.
13
have reported that
the cumulative risk of glaucoma by 5 years among eyes oper-
ated on before 1 year of age was 15.6% (95% CI, 10.223.4),
with similar risk reported in age groups corresponding to
ours.
6
We found the cumulative risk of glaucoma 5 years after
cataract surgery to be 12.7% (95% CI, 8.718.6) for eyes of
children operated on before 9 months of age and 1.8% (95% CI,
1.65.0) for eyes undergoing surgery at 9 months of age or
afterthe corresponding statistics 10 years after surgery being
31.9% (95% CI, 24.441.1) and 4.1% (95% CI, 2.46.8), respec-
tively.
Although surgery is the necessary and sufcient event, the
exact mechanism causing the type of glaucoma after surgery
for congenital cataract is not well understood. Postoperative
inammation of the trabecular meshwork (the loss of mechan-
ical support to the trabecular meshwork) or vitreous sub-
stances that are toxic to the trabecular meshwork may be
involved.
28
There have been several reports of risk factors
associated with glaucoma,
48,12,14,1517-23,32
but with inconsis-
tent results.
Two previously published larger studies on risk factors did
not include children with primary intraocular lens implanta-
tion.
6,11
Furthermore, Rabiah
6
excluded children with a fol-
low-up of 5 years, which may have led to selection bias. The
other study, by Chen et al.,
11
was based on patients seen by a
glaucoma specialist, also leading to possible selection bias,
which is reected in the high percentage of aphakic glaucoma
reported in this study (58.7%). However, both studies found
age at surgery, microcornea, and surgery for secondary cataract
to be risk factors, and Rabiah
6
also found primary posterior
TABLE 3. RR of Developing Glaucoma According to Various Characteristics, Overall and Stratied by
Age at Cataract Surgery in Danish Children with Pediatric Cataract Diagnosed from 1977 to 2001
Variable
Glaucomatous
Eyes*
Surgical
Eyes*
RR (95% CI)
Unadjusted Adjusted
Type of surgery
Lensectomy 43 640 1 1
Lensectomy, anterior vitrectomy 27 269 2.30 (1.284.14) 1.56 (0.822.98)
Unspecied 2 37 1.07 (0.254.61)
P 0.02
1.00 (0.214.70)
P 0.39
Posterior capsule
Intact 30 506 1 1
Not intact 40 403 2.13 (1.223.72)
P 0.01
1.26 (0.682.34)
P 0.47
Surgery for secondary cataract
None 41 1 1
Once 22 1.09 (0.582.07) 1.21 (0.662.23)
Twice or more 9 1.28 (0.562.93)
P 0.82
1.15 (0.462.86)
P 0.78
Nystagmus
No 49 806 1 1
Yes 22 134 2.13 (1.114.11)
P 0.02
1.26 (0.612.59)
P 0.54
PFV
No 69 905 1 1
Yes 2 35 1.14 (0.304.39)
P 0.85
1.41 (0.375.41)
P 0.62
Microcornea
No 38 188 1 1
Yes 15 58 1.05 (0.472.34)
P 0.91
1.16 (0.472.87)
P 0.74
Etiology
Nonhereditary 50 581 1 1
Hereditary 22 343 0.69 (0.371.30)
P 0.25
0.68 (0.381.24)
P 0.21
Clinical manifestation
Isolated cataract 43 744 1 1
Cataract plus 29 202 2.26 (1.234.14)
P 0.009
1.65 (0.853.17)
P 0.14
Laterality
Bilateral 65 759 1 1
Unilateral 7 187 0.59 (0.261.32)
P 0.20
1.39 (0.583.33)
P 0.46
Primary intraocular lens implantation
No 66 619 1 1
Yes 6 327 0.37 (0.140.99)
P 0.05
0.77 (0.282.12)
P 0.61
Morphology
Other 7 212 1 1
Nuclear 35 498 1.84 (0.675.03)
P 0.23
2.19 (0.835.79)
P 0.12
* The number of cases differs between risk factors due to unspecied or missing information.
Adjusted for age at surgery.
Time dependent variable; performed before diagnosis of glaucoma.
