Académique Documents
Professionnel Documents
Culture Documents
Ant 328 Final Paper
Transféré par
mmanyapuCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ant 328 Final Paper
Transféré par
mmanyapuDroits d'auteur :
Formats disponibles
Manyapu 1
Mallika Manyapu
ANT 328
04/22/14
Title: Skirts in the Doctors Office: How Women Physicians Live in a Male-Dominated Field
Introduction: Topic and Why?
I was standing in small kitchen apartment in my uncomfortable black shoes,
uncomfortable skin-colored tights, and uncomfortable plain, black interview suit. My normally
unruly hair was neatly pulled back, my nails colorless, and my makeup absolutely minimal. This,
I was told, was how female medical school interviewees dress to impress. In my extensive
preparations for medical school interviews, I gathered all kinds of advice, from you must wear a
pant-suit to establish yourself, to you should wear a skirt in case you have some old misogynist
interviewer. While I am in no way a fashionista, I do enjoy the occasional splurge of color and
artistic self-representation through clothes and make up. What does this masculine uniform say
to young aspiring women physicians? Do we have to dress like men to be respected, or is there
no hope for the pervasive sexism and traditionalism?
While I was not so sheltered and naive to believe that women physicians live the same
kind of life as male physicians, I did begin to wonder how women physicians are treated today in
a still highly masculine field. If our appearance is placed under such scrutiny even before
reaching medical school, what does this suggest about current state of affairs of female
physicians? While men also have a uniform of sorts for interviews and within the medical field,
it seemed to me that the female uniform was even more conservative, strict, and masculine. As a
future physician, this topic was of particular interest to me. For months, people would ask me
why do you want to be a doctor? However, it was more surprising to hear the skepticism and
Manyapu 2
slight disapproval when other older females questioned my career choice. Over the course of my
medical school interview season, I discovered that while many physicians experience a certain
degree of frustration and tiredness with the job, women physicians sometimes experience this to
a higher degree. From casual conversations about lack of sleep, constant planning ahead, and a
perpetual to-do list, many of the women physicians I encountered were happy, but not ecstatic
about the growing number of women in the medical field. Thus, with these contextualization
cues, I set out to find out what female physicians deal with on a daily basis.
Background Research:
For years, women have been under-represented or under-appreciated in the field of
medicine largely because of the barriers in education and social standing. However, with recent
social changes over the past few decades, women have made a significant impact in the medical
field in treatments, healthcare delivery, research, and more (1, 4, 7). Despite these advancements,
however, many women and young females still feel some sting of stereotypes and social
expectations in certain environments, such as in interactions with unsuspecting patients who did
not expect a female physician, patriarchal driven research symposiums, white coat ceremonies
and in daily lunch conversations with colleagues (6).
According to the American Medical Womens Association (AMWA), the number of
women in the physician workforce has doubled over the past twenty years (2, 5). From 7 percent
in 1970 to near 25-30 percent in 2013, the growth rate for female physicians has been three times
that of the general physician population. This increase is evident even in the student population,
with most graduating classes from medical schools consisting of approximately half women (5).
However, there are still some apparent discrepancies between females and males within the
medical field, most evident by differences in compensation, number of hours worked, job status,
Manyapu 3
participation in academic research, and approach to patient care (1, 2, 5). For example, compared
to men, women faculty holding full professorships in medical schools is around 10 percent
compared to 30 percent of men holding full professorships (3, 4). This trend is persistent through
academic medicine, with fewer women publishing journal articles, fewer women advancing to
academic senior ranks, and female medical school faculty receiving lower compensation
compared to their male co-workers (4).
A recent survey conducted by the Physician Compensation Survey showed that male
physicians make an average 40 percent more than female physicians. There are several reasons
for why female physicians earn and achieve less than their male counterparts. One reason women
are not as involved in academic medicine as men is because of their specialty choices in mostly
primary care fields, including general practitioner, pediatrics, family medicine, psychiatry, and
internal medicine. In general, physicians in these fields focus less on academic medicine
involving research, interdisciplinary field collaboration, and treatment trials, and thus by default,
women are often excluded from such academic discussions. In addition, these physicians make
significant less income than highly specialized fields such as surgery, cardiology, and radiology,
placing physicians in these fields at a lower tier (3). Due to a variety of unproven hypotheses,
women constitute much of the primary care work force compared to men. Furthermore, female
physicians spend more time with their patients than male doctors do, contributing to a smaller
patient pool in comparison (5).
