Académique Documents
Professionnel Documents
Culture Documents
Acute Lymphoblastic Leukemia
Transféré par
mtyboy0 évaluation0% ont trouvé ce document utile (0 vote)
166 vues34 pagesEssay about acute lymphoblastic leukemia, including an overview, its description and possible treatments.
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentEssay about acute lymphoblastic leukemia, including an overview, its description and possible treatments.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
166 vues34 pagesAcute Lymphoblastic Leukemia
Transféré par
mtyboyEssay about acute lymphoblastic leukemia, including an overview, its description and possible treatments.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 34
Acute Lymphoblastic Leukemia
Author: Karen Seiter, MD; Chief Editor: Emmanuel C Besa, MD more...
Updated: Jan 16, 2013
Practice Essentials
Signs and symptoms
Signs and symptoms of acute lymphoblastic leukemia (ALL) include the following:
Fever
Decreased neutrophil count
Signs and symptoms of anemia, such as pallor, fatigue, dizziness, palpitations, cardiac flow
murmur, and dyspnea with even mild exertion
Bleeding (eg, from thrombocytopenia due to marrow replacement)
Disseminated intravascular coagulation (DIC) at diagnosis (about 10% of cases)
Palpable lymphadenopathy
Symptoms related to a large mediastinal mass (eg, shortness of breath), particularly with T-cell
ALL
Bone pain (severe and often atypical)
Left upper quadrant fullness and early satiety due to splenomegaly (about 10-20% of cases)
Symptoms of leukostasis, such as respiratory distress and altered mental status
Renal failure in patients with a high tumor burden Next Section: Physical Examination
Fever and other signs of infection, including pneumonia
Petechiae (particularly on lower extremities) and ecchymoses
Signs relating to organ infiltration with leukemic cells and lymphadenopathy
Rashes from skin infiltration with leukemic cells
See Clinical Presentation for more detail.
Diagnosis
Laboratory tests and other studies used in the workup for ALL include the following:
Complete blood count with differential
Coagulation studies
Peripheral blood smear
Chemistry profile, including lactic dehydrogenase, uric acid, liver function, and BUN/creatinine
Appropriate cultures (in particular, blood cultures) in the presence of fever or other signs of
infectionPrevious
Chest x-ray
Computed tomographyPrevious
Multiple-gated acquisition scanning
Electrocardiography
Bone marrow aspiration and biopsy (definitive for confirming leukemia)
Immunohistochemistry
Flow cytometry
Cytogenetics
Polymerase chain reaction
Gene expression profiling
See Workup for more detail.
Management
Treatment of ALL may include the following:
Induction chemotherapy (eg, standard 4- or 5-drug regimen, ALL-2, or hyper-CVAD)
Consolidation chemotherapy
Maintenance chemotherapy
Intrathecal chemotherapy for central nervous system (CNS) prophylaxis
Supportive care (blood products, antibiotics, and growth factors)
Special considerations apply to the treatment of mature B-cell ALL, Philadelphia
chromosomepositive (Ph+) ALL, ALL in older children and younger adults, relapsed ALL, and
ALL in patients with hyperuricemia or at high risk for tumor lysis syndrome.
Patients with Ph+ ALL, who have developed resistance to other therapies, can now be
treated with the newly approved drug ponatinib. Approval was based on the PACE trial
involving 449 patients with CML or Ph+ ALL. Study results showed 34% of patients with
blast-phase CML/Ph+ ALL achieved a normal white blood cell count within 6 months of
treatment with the drug.
[1]
See Treatment and Medication for more detail.
Image library
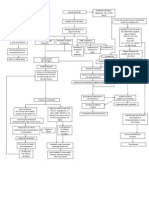
Diagnostic workup of a patient with preB-cell acute lymphoblastic
leukemia. Bone marrow aspiration revealed French-American-British L2 morphology.
Background
Acute lymphoblastic leukemia (ALL) is a malignant (clonal) disease of the bone marrow in
which early lymphoid precursors proliferate and replace the normal hematopoietic cells of the
marrow. ALL may be distinguished from other malignant lymphoid disorders by the
immunophenotype of the cells, which is similar to B- or T-precursor cells. Immunochemistry,
cytochemistry, and cytogenetic markers may also aid in categorizing the malignant lymphoid
clone.
The image below shows preB-cell ALL.
Diagnostic workup of a patient with preB-cell acute lymphoblastic
leukemia. Bone marrow aspiration revealed French-American-British L2 morphology.
See also Pediatric Acute Lymphoblastic Leukemia and Acute Myelogenous Leukemia.
Pathophysiology
The malignant cells of acute lymphoblastic leukemia (ALL) are lymphoid precursor cells (ie,
lymphoblasts) that are arrested in an early stage of development. This arrest is caused by an
abnormal expression of genes, often as a result of chromosomal translocations. The lymphoblasts
replace the normal marrow elements, resulting in a marked decrease in the production of normal
blood cells. Consequently, anemia, thrombocytopenia, and neutropenia occur to varying degrees.
The lymphoblasts also proliferate in organs other than the marrow, particularly the liver, spleen,
and lymph nodes.
Etiology
Less is known about the etiology of acute lymphoblastic leukemia (ALL) in adults compared
with acute myelogenous leukemia (AML). Most adults with ALL have no identifiable risk
factors.
Although most leukemias occurring after exposure to radiation are AML rather than ALL, an
increased prevalence of ALL was noted in survivors of the Hiroshima atomic bomb but not in
those who survived the Nagasaki atomic bomb.
Rare patients have an antecedent hematologic disorder (AHD) such as myelodysplastic
syndrome (MDS) that evolves to ALL. However, most patients with MDS that evolves to acute
leukemia develop AML rather than ALL.
Increasingly, cases of ALL with abnormalities of chromosome band 11q23 following treatment
with topoisomerase II inhibitors for another malignancy have been described. However, most
patients who develop secondary acute leukemia after chemotherapy for another cancer develop
AML rather than ALL.
Epidemiology
Acute lymphoblastic leukemia (ALL) is the most common type of cancer and leukemia in
children in the United States. In adults, this disease is less common than acute myelogenous
leukemia (AML). Approximately 1000 new cases of ALL occur in adults each year. However,
due to the fact that there are more adults than children, the number of cases seen in adults is
comparable to that seen in children.
Worldwide, the highest incidence of ALL occurs in Italy, the United States, Switzerland, and
Costa Rica, and this disease is slightly more common in men than in women.
Prognosis
Only 20-40% of adults with acute lymphoblastic leukemia (ALL) are cured with current
treatment regimens.
Patients with acute lymphoblastic leukemia (ALL) are divided into 3 prognostic groups: good
risk, intermediate risk, and poor risk.
Good risk includes the following:
No adverse cytogenetics
Age younger than 30 years
White blood cell (WBC) count of less than 30,000/L
Complete remission within 4 weeks
Intermediate risk includes those whose condition does not meet the criteria for either good risk or
poor risk.
Poor risk includes the following:
Adverse cytogenetics [(t9;22), (4;11)]
Age older than 60 years
Precursor B-cell WBCs with WBC count greater than 100,000/L
Failure to achieve complete remission within 4 weeks
Patients with precursor B-cell ALL have an extremely poor prognosis. Essentially, following
standard chemotherapy or autologous transplantation, long-term survival is not achieved. Several
reports have indicated that some patients with precursor B-cell ALL and t(4;11) may have
prolonged survival following allogeneic transplantation; therefore, this is the treatment of choice.
Immunophenotype effects on prognosis
Czuczman et al studied 259 patients treated with several Cancer and Leukemia Group B
(CALGB) protocols for newly diagnosed acute lymphoblastic leukemia (ALL) and found no
significant difference in response rates, remission duration, or survival for patients expressing
myeloid antigens versus those not expressing myeloid antigens.
[2]
B-lineage phenotype was
expressed in 79% of patients; one third of these coexpressed myeloid antigens. Seventeen
percent of patients demonstrated T-lineage ALL; one quarter of these coexpressed myeloid
antigens.
[2]
T-lineage ALL was associated with younger age, male sex, presence of a mediastinal mass,
higher WBC count and hemoglobin level, longer survival, and longer disease-free survival. The
number of T markers expressed also had prognostic significance. Patients expressing 6 or more
markers had longer disease-free and overall survival compared with patients expressing 3 or
fewer markers.
In a report by Preti et al, 64 of 162 patients with newly diagnosed ALL coexpressed myeloid
markers.
[3]
Patients coexpressing myeloid markers were significantly older, had a higher
prevalence of CD34 expression, and had a lower prevalence of common ALL antigen expression
than patients without myeloid expression. A trend toward a decreased remission rate was
observed for patients coexpressing myeloid markers (64%) relative to those who did not
coexpress such markers (78%).
[3]
However, no significant effect on remission duration or overall
survival was observed.
Chromosome number and prognosis
The effect of chromosome number on prognosis is displayed in Table 1, below.
Table 1. Effect of Chromosome Number on Prognosis (Open Table in a new window)
Chromosome Number 3-Year Event-Free Survival
Near tetraploidy 46-56%
Normal karyotype 34-44%
Hyperdiploidy >50 32-59%
Hyperdiploidy 47-50 21-53%
Pseudodiploidy 12-25%
Hypodiploidy 11%
Complications and prognosis
The most common complication is failure of the leukemia to respond to chemotherapy. These
patients do poorly, because they usually do not respond to other chemotherapy regimens.
Death in those with ALL may occur as a result of uncontrolled infection or hemorrhage. This
may occur even after the use of appropriate blood product and antibiotic support.
Patient Education
Patients with acute lymphoblastic leukemia (ALL) should be instructed to immediately seek
medical attention if they are febrile or have signs of bleeding. Furthermore, while receiving
chemotherapy, patients with leukemia should avoid exposure to crowds and people with
contagious illnesses, especially children with viral infections.
Although activity may occur as tolerated, patients with ALL may not participate in strenuous
activities such as lifting or exercise. In addition, a neutropenic diet is recommended in these
individuals, as follows:
No fresh fruits or vegetables may be eaten.
All foods must be cooked.
Meats are to be cooked until well done.
For patient education information, see Blood and Lymphatic System Center and Cancer and
Tumors Center, as well as Leukemia.
Proceed to Clinical Presentation
History
Patients with acute lymphoblastic leukemia (ALL) present with either symptoms relating to
direct infiltration of the marrow or other organs by leukemic cells or symptoms relating to the
decreased production of normal marrow elements.
