Académique Documents
Professionnel Documents
Culture Documents
10.1007 - s11904 012 0129 5
Transféré par
Monica Sari Suryadi0 évaluation0% ont trouvé ce document utile (0 vote)
85 vues13 pagesImmune reconstitution inflammatory syndrome is a frequent early complication of antiretroviral therapy (ART) in patients with advanced HIV. Corticosteroids have been used to treat more severe cases of IRIS associated with mycobacterial and fungal infections.
Description originale:
Titre original
10.1007_s11904-012-0129-5
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentImmune reconstitution inflammatory syndrome is a frequent early complication of antiretroviral therapy (ART) in patients with advanced HIV. Corticosteroids have been used to treat more severe cases of IRIS associated with mycobacterial and fungal infections.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
85 vues13 pages10.1007 - s11904 012 0129 5
Transféré par
Monica Sari SuryadiImmune reconstitution inflammatory syndrome is a frequent early complication of antiretroviral therapy (ART) in patients with advanced HIV. Corticosteroids have been used to treat more severe cases of IRIS associated with mycobacterial and fungal infections.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 13
CO-INFECTIONS (C BENSON, SECTION EDITOR)
Management of the Immune Reconstitution
Inflammatory Syndrome
Graeme Meintjes & James Scriven & Suzaan Marais
Published online: 3 July 2012
#Springer Science+Business Media, LLC 2012
Abstract The immune reconstitution inflammatory syn-
drome (IRIS) is a frequent early complication of antiretroviral
therapy (ART) in patients with advanced HIV. Because there
is no confirmatory diagnostic test, the diagnosis is based on
clinical presentation and exclusion of alternative causes for
deterioration, such as antimicrobial drug resistance. Opportu-
nistic infection treatment should be optimized. Mild cases
may require symptomatic therapy alone or nonsteroidal anti-
inflammatory drugs. Corticosteroids have been used to treat
more severe cases of IRIS associated with mycobacterial and
fungal infections. There is evidence from a randomized con-
trolled trial that prednisone reduces morbidity and improves
symptoms in paradoxical tuberculosis (TB)-IRIS. Neurologi-
cal TB-IRIS is potentially life-threatening; high-dose cortico-
steroids are indicated and ART interruption should be
considered if level of consciousness is depressed. When con-
sidering corticosteroid treatment clinicians should be aware of
their side effects and only use them when the diagnosis of
IRIS is certain. In viral forms of IRIS corticosteroids are
generally avoided.
Keywords HIV
.
AIDS
.
Antiretroviral therapy
.
Immune
reconstitution inflammatory syndrome
.
Tuberculosis
.
Cryptococcosis
.
Mycobacterial disease
.
Cytomegalovirus
.
Kaposis sarcoma
.
Progressive multifocal
leukoencephalopathy
.
Viral hepatitis
.
Corticosteroids
Introduction
During early antiretroviral therapy (ART) a proportion of
patients experience deterioration due to the immune recon-
stitution inflammatory syndrome (IRIS). This proportion
has been up to 25 % in some series [13]. IRIS manifests
with inflammatory reactions, targeted at the antigens of
opportunistic infections (OIs) driven by rapidly recovering
G. Meintjes
:
J. Scriven
:
S. Marais
Clinical Infectious Diseases Research Initiative,
Institute of Infectious Diseases and Molecular Medicine,
University of Cape Town,
Cape Town, South Africa
J. Scriven
e-mail: james.scriven@liverpool.ac.uk
S. Marais
e-mail: marais.suzaan@gmail.com
G. Meintjes
Division of Infectious Diseases and HIV Medicine,
University of Cape Town,
Cape Town, South Africa
G. Meintjes
GF Jooste Hospital,
Cape Town, South Africa
G. Meintjes
Department of Medicine, Imperial College London,
London, UK
J. Scriven
Liverpool School of Tropical Medicine, Liverpool University,
Liverpool, UK
S. Marais
Division of Neurology, Department of Medicine,
University of Cape Town,
Cape Town, South Africa
G. Meintjes (*)
:
J. Scriven
:
S. Marais
Institute of Infectious Diseases and Molecular Medicine,
Faculty of Health Sciences, University of Cape Town,
Anzio Road, Observatory,
Cape Town 7925, South Africa
e-mail: graemein@mweb.co.za
Curr HIV/AIDS Rep (2012) 9:238250
DOI 10.1007/s11904-012-0129-5
immune function. IRIS is most frequently described in as-
sociation with mycobacterial, fungal, and viral infections.