In addition to these issues, there are three key barriers preventing women from rising
through the ranks of the medical field. The first issue that women face is the traditional attitude
that prescribes women as responsible for housework, raising children, and providing care to the
family as a whole (3, 4, 6). Although this traditional gender role has morphed and changed much
Manyapu 4
over the years, there is still a pervasive, often assumed, idea that women know more about
raising family and running a house, and thus, are expected to fulfill those roles. This family role
can often make devoting time and energy to other avenues such as research or teaching much
more difficult. In contrast, male physicians are often encouraged to dedicate their lives to their
careers and thus move through the social and political spheres with much more ease (6).
The second factor contributing to womens differential success in the medical field is
unspoken and subtle hints of sexism (4, 6). While sexism has proven to impact training,
recruitment, promotion, management, and the routine work of female physicians, a 2010 survey
by the AMWA showed that women frequently experience sexist behavior with lack of
recognition, disrespect, and inappropriate sexual behavior and language. While these behaviors
have improved over the past few decades, the underlying ideas of sexism still persist and
negatively affect female physicians in their attempts to achieve success and status (4).
The third and most prominent issue that I myself have experienced as a pre-medical
student is the lack of female mentors for women. It is well known that advancement in any career
is heavily dependent on having an effective mentor and social capital force (4, 6). However,
because the number of working women has only slowly increased, there is a definite lack of
female mentors. Women in medicine have unique challenges from balancing home and work life
to interacting with certain patients that only someone with those experiences can adequately
advise. With this, the general lack of experience in the medical field that women sometimes face
compromise the issue further (6).
All of these issues affect women physicians ability to advance through the medical
sphere, manifested through unequal pay, inadequate access to academic resources, and a general
Manyapu 5
lack of experience in the medical system and structure. Besides these extrinsic factors, there is
also some evidence for differential treatment on the patient-doctor level.
Methods:
I originally wanted to focus my research and observations on the experience of minority,
female physicians. While partly for personal reasons, I was also curious about how minority,
female physicians lived with not just one differential aspect, but two: gender and ethnicity.
However, this topic proved difficult to pursue for a variety of reasons. For one, it was difficult
for me to find a female minority physician within the Emory area. Since I do not have a car for
easy transportation, I was limited to this particular area. While countless female minority
physicians do exist, I am sure, the few I approached were either uninterested or too busy to
indulge in my research. Whether the lack of interest stemmed from a busy schedule or hesitation
with the topic, I can only hypothesize. In addition to logistical issues, I also found it difficult to
differentiate between confounding variables of gender and ethnicity/race. Often times, I realized
that the differential treatment could be attributed to either gender or ethnicity/race, and analyzing
which variable came first was near impossible. I saw that real-world social and professional
interactions involve a variety of reactions that influence one another, including gender,
race/ethnicity, experience, language, accents, and location, to name just a few of what I
witnessed on frequent basis in one department of an outpatient clinic.
Consequently, with the limited amount of time I had, I chose to focus only on gender. I
shadowed one female, white American doctor, at Emorys Childrens Healthcare of Atlanta
Childrens Center and interviewed two American-born, second-year fellows. All three doctors
worked primarily in the Gastroenterology Department. I followed and observed Dr. Bethany
Manyapu 6
Smith*
1
in her clinic rotations on three separate occasions on Wednesday afternoons from
1:00PM-5:00PM, and interviewed the two fellows, Sameera Sana* and Talia Holmes*, Friday
afternoons after their own respective clinic rotations. Here, I will provide a brief background
about each person.