1794 Haargaard et al. IOVS, May 2008, Vol. 49, No. 5
capsulotomyanterior vitrectomy to be a risk factor for aphakic
glaucoma. The latter result was uncertain, however, because
there were a few surgical cases involving another surgical
technique. In our study, we were able to investigate various
risk factors for glaucoma, including primary IOL implantation
and surgical technique.
In our study, we found some of these previously reported
potential risk factors (e.g., age at surgery, primary IOL implan-
tation, and surgery with posterior capsulotomy and anterior
vitrectomy) to be associated with glaucoma in univariate anal-
yses. Age at surgery turned out to be the most important risk
factor for later glaucoma development, so that when adjust-
ment was made for age at surgery, the other associations were
no longer present. Likewise, in a recent study by Trivedi et al.
16
no association between primary IOL implantation and micro-
cornea and postoperative development of glaucoma after pe-
diatric cataract surgery could be found when subjects were
stratied according to age at surgery of 6 months and 6
months.
The optimal time for congenital cataract surgery consider-
ing both visual outcome and the potential for postoperative
complications, especially glaucoma, is currently debated. To
achieve good visual acuity, early surgery (before the age of
610 weeks) depending on laterality
3236
is favored. In one
study, the risk of developing glaucoma after surgery in these
rst critical months has been reported to be highest during the
rst 4 weeks of life.
13
However, in our study, only one of seven
patients operated on within the rst month of life had subse-
quent development of glaucoma, and we saw no indication
that the effects of surgery within the rst 2 months of life differ
compared with the months immediately following, up to 8
months of age. We note, however, that few Danish infants
underwent surgery the rst month, perhaps because Denmark
lacks screening procedures (red reex) used for assessing the
presence of congenital cataract in the newborn child. Another
reason may be that surgeons previously have been reluctant to
operate on infants less than 2 months of age. Thus, we were
not able to draw any rm conclusions regarding the safety of
surgery during the very rst weeks of life.
The mean interval between primary cataract surgery and
glaucoma development has been reported to be approximately
4 to 5 years,
6,10,37
but there have been reports of cases occur-
ring several decades later.
4,5,28,37,38
It is obvious that measure-
ment of IOP and other relevant measurements such as axial
length in small children below 4 to 5 years of age are difcult,
and in most cases a comprehensive eye examination requires
general anesthesia of the infant. In Denmark there are not yet
any national recommendations on when and how frequently
children who have had surgery for pediatric cataract should be
examined. In addition, some of the cases included in this study
are from a time when the focus on glaucoma after pediatric
cataract surgery was low; hence, the discovery of glaucoma
may have been delayed in some early cases. Our study supports
that patients who undergo surgery for pediatric cataract should
be examined regularly for glaucoma throughout their lives. In
the present investigation new cases of glaucoma continued to
be diagnosed at a high rate, even 10 years after cataract sur-
gery.
In conclusion, we found that surgery for pediatric cataract
during the rst 8 months of life was associated with a substan-
tially increased risk of glaucoma, whereas surgery at 9
months of age resulted in a lower risk. Glaucoma developed
anytime after surgery, as much as 10 years later, prompting
both early and long-term follow-up of these children. However,
bilateral central and/or dense congenital cataracts often leave
the clinicians with little choice regarding age of surgery be-
cause of the risk of amblyopia, with the viable way being the
close follow-up of children with early surgical intervention.
References
1. Egbert JE, Wright MM, Dahlhauser KF, Keithahn MA, Letson RD,
Summers CG. A prospective study of ocular hypertension and
glaucoma after pediatric cataract surgery. Ophthalmology. 1995;
102:10981101.
2. Keech RV, Tongue AC, Scott WE. Complications after surgery for
congenital and infantile cataracts. Am J Ophthalmol. 1989;108:
136141.
3. Robb RM, Petersen RA. Outcome of treatment for bilateral con-
genital cataracts. Ophthalmic Surg. 1992;23:650656.
4. Mills MD, Robb RM. Glaucoma following childhood cataract sur-
gery. J Pediatr Ophthalmol Strabismus. 1994;31:355360.
