Académique Documents
Professionnel Documents
Culture Documents
Stenosis Nonsurgical - PMR Clinics
Transféré par
ialexflorinDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Stenosis Nonsurgical - PMR Clinics
Transféré par
ialexflorinDroits d'auteur :
Formats disponibles
Nonsurgical management of patients
with lumbar spinal stenosis: a literature
review and a case series of three patients
managed with physical therapy
Julie M. Whitman, PT, DSc
a,b,
*
,
Timothy W. Flynn, PT, PhD
b,c
,
Julie M. Fritz, PT, PhD
d
a
Wilford Hall Air Force Medical Center, 2200 Bergquist Drive, Suite 1,
Lackland Air Force Base, TX 78236-5300, USA
b
US Army-Baylor University Postprofessional Doctoral Program in Orthopaedic & Manual
Physical Therapy, Brooke Army Medical Center, 3851 Roger Brooke Drive,
Fort Sam Houston, TX 78234, USA
c
US Army-Baylor University Graduate Program in Physical Therapy,
Academy of Health Sciences, 3151 Scott Road, Fort Sam Houston, TX 78234-6138, USA
d
Department of Physical Therapy, University of Pittsburgh, 6035 Forbes Tower,
Pittsburgh, PA 15260, USA
Lumbar spinal stenosis (LSS) is a recognized source of signicant disabil-
ity among the elderly and a substantial expense to the health care system.
Patients with LSS may actually suer from greater physical burden than
those with many other signicant medical conditions, such as chronic ob-
structive pulmonary disease, systemic lupus erythematosus, and congestive
heart failure [1]. LSS is a prevalent condition, with an estimated 13% to
14% of those patients who seek help from a specialty physician and 3% to
4% who see a general practitioner for low back pain (LBP) diagnosed with
LSS [14]. From 1979 through 1992, data from the National Hospital Dis-
charge Survey revealed an eightfold increase in surgery for spinal stenosis
[2], and this disorder is noted as the most common diagnosis associated with
spinal surgery in patients over 65 years of age [57]. Over thirty thousand
The opinions and assertions contained herein are the private views of the authors and are
not to be construed as ocial or as reecting the views of the Department of Defense.
* Corresponding author. Physical Therapy Clinic, 377
th
Medical Group, Kirtland Air Force
Base, NM 87117-5524, USA.
E-mail address: Julie.Whitman@59mdw.whmc.af.mil or Julie92@swbell.net (J.M. Whitman).
1047-9651/03/$ see front matter 2003, Elsevier Science (USA). All rights reserved.
PII: S 1 0 4 7 - 9 6 5 1 ( 0 2 ) 0 0 0 7 6 - 1
Phys Med Rehabil Clin N Am
14 (2003) 77101
surgical procedures for LSS are performed annually with an inpatient
expense of almost one billion dollars [8,9]. Although the substantial societal
impact of LSS is apparent, there is uncertainty about the natural history of
the disorder and evidence for both nonsurgical and surgical management
remains unclear [2,5,7,10,11]. As the population continues to age, it will
become increasingly important to determine the appropriate strategies for
management of patients suering from this spinal disorder. The purpose
of this article is to briey review the clinical diagnosis and presentation of
LSS, review the status of the literature on nonsurgical management of the
condition, and to present three cases of patients managed with manual phys-
ical therapy.
LSS has been dened as a focal narrowing of the spinal canal, nerve root
canals, or intervertebral foramina [12,13]. Classication of the disorder may
be made based on the location of the narrowing, either in the central or lat-
eral canal, or on the etiology of the stenosis, either primary or secondary
[12,14]. Primary stenosis refers to various congenital etiologies whereas sec-
ondary or acquired stenosis is from degenerative, post surgical (iatrogenic),
spondylolisthetic, posttraumatic, or combined etiologies [12,15,16]. The
most frequently reported classication of LSS is that of degenerative etiol-
ogy, especially among the elderly [15,1720]. Although LSS is classied
according to the structural ndings from imaging studies, many researchers
report signicant radiographic LSS in asymptomatic individuals [2124],
and no consistent strong relationship has been identied between imaging
ndings and results of treatment [2,2527]. Thus, the magnitude of symp-
toms cannot be directly attributed to the severity of degenerative changes.
Researchers report that in addition to a xed structural component, LSS has
a dynamic or movement-associated component. Compressive forces (axial
loading) and spinal extension have been demonstrated to decrease the
cross-sectional area (CSA) of the central spinal canal and the neuroforamen,
whereas spinal exion and nonweight-bearing postures have been demon-
strated to increase CSAs [2834]. In addition, evidence suggests that the
structural and dynamic elements of stenosis may lead to increased epidural
pressures [35] or vascular congestion or insuciency [3639] in the spinal
region, thus contributing to the symptoms associated with LSS [40]. This
dynamic component helps to explain the typical clinical presentation of a
patient with LSS. Symptoms are increased when standing and walking due
to increased spinal extension and compressive loading, and are decreased
when sitting. Ultimately, the patients clinical presentation must corroborate
the imaging ndings before a diagnosis of lumbar spinal stenosis can be
made [2,41].
Clinical presentation
Factors from both the history and physical examinations are important
in the diagnosis of LSS. Patients diagnosed with degenerative LSS are typ-
78 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
ically over 50 years of age with an insidious onset of chronic, progressive
LBP, and more recent onset of lower extremity (LE) symptoms [7,15,
4043]. Many patients with LSS suer from neurogenic claudication, a com-
bination of pain, tension, and weakness that occurs with walking and is
relieved when sitting [7,40,42,44]. Neurological changes are reported in
20% to 50% of patients [7,41], but cauda equina syndrome is rare [7,16,26,
4547]. Patients with LSS frequently demonstrate lumbar spine motion
restrictions and experience pain with lumbar extension [15,35,41,48,49].
Activities requiring lumbar extension or weight bearing (such as walking,
standing, or going down stairs) typically increase symptoms associated with
LSS, whereas activities or positions involving decreased weight bearing
or lumbar exion (such as sitting, stooping or bending forward, lying down,
or leaning forward on a shopping cart or walker) ease symptoms [35,40,
42,48]. Diminished walking tolerance is considered to be one of the most sig-
nicant functional limitations associated with LSS with measures or reports
of walking tolerance often used as a functional outcome measure for these
patients with LSS [15,26,48,49].
Several researchers have quantied the value of examination ndings for
the diagnosis of LSS. Katz and colleagues [41] identied the absence of pain
while seated as a highly specic nding for the diagnosis of LSS (Specicity
[Sp] 0.93). In other words, a patient report of no pain with sitting is help-
ful to rule in the diagnosis of LSS. These researchers also report the ndings
of pain below the buttocks, age over 65, and no pain with exion as highly
sensitive for the diagnosis of LSS (Sensitivity [Sn] 0.88, Sn 0.77, and
Sn 0.79, respectively) [41]. Fritz et al [50] identied a patient ranking of
sitting as the best posture (Sn 0.89) and standing or walking as the worst
posture as highly sensitive (Sn 0.89). The absence of ranking sitting as the
best posture and standing or walking as the worst posture decreased the
likelihood of the patient having LSS (Negative Likelihood Ratios 0.28 and
0.33, respectively). Additionally, a two-stage treadmill test (TSTT) has been
suggested as a diagnostic tool in determining the presence of LSS [50]. The
TSTT is conducted by comparing the results of a patients walking tolerance
with a level and inclined (15%) bout of walking at a self-selected comfortable
pace. The best classication of those with LSS, as determined by a radiolog-
ical reference standard, occurred with the ndings of an earlier onset of
symptoms and prolonged recovery time with level treadmill walking
(Sp 0.947, Positive Likelihood Ratio [PLR] 14.51) [50]. As a single nd-
ing, the presence of a longer total walking time during inclined walking is
predictive of LSS (Sp 0.923, PLR6.49) [50].
Conservative management
Many researchers and reviewers suggest that patients with LSS undergo
a period of conservative therapy before considering surgical intervention
[2,16,5154]. Despite this frequent recommendation, however, the recent
79 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
report by the Agency for Healthcare Research and Quality [2] stated that
only 15 of the 147 surgical management trials they reviewed reported that the
patients received, and showed no improvement after, a course of conserva-
tive treatment. The actual amount of prior conservative treatment reported
in these 15 studies was as little as 2 weeks in duration [2]. These facts may
reect the paucity of evidence available on the natural history of LSS and
the clinical course of patients managed conservatively, and the limitations
in drawing conclusions from the studies currently available. Conservative
management strategies for LSS frequently include combinations of varied
types of interventions such as bed rest, medications, epidural steroid injec-
tions, acupuncture, physical agents, postural or ergonomic advice, corsets,
and exion-based exercise programs. Outcome measures used for both sur-
gical and nonsurgical studies are often not assessed by blinded individuals,
are not objective in nature, or are poorly dened. No studies exist that inves-
tigate the ecacy of a focused, noninvasive intervention program compared
with a control group using a large sample size, well-established outcome
measures, testers blinded to group assignment, and evaluation of long-term
outcomes.
Available evidence does demonstrate that the natural history of LSS does
not appear to be one of inevitable deterioration, and some patients with LSS
may improve over time. In a study on the natural history of patients with
LSS followed over a 4-year period, Johnsson et al [43] reported that 85% of
subjects demonstrated either improvement or no change in symptoms and
70% reported either increases or no change in walking tolerance with no
treatment administered.
Several studies have documented the outcomes of conservative treatment
regimens or compared surgical with nonsurgical approaches [15,26,51,55
61]. Only one study randomly assigned patients to either surgical or non-
surgical treatment groups. Amundsen and colleagues [26] reported long-term
outcomes for 18 subjects with moderate symptoms who were randomized
into the nonsurgical group and 50 subjects with mild to moderate symp-
tomatic LSS who were nonrandomly assigned to nonsurgical treatment.
Nonsurgical intervention included admission to an inpatient ward for 1
month, use of a hyperextension back brace, back school education, and
encouragement to walk and move as normally as possible. Subjects were
advised to wear the brace for 2 to 3 more months after discharge, start gen-
eral physical training and ambulation, and keep their backs slightly kypho-
tic. Stabilizing exercises were employed, but according to the authors, no
attempt was made to improve mobility of the spine. Outcomes were estab-
lished from a combination of the opinion of the nonblinded examining phy-
sician and the patients self-rating. The researchers reported good results
for 47% to 57% of all nonsurgically treated patients at 4 years. Although the
operational denitions for categorization of level of symptoms at baseline
and the exact method of classication into the overall treatment result
groups of excellent, fair, unchanged, or worse at the follow-up
80 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
assessments were unclear, the results of this study demonstrate that approx-
imately one half of patients with mild to moderate symptoms of LSS are
able to improve with a nonoperative course of treatment [26].
Researchers from the Maine Lumbar Spine Study provided outcome
information on 148 patients with LSS either conrmed by imaging or based
on a strong clinical suspicion of stenosis [51,55]. Subjects in this study were
not randomized into treatment groups and the patients selecting surgery
were worse both clinically and radiographically at baseline than those select-
ing conservative management. A total of 67 patients underwent combina-
tions of assorted nonsurgical treatments, including medications (narcotic
analgesics); epidural steroid injections; bed rest; bracing; and various forms
of exercise, manual medicine intervention, or physical modalities [51,55,56].