Dr. Smith is a middle-aged, born and raised Southern woman who has been practicing
medicine for over twenty years. She has been practicing as a part of Emory healthcare since
completing her residency at Emory and has co-authored two research publications. Dr. Smith has
two children, a 22-year-old son and an 18-year-old daughter. While other co-workers have
mentioned to me before that Dr. Smith has been married, I am not sure she is now. There is no
ring on her finger, and I did not receive explicit information suggesting she is still married.
Dr. Sana is an American-raised, born-in Pakistan-woman in her early thirties finishing up
her last year of a pediatric gastroenterology fellowship. She is married, but her husband lives in
Boston. Originally from the Northeast, Dr. Sana has been at Emory for the past two years.
Dr. Holmes is also an American-raised woman in her early thirties. While her parents
were originally from Russia, Dr. Holmes does not identify much with her Russian roots. She is
married and has a two-year-old son. Shes in her second year of medical fellowship in pediatric
gastroenterology and lives approximately half an hour away from work.
Observations:
As a pre-med student, I have had experience shadowing doctors, nurses, physician
assistants, and emergency medical technicians in various environments. However, this time I
approached my shadowing from an anthropological and sociological point of view. Instead of
paying attention to the medical jargon that was rapidly exchanged between medical
1
Starred names are pseudonyms.
Manyapu 7
professionals, I detailed how the information was being communicated and if there were
differences between male and female co-workers. Furthermore, instead of focusing on how
physicians interacted with patients, I focused on how patients treated physicians.
A typical clinic day began around 1:00 PM on a weekday afternoon, with research
coordinators, nurses, and physicians congregated in a relatively small office room sequestered
among patient rooms and open to the clinic. There were not enough chairs for every person in the
room, so I often pressed myself up against the wall and simply observed and followed Dr. Smith
without discussion. The names of all the patients who are being seen in a day are written on a
white board, and then divided among the two-three physicians, two-three nurses, and two-three
research coordinators present. At least one person from each category sees one patient. In this
particular clinic, all the nurses, one of the coordinators, and one other physician are female. This
leaves one additional male coordinator and two male physicians at any given time. Before
walking into a patients room, Dr. Smith would go over the paper chart and discuss the patient
out loud with either a nurse or another physician. Dr. Smith told me this is to refresh herself on
each patients particular case, as often she only sees a particular patient only two or three times a
year.
On one particular clinic day, a male doctor, Dr. K*, and Dr. Smith were discussing the
merits of continuing a certain treatment for a more difficult patient. The patient was technically
Dr. Smiths, but she had asked Dr. K for his input on this case previously. Their conversation
went as follows:
Dr. S: Tim* was highly resistant to (insert drug here). He does not like needles,
and this treatment requires bi-weekly shots.
Manyapu 8
Dr. K: Yes, but his disease has progressed too far for any other option to be even
plausible. If you see his x-rays and pathology, he will respond to only this drug.
Dr. S: True. I will just prescribe him this drug and hopefully, they wont cause me
too much trouble.
Dr. K: If you need help convincing, let me know.
Most conversations proceeded in some similar fashion. The conversation showed subtle
signs of hierarchy in that Dr. Ks opinions were valued more than Dr. Smiths. More so, whether
intentional or unintentional, Dr. K implied that Dr. Smith might not be able to persuade her
patient to take the appropriate drug. While on the surface, this may be because Dr. K is more
experienced, I believe the difference between Dr. K and Dr. Smith is further complicated by
gender. This conversation is just an excerpt of everyday conversations where female physicians
consulted a male physician and then ultimately agreed with the male physician. In contrast, if
there were no other physicians in the room, Dr. Smith would talk to the nurses about the case
history in a more authoritative tone. These conversations were often the nurses confirming or
denying what Dr. Smith said out loud. For example:
Dr. S: Cindy* was having severe stomach pains two weeks ago, when after ER
admittance, a scope showed bowel obstruction located approximately in the upper
colonic region.
Nurse: Yes, the scope also showed scar tissue in the lower tract regions.
Dr. S: In which, the lab reports confirmed that she had Ulcerative Colitis. What
drug did they start her on?
Nurse: Humira.
