Académique Documents
Professionnel Documents
Culture Documents
Asthma and Obesity in Adults-Ledford
Transféré par
Ari Andry0 évaluation0% ont trouvé ce document utile (0 vote)
10 vues25 pagesAsthma and Obesity in adults Symposium 6 Symposium 6 Dennis K. Ledford, M.D. Professor of medicine and pediatrics university of south florida college of medicine Tampa, florida USA Potential Conflicts of interest Potential conflicts of interest Speaker Bureau: $20,000 AstraZeneca, ImmunoGen Research Paid to University: forest, boehringer ingelheim, genentech, Merck Research Paid to Practice with $10,000 personal: Genentech Legal: Case review
Description originale:
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentAsthma and Obesity in adults Symposium 6 Symposium 6 Dennis K. Ledford, M.D. Professor of medicine and pediatrics university of south florida college of medicine Tampa, florida USA Potential Conflicts of interest Potential conflicts of interest Speaker Bureau: $20,000 AstraZeneca, ImmunoGen Research Paid to University: forest, boehringer ingelheim, genentech, Merck Research Paid to Practice with $10,000 personal: Genentech Legal: Case review
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
10 vues25 pagesAsthma and Obesity in Adults-Ledford
Transféré par
Ari AndryAsthma and Obesity in adults Symposium 6 Symposium 6 Dennis K. Ledford, M.D. Professor of medicine and pediatrics university of south florida college of medicine Tampa, florida USA Potential Conflicts of interest Potential conflicts of interest Speaker Bureau: $20,000 AstraZeneca, ImmunoGen Research Paid to University: forest, boehringer ingelheim, genentech, Merck Research Paid to Practice with $10,000 personal: Genentech Legal: Case review
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 25
Asthma and Obesity in
Asthma and Obesity in
Adults
Adults
Symposium 6
Symposium 6
Dennis K. Ledford, M.D.
Professor of Medicine and Pediatrics
University of South Florida College of
Medicine
Tampa, Florida
USA
Potential Conflicts of Interest
Potential Conflicts of Interest
Speaker Bureau: AstraZeneca
Stock: <$20,000 AstraZeneca,
ImmunoGen
Research Paid to University: Forest,
Boehringer Ingelheim, Genentech, Merck
Research Paid to Practice with <$10,000
personal: Genentech
Legal: Case review < $5,000 not related
Journal: Allergy Watch, JACI
Organizations: AMA, ACP, ACCP, AAAAI
Learning Objectives
Learning Objectives
To address the question: Does obesity
cause asthma or are asthmatic patients
more likely to become obese?
To review how obesity may influence
treatment choices in asthma.
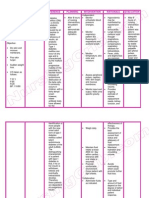
Prevalence
Prevalence
Asthma
Increasing with 6-7% of
adults affected
Increase is greater in
developed countries
Increases dyspnea and
exercise intolerance
Increased burden in
select ethnicities (African
American and Hispanic in
US)
Obesity
NHANES data in USA
shows increase from 15%
in 1976-80 to 32.9% in
2003-04
Increase is greater in
developed countries
Increases dyspnea and
exercise intolerance
Increased burden in
select ethnicities and
poor
Obesity and Asthma
Obesity and Asthma
One causes or increases the severity of
the other, directly or indirectly
GERD, sleep apnea
Decreased activity, effects of medications
Coincidental occurrences (shared risk
factors)
Environmental influences increase both
simultaneously but through different
mechanisms
One mimics the other (obesity symptoms
resemble asthma symptoms)
Asthma and Obesity
Asthma and Obesity
Obesity Increases the Incidence of Asthma
17 prospective studies, 9 in adults and 8 in
children
Each involved several thousand subjects
Follow up periods of 2-21 years
Only 1 failed to show an increased
incidence of asthma in the obese
Obesity antedates asthma
Many controlled for exercise
Most show an effect of overweight as well
Asthma and Obesity
Asthma and Obesity
Obesity and Asthma Control
Obesity Reduces Obesity Doesnt Reduce
Asthma Control Asthma Control
St. Pierre et al. (2006) Kwong et al (2006)*
Dixon et al. (2006)
Lavoie et al. (2006)
Peters-Golden et al. (2006)
Lessard et al. (2008)**
Mosen et al. (2008)
Vogt et al. (2008)
Boulet et al (2007)
* Only study performed in children
** Reduced control occurred despite similar ability to perceive
symptoms
Asthma and Obesity
Asthma and Obesity
Obesity Increases Asthma Severity
3095 patients in the National Asthma Survey
Compared to non-overweight subjects, obese
subjects were significantly more likely to.