Well-established outcome measures were used, including pain ratings, qual-
ity of life assessment, functional status assessment (Roland Scale), and ques-
tions regarding patient satisfaction. At the 1-year follow-up, over 80% of the
nonsurgically treated patients pain did not worsen, and half of these
patients reported improvement. This status remained almost the same at 4
years, with over 70% of the nonsurgical group reporting that they were not
worse and one half of these patients reporting improvement. Additionally,
49% of the nonsurgical patients were satised to live the rest of their lives
at their current status. At the 4-year follow-up, 85.7% of the subjects with
moderate symptoms at baseline who were treated nonsurgically were the
same or better. Although this study indicates that many patients may re-
spond positively or at least remain stable over time, it is dicult to conclude
which particular types of nonsurgical interventions were most ecacious.
Several other studies with both surgical and nonsurgical arms also
support the premise that many patients with LSS may do well without sur-
gery. Hurri et al [57] provided 12-year data for 18 nonsurgically treated pa-
tients, one third of whomhad severe LSS. Improvement was demonstrated in
44% of the nonsurgical group and only 11% worsened. Additionally, both
Johnsson et al [58] and Mariconda et al [59] reported improvements in
small cohorts of patients who either refused surgery or had severe comorbid-
ities that were contraindications for surgery. The nonsurgical interventions
were not well dened in these studies.
Fukusaki et al [60] provided the only well-designed, randomized, con-
trolled trial that compared a conservative treatment with a placebo treat-
ment for patients with LSS. In this study, 53 patients were randomized to
one of three treatment groups (epidural saline, epidural anesthetics, or
epidural anesthetics and steroids). A blinded examiner measured walking
tolerance on a treadmill at 1 week, 1 month, and 3 months. All treatment
groups received relief of symptoms at the 1-week and 1-month testing ses-
sions, but no symptomatic relief remained at the 3-month follow-up session.
This study [60] demonstrated that a local anesthetic block could provide
temporary improvements in neurogenic claudication for patients with
LSS. Epidural steroids, however, did not oer any additional benet in the
81 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
short-term outcomes measured. Further discussion of injections or other
forms of invasive nonsurgical interventions are outside of the scope of the
present article.
Two large case series have reported the results of specic nonsurgical
treatment regimens for LSS. Onel and colleagues [15] prospectively eval-
uated the ecacy of an inpatient treatment program for 145 subjects suer-
ing from either central or lateral stenosis. Treatment included heating
modalities, daily exion and extension exercises, and administration of sal-
mon calcitonin. The 1-month outcome data demonstrated improvements in
lumbar exibility and reported walking tolerance. Ninety-ve percent of the
group demonstrated improvement in global clinical improvement scores,
which included measures of pain, spinal functional capacity, neurogenic
ndings, and neurogenic claudication distances; only two subjects were
referred for surgical intervention due to neurological deterioration. No
long-term outcomes were reported [15]. Simotas et al [61] retrospectively
evaluated the outcomes of a cohort of 49 patients with central LSS. In
the 3 years evaluated, conservative interventions included combinations of
bed rest, oral corticosteroids, corsets, acupuncture, manipulation, trans-
cutaneous electrical nerve stimulation, epidural steroid injections, and non-
steroidal anti-inammatory (NSAID) medications. Additionally, almost all
of the subjects received postural instruction, gentle lumbopelvic mobiliza-
tion, and exion-biased lumbar stabilization exercises. After 3 years, one
quarter of the subjects were signicantly better, almost one half noted at
least some degree of overall improvement, and approximately one third
reported improved walking tolerance. Nine patients (18%) ultimately opted
for surgery. Although the interventions evaluated by Simotas et al [61] were
too varied to establish the ecacy of any specic treatment, this study dem-
onstrated that many patients undergoing nonsurgical intervention do not
face inevitable deterioration, but often remain the same or experience posi-
tive long-term outcomes.
A few small case reports or studies on nonsurgical intervention for LSS
are available in the literature. Kirkaldy-Willis [62] reported on the use of spi-
nal manipulation for 11 patients with central stenosis. Subjects admitted to
the study had not responded to previous conservative measures and were
disabled by pain at the initiation of treatment. Although these patients had
an 11.5-year mean duration of symptoms, improvement was noted in six of
these patients and two were symptom free with no restrictions in work or
other activities after a course of manipulative intervention. Fritz et al [63]
reported on two subjects with LSS who received physical therapy interven-
tion for 6 weeks. The therapy included impairment-specic stretching and
strengthening and body weight supported ambulation. Both patients dem-
onstrated 70% to 100% improvements in pain and disability by discharge
that were maintained 1 month later [63]. DuPriest [64] demonstrated posi-
tive changes in pain and physical examination ndings for one patient with
LSS after 12 sessions of impairment-specic treatment. This patient sought
82 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
treatment after a previously unsuccessful 3-month course of other non-
surgical interventions (intramuscular corticosteroids injection, NSAIDs,
physical modalities, massage, and traction treatments). After undergoing
treatment including manipulation, specic stretching and strengthening
exercises, aerobic exercise (cycling and walking), ultrasound, and a heel lift,
the patient was able to return to daily 4-mile walks and no longer had pain.
These gains remained through the 3-month follow-up period. Rendeiro [65]
also described positive outcomes for a patient with LSS after implementa-
tion of a manual physical therapy program. Although denitive conclusions
on ecacy cannot be drawn from these reports due to small sample sizes,
short-term follow-up, and lack of control groups for comparison, they pro-
vide insight into possible outcomes after participation in noninvasive and
nonmedically oriented intervention programs.
In general, studies investigating the ecacy of nonsurgical intervention
for LSS or comparing nonsurgical versus surgical management for LSS
suer from methodological drawbacks similar to those experienced in
studies investigating surgical management for this disorder. The studies are
often observational in nature without randomization or comparison group,
utilize poorly dened management strategies and poor outcome measures, or
include small sample sizes. Therefore, aside from demonstrating that many
patients suering from LSS may improve or at least remain status quo over
time, a clinician can only derive limited conclusions from the literature to
assist with designing a specic nonsurgical management strategy for individ-
ual patients. In the absence of strong literature-based evidence, providers
must focus on signs and symptoms from the historical and physical exami-
nation to develop a plan of care. Further, the lack of evidence available
serves as an indication that clinical trials designed to determine the ecacy
of dierent types of nonsurgical intervention for patients suering from LSS
are indicated [2].
Case series
The purpose of this small case series is to describe a manual physical ther-
apy program and long-term outcomes for three patients with LSS. The
treating therapist utilized information from the historical and physical
examination to establish an individualized plan of care for the patients. The
treatment program addressed the impairments the treating therapist felt
most contributed to the patients low back and LE symptoms. Previous
studies have been criticized for not including data on dierent dimensions
of outcomes [7]. Therefore, we used a variety of measures to assess outcomes
from multiple dimensions of the Nagi disability model, including the impair-
ment level, the functional limitation level, and disability [63,66]. In addition
to reporting changes in historical and physical examination ndings and
functional limitations, patient reports of global rating of change (GRC), and
overall functional improvement, we included both region-specic and a
83 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
condition-specic self-report questionnaires and a patient report of walking
tolerance.
Instrumentation
The region-specic and condition-specic measures of disability used in
this case series were the Oswestry Disability Index (OSW) and a modied
Spinal Stenosis Scale (SSS), respectively. The OSW is a frequently used
region-specic disability scale for patients with LBP [67]. The OSW used
in this case series was the version studied by Fritz and Irrgang, with specic
questions modied to improve compliance [68]. In a study including 67
patients with acute work-related LBP, Fritz and Irrgang [68] found the
modied OSW to be reliable and responsive with a minimum clinically
important dierence (MCID) of 6 points over a 4-week period of time. The
SSS is a condition-specic self-report questionnaire for patients with LSS
[69,70]. This questionnaire consists of three scales addressing physical func-
tion status, patient satisfaction, and symptom severity. Each scale includes
ve to seven items scored on a Likert response scale, and each scale score
is calculated as the unweighted mean of all answered items. The range of
scores is from 1 to 5, 6, or 7, depending on the subscale, with lower scores
corresponding with less disability, greater satisfaction, or less pain. Our only
modication was to replace the word surgery with the word treatment
on the satisfaction scale of the SSS. In a large prospective observational
study of patients undergoing decompressive surgery for LSS, the dierence
in physical function and symptom severity scale scores between the unsatis-
ed and somewhat satised patients was 0.52 and 0.48, respectively. These
scores represent the MCID for each scale. Although the SSS questionnaire
has been found to be reliable, internally consistent, and more responsive than
was a region-specic measure in studies evaluating surgical outcomes for
patients with LSS [69], the psychometric properties of this modied SSS for
patients undergoing nonsurgical management are unknown.
We used a retrospective GRC as an additional outcome measure, because
no condition-specic measures have been validated for nonsurgically man-
aged patients with LSS. The retrospective GRC as an outcome gold stan-
dard represents a credible option in the absence of an external gold standard
and is a common, feasible, and useful method for assessing outcomes [71].
Jaeschke [71] has described a 15-point global self-rating scale whereby
patients may rate their own perception of improvement. The scale ranges
from 7 (a very great deal worse) to 0 (about the same) to +7 (a very
great deal better). Intermittent descriptors of worsening are assigned values
from 1 to 6, and intermittent descriptors of improvement are assigned
values from 1 to 6.
Many researchers recommend or use a treadmill test to objectively assess
walking tolerance after surgical and nonsurgical treatment [15,27,60,7276].
Because the TSTT, as described by Fritz et al [50], was found to have good
84 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
discriminative ability for patients with LSS, the test was used as a diagnostic
tool only in this case series. Unfortunately, we did not use any form of
treadmill testing to assess maximal walking time or distance either preinter-
vention or postintervention, and thus were only able to provide patient
reports of walking tolerance for these three patients.
Each patients overall functional status change was determined by com-
paring the individuals baseline with 18-month functional limitations. After
reviewing the baseline limitations (Table 1), the patient was asked to Esti-
mate the overall percentage dierence, if any, in your average ability to do
these activities and any other necessary daily activities today versus your
status when you rst came to physical therapy.
Patient description and historical examination ndings
The three subjects were retired military members who were treated in the
Physical Therapy Clinic at Brooke Army Medical Center, San Antonio,
Texas, and followed over an 18-month period. All patients reported LBP
and LE symptoms that were aggravated by standing upright and walking.
In all individuals, lower extremity pain was worse than the LBP and all
symptoms resolved with bending forward or sitting. Table 1 includes more
detailed historical examination ndings.
Patient 1
This 81-year-old male suered from worsening LBP and right LE symp-
toms extending to the posterior calf and plantar surface of the foot. The ini-
tial onset of symptoms started with a fall on to his back and buttocks 5 years
prior. The LBP was an intermittent, deep ache with intermittent, deep, sharp
pain in the right buttock. The right lower calf symptoms were intermittent
with a tired, achy quality. This patient had not exercised regularly since the
fall due to his LBP and LE symptoms and reported a very sedentary life-
style with at least 6 to 8 hours of sitting per day. Standard radiographs dem-
onstrated the following: multilevel degenerative disc disease with moderate
disc space narrowing in L4-5 and L5-S1; pars defect of the left L4 vertebral
body, Grade I anterior listhesis of L4 on L5; and transitional vertebra at
the lumbosacral junction. General health issues included aortic valve re-
placement 1 year prior, hypertension, coronary artery disease, angina (only
when mowing the lawn), shortness of breath with activity, 3-year history of
vertigo, skin cancer removed in 1950s (unsure what type, not recorded in
medical records), and positive smoking history (stopped in 1962).
Patient 2
This 63-year-old male had episodic, worsening LBP since a blow to the
back in high school football 45 years prior. The LBP was described as an
intermittent, deep, sharp pain. His intermittent LE numbness, tingling, and
pain extended along the lateral thigh, leg, and foot. LE symptoms began 8 to
10 years prior and had progressively increased in frequency and intensity.