IRIS may occur in patients already diagnosed with the OI
resulting in recurrence or worsening of clinical features
despite effective treatment (termed paradoxical IRIS) or
may result in the unmasking of an unrecognized infection
that presents with exaggerated inflammatory features
(termed unmasking IRIS) [4, 5]. IRIS places a burden on
health care services particularly in resource-limited settings
where OIs at ART initiation are common. Up to half of IRIS
cases require hospitalization and many require multiple
diagnostic or therapeutic procedures [6]. The mortality as-
sociated with IRIS varies according to the underlying OI,
but is substantial when IRIS affects the central nervous
system (CNS) [7, 8, 9].
The pathogenesis and prevention of IRIS have recently
been reviewed [10]. Here we review IRIS management that
is challenging for a number of reasons: there is only one
randomized controlled trial [11], IRIS may occur in asso-
ciation with a wide range of infections, and even for the
same infection there is considerable heterogeneity. Difficul-
ties in making the diagnosis with certainty may complicate
decisions regarding treatment. In this review we first address
the diagnosis of IRIS, then discuss the common forms of
medical treatment used (corticosteroids and nonsteroidal
anti-inflammatory drugs [NSAIDs]), and then management
of specific forms of IRIS focusing on common and clinically
severe forms. Dermatological forms of IRIS, although com-
mon [12], are not discussed in this review. Finally, we
discuss future directions in IRIS treatment and research.
Diagnosis of IRIS
The diagnosis of IRIS may be challenging, particularly in
settings where access to diagnostic resources are limited. In
cases of unmasking IRIS, the diagnosis involves using con-
ventional diagnostic tests to diagnose the underlying OI. In
paradoxical IRIS the patient deteriorates despite being on
effective treatment for the OI and there is often a wide
differential diagnosis, but there is no confirmatory diagnos-
tic test for paradoxical IRIS. Thus, diagnosis relies upon the
presence of the following: improvement of OI symptoms on
OI treatment prior to ART; deterioration with features of the
OI soon after starting ART; and demonstration of a CD4
and/or HIV viral load response to ART where feasible and
exclusion of alternative causes for deterioration such as a
bacterial infection or an additional OI, a drug reaction, poor
adherence, or resistance to OI treatment. This is complicated
by the finding that paradoxical tuberculosis (TB)-IRIS may
occur in patients with undiagnosed rifampicin-resistant TB
[13]. The differential diagnoses to exclude depend on the
organ system affected. For example, with suspected nodal
TB-IRIS the important differential diagnoses are nodal
Kaposis sarcoma (KS), lymphoma, and nontuberculous
mycobacteria; different to suspected pulmonary TB-IRIS
where bacterial or pneumocystis pneumonia and pulmonary
KS are the important differentials. In certain cases with
suspected IRIS (eg, a TB patient with new pulmonary infil-
trate after starting ART), clinicians may take appropriate
bacterial cultures and treat for a bacterial infection and only
if there is no improvement and investigations for other
causes are negative then make the diagnosis of IRIS. Con-
sensus case definitions for TB and cryptococcal IRIS have
been published [4, 5] and the key principles shared by these
definitions are summarized in Table 1.