Fever is one of the most common symptoms of ALL, and patients with ALL often have fever
without any other evidence of infection. However, in these patients, one must assume that all
fevers are from infections until proven otherwise, because a failure to treat infections promptly
and aggressively can be fatal. Infections are still the most common cause of death in patients
undergoing treatment for ALL.
Patients with ALL often have decreased neutrophil counts, regardless of whether their total white
blood cell (WBC) count is low, normal, or elevated. As a result, these individuals are at an
increased risk of infection. The prevalence and severity of infections are inversely correlated
with the absolute neutrophil count (ANC), which is defined as the number of mature neutrophils
plus bands per unit of volume. Infections are common when the absolute neutrophil count is less
than 500/L, and they are especially severe when it is less than 100/L. See the Absolute
Neutrophil Count calculator.
Symptoms of anemia are common and include fatigue, dizziness, palpitations, and dyspnea upon
even mild exertion. Other patients present with signs of bleeding. Bleeding can be the result of
thrombocytopenia due to marrow replacement. Additionally, approximately 10% of patients with
ALL have disseminated intravascular coagulation (DIC) at the time of diagnosis. These patients
may present with hemorrhagic or thrombotic complications.
Some patients present with palpable lymphadenopathy. Others, particularly those with T-cell
ALL, present with symptoms related to a large mediastinal mass, such as shortness of breath.
Infiltration of the marrow by massive numbers of leukemic cells frequently manifests as bone
pain. This pain can be severe and is often atypical in distribution.
About 10-20% of ALL patients may present with left upper quadrant fullness and early satiety
due to splenomegaly.
Although patients may present with symptoms of leukostasis (eg, respiratory distress, altered
mental status) because of the presence of large numbers of lymphoblasts in the peripheral
circulation, leukostasis is much less common in people with ALL than those with acute
myelogenous leukemia (AML), and it occurs only in patients with the highest WBC counts (ie,
several hundred thousand per L).
Patients with a high tumor burden, particularly those with severe hyperuricemia, can present in
renal failure.
Physical Examination
Patients with acute lymphoblastic leukemia (ALL) commonly have physical signs of anemia,
including pallor and a cardiac flow murmur. Fever and other signs of infection, including lung
findings of pneumonia, can also occur. Fever should be interpreted as evidence of infection, even
in the absence of other signs.
Patients with thrombocytopenia usually demonstrate petechiae, particularly on the lower
extremities. A large number of ecchymoses is usually an indicator of a coexistent coagulation
disorder such as disseminated intravascular coagulation (DIC).
Signs relating to organ infiltration with leukemic cells and, to a lesser degree, lymphadenopathy
may be present.
Occasionally, patients have rashes that result from infiltration of the skin with leukemic cells.
Proceed to Differential Diagnoses
Diagnostic Considerations
As noted earlier, patients with acute lymphoblastic leukemia (ALL) may present with fever
without any other evidence of infection. In these patients, all fevers must be assumed to be due to
infections until proven otherwise. Failure to treat infections promptly and aggressively can be
fatal; infections are still the most common cause of death in patients undergoing treatment for
ALL.
Other conditions that should be considered in the evaluation of suspected acute lymphoblastic
leukemia (ALL) include acute biphenotypic leukemia and natural killer (NK)-cell leukemia.
Differential Diagnoses
Acute Myelogenous Leukemia
Lymphoma, B-Cell
Lymphoma, High-Grade Malignant Immunoblastic
Lymphoma, Mantle Cell
Lymphoma, Non-Hodgkin
Proceed to Workup
Approach Considerations
Patients with acute lymphoblastic leukemia (ALL) may have direct infiltration of the marrow or
other organs by leukemic cells or have decreased production of normal marrow elements. These
can result in decreased neutrophil counts, regardless of whether their total white blood cell
(WBC) count is low, normal, or elevated. The prevalence and severity of infections are inversely
correlated with the absolute neutrophil count (ANC); infections are common when the absolute
neutrophil count is less than 500/L, and they are especially severe when it is less than 100/L.
See the Absolute Neutrophil Count calculator.
Patients also commonly present with anemia, and others present with signs of bleeding, which
can be the result of thrombocytopenia due to marrow replacement. Additionally, approximately
10% of patients with ALL have disseminated intravascular coagulation (DIC).
Leukostasis is another possible presentation due to the presence of large numbers of
lymphoblasts in the peripheral circulation, although this condition is much less common in
people with ALL than those with acute myelogenous leukemia (AML). Leukocytosis occurs only
in patients with the highest white blood cell (WBC) counts (ie, several hundred thousand per
L).
Patients with a high tumor burden, particularly those with severe hyperuricemia, can present in
renal failure.
Routine Laboratory Studies
A complete blood cell (CBC) count with differential demonstrates anemia and thrombocytopenia
to varying degrees in individuals with acute lymphoblastic leukemia (ALL). Patients with ALL
can have a high, normal, or low white blood cell (WBC) count, but they usually exhibit
neutropenia.
Coagulation studies and chemistry profiles
Abnormalities in the prothrombin time (PT) / activated partial thromboplastin time (aPTT) /
fibrinogen / fibrin degradation products may suggest concomitant disseminated intravascular
coagulation (DIC), which results in an elevated PT, decreased fibrinogen levels, and the presence
of fibrin split products.
A review of the peripheral blood smear confirms the findings of the CBC count. Circulating
blasts are usually seen. Schistocytes are sometimes seen if DIC is present.
A chemistry profile is recommended. Most patients with ALL have an elevated lactic
dehydrogenase level (LDH), and they frequently have an elevated uric acid level. In addition,
liver function tests and blood urea nitrogen (BUN)/creatinine determinations are necessary
before the initiation of therapy.
Cultures
Appropriate cultures, in particular blood cultures, should be obtained in patients with fever or
with other signs of infection without fever.
Radiologic Studies
Chest x-ray films may reveal signs of pneumonia and/or a prominent mediastinal mass in some
cases of T-cell acute lymphoblastic leukemia (ALL).
Computed tomography (CT) scans can further define the degree of lymphadenopathy in some
patients, including those with mediastinal masses.
MUGA Scanning and Electrocardiography
Multiple-gated acquisition (MUGA) scans or electrocardiographs (ECGs) are needed when the
diagnosis of acute lymphoblastic leukemia (ALL) is confirmed, because many chemotherapeutic
agents used in the treatment of acute leukemia are cardiotoxic.
An ECG is recommended before the initiation of treatment.
Bone Marrow Aspiration and Biopsy
Bone marrow aspiration and biopsy are the definitive diagnostic tests to confirm the diagnosis of
leukemia. Immunophenotyping helps to elucidate the subtype.
Aspiration slides should be stained for morphology with either Wright or Giemsa stain. The
diagnosis of acute lymphoblastic leukemia (ALL) is made when at least 30% lymphoblasts
(French-American-British [FAB] classification) or 20% lymphoblasts (World Health
Organization [WHO] classification) are present in the bone marrow and/or peripheral blood.
In addition, slides should be stained with myeloperoxidase (MPO) (or Sudan black) and terminal
deoxynucleotidyl transferase (TdT), unless another method is used, such as flow cytometry.
Bone marrow samples should also be sent for flow cytometry and cytogenetics. Approximately
15% of patients with ALL have a t(9;22) translocation (ie, Philadelphia [Ph] chromosome), but
other chromosomal abnormalities may also occur, such as t(4;11), t(2;8), and t(8;14).
Histologic Features
The older, traditional classification of acute lymphoblastic leukemia (ALL) is the French-
American-British (FAB) classification. This has now been replaced by the newer World Health
Organization (WHO) classification but the FAB system is listed for historical purposes, as
follows:
L1 Small cells with homogeneous chromatin, regular nuclear shape, small or absent nucleolus,
and scanty cytoplasm; subtype represents 25-30% of adult cases
L2 Large and heterogeneous cells, heterogeneous chromatin, irregular nuclear shape, and
nucleolus often large; subtype represents 70% of cases (most common)
L3 Large and homogeneous cells with multiple nucleoli, moderate deep blue cytoplasm, and
cytoplasmic vacuolization that often overlies the nucleus (most prominent feature); subtype
represents 1-2% of adult cases
The WHO classifies the L1 and L2 subtypes of ALL as either precursor B lymphoblastic
leukemia/lymphoblastic lymphoma (see the following image) or precursor T lymphoblastic
leukemia/lymphoblastic lymphoma depending on the cell of origin. The L3 subtype of ALL is
included in the group of mature B-cell neoplasms, as the subtype Burkitt lymphoma/leukemia.
Diagnostic workup of a patient with preB-cell acute lymphoblastic
leukemia. Bone marrow aspiration revealed French-American-British L2 morphology.
Immunohistochemistry
A negative myeloperoxidase (MPO) stain and a positive and terminal deoxynucleotidyl
transferase (TdT) is the hallmark of the diagnosis of most cases of acute lymphoblastic leukemia
(ALL). However, positive confirmation of lymphoid (and not myeloid) lineage should be sought
by flow cytometric demonstration of lymphoid antigens, such as CD3 (T-lineage ALL) or CD19
(B-lineage ALL), in order to avoid confusion with some types of myeloid leukemia (eg, M0),
which also stain negative with myeloperoxidase.
Flow Cytometry and Cytogenetics
Although more than 95% of cases of the L1 or L2 subtype of acute lymphoblastic leukemia
(ALL) are positive for Terminal deoxynucleotidyl transferase (TdT), TdT is not specific for
ALL; TdT is absent in L3 (mature B-cell) ALL. However, TdT helps to distinguish ALL from
malignancies of more mature lymphocytes (ie, non-Hodgkin lymphoma [NHL]).
In cases of acute leukemia that are myeloperoxidase (MPO) negative, and TdT positive, the
distinction between acute myelogenous leukemia (AML) and ALL is made based on the analysis
of flow cytometry results. Patients with AML demonstrate myeloid markers such as CD33,
whereas patients with ALL demonstrate lymphoid markers. Further confusion arises, because
some patients with ALL have aberrant expression of myeloid markers, such as CD13. However,
if the cells are TdT positive, MPO negative, CD33 negative, and demonstrate lymphoid markers,
the leukemia is considered ALL. See an example of a flow cytometry study below.
Diagnostic workup of a patient with preB-cell acute lymphoblastic
leukemia. Flow cytometry shows that the cells were positive for CD10, CD19, CD22, CD34, and terminal
deoxynucleotidyl transferase.
