Académique Documents
Professionnel Documents
Culture Documents
Kidney Disease: Underwriter Focus
Transféré par
Bryan Mae H. DegorioCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Kidney Disease: Underwriter Focus
Transféré par
Bryan Mae H. DegorioDroits d'auteur :
Formats disponibles
Apollo Bramwell Nursing School
Moca, Mauritius
Medical Underwriter
Kidney Disorders: Underwriter Focus
Disorders Risk Factors Diagnostics Treatment of Choice Complications Prognosis
KIDNEY
STONES
1. Gender and Age:
Male: 2X more
common, inc at 40-70
y/o
Female: risk peaks @
50 y/o
2. Family Hx
2X the risk
3. Obesity and weight
gain:
Higher BMI and weight
increases the risk
4. Lifestyle:
Low H2O intake
High protein and
calcium
athletes
5. Pre-Existing medical
Conditions
Gout- uric acid stone
HPN- 3X the risk
UTI- struvite stone
Hyperparathyroidism
Imaging Technique:
1. CT scan- the best method in diagnosing
renal stone
Plain- No special prep
Contrast- fasting 4 hours before
2. X-ray- standard x-ray for kidney, ureters
and bladder.
Can detect stones but usually limited
in relation to the size
No special prep, can be done on OPD
bases
3. Ultrasound- not effective in detecting
small stones.
Fasting is necessary with full bladder
4. Intravenous Pyelography- a dye is injected
and the technician takes and x-ray as it
passes in the kidney.
Fasting, risk for allergy
Can be done either inpatient or out-
patient
Others:
1. Urine analysis- use to determine specific
chemical and biological factor.
pH- Norm- 7.0
high- calcium phosphate, struvite
Low- uric acid and cystine stone
Hematuria (blood)- blood in the urine
2. Blood test for stone factors
Creatinine, Calcium, Phosphate, uric acid-
elevates usually in the blood
Note: the size, the location, and
the number of stones.
1. Increase fluid intake
If the stone is less than 5
mm- they pass through
normal urination
Alpha blockers- relax the
muscles in the urinary tract
allowing stone to pass.
2. Surgical Interventions:
a. Extracorporeal Shockwave
lithotripsy- a sound wave is
used to break the stone and
allow it to pass with the
urine/stent can be placed.
- Has 50-90% success rate
- Can be done on outpatient
bases
- Does not work for stone
greater then 3 cm
- Common complications:
Blood in the urine
Bruising on the area
Rarely: kidney damage
b. Ureteroscopy- used for
stone in the lower and
middle ureter. A fiber optic
instrument called
ureteroscope is passed
through the urethra,
bladder and ureter and
removed the stone by laser
or with basket.
Obstruction
and infection
Chronic Kidney
disease- stones
increases the
risk of CKD and
heart attack
Kidney failure-
rarely develop
Great chance of
recurrence:
40% during the
first 5 years
after the initial
attack
75% within 20
years
Renal Failure
Acute or
chronic
Acute Renal failure-
decrease in GFR generally
occurring within hours,
days or weeks that is
associated with
accumulation of waste
products including urea
and creatinine.
Risk Factors:
Pre-renal
o Dehydration, bleeding,
hypoalbuminuria,
decrease cardiac
output, MI, Heart
failure
Intrarenal
o Acute tubular necrosis
due to nephrotoxins,
ischemia, sepsis
Post-renal
o BPH, calculi, tumor
Blood Study:
1. BUN and Creatinine- less sensitive to
changes in GFR
Test Normal Result
BUN 7-20 mg/dl Increase
Creatinine 0.7-1.2 mg/dl increase
2. Urine analysis- useful to identify the cause
of the acute renal failure.
o Ultrasound- identify obstruction/no
special preparation
o CT- identifies obstruction, lesions and
vascular abnormalities.