Odds Ratio
Report continuous symptoms 1.66
Miss work 1.35
Use short acting
2
agonists 1.36
Use inhaled steroids 1.34
Have severe persistent asthma 1.42
(GINA class IV)
Taylor et al. Thorax, Jan 2008
Associations of Obesity and
Associations of Obesity and
Asthma
Asthma
Ford and Mannino showed with NHANES
data 1988-1994 that obese individuals
were 44% more likely to have asthma
Chen in cross sectional study showed that
BMI > 30 associated with asthma OR 2.06
(1.42-4.05) only in females
Hancox in adults and children showed that
28% of risk for asthma in females
associated with overweight
Potential Problems in
Potential Problems in
Assessing Relationship
Assessing Relationship
Difficult to control multiple variables in
studies (genetic, environment, behavior)
Definition of asthma problematic as a
syndrome of syndromes (phenotypes of
asthma)
Definition of obesity problematic
BMI
Total body fat
Body fat distribution
Type of body fat
Potential Problems in
Potential Problems in
Assessing Relationship
Assessing Relationship
Asthma medications may be less effective
in obese patients
Eur Respir J 2006;27:495-503
As weight increased, response to inhaled
beclomethasone decreased and response to
montelukast was not affected
Confusion between control and severity
Weight loss has not consistently improved
pathophysiology of asthma (Chest
2000;118:1315-21)
Potential Problems is
Potential Problems is
Assessing Relationship
Assessing Relationship
Symptoms correlate but diagnosis less
clear
Dyspnea, cough, wheeze
BHR does NOT correlate
No evidence of association of obesity with
atopy, IgE production, eosinophilia
Severity of asthma may be greater in
obesity making association misleading
(Taylor Thorax 2008;63:14-20/Rodrigo
Chest 2007;132:1513-19)
Potential Mechanisms
Potential Mechanisms
Mechanical effect of weight on breathing
physiology
Restriction
Caloric intact modulates asthma
Adipose cells affect inflammation
Proinflammatory adipokine LEPTIN
Antiinflammatory adipokine ADIPONECTIN
Obesity associated with increases in CRP,
TNF, and IL-6
Physiologic Respiratory
Physiologic Respiratory
Factors in Obesity
Factors in Obesity
Reduced lung volumes (FRC)
Reduced airway diameter, TV
Increased airway resistance (males)
Rapid shallow breathing
Increased work of breathing
FEV1/FVC ratio tends to remain normal
Decreased compliance due to compression
and possible fatty tissue in chest wall
GERD
Inflammation in Obesity
Inflammation in Obesity
Leptin increased, adiponectin decreased
Eosinophils with leptin receptors
TNF, Vascular endothelial growth factor,
IL-6, oxidative stress markers increased
C-reactive protein increased
TGF- increased
Eotaxin increased (studies inconsistent)
FeNO increased
Animal Models
Animal Models
Obese mice, both genetic and caloric
excess, show increased AHR that
correlates with weight and possibly
duration of increased weight
Lung size inconsistent
Increased airway response to antigen
without Th2 cytokine increase or
eosinophils
?role for mast cells and LTAs
Animal Models
Animal Models
Obese mice have increased response to
ozone with BHR, pulmonary resistance
and inflammation markers
Greater respiratory pathology with
respiratory viral infection with obese mice
Obese mice have reduced NK cell activity
following influenza infection
Inflammation in Humans
Inflammation in Humans
Decrease in M2 monocytes in adipose
tissue with obesity
Increase in TNF and IL-6
Decrease in inhibitor of IL-1 receptor
Monocytes increased with hypoxia of adipose
tissue
Hormone Changes
Hormone Changes
Leptin increased
Satiety hormone and proinflammatory
Increased AHR in mice without change in Th2
cytokines or eosinophil influx in airway
Increased inflammation response to ozone in
mice, possible effect on Toll like receptors
Two cross sectional human studies show
increase in asthma independent of body mass
Could be secondary to airway inflammation
Associations
Associations
Sutherland, Sears, McLachlan, Poulton, Hancox.