Cytogenetic abnormalities occur in approximately 70% of cases of ALL in adults (see Table 2,
below). These abnormalities include balanced translocations as occur in cases of AML.
However, abnormalities of chromosome number (hypodiploidy, hyperdiploidy) are more
common in ALL than in AML.
Table 2. Common Cytogenetic Abnormalities in ALL (Open Table in a new window)
Abnormality Genes Involved 3-Year Event-Free Survival
t(10;14)(q24;q11) HOX11/TCRA 75%
6q Unknown 47%
14q11 TCRA/TCRD 42%
11q23 MLL 18-26%
9p Unknown 22%
12 TEL 20%
t(1;19)(q23;p13) PBX1/E2A 20%
t(8;14)(q24;q32)
t(2;8)(p12;q24)
t(8;22)(q24;q11)
c-myc/IGH
IGK/c-myc
c-myc/IGL
17%
*
80%
t(9;22)(q34;q11) bcr-abl 5-10%
*
66%
t(4;11)(q21;q23) AF4-MLL 0-10%
*
Traditional regimens.
Hyper-CVAD (cyclophosphamide, vincristine, doxorubicin [Adriamycin], dexamethasone) with rituxan.
Hyper-CVAD with imatinib.
Eighty-five percent of cases of ALL are derived from B cells. The primary distinction is among
the following (see also Table 3, below):
Early (pro-B) ALL, which is TDT positive, CD10 (CALLA) negative, surface immunoglobulin (Ig)
negative
Precursor B ALL, which is TDT positive, CD10 (CALLA) positive, surface Ig negative
Mature B cell (Burkitt) ALL, which is TdT negative, surface Ig positive. Fifteen percent of these
cases are derived from T cells.
Table 3. Immunophenotyping of ALL Cells ALL of B-Cell Lineage (85% of cases of adult
ALL) (Open Table in a new window)
ALL Cells TdT CD19 CD10 CyIg SIg
Early B-precursor ALL + + - - -
PreB-cell ALL (see the image below) + + + + -
B-cell ALL - + +/- +/- +
ALL = acute lymphoblastic leukemia; Cylg = Cytoplasmic immunoglobulin; SIg =Surface immunoglobulin;
TdT = terminal deoxynucleotidyl transferase.
Diagnostic workup of a patient with preB-cell acute lymphoblastic
leukemia. Bone marrow aspiration revealed French-American-British L2 morphology.
These cases are subclassified into different stages corresponding to the phases of normal
thymocyte development. The early subtype is surface CD3 negative, cytoplasmic CD3 positive,
and either double negative (CD4
-
, CD8
-
) or double positive (CD4
+
, CD8
+
). The latter subtype is
surface CD3 positive, CD1a negative, and positive for either CD4 or CD8, but not both. See
Table 4, below.
Table 4. Immunophenotyping of ALL Cells ALL of T-Cell Lineage (15% of cases of adult
ALL) (Open Table in a new window)
ALL Cells TdT Surface CD3 CD4/CD8
Early T-precursor ALL + - +/+ or -/-
T-cell ALL + + +/- or -/+
Polymerase Chain Reaction or Cytogenics
Studies for bcr-abl analysis by polymerase chain reaction (PCR) or cytogenetics may help
distinguish patients with Philadelphia chromosome (Ph)positive ALL from those with the
lymphoid blastic phase of chronic myelogenous leukemia (CML). Most patients with Ph+ ALL
have the p190 type of bcr-abl, whereas patients with lymphoid blastic CML have the p210 type
of bcr-abl.
Gene Expression Profiling
Newer studies are analyzing acute lymphoblastic leukemia (ALL) subtypes by gene expression
profiling. In children with ALL, Bogni et al distinguished 3 groups of patients.
[4]
Interestingly,
one of these groups had a significantly increased risk of developing treatment-related acute
myelogenous leukemia (AML) following chemotherapy for their ALL.
Proceed to Treatment & Management
Approach Considerations
Patients with acute lymphoblastic leukemia (ALL) are best treated by physicians who have
significant experience in the treatment of patients with acute leukemia. In addition, these patients
should be treated in a setting where appropriate supportive care measures (high-level blood
banking and leukapheresis) are available.
Patients with acute lymphoblastic leukemia (ALL) require admission for induction
chemotherapy, and they require readmission for consolidation chemotherapy or for the treatment
of toxic effects of chemotherapy.
Surgical intervention may be required for the placement of a central venous catheter, such as a
triple lumen, Broviac, or Hickman catheter.
Chemotherapy and clinical trials
Only 20-30% of adults with ALL are cured with standard chemotherapy regimens.
Consequently, all patients must be evaluated for entry into well-designed clinical trials. If a
clinical trial is not available, the patient can be treated with standard therapy. Traditionally, the 4
components of ALL treatment are induction, consolidation, maintenance, and central nervous
system (CNS) prophylaxis; these are briefly reviewed in the following sections. Other aspects of
treatment are also discussed.
Transfer considerations
Patients with acute lymphoblastic leukemia (ALL) are best treated at a center with personnel
who have significant experience in the treatment of leukemia. Patients admitted to hospitals that
lack appropriate blood product support facilities, leukapheresis capabilities, or physicians and
nurses familiar with the treatment of patients with leukemia should be transferred to an
appropriate (generally tertiary care) hospital.
Induction Chemotherapy
Standard induction therapy typically involves either a 4-drug regimen of vincristine, prednisone,
anthracycline, and cyclophosphamide or L -asparaginase or a 5-drug regimen of vincristine,
prednisone, anthracycline, cyclophosphamide, and L -asparaginase given over the course of 4-6
weeks. Using this approach, complete remissions (CRs) are obtained in 65-85% of patients. The
rapidity with which a patient's disease enters CR is correlated with treatment outcome.
In a large French study, patients with greater than 5% blasts in their bone marrow on day 15 had
a lower response rate (34% vs 91%), worse disease-free survival, and worse overall survival than
patients with low blast counts on day 15.
[5]
Several other studies have shown that patients whose disease is in CR within 4 weeks of therapy
have longer disease-free survival and overall survival than those whose disease enters remission
after 4 weeks of treatment.
Consolidation Therapy
The use of consolidation chemotherapy in acute lymphoblastic leukemia (ALL) is supported by
several studies. Fiere et al compared consolidation therapy with daunorubicin and cytosine
arabinoside (Ara-C) versus no consolidation therapy in adults with ALL, demonstrating a 38% 3-
year, leukemia-free survival rate for subjects receiving consolidation and maintenance therapy
compared with 0% for those receiving maintenance therapy without consolidation.
[6]
In a study reported by Hoelzer et al, subjects whose disease was in remission after induction
received consolidation therapy consisting of dexamethasone, vincristine, and doxorubicin,
followed by cyclophosphamide, Ara-C, and 6-thioguanine beginning at week 20.
[7]
Subjects also
received maintenance therapy with 6-mercaptopurine and methotrexate during weeks 10-20 and
28-130. The median remission of 20 months was among the longest reported at the time.
In the United Kingdom Acute Lymphoblastic Leukemia XA study, subjects were randomized to
receive early intensification with Ara-C, etoposide, thioguanine, daunorubicin, vincristine, and
prednisone at 5 weeks; late intensification with the same regimen at 20 weeks; both; or neither.
[8]
The disease-free survival rates at 5 years were 34%, 25%, 37%, and 28%, respectively. These
data suggest a benefit to early, rather than late, intensification.
[8]
A study by the Cancer and Leukemia Group B (CALGB) did not show a benefit to consolidation
therapy. Subjects whose disease was in complete remission were randomized to receive
maintenance therapy or intensification with 2 courses of Ara-C and daunorubicin followed by
maintenance. Remission duration and overall survival were not affected by the randomization.
Because most studies have showed a benefit to consolidation therapy, regimens using a standard
4- to 5-drug induction usually include consolidation therapy with Ara-C in combination with an
anthracycline or epipodophyllotoxin.
Maintenance Therapy
The effectiveness of maintenance chemotherapy in adults with acute lymphoblastic leukemia
(ALL) has not been studied in a controlled clinical trial. However, several phase 2 studies
without maintenance therapy have shown inferior results compared with historical controls.
A Cancer and Leukemia Group B (CALGB) study of daunorubicin or mitoxantrone, vincristine,
prednisone, and methotrexate induction followed by 4 intensifications and no maintenance was
closed early because the median remission duration was shorter than in previous studies.
[9]
A
Dutch study using intensive postremission chemotherapy, 3 courses of high-dose Ara-C in
combination with amsacrine (course 1), mitoxantrone (course 2), and etoposide (course 3),
without maintenance, also yielded inferior results.
[10]
Although maintenance appears necessary, using a more intensive versus less intensive regimen
does not appear to be beneficial. Intensification of maintenance therapy from a 12-month course
of a 4-drug regimen compared with a 14-month course of a 7-drug regimen did not show a
difference in disease-free survival between the 2 groups.
[11]
A study by Ness et al found neuromuscular impairments were prevalent in survivors of
childhood ALL and these impairments interfered with physical performance.
[12]
Increased
cumulative doses of intrathecal methotrexate and/or vincristine were associated with long-term
neuromuscular impairments, and these have implications on future function with age.
CNS Prophylaxis
In contrast to patients with acute myelogenous leukemia (AML), patients with acute
lymphoblastic leukemia (ALL) frequently have meningeal leukemia at the time of relapse. A
minority of patients have meningeal disease at the time of initial diagnosis. As a result, central
nervous system (CNS) prophylaxis with intrathecal chemotherapy is essential.
Cortes et al analyzed the prevalence of CNS leukemia in 4 consecutive clinical trials at the MD
Anderson Cancer Center and found that that high-dose systemic chemotherapy reduces CNS
relapse; however, early intrathecal chemotherapy is necessary to achieve the lowest risk of CNS
relapse.
[13]
CNS relapse rates were 31% for group 1 (standard chemotherapy, no CNS
prophylaxis), 18% for group 2 (high-dose systemic chemotherapy, no CNS prophylaxis), 17%
for group 3 (high-dose systemic chemotherapy, intrathecal chemotherapy for high-risk subjects
after achieving remission), and 3% for group 4 hyperfractionated cyclophosphamide, vincristine,
doxorubicin, and dexamethasone (hyper-CVAD).
[13]
All subjects received intrathecal
chemotherapy starting in induction. High-risk subjects received 16 intrathecal treatments, and
low-risk subjects received 4 intrathecal treatments.