Common Forms of Treatment
Corticosteroids
Corticosteroids exert anti-inflammatory effects on most
types of immune cells through direct effects on transcription
of inflammatory mediators via the glucocorticoid responsive
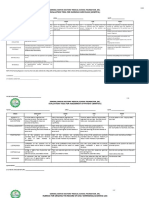
Table 1 Key features common to both the TB and cryptococcal IRIS
case definitions of the INSHI
a
Paradoxical IRIS
Reliable diagnosis of the OI
b
prior to initiating ART
Improvement on treatment for the OI prior to ART
Clinical deterioration within the first months of ART (first 3 months
for TB-IRIS; first 12 months for cryptococcal IRIS)
c
Deterioration with inflammatory manifestations related to the OI
Alternative explanations for deterioration excluded (OI drug
resistance, poor adherence to OI treatment, another infection or
neoplasm, and drug toxicity or reaction)
Unmasking IRIS
d
Not on treatment for the OI when ART initiated
New and unusual, heightened or exaggerated inflammatory
presentation of the OI within the first months of ART (first 3 months
for TB-IRIS; typically first 3 months for cryptococcal IRIS)
c
a
CD4 count and HIV viral load measurements are not a requirement in
these case definitions unlike other IRIS case definitions. The reason for
this is that the definitions were designed to be applicable in resource-
limited settings where these measurements are frequently unavailable;
studies have shown that the vast majority of ART-nave patients ad-
herent to ART have a substantial HIV viral load reduction in the first
months of ART; and it is well documented that IRIS may occur prior to
a CD4 count rise on ART [4, 5]
b
OI, refers to TB or cryptococcosis in this table
c
IRIS may also occur after re-initiation of ART or regimen change due
to treatment failure
d
Unmasking IRIS represents only a subset of patients presenting with a
new diagnosis of the OI after starting ART
ART antiretroviral therapy; INSHI International Network for the Study
of HIV-associated IRIS; IRIS immune reconstitution inflammatory
syndrome; OI opportunistic infection; TB tuberculosis
Curr HIV/AIDS Rep (2012) 9:238250 239
element, indirect genomic effects via interference with other
transcriptional factors such as nuclear factor-B and activa-
tor protein 1, and nongenomic effects on anti-inflammatory
proteins [14, 15]. The result is increased transcription of a
number of anti-inflammatory mediators and decreased tran-
scription of proinflammatory cytokines, chemokines, enzymes,
receptors, and adhesion molecules [16, 17]. In addition, corti-
costeroids have been shown to reduce T-cell survival by en-
hancing apoptosis [16]. Corticosteroids have been used to treat
several HIV-related conditions [18, 19] and certain forms of
IRIS with reports of benefit. However, there are complications
to be considered, particularly in patients with advanced
immunosuppression and with prolonged use. These issues are
summarized in Table 2.
NSAIDs
NSAIDs inhibit cyclooxygenase that converts arachidonic
acid to prostaglandin mediators of inflammation. There are
many reports of clinicians using NSAIDs to treat IRIS [20,
21, 22]. Some clinical guidelines recommend NSAIDs be
used as first-line treatment for mild IRIS related to myco-
bacterial infections, with corticosteroids reserved for more
severe cases [23]. However, there is no clinical trial data on
efficacy, and because they have generally been used in
milder IRIS it remains unclear whether they would benefit
patients with more severe forms of IRIS. One advantage is
that they do not predispose to other infections. Nephrotox-
icity is a concern with long-term use, particularly in patients
with HIV-associated nephropathy and those on tenofovir
[24, 25].
Management of Common and Severe Forms of IRIS
Management of Paradoxical TB-IRIS
Paradoxical TB-IRIS occurs in 15.7 % (95 % credibility
interval [CrI]09.724.5) of patients starting ART while on
treatment for TB [8]. Common clinical features are fever,
lymphadenitis, expanding pulmonary infiltrates, and serous
effusions [5]. The most severe and life-threatening form of
TB-IRIS (CNS involvement) is discussed separately below.
Adjunctive corticosteroids have resulted in improved out-
comes in certain forms of TB such as meningitis [26] and
pericarditis [27]. This benefit is likely related to modulation of
TB-associated immunopathology by corticosteroids. In TB-
IRIS, there were initial observational reports of patients expe-
riencing symptom improvement on corticosteroids [28]. The
only randomized controlled trial of IRIS treatment to be con-
ducted was in patients with paradoxical TB-IRIS: a double-
blind placebo-controlled trial of prednisone excluding patients
with immediately life-threatening TB-IRIS (n055 in each
arm) [11]. Prednisone was dosed at 1.5 mg/kg/day for
2 weeks followed by 0.75 mg/kg/day for 2 weeks. The high
initial dose was chosen because rifampicin induces prednisone
metabolism [29]. If significant clinical deterioration occurred
participants were switched to open-label prednisone at physi-
cian discretion. Prednisone resulted in a significant reduction
in the combined primary end point of days of hospitalization
plus outpatient therapeutic procedures. With prednisone there
was also more rapid improvement in symptoms, quality-of-
life score, and chest radiography, and more rapid reduction in
C-reactive protein. Ten patients in the prednisone armrelapsed
with IRIS symptoms after stopping their 4-week course of
prednisone. These findings suggest that a 4-week course of
prednisone results in reduced morbidity fromTB-IRIS, but for
a subgroup 4 weeks is too short. There was no mortality
difference between prednisone and placebo-treated partici-
pants, but immediately life-threatening cases (eg, those with
neurological involvement) were excluded fromthe trial. There
was no excess of metabolic side effects or severe infections in
those on prednisone, but minor infections (oral candidiasis
and uncomplicated herpes simplex) were more common in
those who received prednisone [11]. Prednisone was asso-
ciated with significant reductions in serum concentrations of
several cytokines (interleukin [IL]-6, IL-10, IL-12, interferon
[IFN]-, tumor necrosis factor [TNF]-) and the chemokine
Table 2 Potential side effects of corticosteroids in HIV-infected patients
Potential infective complications
a
Herpes virus reactivations (herpes simplex virus 1 and 2 and
cytomegalovirus)
Kaposis sarcoma development or progression
Strongyloides hyperinfection
Clinical and biochemical worsening in chronic hepatitis B
Oral, vaginal, or esophageal candidiasis
Increased risk for other infections such as TB
Potential metabolic and other complications
b
Dysglycemia
Hypertension and fluid retention
Avascular bone necrosis and osteoporosis (adds to risk associated with
HIV)
Cushingoid features
Hypermania or depression
Hemorrhagic gastritis
Pharmacokinetic interaction with protease inhibitors (increased
corticosteroid concentrations)
a
These infective complications have been mainly described in patients
not on ART and whether being on ART reduces these risks is unclear.