5. Miyahara S, Amino K, Tanihara H. Glaucoma secondary to pars
plana lensectomy for congenital cataract. Graefes Arch Clin Exp
Ophthalmol. 2002;240:176179.
6. Rabiah PK. Frequency and predictors of glaucoma after pediatric
cataract surgery. Am J Ophthalmol. 2004;137:3037.
7. Parks MM, Johnson DA, Reed GW. Long-term visual results and
complications in children with aphakia: a function of cataract type.
Ophthalmology. 1993;100:826840.
8. Johnson CP, Keech RV. Prevalence of glaucoma after surgery for
PHPV and infantile cataracts. J Pediatr Ophthalmol Strabismus.
1996;33:1417.
9. Ariturk N, Oge I, Mohajery F, Erkan D, Turkoglu S. Secondary
glaucoma after congenital cataract surgery. Int Ophthalmol. 1998;
22:175180.
10. Simon JW, Mehta N, Simmons ST, Catalano RA, Lininger LL. Glau-
coma after pediatric lensectomy/vitrectomy. Ophthalmology.
1991;98:670674.
11. Chen TC, Bhatia LS, Halpern EF, Walton DS. Risk factors for the
development of aphakic glaucoma after congenital cataract sur-
gery. Trans Am Ophthalmol Soc. 2006;104:241251.
12. Lundvall A, Zetterstrom C. Complications after early surgery for
congenital cataracts. Acta Ophthalmol Scand. 1999;77:677680.
13. Vishwanath M, Cheong-Leen R, Taylor D, Russell-Eggitt I, Rahi J. Is
early surgery for congenital cataract a risk factor for glaucoma? Br J
Ophthalmol. 2004;88:905910.
14. Walton DS. Pediatric aphakic glaucoma: a study of 65 patients.
Trans Am Ophthalmol Soc. 1995;93:403413.
15. Watts P, Abdolell M, Levin AV. Complications in infants undergo-
ing surgery for congenital cataract In the rst 12 weeks of life: is
early surgery better? J AAPOS. 2003;7:8185.
16. Trivedi RH, Wilson ME Jr, Golub RL. Incidence and risk factors for
glaucoma after pediatric cataract surgery with and without intraoc-
ular lens implantation. J AAPOS. 2006;10:117123.
17. Asrani S, Freedman S, Hasselblad V, et al. Does primary intraocular
lens implantation prevent aphakic glaucoma in children? J
AAPOS. 2000;4:3339.
18. Biglan AW. Glaucoma in children: are we making progress? J
AAPOS. 2006;10:721.
19. Brady KM, Atkinson CS, Kilty LA, Hiles DA. Glaucoma after cataract
extraction and posterior chamber lens implantation in children. J
Cataract Refract Surg. 1997;23(suppl 1):669674.
20. Lambert SR, Buckley EG, Plager DA, Medow NB, Wilson ME.
Unilateral intraocular lens implantation during the rst six months
of life. J AAPOS. 1999;3:344349.
21. Wilson ME, Peterseim MW, Englert JA, Lall-Trail JK, Elliott LA.
Pseudophakia and polypseudophakia in the rst year of life. J
AAPOS. 2001;5:238245.
22. Plager DA, Yang S, Neely D, Sprunger D, Sondhi N. Complications
in the rst year following cataract surgery with and without IOL in
infants and older children. J AAPOS. 2002;6:914.
23. Lambert SR, Lynn M, Drews-Botsch C, et al. Intraocular lens im-
plantation during infancy: perceptions of parents and the Ameri-
can Association for Pediatric Ophthalmology and Strabismus mem-
bers. J AAPOS. 2003;7:400405.
24. Haargaard B, Wohlfahrt J, Fledelius HC, Rosenberg T, Melbye M.
Incidence and cumulative risk of childhood cataract in a cohort of
2.6 million Danish children. Invest Ophthalmol Vis Sci. 2004;45:
13161320.