Newer Induction Approaches
Standard induction regimens are modeled after pediatric programs and were originally developed
when supportive care was significantly inferior to what is available today. Few antibiotics were
available, and transfusion capabilities were minimal. Consequently, milder regimens were
designed in an attempt to minimize early deaths during induction.
With the addition of third-generation cephalosporins and sophisticated blood-banking
techniques, the ability to support patients through a pancytopenic phase has increased
dramatically. As a result, more intensive induction approaches are used by many physicians.
Two notable examples are the Memorial acute lymphoblastic leukemia (ALL)-2 protocol and the
hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone) protocol.
ALL-2 protocol
The ALL-2 protocol uses an intensive, high-dose, mitoxantrone-based, acute myelogenous
leukemia (AML)-style induction regimen. In a phase 1 study of high-dose mitoxantrone
combined with high-dose cytosine arabinoside (Ara-C), Arlin et al reported that 8 of 8 patients
newly diagnosed with ALL and 8 of 10 patients with ALL who relapsed achieved complete
remission (CR).
[14]
Weiss et al reported treatment of 37 subjects with newly diagnosed ALL with this induction
regimen followed by a first consolidation with vincristine, prednisone, L -asparaginase, and
methotrexate; a second consolidation with Ara-C and etoposide; and then 2 years of maintenance
therapy.
[15]
Of these subjects, 84% achieved CR. The median remission duration was 17 months,
and median survival was 20 months.
[15]
In a randomized phase III trial comparing the ALL-2 regimen with the L-20 regimen (vincristine,
prednisone, cyclophosphamide and doxorubicin), the CR rate was 83% for patients receiving
ALL-2 compared with 70% for patients receiving L-20.
[16]
Overall survival at 4 years was
superior for patients receiving ALL-2 (40%) versus those receiving L-20 (22%).
Hyper-CVAD regimen
The hyper-CVAD regimen is based on the success achieved with short-term, dose-intensive
chemotherapy regimens in children. It incorporates hyperfractionated cyclophosphamide and
intensive doses of Ara-C and methotrexate in combination with dexamethasone and vincristine.
Maintenance therapy with prednisone, vincristine (Oncovin), methotrexate, and mercaptopurine
(Purinethol) (ie, POMP protocol) is given to patients with nonmature B-cell ALL.
From 1992-2000, 288 patients received hyper-CVAD at MD Anderson Cancer Center, which
17% of patients had the Philadelphia (Ph) chromosome, and 13% had T-cell ALL.
[17]
Overall,
92% of patients obtained a CR. The 5-year survival and percentage of patients in CR at 5 years
were both 38%. Patients with Ph+ ALL had a 92% CR rate but only a 12% 5-year survival.
Patients with T-cell ALL had a 75% CR rate and a 48% 5-year survival. Patients with Burkitt
ALL had a 93% CR rate and a 67% 5-year survival.
[17]
Newer modifications of the hyper-CVAD regimen include the addition of imatinib to patients
whose leukemia is Philadelphia chromosome positive, and rituxan to patients whose leukemia is
CD20 positive. Both of these approaches have resulted in improvements in disease-free survival
(see below).
Treatment of Mature B-Cell ALL
Mature B-cell acute lymphoblastic leukemia (ALL) is a special type, representing only 5% of
adult patients with ALL. The hallmark of mature B-cell ALL is the presence of surface
immunoglobulin on the lymphoblasts. Using conventional regimens, only 30-40% of patients
enter complete remission (CR) and few patients survive long term.
Newer short-term intensive therapies show improved results. A report of the hyper-CVAD
regimen showed that disease in 93% of subjects entered CR, median survival was 16 months,
and disease in 67% of subjects alive at 5 years.
In a report by Hoelzer et al, with the use of regimens containing intensive cyclophosphamide and
intermediate methotrexate or ifosfamide and high-dose methotrexate, CR rates were 63%
(cyclophosphamide + intermediate methotrexate) and 74% (ifosfamide + high-dose
methotrexate).
[18]
Disease-free survival rates increased to 50% in the first group and 71% in the second group, and
overall survival increased to 50% compared with 0% for historical controls.
[18]
Although
previously these patients were referred for transplantation in first remission, many physicians
now defer transplantation for the time of relapse because of these improved results.
Burkitt ALL cells are CD20 positive. This allows for the addition of targeted therapy with
rituximab. Many studies are have demonstrated improved efficacy, including prolonged survival,
when rituximab is added to chemotherapy in these patients. The combination of hyper-CVAD
(hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) plus rituxan
resulted in an overall 3-year survival of 80% compared with 50% for historical controls treated
without rituxan.
[19]
Treatment of Ph ChromosomePositive ALL
In the past, Philadelphia chromosomepositive (Ph+) acute lymphoblastic leukemia (ALL) was
treated with the same regimens as other types of ALL, with poor results. However, imatinib
inhibits the bcr-abl fusion protein of Ph+ ALL and thus allows targeted therapy of this disease.
As a single agent, imatinib has limited activity.
In an early study of patients with Ph+ ALL or chronic myelogenous leukemia (CML) in
lymphoid blast crisis, only 4 of 20 patients had a complete response, and all patients progressed
in less than 6 months.
[20]
Imatinib
The German Multicenter ALL (GMALL) trial conducted a randomized study of imatinib versus
standard induction therapy for patients with Ph-positive ALL older than 55 years and reported
the overall complete remission (CR) rate was 96.3% in patients randomly assigned to imatinib
and 50% in patients allocated to standard chemotherapy.
[21]
Severe adverse events were
significantly more frequent during standard induction chemotherapy (90% vs 39%). The
estimated overall survival of all patients was 42% at 24 months, with no significant difference
between the 2 cohorts.
[21]
The addition of imatinib to chemotherapy has resulted in significantly improved outcomes. The
addition of imatinib to hyper-CVAD (hyperfractionated cyclophosphamide, vincristine,
doxorubicin, and dexamethasone) resulted in a 3-year disease-free survival rate of 66% and
overall survival of 55% compared with a 14% 3-year disease-free survival rate and 15% overall
survival for patients treated with hyper-CVAD without imatinib.
[22]
Similar results have been
reported when imatinib is added to other chemotherapy regimens.
Newer tyrosine kinase inhibitors have been developed for patients with chronic myelogenous
leukemia (CML) that has become resistant to imatinib. These agents are also being studied in Ph-
positive ALL.
Nilotinib and dasatinib
Nilotinib is a tyrosine kinase inhibitor that has a higher binding affinity and selectivity for the
ABL kinase than imatinib.
[23]
Nilotinib has 20 to 50 times the inhibitory activity against imatinib-
sensitive CML cell lines relative to imatinib. In a phase II study in patients with
relapsed/refractory Ph-positive ALL, complete responses were reported in 10 (24%) patients
treated with nilotinib.
[23]
Dasatinib is a potent, orally active inhibitor of the BCR-ABL, c-KIT and the SRC family of
kinases.
[24]
Dasatinib is a more potent inhibitor of BCR-ABL and c-KIT than imatinib mesylate,
and it is effective in patients with CML that is resistant to or intolerant of imatinib.
The Gruppo Italiano Malattie Ematologiche dell'Adulto (GIMEMA) presented the interim results
of a prospective study of dasatinib in patients with newly diagnosed Ph-positive ALL.
Prednisone was started 7 days before the first dasatinib administration and continued until day
31. Dasatinib was administered for a total of 84 days. At the time of the report, all 23 patients
treated showed a complete hematologic response by day +22.
Although nilotinib and dasatinib are clearly active in Ph-positive ALL, it is likely that, similar to
the results seen with imatinib, these responses will likely not be durable. Therefore each of these
agents is currently being studied in combination with standard chemotherapy regimens.
That said, these new tyrosine kinase inhibitors are not without their drawbacks and adverse
events. Dasatinib has been associated with pleural effusions and pulmonary arterial
hypertension,
[25]
while nilotinib has been linked to biochemical changes in liver function and QT-
interval prolongation. Development of resistance may also occur with these agents.
In the GIMEMA LAL1205 protocol, patients who had newly diagnosed Ph
+
ALL received only
dasatinib (for 84 d), steroids (for the first 32 d), and intrathecal chemotherapy as induction
therapy.
[26]
Fifty-three patients were able to be evaluated (median age, 53.6 y). All patients
achieved a complete hematologic remission; 49 patients (92.5%) achieved this at day 22.
Postinduction management was decided by the investigator and included no further treatment (2
patients), TKI alone (19 patients), TKI plus chemotherapy and/or autografting (14 patients), and
allografting (18 patients). At 20 months, the overall survival was 69.2% and disease-free survival
was 51.1%. Twenty-three patients relapsed after completing induction.
Ponatinib
Ponatinib (Iclusig), a kinase inhibitor, was approved in December 2012 for patients with Ph+
ALL that is resistant or intolerant to prior tyrosine kinase inhibitor therapy, including those with
the T315I mutation. Data from the Phase 2 PACE trial showed 54% of chronic-phase CML
patients, including 70% of patients with the T315I mutation, achieved a major cytogenetic
response. In patients with advanced disease, 52% of those with accelerated-phase CML, 31% of
those with blast-phase CML, and 41% of those with Ph+ ALL achieved a major hematologic
response to ponatinib.
[27]
These results confirm the phase 1 clinical trial.
[28]
Treatment of the Younger Adult
Older children and younger adults with acute lymphoblastic leukemia (ALL) can be referred to
either adult or pediatric hematologists. Usually, the patient will receive either an adult or
pediatric regimen based on this referral pattern. However, several studies have suggested that
younger patients are best treated on pediatric protocols.
For example, in a retrospective analysis of patients aged 15-20 years treated on either the
FRALLE 93 or LALA 94 trials, the complete remission (CR) rate was 94% for patients receiving
the pediatric regimen compared with 83% for those receiving the adult.
[29]
The 5-year survival
was 67% in the pediatric-regimen group and 41% in the adult-regimen group. Patients treated on
the pediatric regimen were younger (15.9 y) than those treated on the adult regimen (17.9 y);
however, prognostic factors were otherwise matched.
[29]
Similarly, the Childrens Cancer Group (CCG) and CALGB performed an analysis on patients
aged 16-21 years treated on their studies and, again, event-free and overall survival were
improved for patients treated on the CCG protocols.
