Académique Documents
Professionnel Documents
Culture Documents
Poljradiol 75 3 51
Transféré par
masbima_putro0 évaluation0% ont trouvé ce document utile (0 vote)
16 vues4 pagesNeurosurgical treatment of drug-resistant epilepsy on the basis of a fusion of MRI and SPECT images. Epilepsy concerns at least 0.5% of population and in most cases (approx. 70%) can be treated pharmacologically, which helps prevent seizures. In all other patients, such a treatment does not produce the desired results. Their condition may require neurosurgical management.
Description originale:
Titre original
poljradiol-75-3-51
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentNeurosurgical treatment of drug-resistant epilepsy on the basis of a fusion of MRI and SPECT images. Epilepsy concerns at least 0.5% of population and in most cases (approx. 70%) can be treated pharmacologically, which helps prevent seizures. In all other patients, such a treatment does not produce the desired results. Their condition may require neurosurgical management.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
16 vues4 pagesPoljradiol 75 3 51
Transféré par
masbima_putroNeurosurgical treatment of drug-resistant epilepsy on the basis of a fusion of MRI and SPECT images. Epilepsy concerns at least 0.5% of population and in most cases (approx. 70%) can be treated pharmacologically, which helps prevent seizures. In all other patients, such a treatment does not produce the desired results. Their condition may require neurosurgical management.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
Neurosurgical treatment of drug-resistant epilepsy on
the basis of a fusion of MRI and SPECT images case
report
Elbieta Jurkiewicz
1
, Monika Bekiesiska-Figatowska
2
, Jolanta Miko
3
,
Anna Kamiska
4
, Stanisaw Kwiatkowski
5
, Iwona Terczyska
6
1
MRI Laboratory, The Childrens Memorial Health Institute, Warsaw, Poland
2
Department of Imaging Diagnostics, Institute of Mother and Child, Warsaw, Poland
3
Laboratory of Nuclear Medicine, Midzyleski Specialist Hospital in Warsaw, Warsaw, Poland
4
Laboratory of Nuclear Medicine, The Childrens Memorial Health Institute, , Warsaw, Poland
5
Department of Neurosurgery, University Childrens Hospital of Cracow, Cracow, Poland
6
Department of Neurology of Children and Adolescents, Institute of Mother and Child, , Warsaw, Poland
Authors address: Elbieta Jurkiewicz, MRI Laboratory, The Childrens Memorial Health Institute, Warsaw, Poland,
e-mail: e-jurkiewicz@o2.pl
Summary
Background: Epilepsy concerns at least 0.5% of population and in most of the cases (approx. 70%) can be treated
pharmacologically, which helps to prevent seizures. In all other patients, such a treatment does not
produce the desired results. Their condition may require neurosurgical management. The aim of
this work was to fuse anatomical MRI images and functional SPECT images in patients with drug-
resistant epilepsy, without structural changes on MRI or with changes so severe that it would be
impossible to establish which ones are responsible for seizures. The authors presented a case of a
child subjected to a neurosurgical procedure carried out on the basis of the fused MRI and SPECT
images.
Case Report: A seven-year-old boy with an extensive defect of the right hemisphere (cortical dysplasia with
multiple balloon-like cells) operated on three times due to a history of treatment-resistant seizures
present since the age of one. A subsequent MRI examination was performed with magnetic field
intensity of 1.5 T, within a routine epilepsy protocol applying volumetric thin-slice T1-weighted
images. Next, in the interictal period, a SPECT examination was performed with the use of the
99m
Tc-labelled ethyl cysteinate dimer (
99m
TcECD). For fusion and postprocessing, the following
software was used: PMOD (Biomedical Image Quantification PMOD Technologies) with PFUS
(Flexible Image Matching and Fusion Tool) and a program for a quantitative analysis of counts
in the region of interest, so called VOI Constructor (Volume of Interest Constructor). On the basis
of the fusion of images, the boy was subjected to the next operation procedure. The remaining
fragments of the right frontal and parietal lobe adjacent to the occipital lobe were removed. Seizure
remission was obtained and it was already 31 months long when we were writing this article.
Conclusions: Owing to this multi-stage procedure, it was possible to avoid a total anatomical and functional
hemispherectomy. This allowed for a resection limited to regions indicated by integrated imaging.
Removal of cortical areas including lesions was advantageous in this presented case, as it allowed
for saving active regions of the brain.