Many of the infective complications have been described in individual
case reports or small case series. Corticosteroids for short durations
(4 weeks) have generally been well tolerated in patients with HIV
without major adverse effects [11, 128]
b
Metabolic complications occur particularly with prolonged use
ART antiretroviral therapy; TB tuberculosis
240 Curr HIV/AIDS Rep (2012) 9:238250
IP-10 (also termed CXCL-10), not seen in those on placebo
suggesting that, at least in part, its effect is mediated through
reduction in cytokine effector responses [30].
We recommend that if paradoxical TB-IRIS symptoms
are severe or life-threatening, prednisone 1.5 mg/kg/day (or
equivalent) should be prescribed for 2 weeks then tapered
according to clinical response. Most patients experience
symptom improvement with a 4-week course of corticoste-
roids. A minority of cases requires longer durations to
control symptoms (discussed below). For other cases with
significant symptoms, prednisone provides symptom relief
but benefits need to be weighed against risks. For example,
corticosteroids are contraindicated in patients with KS and
their use should be deferred if the diagnosis of TB-IRIS is
not certain pending further investigation.
The average duration of TB-IRIS symptoms is 2
3 months [6, 31]. A minority experience more prolonged
TB-IRIS that typically manifests with tuberculous abscess-
es. In some, symptoms last over a year [5, 32]. Therefore,
some patients require several months of corticosteroids to
control symptoms. In the prednisone clinical trial [11],
among participants who received open-label prednisone
the duration of treatment was decided based on clinical
response during tapering and the median duration of pred-
nisone therapy was 84 days (interquartile range060126).
The risk of corticosteroid metabolic complications becomes
substantial after several months and whether corticosteroids
provide symptom relief and alter natural history in patients
with prolonged TB-IRIS is unclear. Our practice is to treat
with corticosteroids for a maximum of 46 months unless
there is dramatic symptom deterioration on stopping.
When TB-IRIS was first recognized clinical practice was
to interrupt ART in certain patients [33]. However, interrup-
tion may be associated with development of ART drug
resistance, clinical progression, and IRIS may recur upon
ART re-initiation. Interrupting ART for TB-IRIS is generally
discouraged today, and attempts should be made to continue
ART and manage the IRIS. One situation where we consider
interruption is in patients with severe neurological TB-IRIS
(discussed below).
TB-IRIS is generally not an indication for prolonging TB
treatment, but in patients who develop chronic tuberculous
abscesses due to TB-IRIS consideration should be given to
prolonging TB treatment until after these collections have
resolved or for 6 months following the last positive TBculture
on an aspirate from the collection. It is our experience that
these collections may remain positive with drug-susceptible
Mycobacterium tuberculosis for several months presumably
because of poor drug penetration. Aspirations of suppurative
lymphadenitis, other pus collections, and effusions in TB-
IRIS can provide symptom relief and are important in obtain-
ing specimens to exclude drug-resistant TB. Repeated aspira-
tions may be required because of re-accumulation [6].
TB-IRIS hepatic involvement is relatively common [13,
34, 35] presenting with tender liver enlargement and chole-
static liver function derangement. Patients may be moderately
jaundiced. Biopsy demonstrates granulomatous hepatitis. Dif-
ferentiating this from drug-induced liver injury (DILI) related
to ART or TB medication can be difficult, although DILI
usually presents with severe transaminitis. If transaminitis or
jaundice is severe, potentially hepatotoxic drugs should be
interrupted. Anecdotally, patients with hepatic TB-IRIS
respond to corticosteroids with improvement in symptoms
and liver functions.