85 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
T
a
b
l
e
1
H
i
s
t
o
r
i
c
a
l
e
x
a
m
i
n
a
t
i
o
n
n
d
i
n
g
s
P
a
t
i
e
n
t
1
P
a
t
i
e
n
t
2
P
a
t
i
e
n
t
3
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
F
u
n
c
t
i
o
n
a
l
l
i
m
i
t
a
t
i
o
n
s
S
t
a
n
d
i
n
g
u
p
r
i
g
h
t
:
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
i
m
m
e
d
i
a
t
e
l
y
;
m
u
s
t
l
e
a
n
f
o
r
w
a
r
d
P
a
i
n
f
r
e
e
S
t
a
n
d
i
n
g
u
p
r
i
g
h
t
i
m
m
e
d
i
a
t
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
l
e
a
n
f
o
r
w
a
r
d
P
a
i
n
f
r
e
e
S
t
a
n
d
s
2
3
m
i
n
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
S
t
a
n
d
4
5
m
i
n
r
i
g
h
t
L
B
P
G
o
d
o
w
n
s
t
a
i
r
s
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
i
m
m
e
d
i
a
t
e
l
y
P
a
i
n
f
r
e
e
U
p
o
r
d
o
w
n
s
t
a
i
r
s
i
m
m
e
d
i
a
t
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
P
a
i
n
f
r
e
e
W
a
l
k
s
4
m
i
n
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
P
a
i
n
f
r
e
e
T
r
a
n
s
i
t
i
o
n
s
i
n
t
o
/
o
u
t
o
f
c
a
r
,
t
o
/
f
r
o
m
s
u
p
i
n
e
/
s
i
t
t
i
n
g
/
s
t
a
n
d
i
n
g
L
B
P
P
a
i
n
f
r
e
e
L
y
i
n
g
o
n
r
i
g
h
t
s
i
d
e
i
m
m
e
d
i
a
t
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
r
o
l
l
t
o
l
e
f
t
s
i
d
e
P
a
i
n
f
r
e
e
L
y
i
n
g
p
r
o
n
e
i
m
m
e
d
i
a
t
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
P
a
i
n
f
r
e
e
V
a
c
u
u
m
o
n
e
r
o
o
m
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
s
i
t
P
a
i
n
f
r
e
e
S
t
a
n
d
i
n
g
s
t
a
t
i
o
n
a
r
y
5
1
0
m
i
n
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
l
e
a
n
f
o
r
w
a
r
d
o
r
s
i
t
S
t
a
n
d
s
1
0
1
5
m
i
n
L
B
P
,
l
e
f
t
L
E
s
y
m
p
t
o
m
s
t
o
l
e
g
/
f
o
o
t
L
y
i
n
g
s
u
p
i
n
e
i
m
m
e
d
i
a
t
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
P
a
i
n
f
r
e
e
M
o
w
l
a
w
n
>
1
0
m
i
n
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
s
i
t
o
r
b
e
n
d
f
o
r
w
a
r
d
P
a
i
n
f
r
e
e
f
o
r
1
0
m
i
n
,
c
a
n
m
o
w
w
h
o
l
e
l
a
w
n
W
a
t
e
r
l
a
w
n
w
i
t
h
h
o
s
e
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
s
t
o
p
i
m
m
e
d
i
a
t
e
l
y
P
a
i
n
f
r
e
e
(
l
a
s
t
t
i
m
e
h
e
c
o
u
l
d
d
o
t
h
i
s
w
a
s
3
y
e
a
r
s
p
r
i
o
r
t
o
i
n
i
t
i
a
l
v
i
s
i
t
)
86 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
W
a
l
k
>
5
m
i
n
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
s
i
t
o
r
b
e
n
d
f
o
r
w
a
r
d
O
v
e
r
1
m
i
l
e
b
e
f
o
r
e
s
t
o
p
s
d
u
e
t
o
f
a
t
i
g
u
e
W
a
l
k
i
n
g
t
h
r
e
e
b
l
o
c
k
s
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
b
e
n
d
f
o
r
w
a
r
d
o
r
s
i
t
A
l
m
o
s
t
u
n
l
i
m
i
t
e
d
,
w
a
l
k
s
o
v
e
r
8
b
l
o
c
k
s
(
a
p
p
r
o
x
3
0
m
i
n
)
b
e
f
o
r
e
L
B
P
,
l
e
f
t
L
E
s
y
m
p
t
o
m
s
D
o
e
s
d
i
s
h
e
s
L
B
P
a
n
d
r
i
g
h
t
L
E
s
y
m
p
t
o
m
s
;
m
u
s
t
s
i
t
P
a
i
n
f
r
e
e
,
u
n
l
i
m
i
t
e
d
2
4
h
o
u
r
p
a
t
t
e
r
n
W
a
k
e
s
>
5
t
i
m
e
s
p
e
r
n
i
g
h
t
,
e
a
s
e
s
i
m
m
e
d
i
a
t
e
l
y
w
i
t
h
p
o
s
i
t
i
o
n
c
h
a
n
g
e
S
l
e
e
p
s
w
e
l
l
W
a
k
e
s
2
3
t
i
m
e
s
p
e
r
n
i
g
h
t
,
e
a
s
e
s
i
m
m
e
d
i
a
t
e
l
y
w
i
t
h
p
o
s
i
t
i
o
n
c
h
a
n
g
e
S
l
e
e
p
s
w
e
l
l
S
t
i
b
a
c
k
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
r
s
t
5
1
0
m
i
n
i
n
t
h
e
m
o
r
n
i
n
g
S
t
i
b
a
c
k
f
o
r
1
0
m
i
n
i
n
t
h
e
m
o
r
n
i
n
g
E
x
e
r
c
i
s
e
r
o
u
t
i
n
e
N
o
n
e
f
o
r
5
y
e
a
r
s
d
u
e
t
o
L
B
P
a
n
d
L
E
s
y
m
p
t
o
m
s
N
o
t
d
o
i
n
g
e
x
e
r
c
i
s
e
s
d
u
e
t
o
l
a
z
i
n
e
s
s
N
o
n
e
f
o
r
7
8
y
e
a
r
s
d
u
e
t
o
L
E
s
y
m
p
t
o
m
s
C
y
c
l
e
s
1
0
2
0
m
i
n
/
d
;
d
o
e
s
s
p
e
c
i
c
e
x
e
r
c
i
s
e
s
4
7
d
a
y
s
p
e
r
w
e
e
k
W
a
l
k
e
d
3
m
i
l
e
s
d
a
i
l
y
u
n
t
i
l
o
n
s
e
t
o
f
L
B
P
a
n
d
l
e
f
t
L
E
s
y
m
p
t
o
m
s
.
S
t
o
p
p
e
d
e
x
e
r
c
i
s
i
n
g
d
u
e
t
o
p
a
i
n
W
a
l
k
s
T
I
W
,
2
m
i
l
e
s
p
e
r
s
e
s
s
i
o
n
G
e
n
e
r
a
l
a
c
t
i
v
i
t
y
S
i
t
s
m
i
n
i
m
u
m
6
8
h
r
s
p
e
r
d
a
y
,
v
e
r
y
s
e
d
e
n
t
a
r
y
V
e
r
y
a
c
t
i
v
e
N
o
t
a
c
t
i
v
e
,
s
e
d
e
n
t
a
r
y
V
e
r
y
a
c
t
i
v
e
V
e
r
y
a
c
t
i
v
e
u
n
t
i
l
o
n
s
e
t
o
f
s
y
m
p
t
o
m
s
,
n
o
w
v
e
r
y
s
e
d
e
n
t
a
r
y
V
e
r
y
a
c
t
i
v
e
A
b
b
r
e
v
i
a
t
i
o
n
s
:
L
B
P
,
l
o
w
b
a
c
k
p
a
i
n
;
L
E
,
l
o
w
e
r
e
x
t
r
e
m
i
t
y
.
87 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
This patients pain and disability from LSS caused him to retire from work 4
years prior and lumbar decompressive surgery was scheduled 1 year prior to
the initial physical therapy (PT) examination. The back surgery was can-
celled secondary to the patient needing a prostatectomy and the patient was
referred to PT for nonsurgical management of his LSS. The MRI report
from 1 year prior reported a congenitally small spinal canal with central
canal stenosis at L3-4 and L4-5; canal attening at L4-5; collapsed degener-
ative discs at L4-5, L5-S1; and mild right foraminal narrowing at L5-S1.
General health issues included a history of prostate cancer (removed 1 year
prior), hypertension, and allergies.
Patient 3
This 71-year-old male reported a history of worsening intermittent dull
ache in the left buttock and intermittent dull achy symptoms extending
along the lateral left thigh to the proximal one third of the lateral tibia.
These symptoms, of insidious onset 6 weeks prior, had caused this patient
to cease his daily walking program. This patients recent MRI report
included mild spinal canal stenosis at L2-3 and L5-S1 and severe spinal
canal stenosis from L3 through L5. General health issues included diabetes
mellitus type II, hypertension, and glaucoma.
Initial physical examination ndings
All three patients presented with the following impairments: (1) a exed
standing posture and decreased passive extension of the hips, (2) stiness of
the lower lumbar spine and the hips upon manual mobility testing, (3) tight-
ness in the iliopsoas and rectus femoris bilaterally, and (4) active range of
motion limitations with reproduction of lumbar and lower extremity symp-
toms (limited into extension, side bending to the side of LE symptoms, and
quadrant testing to the side of LE symptoms). Patients 2 and 3 tested pos-
itively on the TSTT. Patient 1 underwent a bicycle test to further dierenti-
ate between neurogenic and vascular claudication. Based on the patients
rate of perceived exertion, this individual worked harder on the bicycle test
and exercised twice as long on the bicycle than he had during the TSTT, yet
he complained of no LBP or LE pain while cycling. Lastly, all three patients
demonstrated reex and strength changes in the S1 distribution. Table 2
provides a detailed description of the physical examination ndings for each
patient at baseline and 18 months.
Physical therapy intervention
Each patient received ve sessions of impairment-specic manual physi-
cal therapy intervention. Treatment to the lumbar and lower thoracic spine
regions included both rotational and posterior to anterior mobilization or
manipulation techniques. Posterior to anterior accessory motion mobiliza-
tion techniques were used to address hip stiness and to try to increase hip
88 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
extension mobility. The therapist manually stretched the tight rectus femoris
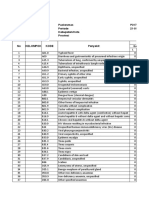
and iliopsoas muscles (see Fig. 1 [AF] for pictures of selected manual phys-
ical therapy techniques used to treat these three patients). After improve-
ment in spinal and hip mobility, gluteal muscle and lower abdominal
muscle strengthening was initiated. With each visit, the patient was
instructed in specic exercises designed to reinforce the physical therapy
interventions that were found to be ecacious in that patients care. The
exercises were continually adjusted until the individual patient felt stretch
or muscle activation in the targeted tissue region. Further sessions with the
therapist (ranging from one to four additional appointments) were used for
reinforcement of the home program. Lastly, all three patients were asked to
go on a daily intentional walk. The patients were instructed to stop walking
when symptoms reached the level that would normally make them stop.