25. Haargaard B, Wohlfahrt J, Fledelius HC, Rosenberg T, Melbye M. A
nationwide Danish study of 1027 cases of congenital/infantile
IOVS, May 2008, Vol. 49, No. 5 Glaucoma after Pediatric Cataract Surgery 1795
cataracts: etiological and clinical classications. Ophthalmology.
2004;111:22922298.
26. Tucker SM, Enzenauer RW, Levin AV, Morin JD, Hellmann J.
Corneal diameter, axial length, and intraocular pressure in prema-
ture infants. Ophthalmology. 1992;99:12961300.
27. Larsen JS. The sagittal growth of the eye. IV. Ultrasonic measure-
ment of the axial length of the eye from birth to puberty. Acta
Ophthalmol (Copenh). 1971;49:873886.
28. Asrani SG, Wilensky JT. Glaucoma after congenital cataract sur-
gery. Ophthalmology. 1995;102:863867.
29. Egbert JE, Kushner BJ. Excessive loss of hyperopia. Arch Ophthal-
mol. 1990;108:12571259.
30. Lin DY, Wei LJ. The robust inference for the Cox proportional
hazards model. J Am Stat Assoc. 1989;84:10741078.
31. Simon JW, OMalley MR, Gandham SB, et al. Central corneal thick-
ness and glaucoma in aphakic and pseudophakic children. J
AAPOS. 2005;9:326329.
32. Lundvall A, Kugelberg U. Outcome after treatment of congenital
unilateral cataract. Acta Ophthalmol Scand. 2002;80:588592.
33. Birch EE, Stager DR. The critical period for surgical treatment of
dense congenital unilateral cataract. Invest Ophthalmol Vis Sci.
1996;37:15321538.
34. Gelbart SS, Hoyt CS, Jastrebski G, Marg E. Long-term visual results
in bilateral congenital cataracts. Am J Ophthalmol. 1982;93:615
621.
35. Lundvall A, Kugelberg U. Outcome after treatment of congenital
bilateral cataract. Acta Ophthalmol Scand. 2002;80:593597.
36. Lambert SR, Lynn MJ, Reeves R, Plager DA, Buckley EG, Wilson ME.
Is there a latent period for the surgical treatment of children with
dense bilateral congenital cataracts? J AAPOS. 2006;10:3036.
37. Chen TC, Walton DS, Bhatia LS. Aphakic glaucoma after congenital
cataract surgery. Arch Ophthalmol. 2004;122:18191825.
38. Phelps CD, Arafat NI. Open-angle glaucoma following surgery for
congenital cataracts. Arch Ophthalmol. 1977;95:19851987.
1796 Haargaard et al. IOVS, May 2008, Vol. 49, No. 5
Vous aimerez peut-être aussi
- Bronchodilators and Other Drugs Used in AsthmaDocument61 pagesBronchodilators and Other Drugs Used in AsthmazingioPas encore d'évaluation
- Relaxation Techniques For People With Epilepsy:: Some Benefits and CautionsDocument3 pagesRelaxation Techniques For People With Epilepsy:: Some Benefits and CautionszingioPas encore d'évaluation
- Brain Tumors Final 001Document50 pagesBrain Tumors Final 001zingioPas encore d'évaluation
- Jurnal 2Document12 pagesJurnal 2zingioPas encore d'évaluation
- Obstructed LaborDocument14 pagesObstructed LaborzingioPas encore d'évaluation
- Obstructed LaborDocument14 pagesObstructed LaborzingioPas encore d'évaluation
- A Second Stage Partogram.7Document6 pagesA Second Stage Partogram.7zingioPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Anatomy and Physiology of The Maxillary Sinus: Harold A. Dehaven, JRDocument8 pagesAnatomy and Physiology of The Maxillary Sinus: Harold A. Dehaven, JRkhanhlinhPas encore d'évaluation
- Cardiac Sarcoidosis EHJ Review 2023Document16 pagesCardiac Sarcoidosis EHJ Review 2023AnaPas encore d'évaluation