Management of Neurological Presentations of Paradoxical
TB-IRIS
Tuberculous meningitis (TBM) is the most severe form of
TB with a dire prognosis in HIV-infected persons, regardless
of the use of ART [26, 36]. Paradoxical neurological TB-
IRIS, which may manifest as meningitis (TBM-IRIS) [9,
3740], intracranial tuberculomata [3, 9, 37, 4144], brain
abscesses [41, 45], radiculomyelitis [9, 37, 40], and spinal
epidural abscesses [37], contributes to this poor outcome.
We previously reported neurological TB-IRIS in 12 % of
cases who presented with paradoxical TB-IRIS; at 6 months
13 % of those with neurological TB-IRIS had died and 17 %
were lost to follow-up [9].
Raised intracranial pressure secondary to cerebral inflam-
mation may result in life-threatening complications such as
seizures, direct compression of vital brain structures, and
brain herniation. Reducing inflammation involving struc-
tures within the confined intracranial space is critical. Cor-
ticosteroids have been associated with reduced mortality in
TBM outside of the context of IRIS [26]. In neurologic TB-
IRIS, oral or intravenous corticosteroids have anecdotally
shown benefit [9, 3941, 43, 45]. Of 23 patients with
neurologic TB-IRIS, 18 of 21 patients treated with predni-
sone (starting dose: 1.5 mg/kg/day) showed an initial im-
provement [9]. In other reports of neurological TB-IRIS,
patients with TBM [39, 40], brain abscesses [41, 45], tuber-
culomata [43], and radiculomyelitis [40] improved with
corticosteroids. Patients with neurological TB may show
rapid, unexpected deterioration; therefore, our practice is
to treat all patients with neurological TB-IRIS with systemic
corticosteroids (prednisone, methylprednisolone, or dexa-
methasone) at an initial dose of prednisone 1.5 mg/kg/day
(or equivalent) for 2 weeks, followed by gradual tapering
according to the patients response. Symptoms may recur
after stopping corticosteroids [43], or reduction in dose,
requiring re-initiation, or increase in dose, and prolonged
treatment.
Currently, no other treatment is of known benefit. Although
the general approach to the treatment of IRIS is to continue
ART, temporary interruption of ART may be considered as a
Curr HIV/AIDS Rep (2012) 9:238250 241
last resort in patients with depressed level of consciousness or
severe disease not responsive to corticosteroids [46]. An illus-
trative case is shown in Fig. 1.
Management of Unmasking TB-IRIS
Unmasking TB-IRIS occurs in patients who have undiag-
nosed TB when ART is started and present with exaggerated
inflammatory features of TB within the first 3 months of
ART [5]. Clinicians working in TB endemic settings should
have a high index of suspicion for TB in patients who
deteriorate after starting ART. In patients where there is a
high index of suspicion for unmasking TB-IRIS and the
presentation is severe (eg, pulmonary TB with respiratory
distress mimicking a bacterial pneumonia) it may be neces-
sary to start empiric TB treatment according to World Health
Organization guidelines for those with danger signs [47].
Some clinicians start corticosteroids for patients with
unmasking pulmonary TB-IRIS complicated by respiratory
failure, although there is no clinical trial evidence to support
this practice.
Management of Mycobacterium Avium ComplexIRIS
Both unmasking and paradoxical presentations of Mycobac-
terium avium complex (MAC)-IRIS are described. MAC-
IRIS presents with focal inflammatory lesions such as lymph-
adenitis (peripheral, abdominal, or thoracic) and abscesses. It
may also involve abdominal organs and the lungs [48, 49].
Cases with abdominal involvement have a more complicated
course with more relapses and hospitalization requirements
[48]. There is a wide spectrum of disease in MAC-IRIS: some
patients have a benign self-limiting course, some patients clear
the infection without MAC treatment and with immune resto-
ration alone, whereas others have several relapses or a severe
protracted course despite ART, MAC treatment, and cortico-
steroids [4850]. In one case series, 10 patients who did not
receive MAC treatment for longer than 2 weeks did not
experience symptoms for longer than those who were treated
for MAC [48]. In contrast, certain MAC-IRIS cases have
lasted over 5 years despite treatment [49].
The protracted course in certain cases may be related to
difficulty in eradicating disseminated infection (especially
with intra-abdominal disease) with ongoing replication of
organisms providing the antigen stimulus for chronic inflam-
mation. With optimal MAC treatment only ~50 % of dissem-
inated MAC cases have complete microbiological response (2
consecutive negative blood cultures) by 16 weeks [51].