Patients 2 and 3 participated in a progressive body-weight supported
treadmill ambulation training program. For this training, a cable and trunk
harness system is used to lift, or unload, a specied amount of body weight
from the patient while the patient walks on the treadmill. Body-weight sup-
port systems have been shown to decrease the downward excursion of the
bodys center of gravity [77] and predictably reduce the vertical component
of the ground reaction force with walking and with running [78]. Theoreti-
cally, this same body weight support system will decrease compression
forces usually placed on the lumbar spine with weight bearing, thus increas-
ing the cross-sectional area of the spinal canal and neuroforamen. Clinically,
it is our experience that many patients with LSS often tolerate walking with
a body-weight supported system for longer periods of time and with less
pain than without the support. Body-weight supported ambulation training
has been advocated for patients with LSS [63], other spinal conditions [79],
and various lower extremity disorders [8082]. For our patients with LSS,
enough body-weight support was used to alleviate LE symptoms and to
allow the patients to walk as normally as possible and as long as possible.
Naturally, the amount of support required uctuated from session to ses-
sion, but the overall goal was to gradually decrease the amount of unloading
used and gradually increase the walking pace and distance.
Orthotics were prescribed for patient 3 after the ecacy of the manual
intervention had been established. These were used to compensate for bio-
mechanical deciencies of the feet that the therapist determined adversely
aected lumbar spine and pelvic mechanics with gait. The foot and ankle
ndings included marked bilateral pes planus (right >left), bilateral na-
vicular drop of approximately 10 mm, no evidence of calcaneal inversion
bilaterally throughout gait, short stride length bilaterally, and an apropul-
sive gait. O-the-shelf orthotics were customized for this patient with 2
degrees medial posting on the left forefoot, left rearfoot, and right rearfoot;
and 4 degrees medial posting to the right forefoot. To determine whether the
orthotics would be benecial for this patient, the time to onset of neurogenic
claudication was measured during three successive trials of walking rst
89 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
T
a
b
l
e
2
P
h
y
s
i
c
a
l
e
x
a
m
i
n
a
t
i
o
n
n
d
i
n
g
s
P
a
t
i
e
n
t
1
P
a
t
i
e
n
t
2
P
a
t
i
e
n
t
3
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
1
8
m
o
n
t
h
s
P
o
s
t
u
r
e
M
a
r
k
e
d
l
y
e
x
e
d
a
t
h
i
p
s
,
L
x
s
p
i
n
e
,
a
n
d
T
x
s
p
i
n
e
U
p
r
i
g
h
t
M
a
r
k
e
d
l
y
e
x
e
d
h
i
p
s
,
L
x
s
p
i
n
e
;
e
x
t
e
n
d
e
d
T
L
j
u
n
c
t
i
o
n
E
x
t
e
n
d
e
d
a
t
t
h
e
T
L
j
u
n
c
t
i
o
n
S
l
i
g
h
t
l
y
e
x
e
d
a
t
h
i
p
s
a
n
d
L
x
s
p
i
n
e
;
s
l
i
g
h
t
r
i
g
h
t
l
a
t
s
h
i
f
t
N
o
r
m
a
l
L
i
m
i
t
e
d
s
t
a
n
d
i
n
g
R
O
M
L
x
e
x
t
,
r
i
g
h
t
S
B
,
r
i
g
h
t
q
u
a
d
r
a
n
t
m
a
r
k
e
d
a
l
l
w
i
t
h
L
B
P
a
n
d
L
E
s
y
m
p
t
o
m
s
L
x
e
x
t
,
r
i
g
h
t
L
x
q
u
a
d
r
a
n
t
m
i
n
L
B
P
o
n
l
y
B
i
l
a
t
S
B
m
a
r
k
e
d
L
B
P
;
L
x
e
x
t
a
n
d
l
e
f
t
q
u
a
d
r
a
n
t
m
a
r
k
e
d
L
B
P
a
n
d
L
E
s
y
m
p
t
o
m
s
L
x
e
x
t
a
n
d
l
e
f
t
q
u
a
d
r
a
n
t
m
i
n
L
B
P
L
x
e
x
t
,
l
e
f
t
S
B
,
a
n
d
l
e
f
t
L
x
q
u
a
d
r
a
n
t
m
a
r
k
e
d
L
B
P
a
n
d
L
E
s
y
m
p
t
o
m
s
E
x
t
w
i
t
h
o
v
e
r
p
r
e
s
s
u
r
e
b
i
l
a
t
b
u
t
t
o
c
k
s
t
i
g
h
t
S
t
i
n
e
s
s
w
i
t
h
s
e
g
m
e
n
t
a
l
m
o
b
i
l
i
t
y
t
e
s
t
i
n
g
M
a
r
k
e
d
S
t
r
i
g
h
t
L
4
,
L
5
;
m
o
d
L
1
L
3
S
t
;
m
o
d
l
o
w
e
r
T
x
s
p
i
n
e
M
o
d
r
i
g
h
t
L
5
M
a
r
k
e
d
S
t
L
4
,
L
5
;
m
o
d
L
1
L
3
S
t
;
m
o
d
l
o
w
e
r
T
x
s
p
i
n
e
M
o
d
S
t
L
4
,
L
5
M
a
r
k
e
d
S
t
r
i
g
h
t
a
n
d
c
e
n
t
r
a
l
L
5
;
m
i
n
S
t
L
4
M
i
n
S
t
r
i
g
h
t
L
5
S
t
i
n
e
s
s
w
i
t
h
P
A
h
i
p
j
o
i
n
t
a
c
c
e
s
s
o
r
y
m
o
b
i
l
i
t
y
t
e
s
t
i
n
g
B
i
l
a
t
m
a
r
k
e
d
B
i
l
a
t
m
o
d
B
i
l
a
t
m
a
r
k
e
d
R
i
g
h
t
m
i
n
B
i
l
a
t
m
a
r
k
e
d
L
e
f
t
m
o
d
I
l
i
o
p
s
o
a
s
t
i
g
h
t
n
e
s
s
B
i
l
a
t
m
a
r
k
e
d
R
i
g
h
t
m
i
n
B
i
l
a
t
m
a
r
k
e
d
B
i
l
a
t
(
r
i
g
h
t
>
l
e
f
t
)
m
o
d
B
i
l
a
t
m
a
r
k
e
d
N
o
r
m
a
l
R
e
c
t
u
s
f
e
m
o
r
i
s
t
i
g
h
t
n
e
s
s
B
i
l
a
t
m
a
r
k
e
d
B
i
l
a
t
m
o
d
B
i
l
a
t
m
i
n
N
o
r
m
a
l
B
i
l
a
t
m
a
r
k
e
d
B
i
l
a
t
m
o
d
D
i
c
u
l
t
y
a
c
t
i
v
a
t
i
n
g
l
o
w
e
r
a
b
d
o
m
i
n
a
l
s
D
i
c
u
l
t
s
u
s
t
a
i
n
i
n
g
c
o
n
t
r
a
c
t
i
o
n
I
n
c
r
e
a
s
e
d
c
o
n
s
i
s
t
e
n
c
y
,
b
u
t
s
t
i
l
l
d
i
c
u
l
t
D
i
c
u
l
t
y
s
u
s
t
a
i
n
i
n
g
c
o
n
t
r
a
c
t
i
o
n
D
i
c
u
l
t
y
s
u
s
t
a
i
n
i
n
g
c
o
n
t
r
a
c
t
i
o
n
D
i
c
u
l
t
y
s
u
s
t
a
i
n
i
n
g
c
o
n
t
r
a
c
t
i
o
n
N
o
r
m
a
l
90 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
M
u
s
c
l
e
w
e
a
k
n
e
s
s
B
i
l
a
t
g
l
u
t
e
u
s
m
e
d
i
u
s
a
n
d
m
a
x
i
m
u
s
N
o
r
m
a
l
B
i
l
a
t
g
l
u
t
e
u
s
m
e
d
i
u
s
a
n
d
m
a
x
i
m
u
s
N
o
r
m
a
l
B
i
l
a
t
g
l
u
t
e
u
s
m
e
d
i
u
s
a
n
d
m
a
x
i
m
u
s
N
o
r
m
a
l
S
t
r
a
i
g
h
t
l
e
g
r
a
i
s
e
R
i
g
h
t
7
0
,
L
B
P
a
n
d
L
E
s
y
m
p
t
o
m
s
,
i
n
c
r
e
a
s
e
s
w
i
t
h
d
o
r
s
i
e
x
i
o
n
R
i
g
h
t
7
5
,
H
S
p
u
l
l
o
n
l
y
,
n
o
c
h
a
n
g
e
w
i
t
h
d
o
r
s
i
e
x
i
o
n
L
e
f
t
6
0
,
L
B
P
,
a
n
k
l
e
D
F
i
n
c
r
e
a
s
e
s
L
B
P
;
r
i
g
h
t
7
0
,
p
o
s
t
t
h
i
g
h
t
i
g
h
t
n
e
s
s
,
n
o
c
h
a
n
g
e
w
i
t
h
d
o
r
s
i
e
x
i
o
n
B
i
l
a
t
8
0
,
m
i
n
p
r
o
x
p
o
s
t
t
h
i
g
h
t
i
g
h
t
n
e
s
s
,
n
o
c
h
a
n
g
e
w
i
t
h
d
o
r
s
i
e
x
i
o
n
L
e
f
t
5
2
;
r
i
g
h
t
6
8
;
b
o
t
h
w
i
t
h
p
o
s
t
t
h
i
g
h
s
y
m
p
t
o
m
s
,
b
o
t
h
i
n
c
r
e
a
s
e
s
w
i
t
h
d
o
r
s
i
e
x
i
o
n
B
i
l
a
t
7
5
,
b
o
t
h
w
i
t
h
p
r
o
x
p
o
s
t
i
p
s
i
l
a
t
t
h
i
g
h
s
y
m
p
t
o
m
s
,
b
o
t
h
i
n
c
r
e
a
s
e
w
i
t
h
d
o
r
s
i
e
x
i
o
n
N
e
u
r
o
l
o
g
i
c
a
l
n
d
i
n
g
s
R
i
g
h
t
A
J
1
,
R
i
g
h
t
P
F
w
e
a
k
n
e
s
s
N
o
c
h
a
n
g
e
N
o
r
m
a
l
e
x
c
e
p
t
b
i
l
a
t
a
b
s
e
n
t
A
J
,
b
i
l
a
t
P
F
w
e
a
k
n
e
s
s
,
s
e
n
s
a
t
i
o
n
t
o
t
h
e
l
e
f
t
l
a
t
e
r
a
l
f
o
o
t
N
o
c
h
a
n
g
e
N
o
r
m
a
l
e
x
c
e
p
t
:
l
e
f
t
a
n
k
l
e
e
v
e
r
s
i
o
n
4
/
5
,
b
o
t
h
P
F
w
e
a
k
n
e
s
s
(
l
>
r
)
,
b
i
l
a
t
a
b
s
e
n
t
A
J
,
a
b
s
e
n
t
l
e
f
t
K
J
,
r
i
g
h
t
K
J
1
N
o
c
h
a
n
g
e
e
x
c
e
p
t
f
u
r
t
h
e
r
s
t
r
e
n
g
t
h
w
i
t
h
l
e
f
t
a
n
k
l
e
P
F
O
n
l
y
p
o
s
i
t
i
v
e
o
r
r
e
m
a
r
k
a
b
l
e
n
d
i
n
g
s
n
o
t
e
d
h
e
r
e
.