- NCP: Nursing Care Plan For Bone FracturesDocument8 pagesNCP: Nursing Care Plan For Bone FracturesElham TabaoPas encore d'évaluation
- Resume of Od1206Document3 pagesResume of Od1206api-23436180Pas encore d'évaluation
- فحص جراحة 11Document144 pagesفحص جراحة 11Ola AlaaPas encore d'évaluation
- Labeled ItDocument50 pagesLabeled ItKaloy KamaoPas encore d'évaluation
- 2011 Surgery IIDocument67 pages2011 Surgery IIamruthkiranbabuji100% (1)
- ACVIM Consensus Statement: J.P. Lulich, A.C. Berent, L.G. Adams, J.L. Westropp, J.W. Bartges, and C.A. OsborneDocument11 pagesACVIM Consensus Statement: J.P. Lulich, A.C. Berent, L.G. Adams, J.L. Westropp, J.W. Bartges, and C.A. OsborneAlana SoaresPas encore d'évaluation
- Anaesthesia For Neurosurgery-PIIS1472029919302656Document6 pagesAnaesthesia For Neurosurgery-PIIS1472029919302656james Wilson09Pas encore d'évaluation
- 5 IV CannulationDocument61 pages5 IV CannulationNursing Superintendent (SH)Pas encore d'évaluation
- Dynamic AuscultationDocument47 pagesDynamic AuscultationSrinivas PingaliPas encore d'évaluation
- ASGE 2012 Endoscopy in Pregnant and Lactating WomenDocument7 pagesASGE 2012 Endoscopy in Pregnant and Lactating WomenjordanPas encore d'évaluation
- A Glossary of Anesthetic Jargon .8Document4 pagesA Glossary of Anesthetic Jargon .8TonyPas encore d'évaluation
- Chapter 8 Self-Assessment Q&ADocument5 pagesChapter 8 Self-Assessment Q&Apblinder1319Pas encore d'évaluation
- Jurnal AccDocument4 pagesJurnal AccAdi W. YengPas encore d'évaluation
- Evaluation of Two Methods of Endotracheal Tube Selection in DogsDocument7 pagesEvaluation of Two Methods of Endotracheal Tube Selection in DogsFelipe Guajardo HeitzerPas encore d'évaluation
- Brochure 2023 Final 0 1683636102Document14 pagesBrochure 2023 Final 0 1683636102KhushaliPas encore d'évaluation
- Ophthalmology 5Th Edition Myron Yanoff Lead Editor Download PDF ChapterDocument51 pagesOphthalmology 5Th Edition Myron Yanoff Lead Editor Download PDF Chaptermary.hanna173100% (5)
- Chronic Osteomyelitis PPT OrthoDocument21 pagesChronic Osteomyelitis PPT OrthoPrageeth RPas encore d'évaluation
- Post TestDocument11 pagesPost Testoomculun100% (6)
- LESSON 2 - Science 9 (Module 1-Activities)Document3 pagesLESSON 2 - Science 9 (Module 1-Activities)leizl MoncadaPas encore d'évaluation
- Pre Op GuidelinesDocument11 pagesPre Op GuidelinesHanif FebrianPas encore d'évaluation
- Lorma Colleges College of Physical and Respiratory TherapyDocument33 pagesLorma Colleges College of Physical and Respiratory TherapyAnab Mohamed Elhassan Abbas AlnowPas encore d'évaluation
- AAO Network GlaucomaDocument59 pagesAAO Network Glaucomasafasayed100% (1)
- Skeletal Anchorage in OrthodonticsDocument8 pagesSkeletal Anchorage in OrthodonticsNingombam Robinson SinghPas encore d'évaluation
- Forcep Delivery LPDocument7 pagesForcep Delivery LPSandhya Gupta100% (1)
- Stereotactic and Functional NeurosurgeryDocument114 pagesStereotactic and Functional NeurosurgerymichaelPas encore d'évaluation
- Developmental Dysplasia of The HipDocument16 pagesDevelopmental Dysplasia of The Hipjonathan_alvaPas encore d'évaluation
- Kumpulan Jurnal JantungDocument200 pagesKumpulan Jurnal JantungMaya RustamPas encore d'évaluation
- Free Paper Programme FinalDocument18 pagesFree Paper Programme FinalShiwali SinghPas encore d'évaluation