Several MAC-IRIS cases with culture positivity for
much longer durations are described [49, 5254]. Cinti
et al. [52] described three cases of MAC with culture-
positive recurrence on ART despite 725 months of
MAC treatment. These patients had focal organ involve-
ment and the authors suggested that this may represent
a variation of IRIS. Phillips et al. [48] reported seven
MAC-IRIS cases that had 13 culture-positive MAC-IRIS
events during follow-up. A case of culture-positive re-
lapse with extensive CNS inflammatory lesions attribut-
ed to IRIS occurred after 14 months of MAC treatment
was stopped [53].
Thus, if MAC-IRIS is prolonged clinicians should re-assess
whether the cultures (fromblood and IRIS disease site) are still
Fig. 1 Illustrative case of paradoxical tuberculosis (TB)immune recon-
stitution inflammatory syndrome management. A 34-year-old HIV-
infected man presented with lymphocytic meningitis and a left pleural
effusion. Disseminated TB was diagnosed and he commenced TB treat-
ment and prednisone (1.5 mg/kg/day). Mycobacterium tuberculosis (sus-
ceptible to rifampicin and isoniazid) was cultured from cerebrospinal
fluid (CSF) and pleural fluid. After 2 weeks of TB treatment, his symp-
toms had improved and he commenced antiretroviral therapy (ART). Two
weeks later, he presented with recurrence of headache and worsening
CSF inflammation compatible with TB meningitis IRIS. Brain CT
performed at IRIS showed an area of focal gyral enhancement in the right
occipital lobe with adjacent cerebral edema (a). His symptoms resolved
on an increased dose of prednisone (2 mg/kg/day), which was tapered and
stopped over a 3-month period. Five months after starting ART he
presented with left-sided chest pain. CTchest revealed a left-sided pleural
effusion and multiple necrotic mediastinal lymph nodes (b). Prednisone
was not restarted. He was prescribed analgesia and TB treatment was
extended for a total duration of 12 months, with resolution of the pleural
effusion and lymphadenopathy
242 Curr HIV/AIDS Rep (2012) 9:238250
positive. If cultures are positive then intensification of MAC
treatment should be considered (with rifabutin, aminoglyco-
side, and/or quinolone) and testing for macrolide resistance
should be performed if available.
In terms of management, Riddell et al. [49] described the
course and treatment of 20 patients with MAC-IRIS, 16 of
whom experienced clinical or radiographic resolution after a
median of 19.5 months (range: 22 days to 5.2 years). Over
half the patients had additional antimycobacterial therapy
(rifabutin, ciprofloxacin, and/or amikacin) added to macro-
lide and ethambutol. Eight were treated with oral cortico-
steroids (mean duration: 17 months). The authors suggest
that some, but not all, patients with MAC-IRIS require
corticosteroids. Two patients were treated with granulocyte
colony-stimulating factor (G-CSF) [49]. In another case
series of 51 patients with non-tuberculous mycobacterial
IRIS (the majority MAC), the median symptom duration
was 6 months and 9 patients were treated with corticoste-
roids, 8 of whom had a prompt clinical response. Five of
these relapsed when corticosteroids were tapered or stopped
[48]. Thus, corticosteroids have anecdotally provided symp-
tom benefit and should be used when symptoms such as
abdominal pain or symptoms related to compression by
nodes or abscesses are prominent. Case reports have de-
scribed corticosteroid prescription for prolonged periods
(eg, over 1 year) [49]. However, the benefit of continuing
corticosteroids for such a long duration is unclear and ad-
verse effects are cumulative. Our practice is to start predni-
sone 1 mg/kg/day (or equivalent) for patients with MAC-
IRIS and significant symptoms (eg, abdominal pain), then
wean according to symptom response. We withdraw cortico-
steroids after a maximum 46 months in MAC-IRIS unless
there was evidence that severe deterioration occurred during
corticosteroid withdrawal. NSAIDs have also been used
[48]. ART should not be interrupted. Lymph node aspira-
tion, surgical excision of nodes, and surgical drainage of
suppurative lesions have also been described [50].
Management of Paradoxical Cryptococcal IRIS
Of patients with cryptococcal meningitis (CM) diagnosed
before ART, 13 %45 % develop paradoxical IRIS after a
median of 49 weeks on ART [7, 55, 56, 57]. Patients
typically present with headache, meningismus, raised intra-
cranial pressure, and in a subset focal neurological signs.