[30]
In a study by the Programme for the Study of Therapeutics for Haematological Malignancies
(PETHEMA), adolescents and young adults were treated with a pediatric regimen (ALL-96),
demonstrating a response to therapy that was similar to previously reported, although a slight
increase in hematologic toxicity was observed in the adult patients.
[31]
The majority of children with ALL are cured with frontline chemotherapy regimens. Many
investigators are trying to translate these results into the adult population. Areas being studied
include increased intensity of standard agents including asparaginase, risk-adapted
chemotherapy, and evaluation of minimal disease.
Transplantation
Relatively few studies have compared transplantation with chemotherapy in adults with acute
lymphoblastic leukemia (ALL). In a study by the Groupe Ouest-Est des Leucemies Airgues et
Maladies du Sang (GOELAMS), subjects younger than 45 years who had a sibling donor and
whose disease was in remission were assigned to allogeneic transplantation.
[32]
The remaining
subjects received methylprednisolone, Ara-C, mitoxantrone, and etoposide chemotherapy
followed by autologous bone marrow transplantation (BMT).
Bone marrow transplantation
For subjects undergoing allogeneic BMT, the rate of freedom from relapse was 70% at 4
years.
[32]
However, because of transplant-related complications, the event-free survival rate was
only 33%. No toxic deaths occurred in the subjects who underwent autologous BMT. However,
the event-free survival rate was only 17% at 4 years because of a high rate of relapse.
[32]
In a prospective, nonrandomized trial, the Bordeaux, Grenoble, Marseille, Toulouse group found
that the 3-year probability of disease-free survival was significantly higher in their group
assigned to allogeneic BMT (68%) compared with subjects assigned to autologous BMT
(26%).
[33]
No benefit was observed with the addition of recombinant interleukin 2 (IL-2) after
autologous BMT.
In the French Group on Therapy for Adult Acute Lymphoblastic Leukemia study, subjects aged
15-40 years whose disease was in complete remission (CR) and who had a human leukocyte
antigen (HLA)-compatible sibling donor underwent allogeneic BMT.
[5]
The other subjects were
randomized to receive autologous BMT or chemotherapy. Overall, no difference in was observed
in 5-year survival between the groups.
[5]
When only high-risk patients were considered (ie,
Philadelphia chromosomepositive (Ph+), null ALL; >35 y; white blood cell [WBC] count
>30,000/L; or time to CR > wk), overall survival rates (44% vs 20%) and disease-free survival
rates (39% vs 14%) were superior for those undergoing allogeneic BMT versus those undergoing
either autologous BMT or chemotherapy.
[5]
Other phase 2 studies have confirmed a benefit for
high-risk patients who undergo allogeneic BMT, with as many as 50% achieving long-term
remissions.
Stem cell transplantation
In the GOELAL02 study, patients with any high-risk feature (age >35 y, nonT-ALL, WBC
>30,000, adverse cytogenetics: t[9;22], t[4;11], or t[1;19], or no CR after induction) received
either allogeneic or autologous stem cell transplantation. For patients younger than 50 years, the
6-year overall survival rate was improved for patients receiving allogeneic transplantation (75%)
compared with those receiving autologous transplantation (40%).
[32]
The United Kingdom Medical Research Council Acute Lymphoblastic Leukemia joint trial with
the Eastern Cooperative Oncology Group (MRC UKALL XII/ECOG E2993) demonstrated that
matched related allogeneic transplantations for acute lymphoblastic leukemia (ALL) in first
complete CR provide the most potent antileukemic therapy and considerable survival benefit for
standard-risk patients. A donor versus no-donor analysis showed that Ph-negative patients with a
donor had a 5-year improved overall survival, 53% versus 45% (P = 0.01), and that the relapse
rate was significantly lower.
[34]
The survival difference was significant in standard-risk patients but not in high-risk patients with
a high nonrelapse mortality rate in the high-risk donor group. Patients randomized to
chemotherapy had a higher 5-year overall survival (46%) than those randomized to autologous
transplantation (37%).
[34]
However, the transplantation-related mortality for high-risk older
patients was unacceptably high and abrogated the reduction in relapse risk.
Allogeneic transplantation can also be effective therapy for patients who have experienced
relapse after chemotherapy. Martino et al treated 37 consecutive patients with primary refractory
or relapsed ALL with intensive salvage chemotherapy.
[35]
Of the 19 patients assigned to
autologous BMT, 10 did not reach transplantation, mostly because of early relapse; 9 received
transplants. Of these, 1 died early and 8 experienced relapse 2-30 months after transplantation.
Of the 10 patients who received allogeneic BMT, 4 died early and 6 were alive and free from
disease 9.7-92.6 months after the transplantation.
[35]
These results are similar to those in patients in earlier stages, indicating that transplant-related
complications are increased in the allogeneic setting. However, a significant number of patients
can be cured. Yet, although autologous transplantation is relatively safe, it is associated with a
high relapse rate, making this modality of little use in patients with ALL.
Unrelated donor transplantation
For patients without a sibling donor, an alternative is an unrelated donor (URD) transplant.
Weisdorf et al found that autologous BMT was associated with a lower transplant-related
mortality rate, but URD transplantations had a lower risk of relapse.
[36]
In patients whose disease
was in second CR, URD transplantations resulted in a superior rate of disease-free survival.
[36]
Although peripheral blood has come to be preferred to bone marrow as the source for stem cells
from unrelated donors (about 75% of transplants), a randomized phase III trial found that
peripheral-blood stem cells did not yield improved survival as compared with bone-marrow cells
and were significantly associated with chronic graft-vs-host disease (GVHD)
[37, 38]
; the authors
suggested that peripheral-blood stem cells might be appropriate for patients at higher risk for
graft failure and bone-marrow cells for all others.
Summary
In summary, most authorities agree that allogeneic transplantation should be offered to young
patients with high-risk features whose disease is in first remission. Young patients without
adverse features should receive induction, consolidation, and maintenance therapy. In these
patients, transplantation is reserved for relapse.
Older patients whose disease is in CR may be considered for such investigational approaches as
allogeneic transplantation with nonmyeloablative chemotherapy (ie, mini-transplants). Although
previously patients with mature B-cell ALL would have been referred for transplantation when
their disease was in first CR with improving results from more intensive chemotherapy regimens,
many clinicians are reserving transplantation for patients who have experienced relapse.
Hematopoietic stem cell transplantation (HSCT) seems to be a valuable option for a subgroup of
infants with mixed-lineage (MLL
+
) ALL carrying poor prognostic factors that include age
younger than 6 months and either poor response to steroids at day 8 or leukocytes more than or
equal to 300 g/L.
[39]
Treatment of Relapsed ALL
Patients with relapsed acute lymphoblastic leukemia (ALL) have an extremely poor prognosis.
Most patients are referred for investigational therapies. Young patients who have not previously
undergone transplantation are referred for such therapy. Reinduction regimens include the hyper-
CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone) protocol and high-dose
cytosine arabinoside (Ara-C)based regimens.
As noted earlier, the hyper-CVAD regimen is based on hyperfractionated cyclophosphamide and
intermediate doses of Ara-C and methotrexate. In a study at the MD Anderson Cancer Center of
66 patients with relapsed ALL, the complete remission (CR) rate was 44% and median survival
was 42 weeks.
Arlin et al reported that 8 of 10 patients with relapsed ALL achieved CR with high-dose Ara-C
and high-dose mitoxantrone.
[14]
A similar regimen using a single high dose of idarubicin in
combination with Ara-C (the Memorial ALL-3 protocol) resulted in CR rates of 58-78% in
patients who experienced relapse.
The Italian ALL R-87 study suggested that a small number of patients who experience relapse
will survive long-term after allogeneic bone marrow transplantation (BMT)
[40]
; however,
autologous BMT is less useful because it is associated with a high rate of relapse. Sixty-one
subjects with ALL in first relapse received induction chemotherapy with intermediate-dose Ara-
C, idarubicin, and prednisone. Subjects whose disease was in remission were to receive
consolidation chemotherapy and then BMT. Of these subjects, 56% achieved CR; however, only
9 of the responders underwent BMT.
[40]
The remaining subjects did not undergo transplantations
because of either early relapse or excessive toxicity. Of the 4 subjects who underwent allogeneic
BMT, 3 were alive and achieved remission at 22, 43, and 63 months, whereas only 1 of the 5
subjects who underwent autologous BMT was alive.
[40]
In August 2012, the FDA approved vincristine liposomal (Marqibo) for the treatment of
Philadelphia chromosome negative (Ph-) acute lymphoblastic leukemia in adults. It is indicated
for patients in second or greater relapse or whose disease has progressed following 2 or more
anti-leukemia therapies. It is a sphingomyelin/cholesterol liposome-encapsulated formulation of
vincristine. In a trial of 65 patients that received at least 1 dose of vincristine liposomal, 15.4% of
the patients had complete remission which lasted a median of 28 days.
[41]
In December 2012, the kinase inhibitor ponatinib was approved for Ph+ ALL that is resistant or
intolerant to prior tyrosine kinase inhibitor therapy. For more information, see Treatment of Ph
Chromosome-Positive ALL.
Novel and Experimental Drug Therapies
A number of new drugs are in development for the treatment of acute lymphoblastic leukemia
(ALL).
Clofarabine is a novel nucleoside analogue that is approved for the treatment of pediatric patients
with refractory or relapsed ALL.
[42]
This agent inhibits DNA synthesis at both DNA polymerase I
and at RNA reductase. Overall response rates average 25%.
506U78 (nelarabine [Arranon]) is a novel purine nucleoside that is a prodrug of guanine
arabinoside (ara-G).
[43]
This agent was approved as an orphan drug by the US Federal Drug
Administration (FDA) in October 2005. Complete responses have been reported in 31% of
patients and in 54% of patients with T-cell ALL. The dose-limiting toxicity of this drug is
neurotoxicity.
[43]
Supportive Care - Blood Products
Patients with acute lymphoblastic leukemia (ALL) have a deficiency in the ability to produce
normal blood cells, and they need replacement therapy. This deficiency is temporarily worsened
by the addition of chemotherapy. All blood products must be irradiated to prevent transfusion-
relatedgraft versus host disease, which is almost invariably fatal.
Packed red blood cells are given to patients with a hemoglobin level of less than 7-8 g/dL or at a
higher level if the patient has significant cardiovascular or respiratory compromise.