Medications:
1. Dopamine and Diuretics
2. Insulin therapy
Renal Replacement therapy:
Dialysis: Indications:
a. Volume overload
b. Elevated serum K and Mg
c. Metabolic acidosis
d. BUN greater than 120 mg/dl
e. Significant changes in mental
status
1. HEMODIALYSIS- the method
of choice when rapid changes
are required in a short period
of time
- A temporary vascular access
is required.
- During the procedure,
substance from the blood
move from the blood
through a semi-permeable
membrane and into a
dialysis solution
- Usually done in in-patient.
- Complications:
o Hypotension
o Blood infection
o Loss of blood
Chronic kidney
disease
Metabolic
acidosis
Fluid
accumulation
Electrolyte
imbalances
40-50% mortality
Chronic Renal Failure- is
the progressive irreversible
loss of kidney function.
- There is decrease in GFR
by < 60 ml/min for > 3
months.
- and inc. urinary albumin
excretion.
Risk factors:
Diabetes- 2/3 of the
cases
Investigations:
1. Serum GFR- is preferred to determine
kidney function.
o <60 ml/min and persistent (present
for less than 3 months) indicates
substantial reduction in renal function.
2. Urine analysis
o Persistent WBC or RBC in the absence
of instrumentations
o Presence of cellular cast
o Albumin/creatinine ratio
Control of risk factors:
1. Control of diabetes with
insulin or oral hypoglycemic
agent
2. Control of hypertension
with anti-hypertensive
medications.
3. Nutritional therapy:
Protein restriction
Water restriction
depending on the stage
Complications:
1. Anemia- low Hb
count
2. Hypertention
3. Cardiovascular
disease (10-30 X
mortality)
4. Dyslipidemia- risk
increases with
CKD
5. Metabolic acidosis
No cure for CKD.
Untreated will lead
to end-stage-renal
disease
It requires long
term treatment.
Hypertension- 1/3 of
the cases
Obesity
Stages of CKD
Stages GFR
ml/min
Stage 1 >90-90
Stage 2 60-89
Stage 3 30-59
Stage 4 15-29
Stage 5 <15 RRT
Normal: <30 mg/g Sodium and potassium
restriction
Phosphate restriction
For GFR >15 ml/min
Renal Replacement Therapy
1. Hemodialysis
Requires fistula or graft
for long term use
Fistula is the
anastomosis between
artery and vein
2. Renal transplant
6. Hyperkalemia
Urinary Tract
Infections
- Is a bacterial
infection
affecting the
urinary tract
- Commonly
due to E-coli
1. Women 8X higher than
in men
2. Pregnancy
3. Menopause
4. Hospitalization-
nosocomial in nature.
5. With indwelling catheter
6. Co-morbidities:
a. DM, co-existing
kidney disorders
1. Urine culture and sensitivity- to identify the
specific bacteria and the appropriate
antibiotic.
- The most accurate diagnostic test
- No special preparation
- It takes time before the result is
available
2. Routine urine test
- Presence of WBC, pus, change in color
of urine (cloudy)
3. CT scan and Intravenous pyelography
- Can only be done if obstruction of
urinary tract system is suspected of
causing the UTI.