Non-neurological presentations (eg, lymphadenitis and
pneumonitis) are also reported [58]. Cryptococcal IRIS is
associated with significant morbidity and mortality particu-
larly in sub-Saharan Africa [59]. Studies in Uganda have
shown that developing paradoxical cryptococcal IRIS dou-
bles the risk of death in CM patients [7]. Diagnostic
workup (including lumbar puncture [LP]) is targeted at
excluding alternative diagnoses including cryptococcal
relapse or an additional neuroinfection. A CT head scan
should be performed in patients with focal neurological
signs as cerebral mass lesions may develop in cryptococcal
IRIS [4]. It is advisable to restart induction phase antifungal
therapy (with the more fungicidal amphotericin B where
feasible) in severe cases, in those with positive cerebrospinal
fluid (CSF) culture, and where antifungal therapy has been
suboptimal [4].
Pressure measurement and therapeutic drainage of CSF
by repeated LP in those with raised intracranial pressure is
recommended as part of the management of CM [60].
Given that raised intracranial pressure is even more common
in patients with CM-IRIS (present in three-quarters or more
[56, 57]), similar emphasis should be placed on pressure
control in IRIS. We follow the pressure control strategy
advised in the 2010 Infectious Diseases Society of America
guidelines. Opening pressure should be measured at presen-
tation and if 25 cm of CSF therapeutic drainage should be
performed to reduce the pressure by 50 % if it is extremely
high or to 20 cm of CSF. Patients with symptoms and
persistently elevated pressures should have daily therapeutic
drainage until opening pressure is within normal limits.
Temporary percutaneous lumbar drains or ventriculoperito-
neal shunts are occasionally required for refractory-raised
pressure [60].
Many clinicians advocate the use of corticosteroids in
cryptococcal IRIS, and there are reports of symptom im-
provement [6163]. However, there is no clinical trial data
and ideally their use should be delayed until cryptococcal
relapse has been excluded. For ongoing symptoms or life-
threatening neurological impairment we suggest using 0.5
1 mg/kg/day of prednisone (or equivalent) for 26 weeks
with duration dependent on clinical response. ART should
be continued. There are case reports of cryptococcal IRIS
treated with other immunomodulatory agents, such as
NSAIDs [22], thalidomide [62], and azathioprine [64]. Al-
though it seems reasonable to use NSAIDs to treat symptoms
such as headache, the use of more potent immunosuppressive
drugs should probably be reserved for those not responsive to
corticosteroids and pressure control.
Management of Cytomegalovirus Immune Recovery
Uveitis
Immune recovery uveitis (IRU) occurs in 37.7 % (95 %
CrI=26.649.4) of patients with previously diagnosed cyto-
megalovirus (CMV) retinitis [65]. The clinical spectrum of
IRU ranges from asymptomatic vitritis, through mild tran-
sient symptomatic vitritis, to persistent uveitis with floaters,
decreased vision, cystoid macular edema (CME), and epi-
retinal membrane formation [66].
Treatment varies according to disease severity [66]. It is
suggested that eyes with mild CME with visual acuity more
Curr HIV/AIDS Rep (2012) 9:238250 243
than 20/30 could be observed without treatment [67]. Local
repository corticosteroid injections (most commonly admin-
istered to the orbital floor or sub-Tenon space) result in
improved vision and decreased inflammation in more severe
cases [6773]. Sub-Tenon triamcinolone for severe uveitis
including CME, vitritis, and papillitis, resulted in improved
vision in 9/10 patients treated [71]. El-Bradey et al. [67]
reported improved vitritis with decline in inflammatory cells
in 60 % of eyes treated with sub-Tenon methylprednisolone,
but vision improved in only 40 % of eyes. Intravitreal
corticosteroids may be a safe alternative to periorbital corti-
costeroids [7476]. Morrison et al. [74] reported significant
improvement in vision and decrease in macular edema at 1-
and 3-month follow-up in eight eyes with IRU treated with
one or more intravitreal triamcinolone injections. Although
infrequently reported, repository corticosteroids carry the
risk of CMV reactivation [77, 78]. It has been suggested
that patients receiving intravitreal corticosteroids be covered
with oral valganciclovir (or intravenous ganciclovir) to pro-
tect against CMV reactivation [74]. IRU has also been
treated with NSAIDs [68, 72, 73, 75], topical corticosteroids
[69, 73, 75], and systemic corticosteroids [68, 70]. Oral
acetazolamide may be effective in treating CME, but its
use is limited by side effects [68, 69]. In severe cases,
surgery may be required for vision-threatening complica-
tions such as epiretinal membrane formation, cataracts, pro-
liferative vitreoretinopathy, and retinal detachment [67, 68,
74, 75]. IRU is not an indication for stopping ART.