Annals Allergy Asthma and Immunology 2009;103-107
Hormone Changes
Hormone Changes
Adiponectin decreased
Inverse association with atherosclerosis and
type 2 diabetes
Augments production of macrophage IL-10
and IL-1 receptor antagonist
Suppresses AHR and Th2 cytokines in mice
Lung tissue has 3 receptors, one of which
(adipoR2), has anti-inflammatory action
All 3 reduced following bronchial allergen
challenge in mice
Decreased FeNO in males
Conclusions
Conclusions
Both obesity and asthma are increasing in
large portions of the world
Obesity may affect the severity of asthma
but is less clear that obesity increases the
occurrence of asthma
Combination of mechanisms likely to link
the two conditions
Shared comorbidities such as GERD
Physical effects
Hormonal effects
Challenges
Challenges
Not clear that animal models will be
sufficient to explain possible relationships
Cross sectional and epidemiologic studies
are unlikely to provide answers but may
help generate questions
Hypothesis driven prospective studies will
be needed but are exceedingly difficult
due to duration of treatment and difficulties
with multiple variables and controls
24
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 06 Renr5908 08 01 All PDFDocument108 pages06 Renr5908 08 01 All PDFFrancisco Ospino Arrieta100% (2)
- Implementasi Sistem Pengenalan Candi Kecil Di Yogyakarta Menggunakan BerbasisDocument7 pagesImplementasi Sistem Pengenalan Candi Kecil Di Yogyakarta Menggunakan BerbasisRivan AuliaPas encore d'évaluation
- Edagogy of Anguages: VerviewDocument54 pagesEdagogy of Anguages: VerviewMukesh MalviyaPas encore d'évaluation
- Interdisciplinary Project 1Document11 pagesInterdisciplinary Project 1api-424250570Pas encore d'évaluation
- Steve Talbott Getting Over The Code DelusionDocument57 pagesSteve Talbott Getting Over The Code DelusionAlexandra DalePas encore d'évaluation
- Ancient India: Book Recommendation: Indian Feudalism Urban Decay in India - RS SharmaDocument5 pagesAncient India: Book Recommendation: Indian Feudalism Urban Decay in India - RS SharmaShraddha 7Pas encore d'évaluation
- North Rig 4Document1 pageNorth Rig 4avefenix666Pas encore d'évaluation
- I. Errors, Mistakes, Accuracy and Precision of Data Surveyed. A. ErrorsDocument53 pagesI. Errors, Mistakes, Accuracy and Precision of Data Surveyed. A. ErrorsJETT WAPPas encore d'évaluation
- SolBridge Application 2012Document14 pagesSolBridge Application 2012Corissa WandmacherPas encore d'évaluation
- C MukulDocument1 pageC Mukulharishkumar kakraniPas encore d'évaluation
- Unit 2 Talents: Phrasal Verbs: TurnDocument5 pagesUnit 2 Talents: Phrasal Verbs: TurnwhysignupagainPas encore d'évaluation
- Quick-Guide M1M 20Document2 pagesQuick-Guide M1M 20KhaledPas encore d'évaluation
- Free DMAIC Checklist Template Excel DownloadDocument5 pagesFree DMAIC Checklist Template Excel DownloadErik Leonel LucianoPas encore d'évaluation
- Bob Jones: This CV Template Will Suit Jobseekers With Senior Management ExperienceDocument3 pagesBob Jones: This CV Template Will Suit Jobseekers With Senior Management ExperienceDickson AllelaPas encore d'évaluation
- Rabbit Book PDFDocument20 pagesRabbit Book PDFMatumelo Rebecca DaemanePas encore d'évaluation
- Cosmology Questions and Answers - SanfoundryDocument9 pagesCosmology Questions and Answers - SanfoundryGopinathan MPas encore d'évaluation
- Vivekananda'S Conception of Normative Ethics and Resolution Ethical Problems in BusinessDocument8 pagesVivekananda'S Conception of Normative Ethics and Resolution Ethical Problems in BusinessYajat BhargavPas encore d'évaluation
- Module 8 - Facilitating Learner - Centered TeachingDocument4 pagesModule 8 - Facilitating Learner - Centered TeachingSheila Mae Paltep100% (3)
- Concept of ConstitutionDocument32 pagesConcept of ConstitutionDorepe Icon0% (1)
- Linguistic LandscapeDocument11 pagesLinguistic LandscapeZara NurPas encore d'évaluation
- DRUG STUDY (Erythromycin)Document3 pagesDRUG STUDY (Erythromycin)Avianna CalliopePas encore d'évaluation
- Neoclassical CounterrevolutionDocument1 pageNeoclassical CounterrevolutionGraziella ValerioPas encore d'évaluation
- User Manual ManoScanDocument58 pagesUser Manual ManoScanNurul FathiaPas encore d'évaluation
- Nursing Care Plan Diabetes Mellitus Type 1Document2 pagesNursing Care Plan Diabetes Mellitus Type 1deric85% (46)
- PMP Exam Questions and Answers PDFDocument12 pagesPMP Exam Questions and Answers PDFAshwin Raghav SankarPas encore d'évaluation
- Tadano450xl PDFDocument12 pagesTadano450xl PDFmunawar0% (1)
- Price List Printer HP Per November 2017Document14 pagesPrice List Printer HP Per November 2017anthony_prawiraPas encore d'évaluation
- Operating Instructions: Vacuum Drying Oven Pump ModuleDocument56 pagesOperating Instructions: Vacuum Drying Oven Pump ModuleSarah NeoSkyrerPas encore d'évaluation
- Chapter 3Document26 pagesChapter 3Francis Anthony CataniagPas encore d'évaluation
- Holy Spirit Mass SongsDocument57 pagesHoly Spirit Mass SongsRo AnnPas encore d'évaluation