Key words: drug-resistant epilepsy brain magnetic resonance imaging (MRI) single photon emission computed
tomography (SPECT) fusion of the images
PDF fi le: http://www.polradiol.com/fulltxt.php?ICID=881149
Received: 2010.04.26
Accepted: 2010.07.08
Signature: Pol J Radiol, 2010; 75(3): 51-54
51
CASE REPORT
Background
Epilepsy concerns at least 0.5% of population and in most
of the cases (approx. 70%) can be treated pharmacologically,
which helps to prevent seizures [1,2]. In all other patients,
such a treatment does not produce the desired results.
Their condition may require neurosurgical management.
A precise localisation of the seizure-onset focus is essen-
tial to plan the range of the neurosurgical procedure, and
to minimise the risk of postoperative neurological deficits.
An invasive EEG is used to localise the focus in a direct
way: deep electrocorticography and intraoperative elec-
trocorticography [3,4]. But of course, noninvasive methods
are preferred. These are imaging examinations, including:
computed tomography (CT) and magnetic resonance ima-
ging (MRI), as well as methods related to nuclear medici-
ne: positron emission tomography (PET), and a more ava-
ilable one - single photon emission computed tomography
(SPECT). CT and MRI detect structural abnormalities of the
brain, while SPECT and PET perfusion and metabolism
disorders. However, the SPECT method does not reveal a
sufficient spatial resolution in order to show precisely the
location of a seizure-onset focus. The MRI examination, on
the other hand, allows for a precise anatomical localisation,
but does not reveal an adequate sensitivity. Therefore, the
aim of the work was to fuse anatomical MRI images and
functional SPECT images in patients with drug-resistant
epilepsy, without structural changes on MRI or with chan-
ges so severe that it would be impossible to establish which
ones are responsible for seizures. We presented a case of a
child subjected to a neurosurgical procedure carried out on
the basis of the fused MRI and SPECT images.
Case Report
A seven-year-old boy, the first child of young and healthy
parents without any family history of epilepsy, with an
extensive defect of the right hemisphere, operated on three
times due to treatment-resistant seizures present since the
age of one. Previous pharmacotherapy included all antie-
pileptic medicines available on the Polish market, at the
highest possible doses, in different regimens, including 25
drugs, without any spectacular results (some of the drugs
increased the seizures or caused aggression). Complex partial
seizures, of changing morphology, were present every day, in
the number ranging from a few to a few dozens a day. The
development of the boy was severely retarded. Neurological
examination showed severe spastic paresis of the left limbs.
The first surgery, performed at the age of 4, consisted in
removing (according to the SPECT and EEG image) the pal-
lium of the right parietal lobe and in undercutting the cor-
tex of the temporal, right occipital, and frontal lobe in the
parasagittal area. Histopathological examination showed
a cortical dysplasia with multiple balloon-like cells. Four
months later, after an infection, there appeared seizures of
the upper limb. Attempted modifications of the pharma-
cological treatment did not result in any clinical improve-
ment. In the second neurosurgical procedure, performed on
the basis of the SPECT and EEG image, the frontal lobe was
exposed, up to its base. With incision of the borderline of
the cortex and the white matter, the pallium was removed
up to the frontal horn of the right lateral ventricle.
There was an improvement which persisted for a few mon-
ths. Afterwards, there appeared seizures of a new type:
psychomotor with vegetative symptoms. EEG was sugge-
stive of focus formation in the left hemisphere, in the pre-
frontal/frontal area. Callosotomy was performed 2/3 of
corpus callosum were incised in the front. Due to a widened
ventricular system and an enlarged porencephalic cyst fol-
lowing hemispherectomy, a drainage system was implanted
between the porencephalic cyst and the peritoneal cavity.
In the next 2 years, the childs condition was good.
A next acute infection led to seizures with a clinically defi-
ned onset within deep frontal areas. There followed deve-
lopmental regress as well. One more change of antiepileptic
treatment failed again. An MRI was carried out with the
use of volumetric thin-slice T1-weighted images.
Next, in the interictal period, a SPECT examination was
performed with the use of the
99m
Tc-labelled ethyl cyste-
inate dimer (
99m
TcECD).
For fusion and postprocessing, the following software
was used: PMOD (Biomedical Image Quantification PMOD
Technologies) with PFUS (Flexible Image Matching and
Fusion Tool) and a program for a quantitative analysis of
counts in the region of interest, so called VOI Constructor
(Volume of Interest Constructor).