Platelets are transfused if the count is less than 10,000-20,000/L. Patients with pulmonary or
gastrointestinal hemorrhage receive platelet transfusions to maintain a value greater than
50,000/L. Patients with central nervous system CNS hemorrhage are transfused to achieve a
platelet count of 100,000/L.
Fresh frozen plasma is given to patients with a significantly prolonged prothrombin time (PT),
and cryoprecipitate is given if the fibrinogen level is less than 100 g/dL.
Grace et al reported age was the only significant predictor of asparaginase-related venous
thromboembolic events (VTE), with ALL patients older than 30 years at very high risk (VTE
rate 42%).
[44]
The investigators reviewed the features, management, and outcome of pediatric (0-
18 y) and adult (18-50 y) patients with ALL with VTE: Of 548 patients, 43 (8%) had VTE,
including 27 of 501 (5%) pediatric and 16 of 47 (34%) adult patients.
[44]
Sinus venous
thrombosis occurred in 1.6% of patients.
Seventy-four percent of patients received low-molecular-weight-heparin after VTE.
[44]
Complications of anticoagulation included epistaxis (9%), bruising (2%), and, in 2 adult patients,
major bleeding. Thirty patients (70%) ultimately received at least 85% of the intended doses of
asparaginase. Thirty-three percent of patients experienced recurrent VTE (pediatric 17% vs
adults 47%). The 48-month event-free survival for patients with VTE was 85.6% compared with
88.2% for those without VTE.
[44]
Supportive Care - Antibiotic Therapy
Antibiotics are given to all febrile patients. At a minimum, include a third-generation
cephalosporin (or equivalent), usually with an aminoglycoside. In addition to this minimum,
other antibiotic agents are added to treat specific documented or possible infections.
Patients with persistent fever after 3-5 days of antibacterial antibiotics should have an antifungal
antibiotic (liposomal or lipid complex amphotericin, new generation azole or echinocandin)
added to their regimen. Patients with sinopulmonary complaints would receive anti-Aspergillus
treatment. Particular care is warranted for patients receiving steroids as part of their treatment,
because the signs and symptoms of infection may be subtle or even absent.
The use of prophylactic antibiotics in neutropenic patients who are not febrile is controversial.
However, most clinicians prescribe them for patients undergoing induction therapy. A commonly
used regimen includes the following:
Ciprofloxacin (oral [PO] 500 mg twice daily [bid])
Fluconazole (200 mg PO daily), itraconazole (200 mg PO bid), or posaconazole (200 mg PO three
times daily [tid])
Acyclovir (200 mg PO 5 times/d) or valacyclovir (500 mg PO daily)
Once patients taking these antibiotics become febrile, they are switched to intravenous
antibiotics.
Supportive Care - Growth Factors
The use of granulocyte colony-stimulating factor (G-CSF) during induction chemotherapy for
acute lymphoblastic leukemia (ALL) is supported by several studies. In a randomized phase 3
trial conducted by Ottoman, 76 subjects received either G-CSF or no growth factor with the
induction chemotherapy (ie, cyclophosphamide, cytosine arabinoside (Ara-C), 6-mercaptopurine,
intrathecal methotrexate, and cranial irradiation). The median duration of neutropenia was 8 days
in subjects receiving G-CSF versus 12 days in subjects receiving no growth factor, and the
prevalence of nonviral infections was decreased by 50% in subjects receiving G-CSF. No
difference in disease-free survival was observed between the 2 groups.
In a randomized phase 3 study reported by Geissler et al, subjects who received G-CSF
beginning on day 2 of induction chemotherapy (ie, with daunorubicin, vincristine, L -
asparaginase, and prednisone) had a marked decrease in the proportion of days with neutropenia
of less than 1000/L (29% for G-CSF vs 84% for controls), a reduction in the prevalence of
febrile neutropenia (12% vs 42% in controls), and a decrease in the prevalence of documented
infections (40% vs 77%) relative to those who received chemotherapy without G-CSF.
[45]
No
difference was observed in response, remission duration, or survival between the 2 groups.
[45]
In the Cancer and Leukemia Group B (CALGB) 9111 study, subjects who received G-CSF
beginning on day 4 of induction chemotherapy had significantly shorter durations of neutropenia
and significantly fewer days of hospitalization compared with those in the group that received
placebo.
[46]
In this study, subjects receiving G-CSF also had higher complete remission (CR)
rates, because fewer deaths occurred during remission induction. Again, no significant effect on
disease-free survival or overall survival was observed.
[46]
The importance of the early use of G-CSF FOR ALL was demonstrated by the study of Bassan et
al, in which subjects who received induction chemotherapy with idarubicin, vincristine, L -
asparaginase, and prednisone and G-CSF on day 4 recovered significantly faster from
neutropenia, had fewer infectious complications, and required less antibiotic than subjects
beginning G-CSF on day 15.
[47]
Outside of the setting of a clinical trial, few data support the use of granulocyte-macrophage
colony-stimulating factor (GM-CSF) in patients with ALL. The GOELAMS investigators
randomly assigned 67 subjects to receive GM-CSF or placebo during induction chemotherapy
with idarubicin, methylprednisolone, and high-dose Ara-C and observed no difference in the CR
rate, the duration of neutropenia, or days with fever for the 2 groups.
[48]
In addition, mucositis of
higher than grade 3 was reduced in subjects receiving GM-CSF (2 of 35 patients vs 6 of 29
patients, respectively.
[48]
In a Groupe d'Etude et de Traitement de la Leucemie Aigue Lymphoblastique de l'Adulte (GET-
LALA) study, in patients who received G-CSF, GM-CSF, or no growth factor during induction
therapy, the median time for neutrophil recovery was 17 days for G-CSF, 18 days for GM-CSF,
and 21 days for no growth factors.
[49]
Hyperuricemia and Tumor Lysis Syndrome
Tumor lysis syndrome is a potentially life-threatening complication that may be seen in patients
receiving chemotherapy for acute leukemias and high-grade non-Hodgkin lymphomas. This
syndrome is characterized by elevated blood levels of uric acid, phosphate, and potassium;
decreased levels of calcium; and acute renal failure.
As mentioned earlier, patients with a high tumor burden, particularly those with severe
hyperuricemia, can present in renal failure. Allopurinol at 300 mg 1-3 times per day is
recommended during induction therapy until blasts are cleared and hyperuricemia resolves.
High-risk patients (those with very high lactate dehydrogenase [LDH] or leukemic infiltration of
the kidneys) can benefit from rasburicase.
In a study by Cortes et al, adults with hyperuricemia or those at high risk for tumor lysis
syndrome not only had an improved plasma uric acid response rate with rasburicase alone (0.20
mg/kg/d intravenously [IV], days 1-5) (87%) or in combination with allopurinol (IV rasburicase
0.20 mg/kg/d, days 1-3, followed by oral [PO] allopurinol 300 mg/d, days 3-5) (78%) than with
allopurinol alone (300 mg/d PO, days 1-5) (66%), but they also had more rapid control of their
plasma uric acid with rasburicase alone (4 h) or with allopurinol (4 h) than with allopurinol alone
(27 h).
[50]
Long-Term Monitoring
Patients with acute lymphoblastic leukemia (ALL) are monitored on an outpatient basis for
disease status and the effects of chemotherapy. Maintenance therapy for these patients is also
administered in an outpatient setting.
In addition, all patients should be on trimethoprim-sulfamethoxazole (TMP-SMZ) to prevent
Pneumocystis carinii pneumonia (PCP), and patients may benefit from receiving oral nystatin or
clotrimazole troches to reduce the risk of candidiasis. Patients with a high risk of relapse may
also need additional antifungal therapy, such as itraconazole.
Proceed to Medication
Medication Summary
The medications used to treat acute leukemia cause severe bone marrow depression. Only
physicians specifically trained in their use should administer these medications. In addition,
access to appropriate supportive care is required.
A regimen of fludarabine and cyclophosphamide and rituximab (FCR) is commonly used. This
combination of 3 of the most active drugs is a good example of a synergistic combination of
drugs with different mechanisms. Different forms of the FCR combination are used; therefore,
the dosing plays a big role in results. FCR provides a cyclical form of treatment, rather than a 1-
time, transplant-conditioning regimen followed by stem cells. In a study by Matutes et al, the
FCR regimen did not quite overcome fludarabine resistance, which remains probably the single
most important hurdle in long-term term outcomes for patients with acute lymphoblastic
leukemia (ALL).
[51]
Corticosteroids
Class Summary
Corticosteroids may be used during induction, consolidation, and/or maintenance therapy for
acute lymphoblastic leukemia (ALL).
View full drug information
Prednisone
Prednisone is a corticosteroid that has a wide range of activities. In ALL, this agent is used
because of its direct antileukemic effects.
View full drug information
Dexamethasone (Baycadron, Maxidex, Ozurdex)
Dexamethasone is another corticosteroid that acts as an important chemotherapeutic agent in the
treatment of ALL. Like prednisone, this agent is used in induction and reinduction therapy and is
also given as intermittent pulses during continuation therapy.
Antineoplastics
Class Summary
Antineoplastic agents are used for induction, consolidation, maintenance, and central nervous
system (CNS) prophylaxis.
Cancer chemotherapy is based on an understanding of tumor cell growth and how drugs affect
this growth. After cells divide, they enter a period of growth (ie, phase G1), followed by DNA
synthesis (ie, phase S). The next phase is a premitotic phase (ie, G2), then, finally, a mitotic cell
division (ie, phase M).
Cell-division rates vary for different tumors. Most common cancers grow slowly compared with
normal tissues, and the rate may be decreased in large tumors. This difference allows normal
cells to recover from chemotherapy more quickly than malignant ones and is the rationale behind
current cyclic dosage schedules.
Antineoplastic agents interfere with cell reproduction. Some agents act at specific phases of the
cell cycle, whereas others (ie, alkylating agents, anthracyclines, cisplatin) are not phase specific.
Cellular apoptosis (ie, programmed cell death) is another potential mechanism of many
antineoplastic agents.
View full drug information
Vincristine (Vincasar PFS)
Vincristine is a vinca alkaloid agent that acts by arresting cells in metaphase.
View full drug information
Vincristine liposomal (Marqibo)
A sphingomyelin/cholesterol liposome-encapsulated formulation of vincristine. Indicated for
treatment of Ph-negative ALL for patients in second or greater relapse or whose disease has
progressed following 2 or more antileukemia therapies.