1. Antibiotic therapy
a. Broad spectrum
antibiotics
2. Non-pharmacologic
management:
a. Increase fluid intake
b. Dietary modification
1. Pyelonephritis
2. Bacteremia
Recurrent infection
http://umm.edu/health/medical/reports/articles/kidney-stones
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Book - MOSBY'S DENTAL DRUG REFERENCE PDFDocument1 496 pagesBook - MOSBY'S DENTAL DRUG REFERENCE PDFMohamed Faizal78% (9)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Case Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Document9 pagesCase Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Bryan Mae H. Degorio0% (3)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- DPH COVID Positive Result LetterDocument3 pagesDPH COVID Positive Result LetterJoe Aronson100% (1)
- Neurobiology of Mental IllnessDocument1 024 pagesNeurobiology of Mental IllnessMario Barragan Cortez100% (1)
- Domiciliary Midwifery RDocument16 pagesDomiciliary Midwifery Rswillymadhu83% (6)
- Case Studies For Bowel EliminationDocument2 pagesCase Studies For Bowel EliminationBryan Mae H. Degorio100% (2)
- A Case Study On Anemia of Chronic DiseaseDocument44 pagesA Case Study On Anemia of Chronic DiseaseKeThSantiban100% (3)
- Allergies or Food Intolerances.: Therapeutic DietDocument3 pagesAllergies or Food Intolerances.: Therapeutic DietBryan Mae H. DegorioPas encore d'évaluation
- Drug Cal - Practice TestDocument2 pagesDrug Cal - Practice TestBryan Mae H. DegorioPas encore d'évaluation
- Worksheet in BloodDocument12 pagesWorksheet in BloodBryan Mae H. DegorioPas encore d'évaluation
- Introduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Document3 pagesIntroduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Bryan Mae H. DegorioPas encore d'évaluation
- Drugs Affecting The Immune SystemDocument4 pagesDrugs Affecting The Immune SystemBryan Mae H. DegorioPas encore d'évaluation
- NMC Standards To Support Learning AssessmentDocument85 pagesNMC Standards To Support Learning AssessmentBryan Mae H. DegorioPas encore d'évaluation
- Skeletal SystemDocument27 pagesSkeletal SystemBryan Mae H. DegorioPas encore d'évaluation
- Systems of Measurement and Drug CalculationDocument13 pagesSystems of Measurement and Drug CalculationBryan Mae H. DegorioPas encore d'évaluation
- Care of Patients with Musculoskeletal IssuesDocument3 pagesCare of Patients with Musculoskeletal IssuesBryan Mae H. DegorioPas encore d'évaluation
- Sampling Process and Measurement ScaleDocument18 pagesSampling Process and Measurement ScaleBryan Mae H. DegorioPas encore d'évaluation
- APA Referencing 6th Ed Quick GuideDocument2 pagesAPA Referencing 6th Ed Quick GuidehartymPas encore d'évaluation
- EmbryologyDocument26 pagesEmbryologyBryan Mae H. Degorio100% (1)
- Disaster Nursing and ManagementDocument39 pagesDisaster Nursing and ManagementBryan Mae H. DegorioPas encore d'évaluation
- APA Referencing 6th Ed Quick GuideDocument2 pagesAPA Referencing 6th Ed Quick GuidehartymPas encore d'évaluation
- Documentation and ReportingDocument32 pagesDocumentation and ReportingBryan Mae H. Degorio100% (1)
- Concept Mapping BMDDocument4 pagesConcept Mapping BMDBryan Mae H. DegorioPas encore d'évaluation
- Is Mentorship Right for Your Nursing CareerDocument17 pagesIs Mentorship Right for Your Nursing CareerBryan Mae H. DegorioPas encore d'évaluation
- Is Mentorship Right for Your Nursing CareerDocument17 pagesIs Mentorship Right for Your Nursing CareerBryan Mae H. DegorioPas encore d'évaluation
- Bowel PreparationDocument2 pagesBowel PreparationBryan Mae H. DegorioPas encore d'évaluation
- Skeletal SystemDocument27 pagesSkeletal SystemBryan Mae H. DegorioPas encore d'évaluation