A
b
b
r
e
v
i
a
t
i
o
n
s
:
A
J
,
a
n
k
l
e
j
e
r
k
r
e
e
x
;
A
R
O
M
,
a
c
t
i
v
e
r
a
n
g
e
o
f
m
o
t
i
o
n
;
B
i
l
a
t
,
b
i
l
a
t
e
r
a
l
;
d
e
g
,
d
e
g
r
e
e
s
;
D
F
,
d
o
r
s
i
e
x
i
o
n
;
,
l
i
m
i
t
e
d
o
r
d
e
c
r
e
a
s
e
d
;
e
x
t
,
e
x
t
e
n
s
i
o
n
;
e
x
,
e
x
i
o
n
;
g
l
u
t
,
g
l
u
t
e
u
s
;
H
S
,
h
a
m
s
t
r
i
n
g
s
;
L
x
,
l
u
m
b
a
r
;
L
x
q
u
a
d
r
a
n
t
,
c
o
m
b
i
n
e
d
m
o
t
i
o
n
i
n
c
l
u
d
i
n
g
e
x
t
e
n
s
i
o
n
a
n
d
i
p
s
i
l
a
t
e
r
a
l
s
i
d
e
-
b
e
n
d
i
n
g
a
n
d
r
o
t
a
t
i
o
n
;
m
a
x
,
m
a
x
i
m
u
s
;
m
e
d
,
m
e
d
i
u
s
;
m
i
n
,
m
i
n
i
m
a
l
;
m
o
d
,
m
o
d
e
r
a
t
e
;
P
A
,
p
o
s
t
t
o
a
n
t
e
r
i
o
r
;
P
F
,
p
l
a
n
t
a
r
e
x
i
o
n
/
p
l
a
n
t
a
r
e
x
o
r
;
p
o
s
t
,
p
o
s
t
e
r
i
o
r
;
p
r
o
x
,
p
r
o
x
i
m
a
l
;
R
F
,
r
e
c
t
u
s
f
e
m
o
r
i
s
;
S
B
,
s
i
d
e
b
e
n
d
i
n
g
;
S
L
R
,
s
t
r
a
i
g
h
t
l
e
g
r
a
i
s
e
;
S
t
,
s
t
i
/
s
t
i
n
e
s
s
;
T
L
,
t
h
o
r
a
c
o
-
l
u
m
b
a
r
;
T
x
,
t
h
o
r
a
c
i
c
;
t
i
g
h
t
,
t
i
g
h
t
n
e
s
s
.
91 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
Fig. 1. Selected physical therapy interventions. (A) Supine iliopsoas muscle stretch. (B) Prone
hip posterior to anterior mobilization. (C) Prone rectus femoris muscle stretch. (D) Lumbar
rotation mobilization/manipulation in neutral. (E) Caudal glide to the hip joint in exion. (F)
Unilateral posterior to anterior lumbar spine mobilization.
92 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
without the orthotics, then immediately with the orthotics, then again im-
mediately without the orthotics. The time to onset of LE symptoms was
equal with both trials of walking without the orthotics, and neurogenic
claudication was appreciably delayed with the orthotics (40% longer before
neurogenic claudication with orthotics). Table 3 provides a summary of the
physical therapy interventions used with each patient.
Outcomes
All three patients demonstrated substantial positive changes that were
sustained up to 18 months. Tables 1 and 2 include the outcome information
for the historical examination ndings, functional limitations for each
patient, and physical examination ndings. The results of each patients
region-specic and condition-specic outcome questionnaires are included
in Table 4. As a group, the patients OSW score improvement ranged from
Fig. 1 (continued)
93 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
66% to 95% of their baseline scores by discharge and 33% to 82% at 18
months. On the Physical Function Scale of the modied SSS, improvement
ranged from 1.0 to 2.6 points from baseline to discharge and 0.9 to 2.6 at 18
months. On the Symptom Severity Scale, improvement ranged from 0.76 to
1.85 by discharge and 0.14 to 1.29 at 18 months. Except for patient 2s 18-
month Symptom Severity Scale score, the magnitude of all of the improve-
ments in outcomes noted by our patients surpassed the MCIDs previously
established by Stucki et al [69] for the Spinal Stenosis Scale and by Fritz and
Irrgang [68] for the modied OSW. Further, all three patients reported
improvements in overall functional status. These results, in addition to the
patients responses on the GRC scale, are reported in Table 4. Finally,
Table 3
Summary of physical therapy interventions
Patient 1 Patient 2 Patient 3
Total no. visits
with therapist
9 10 9
Manual therapy
sessions included:
5 5 6
Spinal
manipulation
(rotational,
PA graded)
Spinal
manipulation
(rotational,
PA graded)
Spinal
manipulation
(rotational,
PA graded)
Hip joint
mobilization
(PA)
Hip joint
mobilization
(PA)
Hip joint
mobilization
(PA)
Hip exor
stretching
Hip exor
stretching
Hip exor
stretching
Body weight
supported
ambulation
Body weight
supported
ambulation
Body weight
supported
ambulation
Gluteal muscle
retraining
Gluteal and lower
abdominal
retraining
Visits focused on
correct performance
of home exercise
program:
Spinal mobility
exercises
Flexion and
rotational spinal
mobilization
exercises
Flexion and
rotational spinal
mobilization
exercises
Flexion and
rotational spinal
mobilization
exercises
Muscle stretching Hip exor muscle
stretching
Hip exor muscle
stretching
Hip exor muscle
stretching
Muscle retraining Gluteal and calf
muscle
retraining
Gluteal and calf
muscle retraining
Gluteal and lower
abdominal muscle
retraining
Aerobic exercise Daily walking Daily: alternate
walk and cycle
Daily walking
Abbreviation: PA, posterior to anterior.
94 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
T
a
b
l
e
4
O
u
t
c
o
m
e
s
P
a
t
i
e
n
t
1
P
a
t
i
e
n
t
2
P
a
t
i
e
n
t
3
B
a
s
e
l
i
n
e
I
n
t
e
r
i
m
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
D
i
s
c
h
a
r
g
e
1
8
m
o
n
t
h
s
B
a
s
e
l
i
n
e
D
i
s
c
h
a
r
g
e
1
8
m
o
n
t
h
s
M
o
d
i
e
d
O
s
w
e
s
t
r
y
3
4
4
w
e
e
k
s
1
0
a
6
a
6
0
2
0
a
4
0
a
4
8
2
a
1
8
a
M
o
d
i
e
d
S
S
S
:
p
h
y
s
i
c
a
l
f
u
n
c
t
i
o
n
s
c
a
l
e
2
.
6
b
3
m
o
n
t
h
s
1
.
6
a
1
.
2
a
2
.
4
1
.
4
a
1
.
5
a
3
.
6
1
a
1
a
M
o
d
i
e
d
S
S
S
:
s
y
m
p
t
o
m
s
e
v
e
r
i
t
y
s
c
a
l
e
2
.
7
1
b
3
m
o
n
t
h
s
1
.
8
6
a
1
.
5
7
a
3
.
1
4
1
.
8
6
a
3
2
.
8
6
2
.
1
a
1
.
5
7
a
M
o
d
i
e
d
S
S
S
:
s
a
t
i
s
f
a
c
t
i
o
n
s
c
a
l
e
N
/
A
3
m
o
n
t
h
s
1
1
N
/
A
1
1
.
6
7
N
/
A
1
1
P
a
t
i
e
n
t
g
l
o
b
a
l
r
a
t
i
n
g
o
f
c
h
a
n
g
e
N
/
A
N
/
A
A
g
r
e
a
t
d
e
a
l
b
e
t
t
e
r
N
/
A
N
/
A
A
v
e
r
y
g
r
e
a
t
d
e
a
l
b
e
t
t
e
r
N
/
A
N
/
A
A
g
r
e
a
t
d
e
a
l
b
e
t
t
e
r
P
a
t
i
e
n
t
a
s
s
e
s
s
m
e
n
t
o
f
o
v
e
r
a
l
l
f
u
n
c
t
i
o
n
a
l
s
t
a
t
u
s
v
e
r
s
u
s
b
a
s
e
l
i
n
e
e
x
a
m
i
n
a
t
i
o
n
N
/
A
N
/
A
A
p
p
r
o
x
i
m
a
t
e
l
y
9
5
%
N
/
A
N
/
A
A
l
m
o
s
t
1
0
0
%
i
m
p
r
o
v
e
m
e
n
t
N
/
A
N
/
A
A
l
m
o
s
t
1
0
0
%
i
m
p
r
o
v
e
m
e
n
t
N
o
d
i
s
c
h
a
r
g
e
O
s
w
e
s
t
r
y
D
i
s
a
b
i
l
i
t
y
I
n
d
e
x
(
O
S
W
)
o
r
m
o
d
i
e
d
S
p
i
n
a
l
S
t
e
n
o
s
i
s
S
c
a
l
e
(
S
S
S
)
d
a
t
a
w
e
r
e
c
o
l
l
e
c
t
e
d
f
o
r
p
a
t
i
e
n
t
1
,
t
h
u
s
t
h
e
a
v
a
i
l
a
b
l
e
i
n
t
e
r
i
m
s
c
o
r
e
s
a
r
e
r
e
p
o
r
t
e
d
a
b
o
v
e
.
a
D
e
n
o
t
e
s
a
c
h
a
n
g
e
s
c
o
r
e
t
h
e
m
i
n
i
m
a
l
c
l
i
n
i
c
a
l
l
y
i
m
p
o
r
t
a
n
t
d
i
e
r
e
n
c
e
(
p
r
e
v
i
o
u
s
l
y
e
s
t
a
b
l
i
s
h
e
d
b
y
S
t
u
c
k
i
e
t
a
l
[
6
9
]
f
o
r
p
o
s
t
s
u
r
g
i
c
a
l
p
a
t
i
e
n
t
s
f
o
r
t
h
e
S
S
S
,
a
n
d
b
y
F
r
i
t
z
a
n
d
I
r
r
g
a
n
g
[
6
8
]
f
o
r
t
h
e
M
o
d
i
e
d
O
s
w
e
s
t
r
y
D
i
s
a
b
i
l
i
t
y
I
n
d
e
x
)
.
b
D
e
n
o
t
e
s
t
h
a
t
d
a
t
a
w
e
r
e
c
o
l
l
e
c
t
e
d
r
e
t
r
o
s
p
e
c
t
i
v
e
l
y
.
95 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
although all three patients were taking pain medications for their lower back
and leg pain at the baseline evaluation, the patients reported only occasional
use of pain medication at the 18-month follow-up appointment.
Discussion
This case series is the rst to use a well-dened, impairment-based, non-
invasive outpatient treatment program for patients with LSS and to provide
patient-centered long-term outcome information. Most studies investigating
the ecacy of conservative interventions or comparing surgical with non-
surgical outcomes for patients with LSS combine invasive treatments, phar-
macological management, physical modalities, and nonspecic exercises
[15,51,55,61,83]. As previously discussed, the use of such unfocused manage-
ment strategies prevents further dierentiation of what aspect of care was
the most benecial for patients with LSS. Additionally, some researchers
have reported on outcomes after prolonged inpatient treatment programs
[15,26]. Although this situation allows for improved experimental control
with human subjects, it is our opinion that a prolonged period of nonsurgi-
cal inpatient care for patients with LSS is not practical in the United States
at this time. The outpatient treatment program we implemented focuses on
the patients individualized, prioritized impairments identied at the initial
examination. The treatments emphasized manual physical therapy tech-
niques targeting each patients prioritized impairments, specic exercises to
either reinforce the manual physical therapy treatment or strengthen specic
muscles, and a walking program. Under this physical therapy program, the
patients experienced signicant improvements, and the potential adverse
eects of invasive therapies or pharmacological management strategies often
included in other nonsurgical treatment programs were avoided.
The use of long-term patient-centered outcome measures that focused on
dierent levels of the disablement model was an asset of this case series.
Many previous reports on nonsurgical management of patients with LSS
only assessed short-term outcomes [15,6365], used combinations of clini-
cian opinion and patient-centered outcomes assessment [26], or did not
establish the patients baseline status before initiating intervention [84].