View full drug information
Asparaginase (Elspar)
Asparaginase breaks down extracellular asparagine into aspartic acid and ammonia. Normal cells
are capable of synthesizing their own asparagine, but many malignant cells are not.
View full drug information
Asparaginase Erwinia chrysanthemi (Erwinaze)
Catalyzes deamidation of asparagine to aspartic acid and ammonia, thereby reducing circulating
levels of asparagine. Lack of asparagine synthetase activity results in cytotoxicity specific for
leukemic cells that depend on an exogenous source of the amino acid asparagine. Indicated as
part of a multiagent chemotherapeutic regimen for patients with acute lymphoblastic leukemia
(ALL) who have developed hypersensitivity to E coli derived asparaginase. It is estimated that
15-20% of patients with ALL develop a hypersensitivity to E coli derived asparaginase, which
extrapolates to approximately 450-600 children in the United States annually.
View full drug information
Methotrexate (Trexall)
Methotrexate is an antimetabolite of the folic acid analogue type. This agent inhibits
dihydrofolate reductase, resulting in inhibition of DNA synthesis, repair, and cellular replication.
View full drug information
Mercaptopurine (Purinethol)
Mercaptopurine is antimetabolite of the purine analogue type. Its primary effect is inhibition of
DNA synthesis.
View full drug information
Cyclophosphamide
Cyclophosphamide is an alkylating agent of the nitrogen mustard type that acts by inhibiting cell
growth and proliferation.
View full drug information
Cytarabine
Cytosine arabinoside is an antimetabolite that induces activity as a result of activation to
cytarabine triphosphate and includes inhibition of DNA polymerase and incorporation into DNA
and RNA.
View full drug information
Daunorubicin (Cerubidine)
Daunorubicin is an anthracycline that inhibits topoisomerase II. This agent also inhibits DNA
and RNA synthesis by intercalating between DNA base pairs.
View full drug information
Idarubicin (Idamycin)
Idarubicin is a topoisomerase II inhibitor that inhibits cell proliferation by inhibiting DNA and
RNA polymerase.
View full drug information
Mitoxantrone (Novantrone)
Mitoxantrone is also a topoisomerase II inhibitor. This agent inhibits cell proliferation by
intercalating DNA and inhibiting topoisomerase II.
View full drug information
Dasatinib (Sprycel)
Dasatinib is a multiple tyrosine kinase inhibitor that inhibits the growth of cell lines
overexpressing BCR-ABL. This agent is indicated for Philadelphia chromosomepositive acute
lymphoblastic leukemia (Ph+ ALL) in individuals with resistance to or who were intolerant of
previous therapy.
View full drug information
Nelarabine (Arranon)
Nelarabine is a prodrug of the deoxyguanosine analogue 9-beta-D-arabinofuranosylguanine (ara-
G) that is converted to the active 5'-triphosphate, ara-GTP, a T-cellselective nucleoside
analogue. Leukemic blast cells accumulate ara-GTP, which allows for incorporation into DNA,
leading to inhibition of DNA synthesis and cell death.
This agent is approved by the US Food and Drug Administration (FDA) as an orphan drug to
treat persons with T-cell ALL whose disease has not responded to or which has relapsed with at
least 2 chemotherapy regimens.
View full drug information
Clofarabine (Clolar)
Clofarabine is a purine nucleoside antimetabolite that inhibits DNA synthesis and is indicated for
relapsed or refractory acute lymphoblastic leukemia in pediatric patients. Pools of cellular
deoxynucleotide triphosphate are decreased by inhibiting ribonucleotide reductase and
terminating DNA chain elongation and repair. This agent also disrupts mitochondrial membrane
integrity. It is indicated for the treatment of patients aged 1-21 years who have relapsed or
refractory acute ALL. For adults older than 21 years, base dosing on surface area as in pediatrics.
Clofarabine is not indicated for adults older than 21 years.
Tyrosine Kinase Inhibitors
Class Summary
Philadelphia chromosome-positive (Ph+) ALL is treated with tyrosine kinase inhibitors. These
agents provide targeted therapy by inhibiting the BCR-ABL fusion protein.
View full drug information
Imatinib (Gleevec)
Imatinib is indicated for relapsed or refractory Ph+ ALL. It is also indicated for newly diagnosed
PH+ CML in chronic phase and for Ph+ CML in blast crisis, accelerated phase, or chronic phase
after failure of interferon-alpha therapy.
View full drug information
Nilotinib (Tasigna)
Nilotinib is indicated for newly diagnosed Ph+ CML in chronic phase and for the treatment of
Ph+ CML (chronic phase, accelerated phase) in patients resistant or intolerant to prior therapy
including imatinib.
View full drug information
Dasatinib (Sprycel)
Dasatinib is indicated for Ph+ ALL with resistance or intolerance to prior therapy. It is also
indicated for newly diagnosed Ph+ CML in chronic phase, CML (chronic, accelerated, or plast
phase Ph+) with resistance or intolerance to prior therapy including imatinib.
View full drug information
Ponatinib (Iclusig)
Ponatinib is a kinase inhibitor indicated for patients with CML or Ph+ ALL that is resistant or
intolerant to prior tyrosine kinase inhibitor therapy, including those with the T315I mutation.
Colony-Stimulating Factors
Class Summary
Colony-stimulating factors (CSF) act as hematopoietic growth factors that stimulate THE
development of granulocytes. These agents are used to treat or prevent neutropenia when patients
receive myelosuppressive cancer chemotherapy and to reduce the period of neutropenia that is
associated with bone marrow transplantation (BMT). Colony-stimulating factors are also used to
mobilize autologous peripheral blood progenitor cells for BMT and in management of chronic
neutropenia.
View full drug information
Filgrastim (Neupogen)
Filgrastim is a granulocyte colony-stimulating factor (G-CSF) that activates and stimulates the
production, maturation, migration, and cytotoxicity of neutrophils.
View full drug information
Pegfilgrastim (Neulasta)
Pegfilgrastim is a long-acting filgrastim created by the covalent conjugate of recombinant G-CSF
(ie, filgrastim) and monomethoxypolyethylene glycol. As with filgrastim, this agent acts on
hematopoietic cells by binding to specific cell surface receptors, thereby activating and
stimulating production, maturation, migration, and cytotoxicity of neutrophils.
Antimicrobials
Class Summary
Prophylactic antimicrobial drugs are given to prevent infection in patients receiving
chemotherapy.
View full drug information
Trimethoprim-sulfamethoxazole (Septra, Bactrim)
Trimethoprim-sulfamethoxazole (TMP-SMZ) inhibits bacterial growth by inhibiting the
synthesis of dihydrofolic acid. All immunocompromised patients should be treated with TMP-
SMZ to prevent Pneumocystis carinii pneumonia (PCP).
Antifungals
Class Summary
These agents may change the permeability of the fungal cell, resulting in a fungicidal effect.
View full drug information
Nystatin
Nystatin is used to prevent fungal infections in mucositis. This agent is a fungicidal and
fungistatic antibiotic from Streptomyces noursei that is effective against various yeasts and
yeastlike fungi. Nystatin acts by changing the permeability of the fungal cell membrane after
binding to cell membrane sterols, causing cellular contents to leak.
Treatment with this agent should continue until 48 hours after the symptoms disappear. Nystatin
is not substantially absorbed from the gastrointestinal tract.
View full drug information
Clotrimazole
Clotrimazole may be used instead of nystatin to prevent fungal infections. It is a broad-spectrum
antifungal agent that inhibits yeast growth by altering cell membrane permeability, causing death
of fungal cells.
View full drug information
Itraconazole (Sporanox)
Itraconazole has fungistatic activity and is used to prevent fungal infections in high-risk patients.
This drug is a synthetic triazole antifungal agent that slows fungal cell growth by inhibiting
CYP-dependent synthesis of ergosterol, a vital component of fungal cell membranes. The
bioavailability of this drug is greater in the oral solution compared with the capsule formulation.