- Disaster Nursing and ManagementDocument39 pagesDisaster Nursing and ManagementBryan Mae H. DegorioPas encore d'évaluation
- 04 Tissue, Glands and MembranesDocument52 pages04 Tissue, Glands and MembranesBryan Mae H. Degorio100% (1)
- The Adult LearningDocument15 pagesThe Adult LearningBryan Mae H. DegorioPas encore d'évaluation
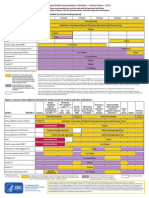
- Adult Immunization ScheduleDocument3 pagesAdult Immunization ScheduleBryan Mae H. DegorioPas encore d'évaluation
- Key Principles of Catholic Social TeachingDocument1 pageKey Principles of Catholic Social TeachingBryan Mae H. DegorioPas encore d'évaluation
- Preceptor Handbook For Nursing EducationDocument41 pagesPreceptor Handbook For Nursing EducationBryan Mae H. Degorio0% (1)
- Human Immunodeficiency Virus /AIDSDocument7 pagesHuman Immunodeficiency Virus /AIDSBryan Mae H. DegorioPas encore d'évaluation
- Nurses' Postoperative Pain Management PracticesDocument6 pagesNurses' Postoperative Pain Management PracticesIndah PratiwiPas encore d'évaluation
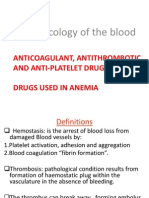
- Pharmacology of The BloodDocument63 pagesPharmacology of The BloodSawsan Z. JwaiedPas encore d'évaluation
- Circadian Rhythm Sleep Disorders CRSDDocument11 pagesCircadian Rhythm Sleep Disorders CRSDjaime manciaPas encore d'évaluation
- Difference Between Endotoxins and ExotoxinsDocument6 pagesDifference Between Endotoxins and ExotoxinsJasna KPas encore d'évaluation
- Health Ed II Module 4Document17 pagesHealth Ed II Module 4saturnino corpuzPas encore d'évaluation
- Learn Acupressure Point Names and Locations For Self-Treatment - HerbalShopDocument23 pagesLearn Acupressure Point Names and Locations For Self-Treatment - HerbalShoptrinitysugumarPas encore d'évaluation
- Identifying ErrorsDocument2 pagesIdentifying ErrorsLourdes Marianne MenesesPas encore d'évaluation
- PEP Practice QuestionsDocument8 pagesPEP Practice QuestionsCynthia ObiPas encore d'évaluation
- RCT Appraisal Sheets 2005 EnglishDocument4 pagesRCT Appraisal Sheets 2005 EnglishAmanda SoebadiPas encore d'évaluation
- The Mind and Body-Mind RelationshipDocument34 pagesThe Mind and Body-Mind RelationshipAbdul Nazar100% (3)
- Drugs To Watch With WARFARINDocument3 pagesDrugs To Watch With WARFARINRajendra RaiPas encore d'évaluation
- Laser Hair RemovalDocument28 pagesLaser Hair RemovalHania KhanPas encore d'évaluation
- Becky Patty ResumeDocument1 pageBecky Patty Resumeapi-510748241Pas encore d'évaluation
- NRP 1Document12 pagesNRP 1syasyaPas encore d'évaluation
- Naranjo AlgorithmDocument3 pagesNaranjo AlgorithmmilkymilkyPas encore d'évaluation
- Epigenetics Congress 2018 BookDocument120 pagesEpigenetics Congress 2018 BookAnonymous FoOawtbV8Pas encore d'évaluation
- Antibacterial Activities of Ethanol Extracts ofDocument9 pagesAntibacterial Activities of Ethanol Extracts ofGenesis JosePas encore d'évaluation
- AIDS Is Man-Made by William CooperDocument3 pagesAIDS Is Man-Made by William CooperPeter100% (3)
- DIABETIC FOOT ULCER CASEDocument28 pagesDIABETIC FOOT ULCER CASEBima Sena Arya YudhaPas encore d'évaluation
- Nursing Care PlansDocument3 pagesNursing Care PlansAvonne SabilePas encore d'évaluation
- Bookshelf NBK236643 PDFDocument320 pagesBookshelf NBK236643 PDFarumPas encore d'évaluation
- Cpga002 0Document4 pagesCpga002 0sakif sPas encore d'évaluation
- Alpers' DiseaseDocument5 pagesAlpers' DiseaseDANY PAUL BABYPas encore d'évaluation
- VPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesDocument94 pagesVPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesSunil100% (41)
- Aspartame's DangersDocument67 pagesAspartame's DangersCrazy LukePas encore d'évaluation