We examined changes over time at the impairment, functional limitation,
and disability levels of the disability model at baseline and up to 18 months
after initiation of physical therapy. Some areas for improvement in the out-
come assessment tools that were utilized have been identied, however.
Although the condition-specic SSS is a promising health outcome measure-
ment tool for those with LSS, the psychometric properties of the modied
SSS for those receiving nonsurgical intervention needs to be established.
Additionally, even though the SSS asks questions specically addressing the
patients walking tolerance, a more quantitative measure of this prevalent
functional limitation would be benecial. We suggest that future research
studies incorporate assessment of walking tolerance with a treadmill test
96 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
at baseline, at discharge, and at scheduled follow-up sessions. Lastly, our
method of quantifying the patients overall functional improvement could
possibly be improved by using the Patient Specic Functional Scale (PSFS)
[8587]. This is a patient-specic questionnaire that requires patients to
identify up to ve important activities that they are having diculty with
as a result of their condition. The patient rates diculty on an 11-point
numerical scale (0 unable to perform the activity; 10 able to perform
activity at the same level as before the injury or problem) and the average
score for up to ve activities is established as the PSFS score. This scale
has been established as reliable, valid, and responsive in other populations
[8587], but use with the LSS population has not been established.
This small case series demonstrates that patients with LSS can make sig-
nicant gains in disability, symptoms, and function in relatively short peri-
ods of time; and that these gains can be maintained up to 18 months.
Although the outcomes attained in this series seem promising, no cause and
eect relationship can be established from case reports. Additionally, the
treating therapist administered all questionnaires and assessments. Failure
to perform outcome assessments in a blinded fashion is a threat to the val-
idity of our ndings. Our intention, however, is for this small case series to
serve as a demonstration of the positive outcomes that are possible through
the use of a focused, impairment-specic manual physical therapy manage-
ment program. Additionally, it can provide insight into the types of out-
comes that may be benecial for assessing the progress of patients with
LSS. The authors are currently involved in a randomized clinical trial com-
paring two conservative management strategies and a randomized clinical
trial comparing conservative management and surgical management of LSS.
References
[1] Fanuele JC, Birkmeyer NJO, Abdu WA, et al. The impact of spinal problems on the health
status of patients: have we underestimated the eect? Spine 2000;25:150914.
[2] ECRI Health Technology Assessment Group. Treatment of degenerative lumbar spinal
stenosis. Evidence report/technology assessment no. 32 (Prepared by ECRI under Contract
No. 290-97-0020). Rockville, MD: Agency for Healthcare Research and Quality; June
2001. Publication #AHRQ01-E048.
[3] Hart LG, Deyo RA, Cherkin DC. Physician oce visits for low back pain. Frequency,
clinical evaluation, and treatment patterns from a US national survey. Spine 1995;1:
119.
[4] Long DM, BenDebba M, Torgerson WS, et al. Persistent back pain and sciatica in the
United States: patient characteristics. J Spinal Disord 1996;9:4058.
[5] Ciol MA, Deyo RA, Howell E, et al. An assessment of surgery for spinal stenosis: time
trends, geographic variations, complications and reoperations. J Am Geriatr Soc 1996;
44(3):28590.
[6] Taylor VM, Deyo RA, Cherkin DC, et al. Low back pain hospitalization: recent United
States trends and regional variations. Spine 1994;19:120713.
[7] Turner JA, Ersek M, Herron L, et al. Surgery for lumbar spinal stenosis. Attempted meta-
analysis of the literature. Spine 1992;17:18.
97 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
[8] Katz JN, Dalgas M, Stucki G, et al. Diagnosis of lumbar spinal stenosis. Rheum Dis Clin
North Am 1994;20:47183.
[9] Katz JN, Lipson SJ, Chang LC, et al. Seven- to 10-year outcome of decompressive surgery
for degenerative lumbar spinal stenosis. Spine 1996;21:928.
[10] Gibson JNA, Grant IC, Waddell G. The cochrane review of surgery for lumbar disc
prolapse and degenerative lumbar spondylosis. Spine 1999;24:182032.
[11] Waddell G, Gibson JNA. Scientic evidence on the management of lumbar spinal stenosis.
In: Gunzburg R, Szpalski M, editors. Lumbar spinal stenosis. Philadelphia: Lippincott,
Williams & Wilkins; 2000. p. 36771.
[12] Arnoldi CC, Brodsky AE, Cauchoix J, et al. Lumbar spinal stenosis and nerve root
entrapment syndromes. Denition and classication. Clin Orthop 1976;MarApr(115):45.
[13] Penning L. Functional pathology of lumbar spinal stenosis. Clin Biomech 1992;7:317.
[14] Postacchini F. Management of lumbar spinal stenosis. J Bone Joint Surg 1996;78:
15464.
[15] Onel D, Sari H, Donmez C. Lumbar spinal stenosis: clinical/radiologic therapeutic
evaluation in 145 patients. Conservative treatment or surgical intervention? Spine 1993;
18:2918.
[16] Spivak JM. Degenerative lumbar spinal stenosis. J Bone Joint Surg 1998;80:105366.
[17] Airaksinen O, Herno A, Turunen V, et al. Surgical outcome of 438 patients treated
surgically for lumbar spinal stenosis. Spine 1997;22:227882.
[18] Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al. Pathology and pathogenesis of
lumbar spondylosis and stenosis. Spine 1978;3:31928.
[19] Postacchini F, Gumina S, Cinotti G, et al. Ligamenta ava in lumbar disc herniation and
spinal stenosis. Spine 1994;19:91722.
[20] Rausching W. Normal and pathologic anatomy of the lumbar root canals. Spine 1987;
12:10109.
[21] Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic resonance scans of the lumbar
spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg 1990;72:
4038.
[22] Hitselberger WE, Witten RM. Abnormal myelograms in asymptomatic patients. J Neuro-
surg 1968;28:2046.
[23] Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of
the lumbar spine in people without back pain. N Engl J Med 1994;331:6973.
[24] Wiesel SW, Tsourmas N, Feer HL, et al. A study of computer-assisted tomography.
I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine 1984;9:
54951.
[25] Amundsen T, Weber H, Lilleas F, et al. Lumbar spinal stenosis. Clinical and radiologic
features. Spine 1995;20:117886.
[26] Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical
management? A prospective 10-year study. Spine 2000;25:142436.
[27] Herno A, Airaksinen O, Tapani S, et al. Computed tomography ndings 4 years after
surgical management of lumbar spinal stenosis. No correlation with clinical outcome. Spine
1999;24:22349.
[28] Infusa A, An HS, Lim TH, et al. Anatomic changes of the spinal canal and intervertebral
foramen associated with exion-extension movement. Spine 1996;21:241220.
[29] Liyang D, Yinkan X, Zhang W, et al. The eect of exion-extension motion of the lumbar
spine on the capacity of the spinal canal: an experimental study. Spine 1989;14:5235.
[30] Panjabi MM, Takata K, Goel VK. Kinematics of the lumbar intervertebral foramen. Spine
1983;3:34857.
[31] Penning L, Wilmink JT. Posture-dependent bilateral compression of L4 or L5 nerve root in
facet hypertrophy. A dynamic CT-myelographic study. Spine 1987;12:488500.
[32] Schonstrom N, Lindahl S, Willen J, et al. Dynamic changes in the dimensions of the
lumbar spinal canal: an experimental study in vitro. J Orthop Res 1989;7:11521.
98 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
[33] Sortland O, Magnaes B, Hauge T. Functional myelography with metrizamide in the
diagnosis of lumbar spinal stenosis. Acta Radiol Suppl 1977;355:4254.
[34] Willen J, Danielson B, Gaulitz A, et al. Dynamic eects on the lumbar spinal canal. Axially
loaded CT-myelography and MRI in patients with sciatica and/or neurogenic claudication.
Spine 1997;22:296876.
[35] Takahashi K, Miyazaki T, Takino T, et al. Epidural pressure measurements. Relationship
between epidural pressure and posture in patients with lumbar spinal stenosis. Spine
1995;20:6503.
[36] Baker AR, Collins TA, Porter RW, et al. Laser Doppler study of porcine cauda equina
blood ow: the eect of electrical stimulation of the rootlets during single and double site,
low pressure compression of the cauda equina. Spine 1995;20:6604.
[37] Iwamoto H, Matsuda H, Noriage A, et al. Lumbar spinal canal stenosis examined elec-
trophysiologically in a rat model for chronic cauda equina compression. Spine 1997;22:
263640.
[38] Jespersen SM, Hansen ES, Hoy K, et al. Two-level spinal stenosis in minipigs.
Hemodynamic eects of exercise. Spine 1995;20:276573.
[39] Watanabe R, Parke WW. Vascular and neural pathology of lumbosacral spinal stenosis.
J Neurosurg 1986;64:6470.
[40] Bridwell KH. Lumbar spinal stenosis. Diagnosis, management, and treatment. Clin Geriatr
Med 1994;10:677701.
[41] Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis. Diagnostic value
of the history and physical examination. Arthritis Rheum 1995;38:123641.
[42] Ciric E, Mikhael MA, Tarkington JA, et al. The lateral recess syndrome. J Neurosurg
1980;53:43343.
[43] Johnsson KE, Rosen I, Uden A. The natural course of lumbar spinal stenosis. Clin Orthop
Rel Res 1992;Jun(279):826.
[44] Verbiest H. Lumbar spinal stenosis: morphology, classication, long term results. In:
Weinstein J, Wiesel S, editors. The lumbar spine. Philadelphia: W.B. Saunders; 1990.
p. 54689.
[45] Johnsson KE. Lumbar spinal stenosis. A retrospective study of 163 cases in southern
Sweden. Acta Orthop Scand 1995;66:4035.
[46] Tuite GF, Doran SE, Stern JD, et al. Outcome after laminectomy for lumbar spinal
stenosis. Part II: radiographic changes and clinical correlations [see comments]. J Neurosurg
1994;81:70715.
[47] Tuite GF, Stern JD, Doran SE, et al. Outcome after laminectomy for lumbar spinal
stenosis. Part I: clinical correlations [published erratum appears in J Neurosurg 1995;82(5):
912]. J Neurosurg 1994;81:699706.
[48] Iversen MD, Katz JN. Examination ndings and self-reported walking capacity in patients
with lumbar spinal stenosis. Phys Ther 2001;81:1296306.
[49] Makan P, Fairbank JLT, Wanders L. Clinical assessment of lumbar spinal stenosis. J Bone
Joint Surg (Britain) 1998;80-B(Suppl II):158.
[50] Fritz JM, Erhard RE, Delitto A, et al. Preliminary results of the use of a two-stage
treadmill test as a clinical diagnostic tool in the dierential diagnosis of lumbar spinal
stenosis. J Spinal Disord 1997;10:4106.
[51] Atlas SJ, Keller RB, Robson D, et al. Surgical and nonsurgical management of lumbar
spinal stenosis: four-year outcomes from the Maine Lumbar Spine Study. Spine 2000;25:
55662.
[52] Fritz JM, Delitto A, Welch WC, et al. Lumbar spinal stenosis: a review of current concepts
in evaluation, management, and outcome measurements. Arch Phys Med Rehabil 1998;
79:7008.
[53] Jenis LG, An HS. Spine update. Lumbar foraminal stenosis. Spine 2000;25:38994.
[54] Nagler W, Hausen HS. Conservative management of lumbar spinal stenosis. Identifying
patients likely to do well without surgery. Postgrad Med 1998;103:6971.
99 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
[55] Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, part III. 1-year
outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine 1996;
21:178795.