Manyapu 9
In between patients and in small openings of time, discussions would range from a recent
research article someone had read to what sport his/her child was attempting this time. In these
conversations, I noticed that there was a more academic tone to interactions between male
physicians while female physicians discussed the home life, as well. Dr. Smith, who has a
twenty-two year old son in college, was discussing his job prospects with another female
physician who also has a son. In contrast, her conversations with her male co-workers often
revolved around academic medicine. The conversations topics for female-female interactions,
and even for male-male interactions, showed a wider range than the male-female interactions.
This carried over in most aspects of medicine such as in research symposiums, lunch breaks, and
research meetings. For instance, in the few research symposiums and meetings I have attended
with Dr. K and Dr. Smith, I rarely saw a female lead the event. There were female physicians
present, and even some who participated in active discussions, but a male physician usually
began the conversation and ended the conversation. It almost seemed like the female physicians
were participant observers and not necessarily integral to the discussions.
When I asked Dr. Smith if she enjoys research, she simply stated, Usually. Its all very
tedious and time consuming, sometimes. Dr. Smith has co-authored two papers, in contrast to
Dr. K who has co-authored over ten journal articles. I remember on one occasion, Dr. K was
discussing with Dr. Smith a potential new research idea for one of his undergraduate students,
when Dr. Smith almost bitterly said, You know, you stole my patient for that last paper you
published. To which, Dr. K replied most apologetically, Oh really? You were supposed to be
an author on that paper as well On these occasions, Dr. Smith would dismiss the comment
and continue conversing about whatever previously discussed topic. While I personally believe
Dr. K did not intentionally leave Dr. Smith out of the paper, it is important to note that the only
Manyapu 10
other person he made sure to include in the paper was a male physician. Dr. Smith could have
argued for her name and reputation, but dismissed the matter as futile and commonplace. This
implies that such occurrences have happened before, where the female physician is forgotten in
academic medicine and related discussions. I see this as a veiled level of sexism.
In patient rooms, Dr. Smith encountered a variety of patients. Emorys patient pool is
quite diverse, with Atlanta metro families able to afford Emory healthcare coupled with rural
families afflicted with a rare disease that Emory specialists are best equipped to handle. Some
patients responded quite excitedly and warmly whenever Dr. Smith walked into the room.
Sometimes these patients families also shared the same enthusiasm. Dr. Smith would precede
her medical questions with casual conversation topics such as school, work, or a certain event
relevant to the patient. On one occasion, however, Dr. Smith was wary to enter the patient room.
She asked one of the male coordinators to talk with the patients family first, before she entered
the room. At first, I did not quite understand why, but upon entering the room later I could see
and feel the tension. The patient was a fourteen-year-old girl, present with her mother and father.
The family hailed from a small town in Georgia and, I was later told, owned a large farm estate.
The father did most of the talking, describing their daily activities, diet, etc. Neither mother nor
daughter gave much input unless specifically prompted by Dr. Smith. When Dr. Smith was
discussing treatment options, the father loudly contested most of the options as tedious,
expensive, or difficult. It was only with the male coordinator verbally supporting Dr. Smiths
suggested treatments and advice was Dr. Smith able to convince the patients father of the
appropriate treatment. After walking out of the room, Dr. Smith audibly sighed and absent-
mindedly shook her head in frustration. I later asked the male coordinator, who happens to be a
good friend and mentor of mine, what the background story for this particular patient was. He
Manyapu 11
shrugged and simply stated, He doesnt really listen to Dr. Smith in general. While it was
never explicitly stated, I inferred that the patients father prescribes to traditional gender roles
both at home and in public.
While I was not able to shadow the fellows on their clinic rounds, I did converse with
them about their experiences as female physicians and what they foresee for the future. Both Dr.