Owing to the method of interpolation, SPECT images were
not only adjusted to the anatomical MRI image, but also
made uniform with respect to spatial resolution, and divi-
ded into the same number of transverse sections, with
exactly the same thickness of each section as in the MRI (so
called corregistered data).
In the fused MRI and SPECT image, in the obtained transver-
se, sagittal and coronary sections, the location of the lesions
was determined, in which the initially visually evaluated
perfusion defect overlapped with the grey matter of the cor-
tex measuring at least 0.5 cm
3
. A mean number of counts in
the anatomically-adjusted region was compared with a mean
number of counts within the brain, which was accepted as a
reference value, defining the border between a normal and a
decreased brain perfusion. The mean count in the anatomi-
cally-adjusted region was also compared with the mean count
in a corresponding region in the other hemisphere (a differen-
ce of >15% was assumed as a verification of the deficit).
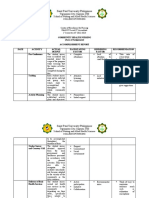
Three regions with visually detected perfusion deficits (in
the medial part of the right temporal lobe, in the remaining
part of the right frontal lobe and in a fragment of the right
parietal lobe) were subjected to the above presented quan-
titative evaluation. The qualitative analysis showed that
two of the three regions; the remaining part of the right
frontal lobe (Figure 1) and of the right parietal lobe meet
the conditions of perfusion deficit (Table 1).
The outcomes of the integrated neuroimaging were com-
pared with clinical data and EEG in which the focus was
found in centroparietal leads, on the right.
On the basis of the image fusion, the boy was subjected
to one more procedure. The remaining fragments of the
Case Report
52
Pol J Radiol, 2010; 75(3): 51-54
frontal and parietal lobe adjacent to the occipital lobe were
removed.
Seizure remission was obtained and it was already 31 mon-
ths long when we were writing this article. EEG showed
a slow basic activity in the frontal-central-parietal and
right anterior temporal region, without any distinct chan-
ges of epileptic type. However, due to the characteristics
and extension of the defect and a serious past course of the
disease, the boy is still being administered CBZ and VPA in
the therapeutic doses (remaining unchanged for over two
years). A systematic developmental progress is observed;
paresis of the left limbs is currently of moderate degree.
Discussion
Noninvasive tests visualizing brain activity can be divi-
ded into those carried out during an epileptic seizure (ictal
SPECT) or interictally (interictal SPECT and other: MRI, CT,
PET). From among the other ones, PET reveals the highest
sensitivity in the detection of the seizure-onset foci in
patients with temporal lobe epilepsy (84%), while the sen-
sitivity of SPECT (interictal) amounts to 66%, and of MRI to
55%. In nontemporal lobe epilepsy, the highest sensitivity
is revealed by interictal SPECT (60%); MRI and PET 43%
and 33%, respectively. However, the highest sensitivity of
all has ictal SPECT 90% in the temporal epilepsy and 81%
in the nontemporal one [5,6]. SPECT carried out during an
epileptic seizure shows foci of hyperperfusion. In the inte-
rictal period, perfusion deficits correspond to them.
Inability to show structural changes makes the MRI exami-
nation of the brain inappropriate for planning the resection
of seizure-onset foci. It is the same with multiple lesions,
e.g. in tuberous sclerosis, or in case of one but extensive
lesion, when it is not known which part of it is responsible
for seizures, and removal of the whole lesion is impossible.
Detection of a focus of abnormal perfusion/metabolism in
SPECT, on the other hand, is insufficient to plan a neuro-
surgical procedure, due to inadequate spatial resolution of
this method.
In patients with drug-resistant epilepsy qualified for surge-
ry, it is necessary to perform both examinations and to fuse
their images with a specialist software. This should allow
for a precise determination of the focus and then, after
downloading of the data to neuronavigation system, the
resection of the lesion [7]. The literature involves reports
on methodology and usefulness of the fusion of images in
the localisation of epileptogenic foci [8,9].
The reported case concerned drug-resistant epilepsy
manifesting itself with everyday seizures in the number
reaching a few dozens a day, in a boy with cortical dys-
plasia. Malformations of cortical development (MCD), inc-
luding cortical dysplasia, constitute a common cause of
drug-resistant epilepsy [10]. An additional difficulty in our
case was the fact that the boy had already been subjected
to surgical procedures three times, with seizure recurrence.