[56] Keller RB, Atlas SG, Singer DE, et al. The Maine Lumbar Spine Study, I. Background and
concepts. Spine 1996;21:176976.
[57] Hurri H, Slatis P, Soini J, et al. Lumbar spinal stenosis: assessment of long-term out-
come 12 years after operative and conservative treatment. J Spinal Disord 1998;11:1105.
[58] Johnsson KE, Uden A, Rosen I. The eect of decompression on the natural course of
spinal stenosis. A comparison of surgically treated and untreated patients. Spine 1991;
16:6159.
[59] Mariconda M, Zanforlino G, Celestino GA, et al. Factors inuencing the outcome of
degenerative lumbar spinal stenosis. J Spinal Disord 2000;13:1317.
[60] Fukusaki M, Kobayashi I, Hara T, et al. Symptoms of spinal stenosis do not improve after
epidural steroid injection. Clin J Pain 1998;14:14851.
[61] Simotas AC, Dorey FJ, Hansraj KK, et al. Nonoperative treatment for lumbar spinal
stenosis. Clinical and outcome results and a 3-year survivorship analysis. Spine 2000;25:
197204.
[62] Kirkaldy-Willis WH. Manipulation. In: Kirkaldy-Willis W, editor. Managing low back
pain. New York: Churchill Livingstone; 1983. p. 17583.
[63] Fritz JM, Erhard RE, Vignovic M. A nonsurgical treatment approach for patients with
lumbar spinal stenosis. Phys Ther 1997;77:96273.
[64] DuPriest CM. Nonoperative management of lumbar spinal stenosis. J Manipulative
Physiol Ther 1993;16:4114.
[65] Rendeiro DG. Conservative management of lumbar spinal stenosisa case report. J Man-
ual Manipulative Ther 2000;8:139.
[66] Nagi SZ. Some conceptual issues in disability and rehabilitation. In: Sussman M, editor.
Sociology and rehabilitation. Washington, DC: American Sociological Association; 1965.
p. 10013.
[67] Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability
questionnaire. Physiotherapy 1980;66:2713.
[68] Fritz JM, Irrgang JJ. A comparison of a modied Oswestry Low Back Pain Disability
Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther 2001;81:77688.
[69] Stucki G, Daltroy L, Liang MH, et al. Measurement properties of a self-administered
outcome measure in lumbar spinal stenosis. Spine 1996;21:796803.
[70] Stucki G, Liang MH, Fossel AH, et al. Relative responsiveness of condition-specic and
generic health status measures in degenerative lumbar spinal stenosis. J Clin Epidemiol
1995;48:136978.
[71] Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the
minimally clinically important dierence. Control Clin Trials 1989;10:40715.
[72] Deen HG, Gordon MD, Zimmerman RS, et al. Test-retest reproducibility of the exercise
treadmill examination in lumbar spinal stenosis. Mayo Clin Proc 2000;75:10027.
[73] Deen HG, Zimmerman RS, Lyons MK, et al. Use of the exercise treadmill to measure
baseline functional status and surgical outcome in patients with severe lumbar spinal
stenosis. Spine 1998;23:2448.
[74] Deen HG, Zimmerman RS, Lyons MK, et al. Measurement of exercise tolerance on the
treadmill in patients with symptomatic lumbar spinal stenosis: a useful indicator of
functional status and surgical outcome. J Neurosurg 1995;83:2730.
[75] Herno A, Partanen K, Talaslahti T, et al. Long-term clinical and magnetic resonance
imaging follow-up assessment of patients with lumbar spinal stenosis after laminectomy.
Spine 1999;24:15337.
[76] Herno A, Saari T, Suomalainen O, et al. The degree of decompressive relief and its relation
to clinical outcome in patients undergoing surgery for lumbar spinal stenosis. Spine
1999;24:10104.
100 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
[77] Finch L, Barbeau H, Arsenault B. Inuence of body weight support on normal human.
Phys Ther 1991;71:84256.
[78] Flynn TW, Canavan PK, Cavanagh PR, et al. Plantar pressure reduction in an incremental
weight-bearing system. Phys Ther 1997;77:4106.
[79] Olsen J, Svendsen B. Medical exercise therapy: an adjunct to orthopaedic manual therapy.
Orthop Prac 1992;4:710.
[80] Hunter D, Cole EZ, Murray JM, et al. Energy expenditure of below-knee amputees during
harness-supported treadmill ambulation. J Orthop Sports Phys Ther 1995;21:26876.
[81] Kelsey DD, Tyson E. A new method of training for the lower extremity using unloading.
J Orthop Sports Phys Ther 1994;19:21823.
[82] Kline MK, Axen K, Haas F. Mechanical unweighting eects on treadmill exercise and pain
in elderly people with osteoarthritis of the knee. Phys Ther 1996;76:38794.
[83] Swezey RL. Outcomes for lumbar stenosis: a 5-year follow-up study. J Clin Rheumatol
1996;2:12934.
[84] Herno A, Airaksinen O, Saari T, et al. Lumbar spinal stenosis: a matched-pair study of
operated and non-operated patients. Br J Neurosurg 1996;10:4615.
[85] Chatman A, Neel J, Hyams S, et al. The Patient Specic Functional Scale: measurement
properties in patients with knee dysfunction. Phys Ther 1997;77:8209.
[86] Stratford PW, Gill C, Westaway M, et al. Assessing disability and change on individual
patients: a report of a patient specic measure. Physiother Can 1995;47:25863.
[87] Westaway M, Stratford PW, Binkley J. The Patient Specic Functional Scale: validation of
its use in persons with neck dysfunction. J Orthop Sports Phys Ther 1998;27:3318.
101 J.M. Whitman et al / Phys Med Rehabil Clin N Am 14 (2003) 77101
Vous aimerez peut-être aussi
- Exercise Physiology for the Pediatric and Congenital CardiologistD'EverandExercise Physiology for the Pediatric and Congenital CardiologistPas encore d'évaluation
- BMC Musculoskeletal DisordersDocument8 pagesBMC Musculoskeletal DisordersGabriela Corrales CerdeiraPas encore d'évaluation
- Sports Hernia and Athletic Pubalgia: Diagnosis and TreatmentD'EverandSports Hernia and Athletic Pubalgia: Diagnosis and TreatmentDavid R. DiduchPas encore d'évaluation
- Tennis Elbow JOSPT ArticleDocument11 pagesTennis Elbow JOSPT ArticleHasan RahmanPas encore d'évaluation
- Musculoskeletal Medicine in Primary Care: An Essential Guide for Examination, Diagnosis and ManagementD'EverandMusculoskeletal Medicine in Primary Care: An Essential Guide for Examination, Diagnosis and ManagementÉvaluation : 4 sur 5 étoiles4/5 (2)
- s00586 010 1543 2Document11 pagess00586 010 1543 2mohamed hazemPas encore d'évaluation
- Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsD'EverandPostural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsNicholas GallPas encore d'évaluation
- Ptc-63-166 Esclerosis Multiple TesrtDocument15 pagesPtc-63-166 Esclerosis Multiple TesrtIsrael BlancoPas encore d'évaluation
- The Effectiveness of Physiotherapy Exercises in Subacromial Impingement Syndrome: A Systematic Review and Meta-AnalysisDocument20 pagesThe Effectiveness of Physiotherapy Exercises in Subacromial Impingement Syndrome: A Systematic Review and Meta-AnalysisBruno FellipePas encore d'évaluation
- Mechanical or Inflammatory Low Back Pain PDFDocument7 pagesMechanical or Inflammatory Low Back Pain PDFHugo FalquetoPas encore d'évaluation
- AMBULATIONDocument12 pagesAMBULATIONDeborah SalinasPas encore d'évaluation
- Knee Osteoarthritis Patient 5Document8 pagesKnee Osteoarthritis Patient 5TanvirPas encore d'évaluation
- Objective. Design. Setting. Subjects. MethodsDocument2 pagesObjective. Design. Setting. Subjects. MethodsUmi RianaPas encore d'évaluation
- Spondilolistesis Klasifikasi MeyerdingDocument6 pagesSpondilolistesis Klasifikasi MeyerdingAriandindi AriandiPas encore d'évaluation
- Movement Detection Impaired in Patients With Knee Osteoarthritis Compared To Healthy Controls: A Cross-Sectional Case-Control StudyDocument10 pagesMovement Detection Impaired in Patients With Knee Osteoarthritis Compared To Healthy Controls: A Cross-Sectional Case-Control StudyDavid SugiartoPas encore d'évaluation
- Frozen Shoulder - Evidence and A Proposed Model Guiding RehabilitationDocument14 pagesFrozen Shoulder - Evidence and A Proposed Model Guiding RehabilitationMarlene RodriguezPas encore d'évaluation
- Anak Jurnal 11Document7 pagesAnak Jurnal 11Nurfitrianti ArfahPas encore d'évaluation
- 2015 Article 841Document6 pages2015 Article 841Anh ThưPas encore d'évaluation
- Clasificacion Degenerativa de EspondilolistesisDocument10 pagesClasificacion Degenerativa de EspondilolistesisCiro Madrid FloresPas encore d'évaluation
- Lower Back Pain Among Medical StudentsDocument5 pagesLower Back Pain Among Medical StudentsCharlie HigginsPas encore d'évaluation
- Subacromial Impingement Syndrome and Rotator Cuff Tendinopathy: The Dilemma of DiagnosisDocument4 pagesSubacromial Impingement Syndrome and Rotator Cuff Tendinopathy: The Dilemma of DiagnosisTomBramboPas encore d'évaluation
- Spinal Stenosis DiagnosisDocument10 pagesSpinal Stenosis DiagnosisDayuKurnia DewantiPas encore d'évaluation
- Alvin 2018 CervicalDocument7 pagesAlvin 2018 CervicalikhwanPas encore d'évaluation
- Severidad Oa RodillaDocument10 pagesSeveridad Oa RodillaFrancisco Vicent PachecoPas encore d'évaluation
- BiotekDocument12 pagesBiotekyenny handayani sihitePas encore d'évaluation
- Functional Thoracic Hyperkyphosis Model For Chronic Subacromial Impingement SyndromeDocument17 pagesFunctional Thoracic Hyperkyphosis Model For Chronic Subacromial Impingement SyndromeOriol Ruiz PujolPas encore d'évaluation
- Hamstring Length in Patellofemoral Pain Syndrome: Lisa C. White, Philippa Dolphin, John DixonDocument5 pagesHamstring Length in Patellofemoral Pain Syndrome: Lisa C. White, Philippa Dolphin, John DixonMamedPas encore d'évaluation
- Clinical ResearcheffectsDocument7 pagesClinical ResearcheffectsJackielyn C. AportaderaPas encore d'évaluation
- Laslett (2008) Clinical Perspective SI JointDocument11 pagesLaslett (2008) Clinical Perspective SI JointpaolofisioPas encore d'évaluation
- Study Material 4th Year - Research - Sumbul Ansari Et AlDocument10 pagesStudy Material 4th Year - Research - Sumbul Ansari Et AlAman hussainPas encore d'évaluation
- Correlation Between Severity of Spinal Stenosis and Multifidus Atrophy in Degenerative Lumbar Spinal StenosisDocument8 pagesCorrelation Between Severity of Spinal Stenosis and Multifidus Atrophy in Degenerative Lumbar Spinal StenosisIhsan KPas encore d'évaluation
- BMC Musculoskeletal DisordersDocument10 pagesBMC Musculoskeletal DisordersVizaPas encore d'évaluation
- Matsuwaka 2018Document9 pagesMatsuwaka 2018Dwi SahyatiPas encore d'évaluation
- The Effectiveness of Shoe Insoles For The Prevention and Treatment of Low BackDocument19 pagesThe Effectiveness of Shoe Insoles For The Prevention and Treatment of Low BackhasPas encore d'évaluation