Sana and Dr. Holmes began with explicitly stating that they do not feel marginalized in any
shape, way, or form. In fact, Dr. Sana explained, The differences between female and male
physicians are more a product of old values. Sometimes I see the difference between an old
professor and a newer, younger colleague, but even that is really subtle. She further explained
this by citing a time when she was sharing the rough draft of her now-published paper to
colleagues and professors. She had sent it to two of her mentors, one female and one male. Her
male mentor critiqued and criticized much more than her female mentor did. She said, I
remember his email came back with a lot more red marks than her email. But I attribute this to
him being more experienced, and in the end, his harsh feedback was really helpful. Dr. Sana did
state, however, that she believes she is so successful right now because she has not had to come
home to children or a husband for the past two-three years. Although she finds it difficult to be in
a long-distance relationship, she stated that this gives her much more free time.
Dr. Holmes, who took a break between her residency and fellowship to give birth to her
now two-year old son, stated that she is often tired by Friday with taking care of her child,
working long hours, and being a fellow. She credits her mentors for helping her through the
process, and her co-workers for helping with the research and practicing side. She said, I wont
be a first author for a while probably, but it definitely does help to have someone do the work
with you. Dr. Holmes and one of her co-workers are splitting the tasks for research so that she
Manyapu 12
does not have to shoulder the entire burden of conducting the research and writing the paper. Dr.
Holmes further said that although she can see how being a woman physician is difficult with
balancing all the tasks at hand, working with more traditional male counterparts, she thinks that
her generation is changing the face of medicine all together. Everything is more collaborative
now than in previous decades. Theres really no rhyme or reason to discredit the female voice
anymore.
While both Dr. Holmes and Dr. Sana agreed that there is no way to completely eliminate
differences between female and male physicians, they each believe that in the coming years, the
traditional gender roles will be even more blurred.
Discussions:
The women I interacted with, Dr. Smith, Dr. Holmes, and Dr. Sana, always appeared
impeccably clean, professional, and put together albeit in varying ways. For instance, I rarely
saw Dr. Smith without makeup, a female flattering suit, or heels. On clinic days, I noticed little
hints of personality in her jewelry and color choice combinations. In contrast, Dr. Holmes and
Dr. Sana wore minimal makeup, and what I believe to be, more comfortable clothes that rarely
included heels or stiff pantsuits. In fact, co-workers have commented to me that Dr. Sana always
had the most comfortable and fashionable flats, while Dr. Holmes worked the indie and long
free-flowing skirts. These differences in appearance show the growing changes and trends that
female physicians face today.
Nevertheless, from these experiences, I have seen that the glass ceiling that was present
in past decades is still present today. From the unequal access to resources, significant
discrepancy in pay, and limited representation in academic areas, women physicians share issues
of pressurized adherence to typical gender roles, sexism, and lack of experienced mentors. From
Manyapu 13
an observer point of view, I witnessed a slightly, lopsided communication between male
physicians versus female physicians, where female physicians were more likely to not only
consult a male physician, but were also more likely to agree with the male physician. In fact,
there was a slight hierarchy of opinion, with the male physicians thoughts nearly always prized
more than that of female physicians. In contrast, woman-to-woman physician interactions were
often more discussion based, with back-and-forth conversation. However, I believe this male-
weighted communication is not simply because of an inherent patriarchal structure, although that
does play a role. From my observations, it is clear that because women physicians are relatively
new to the academic and medical sphere, as a whole, and women physicians are more
inexperienced when compared to male physicians. In medicine, experience and knowledge is
perhaps the most important factor for advancement, higher compensation, and a renowned
reputation, since someone elses life is quite literally in his/her hands. Thus, it makes logical
sense for an inexperienced person to refer to a more experienced person. Unfortunately, this
perpetuates the cycle in such a way that almost inevitably places the woman physician at a lower
position than a male physician. The patriarchal structures that has been in place within the
medical field for decades have naturally placed women at a disadvantage with educational and
advancement opportunities. Thus, this poses an additional challenge for women physicians who
wish to break out and establish themselves as reputable and independent physicians. For women
who hold a vital familial role at home, whether as a mother or household caretaker or more,
breaking through the glass ceiling can come at a cost. While I do believe it is possible for women
physicians to have it all, a successful career and a family life, the current hierarchal structure
and high responsibility physicians possess make achieving both aspects challenging.