With the use of MRI, it would be completely impossible to
distinguish the focus responsible for the next recurrence,
Mean count
in the region
Mean count
in the brain
Mean count in a
corresponding region
of the contralateral
hemisphere
Percentage diference
ROI ROI in the other
hemisphere
ROI 1 (right frontal lobe) 177 193 232 >20%
ROI 2 (right parietal lobe) 175 193 234 >20%
Table 1. Quantative analysis of SPECT activity in the regions with perfusion defects.
Figure 1. MRI image (A). Fusion of the MRI and SPECT image in the interictal phase (B) with a marked region of perfusion defcit within a fragment
of the right frontal lobe, left after the previous surgical procedure (ROI 1 white colour). A corresponding region in the frontal lobe of the
left hemisphere, marked with black colour, revealing a normal perfusion in the SPECT examination.
Pol J Radiol, 2010; 75(3): 51-54 Jurkiewicz E et al Neurosurgical treatment of drug-resistant epilepsy
53
from all the extensive cortico-subcortical scars after sur-
geries and from the remaining abnormal cortex. Only the
fusion of thin-slice volumetric MRI images and SPECT exa-
mination with the calculation of mean counts in SPECT in
the region of the cortex defined on the basis of the MRI,
allowed for indication of the most probable locations of the
seizure-onset focus. Finally, the surgery (despite so many
attempts and stages) allowed for resignation from a com-
plete anatomical and functional hemispherectomy. The
operation could be restricted to regions indicated by inte-
grated imaging. Resection of the abnormal regions within
the cortex was advantageous in case of the presented child,
as it allowed for saving the active areas. Implantation of
a valve due to the development of free fluid regions can
be called a neurosurgical failure but regarding the achie-
ved result, this is the option connected with the least side
effects. The conducted procedures differ from classic hemi-
spherectomies and produced a good clinical result and a
safe postoperative course.
Conclusions
1. Fusion of MRI and SPECT images allows for combining a
high sensitivity of the isotopic method (in the detection
of seizure-onset foci) with a high spatial resolution of the
MRI method.
2. Owing to the surgical procedure carried out on the basis
of fused MRI and SPECT images, it was possible to avoid
a total anatomical and functional hemispherectomy and
to limit the resection to the regions indicated by integra-
ted imaging, saving the active regions.
3. Surgery based on fused images is, according to a neuro-
surgeon, the best method to plan a resection in case of
cortical dysplasia.
1. Won HJ, Chang KH, Cheon JE et al: Comparison of MR imaging with
PET and ictalSPECT in 118 patients with intractable epilepsy. Am J
Neuroradiol, 1999; 20: 59399
2. Goffin K, Dedeuwaerdere S, Van Laere K et al: Neuronuclear
assessment of patients with epilepsy. Semin Nucl Med, 2008; 38(4):
22739
3. Dupont P, Van PaesschenW, Palmini A et al: Ictal perfusion patterns
associated with single MRI-visible focal dysplastic lesions:
implications for the noninvasive delineation of the epileptogenic
zone. Epilepsia, 2006; 47(9): 155057
4. Vera P, Kaminska A, Cieuta C et al: Use of subtraction ictal SPECT
co-registered to MRI for optimizing the localization of seizure foci in
children. J Nucl Med, 1999; 40(5): 78692
5. Spencer SS: The relative contributions of MRI, SPECT, and PET
imaging in epilepsy. Epilepsia, 1994; 35(Suppl.6): S7289
References:
6. Spencer SS, Theodore WH, Berkovic SF: Clinical applications: MRI,
SPECT, and PET. Magn Reson Imaging, 1995; 13: 111924
7. Murphy MA, OBrien TJ, Morris K et al: Multimodality image-
guided surgery for the treatment of medically refractory epilepsy. J
Neurosurg, 2004; 100(3): 45262
8. Grova C, Jannin P, Biraben A et al: A methodology for generating
normal and pathological brain perfusion SPECT images for
evaluation of MRI/SPECT fusion methods: application in epilepsy.