- Normal Inter-Limb Differences During The Straight 2012Document9 pagesNormal Inter-Limb Differences During The Straight 2012Alejandro Javier Torres MorenoPas encore d'évaluation
- Seminario 7. Paciente Con Estenosis LumbarDocument9 pagesSeminario 7. Paciente Con Estenosis LumbarMarc SaenzPas encore d'évaluation
- Altered Cocontraction Patterns of Humeral Head Depressors in Patients With Subacromial Pain Syndrome: A Cross-Sectional Electromyography AnalysisDocument7 pagesAltered Cocontraction Patterns of Humeral Head Depressors in Patients With Subacromial Pain Syndrome: A Cross-Sectional Electromyography Analysis오현수Pas encore d'évaluation
- Kinesiology The Mechanics and Pathomechanics of Human Movement 3rd Edition Ebook PDFDocument62 pagesKinesiology The Mechanics and Pathomechanics of Human Movement 3rd Edition Ebook PDFbruce.glinski869100% (47)
- Fisioterapi Pada ICCUDocument10 pagesFisioterapi Pada ICCUZubaydatul UlumPas encore d'évaluation
- 10.1007@s10067 020 04988 7Document11 pages10.1007@s10067 020 04988 7NyLa LibertyPas encore d'évaluation
- Patellofemoral Pain: Jennifer E. Earl, PHD, Atc, Carole S. Vetter, MD, AtcDocument20 pagesPatellofemoral Pain: Jennifer E. Earl, PHD, Atc, Carole S. Vetter, MD, AtcGabriela Soto CoñuecarPas encore d'évaluation
- FFFGVDocument10 pagesFFFGVyundaPas encore d'évaluation
- Association of Lumbar Spine Radiographic Changes With Severity of Back Pain-Related Disability Among Middle-Aged, Community-Dwelling Women - PMCDocument17 pagesAssociation of Lumbar Spine Radiographic Changes With Severity of Back Pain-Related Disability Among Middle-Aged, Community-Dwelling Women - PMCSumanta KamilaPas encore d'évaluation
- DSA10 Scoliosis, Posture and Muscle BalanceDocument11 pagesDSA10 Scoliosis, Posture and Muscle BalanceWilliam JonesPas encore d'évaluation
- SpinDocument6 pagesSpinDaysdream JohnPas encore d'évaluation
- Conservative Management of A Young Adult With Hip ArthrosisDocument9 pagesConservative Management of A Young Adult With Hip ArthrosisKanika SinhaPas encore d'évaluation
- Ejercicio y Rehabilitación en Personas Con Esclerosis MultipleDocument43 pagesEjercicio y Rehabilitación en Personas Con Esclerosis MultipleEdher PliegoPas encore d'évaluation
- Minimally Invasive Decompression and Physiotherapy For Lumbar Spinal Stenosis in Geriatric PatientsDocument11 pagesMinimally Invasive Decompression and Physiotherapy For Lumbar Spinal Stenosis in Geriatric Patientsseptiani hasibuanPas encore d'évaluation
- Braly B y ColsDocument12 pagesBraly B y ColsmilelytaPas encore d'évaluation
- Treatment Options For Patellar Tendinopathy A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy A Systematic ReviewRonny Araya AbarcaPas encore d'évaluation
- Prevalencia Hernias 2022Document9 pagesPrevalencia Hernias 2022QuiroprácticaParaTodosPas encore d'évaluation
- Scapular Dyskinesis: From Basic Science To Ultimate TreatmentDocument17 pagesScapular Dyskinesis: From Basic Science To Ultimate TreatmentAlonso FernandezPas encore d'évaluation
- Treatment Options For Patellar Tendinopathy: A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy: A Systematic ReviewEstefa Roldan RoldanPas encore d'évaluation
- Clinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewDocument13 pagesClinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewHarshoi KrishannaPas encore d'évaluation
- March2011EditorsNoteDocument11 pagesMarch2011EditorsNoteCotta MüllerPas encore d'évaluation
- TheprevalenceofdepressionanditsrelevancetoclinicalDocument7 pagesTheprevalenceofdepressionanditsrelevancetoclinicalYasmin AbassPas encore d'évaluation
- Salsa Bili 487Document12 pagesSalsa Bili 487Monica ViverosPas encore d'évaluation
- Aspinall 2020Document22 pagesAspinall 2020Milton Ricardo de Medeiros FernandesPas encore d'évaluation
- A Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051Document8 pagesA Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051sebafigueroa94Pas encore d'évaluation
- Low Rate of Return To Impact Activity Following Core Decompression For Femoral Head AVN in Military ServicemembersDocument6 pagesLow Rate of Return To Impact Activity Following Core Decompression For Femoral Head AVN in Military ServicemembersJPPas encore d'évaluation
- Missing Pilot: A Dangerous JourneyDocument1 pageMissing Pilot: A Dangerous JourneyialexflorinPas encore d'évaluation
- The Miracle of Silk: Silk. The Word Itself Is Beautiful. The Story of Silk Starts inDocument1 pageThe Miracle of Silk: Silk. The Word Itself Is Beautiful. The Story of Silk Starts inialexflorinPas encore d'évaluation
- L1 U06 La RCDocument1 pageL1 U06 La RCialexflorinPas encore d'évaluation
- L1 U03 La RCDocument1 pageL1 U03 La RCialexflorinPas encore d'évaluation
- L1 U01 LB RCDocument1 pageL1 U01 LB RCialexflorinPas encore d'évaluation
- L1 U04 La RC PDFDocument1 pageL1 U04 La RC PDFialexflorinPas encore d'évaluation
- L1 U05 LB RC PDFDocument1 pageL1 U05 LB RC PDFialexflorinPas encore d'évaluation
- L1 U01 LA RC - PdfeqDocument1 pageL1 U01 LA RC - PdfeqialexflorinPas encore d'évaluation
- Olicy: Magna Carta of Public Health Workers: Does It Really Fulfill Its Intent?Document4 pagesOlicy: Magna Carta of Public Health Workers: Does It Really Fulfill Its Intent?Krystal Jane SalinasPas encore d'évaluation
- Health6q4Document80 pagesHealth6q4Pretpret Arcamo BanlutaPas encore d'évaluation
- Workcover Guides Evaluation Permanent Impairment 3rd Edition 0970Document104 pagesWorkcover Guides Evaluation Permanent Impairment 3rd Edition 0970workcovervictim8242Pas encore d'évaluation
- Internship 1 4Document75 pagesInternship 1 4Mariah Sharmane Juego Santos100% (2)
- Procedure Checklist Hot and Cold Application: Camarines Sur Polytechnic CollegesDocument2 pagesProcedure Checklist Hot and Cold Application: Camarines Sur Polytechnic CollegesElaine Frances IlloPas encore d'évaluation
- Community Medicine Term 1 QBankDocument9 pagesCommunity Medicine Term 1 QBankFaiza TasneemPas encore d'évaluation
- Peace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationDocument6 pagesPeace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationAccessible Journal Media: Peace Corps DocumentsPas encore d'évaluation
- Daftar List E-CatalogDocument24 pagesDaftar List E-CatalogPebriana Sonia SasiaPas encore d'évaluation
- Oral Exam NotesDocument3 pagesOral Exam NotesDrumz StaffPas encore d'évaluation
- Rev Plans For 20eb0110 - Provincial HospitalDocument20 pagesRev Plans For 20eb0110 - Provincial HospitalElvin AsanasPas encore d'évaluation
- The Differences in Diagnosis Between Western and Oriental MedicineDocument7 pagesThe Differences in Diagnosis Between Western and Oriental MedicineRene CardozoPas encore d'évaluation
- Medical Students Career Choice GuidelineDocument16 pagesMedical Students Career Choice Guidelineአማረ ተመስገንPas encore d'évaluation
- Trade/Generic Name Classification Action of Medication Dosage/Route/ Frequency Indications For Use (Patient Specific)Document16 pagesTrade/Generic Name Classification Action of Medication Dosage/Route/ Frequency Indications For Use (Patient Specific)lightzapPas encore d'évaluation
- Teaching Care Plan ExampleDocument3 pagesTeaching Care Plan ExampleAyaBasilioPas encore d'évaluation
- Case StudyDocument49 pagesCase StudyLennie Marie B Pelaez100% (1)
- Chokde Hudierez - Virtual Hospital Pharmacy Internship JournalDocument5 pagesChokde Hudierez - Virtual Hospital Pharmacy Internship JournalCHOKDE HUDIEREZPas encore d'évaluation
- Standard Claim Form HospitalDocument2 pagesStandard Claim Form Hospitalnpatel35Pas encore d'évaluation
- Gambaran Pelaksanaan Kegiatan Program Pengelolaan Penyakit Kronis (Prolanis) Bpjs Kesehatan Di Puskesmas Siak Hulu IIIDocument10 pagesGambaran Pelaksanaan Kegiatan Program Pengelolaan Penyakit Kronis (Prolanis) Bpjs Kesehatan Di Puskesmas Siak Hulu IIIDiky WahyuPas encore d'évaluation
- Barangay Sinabaan: Republic of The Philippines Province of PangasinanDocument2 pagesBarangay Sinabaan: Republic of The Philippines Province of PangasinanOmar DizonPas encore d'évaluation
- AMSTAR-2 ChecklistDocument10 pagesAMSTAR-2 ChecklistMuammar EmirPas encore d'évaluation
- Xavier BrochureDocument20 pagesXavier BrochureJohn PareraPas encore d'évaluation
- Bio Project File 2Document19 pagesBio Project File 2jiya singhPas encore d'évaluation
- Assessor Guidebook For Quality Assurance in Primary Health Centre PDFDocument220 pagesAssessor Guidebook For Quality Assurance in Primary Health Centre PDFDr Basant Kumar GuptaPas encore d'évaluation
- Obstetric Examination: 10/26/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 1Document44 pagesObstetric Examination: 10/26/2011 © Clinical Skills Resource Centre, University of Liverpool, UK 1Sangamesh SarjaPas encore d'évaluation
- Gyn - DelivaryDocument1 pageGyn - DelivaryRakshan Farm FreshPas encore d'évaluation
- Acute Ozone ExposureDocument2 pagesAcute Ozone ExposurevibhuPas encore d'évaluation
- SP PaperDocument10 pagesSP Paperapi-506783921Pas encore d'évaluation
- Laporan Bulanan Lb1: 0-7 HR Baru LDocument20 pagesLaporan Bulanan Lb1: 0-7 HR Baru LOla SarlinaPas encore d'évaluation
- 122512-Texto Do Artigo-229626-1-10-20161101 PDFDocument6 pages122512-Texto Do Artigo-229626-1-10-20161101 PDFGita TikihaiPas encore d'évaluation
- Guia de Productos PDFDocument32 pagesGuia de Productos PDFJulio Cesar Ramirez OlavePas encore d'évaluation
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (32)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4.5 sur 5 étoiles4.5/5 (82)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceD'EverandTo Explain the World: The Discovery of Modern ScienceÉvaluation : 3.5 sur 5 étoiles3.5/5 (51)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeD'EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeÉvaluation : 4.5 sur 5 étoiles4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesD'EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesÉvaluation : 4.5 sur 5 étoiles4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsD'EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsÉvaluation : 4.5 sur 5 étoiles4.5/5 (39)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (46)
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (60)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsD'EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsPas encore d'évaluation
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBID'EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIÉvaluation : 4 sur 5 étoiles4/5 (20)