Manyapu 14
However, after speaking with representatives of a younger population of physicians, I see
a slowly changing trend among the fellows. The fellows have much more access to a wide
variety of mentors, from male to female, and of all ages. This makes it easier to establish a base
and connection among the academic world. Further, the two fellows I spoke with seem to be
relatively happy with their work and home life. While often tired and sometimes stressed, the
fellows attribute this more to the job itself than to being a woman in the field. I predict that the
next generation of American-raised female physicians will have been exposed to the possibilities
of a work-home balance and will be generally less tolerant of differential treatment. This leads
me to believe that these same physicians will stretch the cycle and push up against the glass
ceiling with greater numbers and force. Through this, there may be more evident equality
manifested through salary and status. While it will be challenging to change the culture among
patient-doctor relationships and co-worker interactions, there are also signs of progress that will
perhaps turn the tide with the increasing number of female physicians. The changes in daily
wardrobe manifest this progress. Why experts still recommend medical school interviewees to
cater to some of the old ways, I am not sure, but the professional and female wardrobe seems to
be slowly evolving. More so, the current incoming medical school student population is
approximately half female and half male according to USA News. Even in this small
gastroenterology department, there are three female physicians, four male physicians, three
female fellows, and three male fellows total. In addition, with the possibility of male physicians
becoming more invested at home, as well, there is hope yet for American female physicians.
Conclusion:
There are obviously many limitations to my study due to the short period time of the
research and exposure to only one small clinic office, one physician, and two fellows. It is
Manyapu 15
impossible to assume that my observations apply to every female physician in every doctors
office or hospital. My focus was on American-raised female physicians, a select population that
has experiences vastly different from the rest of the world. Further research could include a more
widespread observation of other clinical offices and for a longer period of time. In addition, I
believe it is important to note that age does play a factor. Because of the many technological,
political, social, and cultural transformations that have occurred even in the past ten years, there
will be varying experiences in the doctors office or hospital regardless of gender or
ethnicity/race. Furthermore, interviewing male physicians, of various ages, on what they
perceive the female physician life to be like would add to a further study.
Manyapu 16
References
1. Levinson, Wendy, Susan W. Tolle, and Charles Lewis. "Women in Academic Medicine." New
England Journal of Medicine 321.22 (1989): 1511-517.
2. Mcmurray, Julia E., Mark Linzer, Thomas R. Konrad, Jeffrey Douglas, Richard Shugerman,
and Kathleen Nelson. "The Work Lives of Women Physicians. Results from the Physician Work
Life Study." Journal of General Internal Medicine 15.6 (2000): 372-80.
3. Morantz-Sanchez, Regina Markell. Sympathy & Science: Women Physicians in American
Medicine. Chapel Hill: University of North Carolina, 2000.
4. Carr, Phyllis L. "Comparing the Status of Women and Men in Academic Medicine." Annals of
Internal Medicine 119.9 (1993): 908.
5. Rizvi, Rabab, Lindsay Raymer, Mark Kunik, and Joslyn Fisher. "Facets of Career Satisfaction
for Women Physicians in the United States: A Systematic Review." Women & Health 52.4
(2012): 403-21.