Phys Med Biol, 2003; 48(24): 402343
9. Matthews R, Franceschi D, Xia W et al: Parietal lobe epileptic focus
identified on SPECT-MRI fusion imaging in a case of epilepsia
partialis continua. Clin Nucl Med, 2006; 31(12): 82628
10. Sporis D, Hajnsek S, Boban M et al: Epilepsy due to malformations of
cortical development correlation of clinical, MRI and Tc-99mECD
SPECT findings. Coll Antropol, 2008; 32(2): 34550
Case Report
54
Pol J Radiol, 2010; 75(3): 51-54
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Essential Guide For Good Prostate Health: in This Issue - .Document9 pagesThe Essential Guide For Good Prostate Health: in This Issue - .untarai100% (1)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Reaching Every Purok RevDocument16 pagesReaching Every Purok RevJonathan Renier VerzosaPas encore d'évaluation
- ReflectionDocument11 pagesReflectionSarahJane100% (1)
- Referat Mata KeratititsDocument28 pagesReferat Mata KeratititsjantyPas encore d'évaluation
- ACA 122-My Academic Plan (MAP) Assignment: InstructionsDocument5 pagesACA 122-My Academic Plan (MAP) Assignment: Instructionsapi-557842510Pas encore d'évaluation
- Practice - English Lesson - Fira Yuniar - 200704009Document5 pagesPractice - English Lesson - Fira Yuniar - 200704009Fira YuniarPas encore d'évaluation
- IV TherapyDocument6 pagesIV TherapySarah SPas encore d'évaluation
- Proper Pet Care in BangladeshDocument2 pagesProper Pet Care in BangladeshNoshin NawarPas encore d'évaluation
- Coping With Addiction: 6 Dysfunctional Family RolesDocument4 pagesCoping With Addiction: 6 Dysfunctional Family RolesMy LanePas encore d'évaluation
- Planned Parenthood: by Alyssa Lynd & Eunice HanDocument17 pagesPlanned Parenthood: by Alyssa Lynd & Eunice HanSangamesh SarjaPas encore d'évaluation
- Antenatal Therapy For Fetal Supraventricular TachyarrhythmiasDocument14 pagesAntenatal Therapy For Fetal Supraventricular TachyarrhythmiasandreaPas encore d'évaluation
- Successful Aging and Frailty Opposite Sides of The SameDocument5 pagesSuccessful Aging and Frailty Opposite Sides of The SameGary Xavier Puc CetzPas encore d'évaluation
- Final English 211c Part ADocument4 pagesFinal English 211c Part Aapi-341958041Pas encore d'évaluation
- Post Diwali Detox ChallengeDocument4 pagesPost Diwali Detox ChallengeAditya MehtaPas encore d'évaluation
- Family PlanningDocument42 pagesFamily PlanningRendy BayhaqiPas encore d'évaluation
- Comparison Between Hygiene and SanitationDocument4 pagesComparison Between Hygiene and SanitationtibebuPas encore d'évaluation
- Ar ResumeDocument2 pagesAr Resumeapi-462238327Pas encore d'évaluation
- Wells Score For DVT ProbabilityDocument10 pagesWells Score For DVT ProbabilityrhomadianaPas encore d'évaluation
- COVID19 HandookDocument86 pagesCOVID19 HandookRagavPas encore d'évaluation
- Medical History Report Medical Prescreen QuestionnaireDocument4 pagesMedical History Report Medical Prescreen Questionnairejames antonioPas encore d'évaluation
- Advanced Physiotherapeutic SyllabusDocument1 pageAdvanced Physiotherapeutic SyllabusAnup SharmaPas encore d'évaluation
- BSNDocument1 pageBSNAnonymous 75TDy2yPas encore d'évaluation
- DWIHN Access To HealthcareDocument1 pageDWIHN Access To HealthcareWXYZ-TV Channel 7 DetroitPas encore d'évaluation
- Daftar PustakaDocument2 pagesDaftar PustakaAnonymous 65zjdAVPas encore d'évaluation
- Galvano-Spa-Bath and HealthDocument2 pagesGalvano-Spa-Bath and HealthDeu na telha com Janaína BensdorpPas encore d'évaluation
- Health 7: Learning More About Noncommunicable Diseases Written Report About CancerDocument2 pagesHealth 7: Learning More About Noncommunicable Diseases Written Report About CancerRafaella Feroza CastroPas encore d'évaluation
- Vacant Seats For Transfer - Admissions 2022Document4 pagesVacant Seats For Transfer - Admissions 2022Shahroz RindPas encore d'évaluation
- Systemic Inflammatory Response Syndrome (SIRS) PrognosisDocument16 pagesSystemic Inflammatory Response Syndrome (SIRS) PrognosisIPGDx100% (1)
- Group 4 - Accomplishment ReportDocument5 pagesGroup 4 - Accomplishment ReportMa. Millen PagadorPas encore d'évaluation
- Gnadia Pasandidega1Document2 pagesGnadia Pasandidega1Craig DavisPas encore d'évaluation