Vous aimerez peut-être aussi
- Acute Lymphocytic LeukemiaDocument12 pagesAcute Lymphocytic Leukemiajustin_sanePas encore d'évaluation
- Gastrointestinal System Disorders NCLEX Practice QuizDocument82 pagesGastrointestinal System Disorders NCLEX Practice QuizZhailyn Joy DumlaoPas encore d'évaluation
- Case Study - Incomplete Abortion Related To APSDocument8 pagesCase Study - Incomplete Abortion Related To APSRomeo ReyesPas encore d'évaluation
- CASE STUDY: B-ALL WITH APLASTIC ANEMIADocument15 pagesCASE STUDY: B-ALL WITH APLASTIC ANEMIAShakira HashimPas encore d'évaluation
- Preeclampsia Risk Factors and Maternal-Fetal ComplicationsDocument18 pagesPreeclampsia Risk Factors and Maternal-Fetal ComplicationsMary BlancoPas encore d'évaluation
- Hirschprungs DiseaseDocument26 pagesHirschprungs DiseaseAndrian PramanaPas encore d'évaluation
- Assisting: Venous Cut DownDocument4 pagesAssisting: Venous Cut DownJimnah Rhodrick BontilaoPas encore d'évaluation
- GRP 20 Final Abscess Case StudyDocument14 pagesGRP 20 Final Abscess Case StudyBorja, Kimberly GracePas encore d'évaluation
- Idiopathic Thrombocytopenic Purpura (ITP)Document20 pagesIdiopathic Thrombocytopenic Purpura (ITP)saiibelieves0% (1)
- Pathophy - Nephrotic SyndromeedDocument1 pagePathophy - Nephrotic Syndromeedianecunar100% (1)
- Ulcerative ColitisDocument18 pagesUlcerative ColitisHoussein EL HajjPas encore d'évaluation
- CyclosporineDocument3 pagesCyclosporineraki9999Pas encore d'évaluation
- Rabies: Ragina AguilaDocument55 pagesRabies: Ragina AguilaCharles Lester AdalimPas encore d'évaluation
- Pathophysiology of DMDocument4 pagesPathophysiology of DMNicole Louise N. VillanuevaPas encore d'évaluation
- MedSurg Notes - Cancer of The LiverDocument2 pagesMedSurg Notes - Cancer of The LiverMae CeaesarPas encore d'évaluation
- Pathophysiology of Ureteral CalculiDocument14 pagesPathophysiology of Ureteral CalculiEdmel Pamplona DuquesaPas encore d'évaluation
- The Painless Abdominal Mass: Morning Report December 2010Document14 pagesThe Painless Abdominal Mass: Morning Report December 2010Emily EresumaPas encore d'évaluation
- Purpura and Petechiae: Symptoms and Types of Idiopathic Thrombocytopenic Purpura (ITPDocument7 pagesPurpura and Petechiae: Symptoms and Types of Idiopathic Thrombocytopenic Purpura (ITPMarie Joe AbainzaPas encore d'évaluation
- Drug StudyDocument5 pagesDrug StudyJanine Erika Julom BrillantesPas encore d'évaluation
- The Child With Hematologic DisordersDocument149 pagesThe Child With Hematologic DisordersNics FranciscoPas encore d'évaluation
- Spontaneous AbortionDocument8 pagesSpontaneous Abortionsaber_fate_11Pas encore d'évaluation
- Rare Muscle Diseases: PM and DMDocument2 pagesRare Muscle Diseases: PM and DMintrovoyz041Pas encore d'évaluation
- Pathophysiology of DiarrheaDocument3 pagesPathophysiology of DiarrheaFathur RahmatPas encore d'évaluation
- Gastric CancerDocument7 pagesGastric CancerMicah PingawanPas encore d'évaluation
- Bea-Case StudyDocument21 pagesBea-Case Studybea pegadPas encore d'évaluation
- Idiopathic Thrombocytopenic PurpuraDocument8 pagesIdiopathic Thrombocytopenic PurpuraMonette Abalos MendovaPas encore d'évaluation
- Management For Acute Lymphocytic LeukemiaDocument3 pagesManagement For Acute Lymphocytic LeukemiamarivohPas encore d'évaluation
- Nursing Diagnosis for Family AssessmentDocument106 pagesNursing Diagnosis for Family AssessmentShaira Ann CalambaPas encore d'évaluation
- Acute Glomerulonephritis: What is it and What Causes itDocument12 pagesAcute Glomerulonephritis: What is it and What Causes itSara Sonnya Ayutthaya NapitupuluPas encore d'évaluation
- Hepatitis VirusDocument37 pagesHepatitis Virusapi-19916399Pas encore d'évaluation
- Aklan State University Nursing Readings on Pyloric StenosisDocument5 pagesAklan State University Nursing Readings on Pyloric Stenosisensoooooooooo100% (1)
- Paroxysmal Nocturnal Hemoglobinuria Case StudyDocument87 pagesParoxysmal Nocturnal Hemoglobinuria Case Studyrachael100% (4)
- Anemia Pathophysiology All in 1 by Francis OliverosDocument3 pagesAnemia Pathophysiology All in 1 by Francis Oliverosfrancis00090Pas encore d'évaluation
- Vii. Pathophysiology A. AlgorithmDocument2 pagesVii. Pathophysiology A. AlgorithmJonna Mae TurquezaPas encore d'évaluation
- Abdominal Trauma Signs, Symptoms and Nursing CareDocument24 pagesAbdominal Trauma Signs, Symptoms and Nursing CareSurgeryClassesPas encore d'évaluation
- Co AmoxiclavDocument1 pageCo AmoxiclavMuhammad ArsalanPas encore d'évaluation
- Are Viruses Living or Non-Living Organisms?Document8 pagesAre Viruses Living or Non-Living Organisms?Sydney Cloyce NagalPas encore d'évaluation
- HPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDocument21 pagesHPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDaffa IbnurasyPas encore d'évaluation
- RevalidaDocument5 pagesRevalidaHawkins FletcherPas encore d'évaluation
- Pathophysiology of Malaria: How Parasite Infection Affects the BodyDocument20 pagesPathophysiology of Malaria: How Parasite Infection Affects the Bodymelia100% (1)
- Acute Disease Case Study: Metabolism - HypothermiaDocument8 pagesAcute Disease Case Study: Metabolism - HypothermiaRegina PerkinsPas encore d'évaluation
- Acute Cholecystitis SeminarDocument42 pagesAcute Cholecystitis SeminarNatnaelPas encore d'évaluation
- PPH Introduction 1Document95 pagesPPH Introduction 1regine maePas encore d'évaluation
- Epidemiology, Pathogenesis, and Pathology of NeuroblastomaDocument21 pagesEpidemiology, Pathogenesis, and Pathology of NeuroblastomaHandre PutraPas encore d'évaluation
- CholelitiasisDocument42 pagesCholelitiasisEdwin YosuaPas encore d'évaluation
- IntussusceptionDocument33 pagesIntussusceptionNovendi RizkaPas encore d'évaluation
- Biliary AtresiaDocument8 pagesBiliary AtresiaBrooke MauriPas encore d'évaluation
- Pamantasan NG Cabuyao College of Health Allied Sciences College of NursingDocument43 pagesPamantasan NG Cabuyao College of Health Allied Sciences College of NursingSofea MustaffaPas encore d'évaluation
- Testicular Cancer Nursing ManagementDocument33 pagesTesticular Cancer Nursing ManagementCheeBrendaPas encore d'évaluation
- Cholecystitis Litiasis EctomyDocument23 pagesCholecystitis Litiasis EctomyTimothy WilliamsPas encore d'évaluation
- CA Intro DXTX PDFDocument121 pagesCA Intro DXTX PDFwokorowPas encore d'évaluation
- OUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisDocument20 pagesOUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisMikaCasimiroBalunanPas encore d'évaluation
- Tenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleDocument12 pagesTenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleBagusHibridaPas encore d'évaluation
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutD'EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutÉvaluation : 5 sur 5 étoiles5/5 (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Myeloid LeukemiaDocument8 pagesMyeloid LeukemiaMiriam AguilarPas encore d'évaluation
- Why Your DNA Isn't Your Destiny: Biopsychology Comprehension QuestionsDocument6 pagesWhy Your DNA Isn't Your Destiny: Biopsychology Comprehension Questionspiccolo23Pas encore d'évaluation
- The 2016 WHO Classification andDocument11 pagesThe 2016 WHO Classification andIsmi RachmanPas encore d'évaluation
- Who Diagnostic Criteria MyelofibrosisDocument1 pageWho Diagnostic Criteria Myelofibrosispieterinpretoria391Pas encore d'évaluation
- Focus On Myeloproliferative Diseases and Myelodysplastic SyndromesDocument6 pagesFocus On Myeloproliferative Diseases and Myelodysplastic SyndromesBopiyudha bopiyudhaPas encore d'évaluation
- Approach To Anemia: - Reticulocyte Count Is Most Important TestDocument15 pagesApproach To Anemia: - Reticulocyte Count Is Most Important TestJanella SuertePas encore d'évaluation
- Medicine Triple ADocument186 pagesMedicine Triple AAnup Bhele100% (1)
- 291 - 41st Annual Intensive Review of Internal Medicine Post TestDocument14 pages291 - 41st Annual Intensive Review of Internal Medicine Post TestKendra GreyPas encore d'évaluation
- About Myelodysplastic Syndromes: Overview and TypesDocument12 pagesAbout Myelodysplastic Syndromes: Overview and TypesAulya ArchuletaPas encore d'évaluation
- Primary MyelofibrosisDocument82 pagesPrimary MyelofibrosisEmmanuel EkanemPas encore d'évaluation
- Comparison of Platelet Count Methods in The Presence of Interfering Substances - Marionneaux 2010Document1 pageComparison of Platelet Count Methods in The Presence of Interfering Substances - Marionneaux 2010Steven Marionneaux, MS, MT(ASCP)Pas encore d'évaluation
- Acute Myeloid LeukemiaDocument33 pagesAcute Myeloid LeukemiardLuis1Pas encore d'évaluation
- AMLDocument19 pagesAMLquerokeropi100% (1)
- Up To Date LMMCDocument23 pagesUp To Date LMMCLuciano LaranjeiraPas encore d'évaluation
- Myelodysplastic SyndromesDocument38 pagesMyelodysplastic SyndromesMohamad AttiaPas encore d'évaluation
- Biology of Blood and Marrow Transplantation: PediatricDocument8 pagesBiology of Blood and Marrow Transplantation: PediatricMichael John AguilarPas encore d'évaluation
- Acute Myeloid Leukemia With Myelodysplasia RelatedDocument6 pagesAcute Myeloid Leukemia With Myelodysplasia RelatedAgus WiniPas encore d'évaluation
- Chapter 13 Neoplastic Proliferations of White CellsDocument16 pagesChapter 13 Neoplastic Proliferations of White CellsOmar100% (1)
- Natural Gas Condensate MSDSDocument15 pagesNatural Gas Condensate MSDSHafiz AkhtarPas encore d'évaluation
- How I Investigate Basophilia in Daily Practice: Joffrey Feriel - François Depasse - Franck GenevièveDocument9 pagesHow I Investigate Basophilia in Daily Practice: Joffrey Feriel - François Depasse - Franck GenevièveMarina TaveiraPas encore d'évaluation
- Vox Sanguin Mei 22 - OptDocument146 pagesVox Sanguin Mei 22 - OptRika DatuadamPas encore d'évaluation
- PDF 20220916 142849 0000-1Document20 pagesPDF 20220916 142849 0000-1Darman SyahPas encore d'évaluation
- 505 FullDocument11 pages505 FullRolando Jose CastilloPas encore d'évaluation
- CitologieDocument14 pagesCitologieAlexandra CrisanPas encore d'évaluation
- How we manage immune thrombocytopenia in the elderlyDocument13 pagesHow we manage immune thrombocytopenia in the elderlyAngela Hilda Villanueva SocolaPas encore d'évaluation
- New Drug 2009Document24 pagesNew Drug 2009NAVNEET BAGGAPas encore d'évaluation
- Bone Marrow Puncture & Transplantation: Prof. Dr. Dr. Adi Priyana SPPK Bag. Patologi KlinikDocument15 pagesBone Marrow Puncture & Transplantation: Prof. Dr. Dr. Adi Priyana SPPK Bag. Patologi Klinikelsie levina aisha lourentPas encore d'évaluation
- Myelodysplastic Syndrome: DR Mika Lumbantobing, Sppd-KhomDocument20 pagesMyelodysplastic Syndrome: DR Mika Lumbantobing, Sppd-KhomsehatkabauPas encore d'évaluation
- HEMA 2 - Midterm Topic 3 - Anemia of Bone Marrow DisorderDocument10 pagesHEMA 2 - Midterm Topic 3 - Anemia of Bone Marrow DisorderLowenstein JenzenPas encore d'évaluation
- AnemiaDocument51 pagesAnemiaAravind A SPas encore d'évaluation