6. Rostami, Vida. "Women in Medicine." Women's Health Activist. N.p., 1 Nov. 2011. Web.
7. Tesch, B. J., H. M. Wood, A. L. Helwig, and A. B. Nattinger. "Promotion of Women
Physicians in Academic Medicine." Survey of Anesthesiology 39.5 (1995): 329.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Early Stages of Schizophrenia PDFDocument280 pagesThe Early Stages of Schizophrenia PDFJoão Vitor Moreira MaiaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Neuropsychiatry and Behavioral NeurologyDocument302 pagesNeuropsychiatry and Behavioral NeurologyTomas Holguin70% (10)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Alveolarosteitis Andosteomyelitis Ofthejaws: Peter A. KrakowiakDocument13 pagesAlveolarosteitis Andosteomyelitis Ofthejaws: Peter A. KrakowiakPam FNPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Use of A Modified Matrix Band Technique To Restore Subgingival Root CariesDocument6 pagesUse of A Modified Matrix Band Technique To Restore Subgingival Root CariesDina NovaniaPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Coping With Addiction: 6 Dysfunctional Family RolesDocument4 pagesCoping With Addiction: 6 Dysfunctional Family RolesMy LanePas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Loeffler SyndromeDocument19 pagesLoeffler SyndromeYama Sirly PutriPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- JWC Convatec Wound-Hygiene-28pp 14-Feb CA Web-LicDocument28 pagesJWC Convatec Wound-Hygiene-28pp 14-Feb CA Web-LicAjeng Kania100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
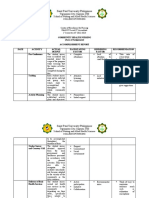
- Group 4 - Accomplishment ReportDocument5 pagesGroup 4 - Accomplishment ReportMa. Millen PagadorPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- 504 Morocco Fact SheetsDocument3 pages504 Morocco Fact Sheetsopiakelvin2017Pas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Disorders of The Upper Respiratory TractDocument3 pagesDisorders of The Upper Respiratory TractJannelle Dela CruzPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Riddle of DeathDocument2 pagesRiddle of DeathReka182Pas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Handicapped ChildrenDocument36 pagesHandicapped ChildrenAbdur RehmanPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Johansen HutajuluDocument25 pagesJohansen HutajuluRSUD DoloksanggulPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- SDF Bendit - Young - WebDocument10 pagesSDF Bendit - Young - Webmadhu kakanurPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- 2019 Autogenous Soft Tissue Grafting For Periodontal and Peri-Implant Plastic Surgical ReconstructionDocument8 pages2019 Autogenous Soft Tissue Grafting For Periodontal and Peri-Implant Plastic Surgical Reconstructionayu calisthaPas encore d'évaluation
- Secondary Health 7 Q4 Module4Document9 pagesSecondary Health 7 Q4 Module4Rona RuizPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Bicipital TendonitisDocument2 pagesBicipital TendonitisJ Cheung100% (2)
- Diarrhea Nursing Care PlanDocument2 pagesDiarrhea Nursing Care PlanKrizha Angela NicolasPas encore d'évaluation
- Gerontik Setelah UtsDocument93 pagesGerontik Setelah UtsNidaa NabiilahPas encore d'évaluation
- Tubercular Meningitis in Children: Grisda Ledivia Lay, S.Ked 1508010038 Pembimbing: DR - Donny Argie, SP - BSDocument12 pagesTubercular Meningitis in Children: Grisda Ledivia Lay, S.Ked 1508010038 Pembimbing: DR - Donny Argie, SP - BSAulia PuspitaPas encore d'évaluation
- Herbal Its Project Biology.....Document52 pagesHerbal Its Project Biology.....MISHAPas encore d'évaluation
- Lansia Di Panti Jompo USADocument10 pagesLansia Di Panti Jompo USADWI INDAHPas encore d'évaluation
- DI Abdomen P 001 015 BeginingDocument15 pagesDI Abdomen P 001 015 Beginingtudoranluciana1Pas encore d'évaluation
- MCQ Immunology BasicDocument71 pagesMCQ Immunology BasicMatthew HallPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Aplikasi Sim Dalam Asuhan KeperawatanDocument14 pagesAplikasi Sim Dalam Asuhan KeperawatanCitra Puspita SariPas encore d'évaluation
- Temporomandibular Joint Disorders: Coverage RationaleDocument14 pagesTemporomandibular Joint Disorders: Coverage RationaleVitalii RabeiPas encore d'évaluation
- Gnadia Pasandidega1Document2 pagesGnadia Pasandidega1Craig DavisPas encore d'évaluation
- SMNR - 4... Wound HealingDocument62 pagesSMNR - 4... Wound HealingDrAmar GillPas encore d'évaluation
- SalmonellaDocument103 pagesSalmonellabrucella2308Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Mariam Burchuladze: Group 7 / Reflection EssayDocument1 pageMariam Burchuladze: Group 7 / Reflection EssayMariam BurchuladzePas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)