Management of Progressive Multifocal
LeukoencephalopathyIRIS
Progressive multifocal leukoencephalopathy (PML) is a de-
myelinating condition caused by reactivation of the JC
polyomavirus (JCV). PML-IRIS presents as newly diag-
nosed inflammatory PML or an inflammatory reaction at
the site of previously diagnosed PML soon after ART initi-
ation [79]. The pathological inflammatory response is often,
but not invariably, reflected by gadolinium enhancement of
lesions on MRI, which is not a feature of PML lesions
outside of the context of IRIS [80, 81, 8284]. Features
of intense inflammation may be observed on brain biopsy
specimens [85, 86].
There is currently no known antiviral agent effective
against JCV, which makes this form of IRIS one of the most
difficult to manage [79, 87]. The goal of treatment in HIV-
associated PML is the restoration of the host immune re-
sponse to infection through ART. However, in patients with
PML-IRIS temporary discontinuation of ART may decrease
inflammation and result in temporary clinical improvement.
Stopping ART for 23 weeks, with [79, 88] or without [86]
simultaneous corticosteroid treatment, has anecdotally been
associated with good outcome during follow-up [79, 86,
88], but interrupting ART carries the same risks as described
above and IRIS may recur upon re-initiation.
The use of corticosteroids in PML-IRIS is controversial
but may be indicated in some patients, particularly those
with severe progressive inflammatory disease [89, 90]. In a
systematic review, Tan et al. [81] reported good neurolog-
ical recovery in 7/12 patients who received corticosteroids
for PML-IRIS, while 5 died. Corticosteroids were usually
prescribed for severe neurological deterioration or when
there was evidence of inflammation on neuroimaging.
Those who survived received corticosteroids earlier after
IRIS diagnosis compared to those who did not (mean: 3 vs
12 weeks after diagnosis). Features of inflammation includ-
ing contrast enhancement of lesions on MRI [81, 91] and
increased CSF lymphocyte count and protein concentrations
[80] have been associated with improved survival in PML.
Therefore, some authors argue that the inflammatory re-
sponse in PML is predominantly protective [83, 92] and
that corticosteroid treatment should be reserved for patients
with clinical or radiological signs of impending brain herni-
ation due to cerebral edema [93]. Studies to better define the
role of corticosteroids and alternative management strate-
gies are required.
Management of Kaposis SarcomaIRIS
Although ART usually results in resolution of cutaneous KS
[94], there are a number of reports of rapid deterioration on
ART consistent with IRIS [9597]. In a Mozambiquean ART
cohort, 5.8 % developed KS-IRIS (paradoxical or unmasking)
after a median of 14 weeks on ART [98]; 31 % of those with
KS prior to ART developed paradoxical KS-IRIS, similar to
findings from North America [20]. Features include increase
in number or size of skin lesions, ulceration, limb edema, and
mucosal involvement [95, 97, 98, 99]. Visceral involvement
is also described. Although this is usually with worsening skin
KS it has also been reported in the absence of, or during
regression of, cutaneous disease [99, 100].
Optimal treatment of KS-IRIS is based on expert opinion
rather than clinical trials. In contrast to other forms of IRIS,
corticosteroids are not recommended as their use has resulted
in new KS presentation and worsening [101103]. In patients
with severe cutaneous KS-IRIS or visceral involvement there
are several reports of response to systemic chemotherapy with
agents such as doxorubicin, bleomycin, and vincristine [98,
99]. Early systemic chemotherapy is reported to be effective in
suppressing IRIS-associated flares that are rapidly progressive
[99]. Multiple cycles are required. Localized radiotherapy
may also be required [95, 97]. ART should be continued
during this time. Despite access to such treatments, mortality
rates up to 25 %32 % are reported [98, 99], mainly attrib-
uted to pulmonary KS [99]. There is also a report of successful
treatment with IFN- [104].
244 Curr HIV/AIDS Rep (2012) 9:238250
Management of Hepatitis B and Hepatitis C IRIS
Liver enzyme elevation (LEE) is common on ART. Patients
co-infected with hepatitis B (HBV) or hepatitis C (HCV) are
at increased risk, with reports suggesting that approximately
one-third develop significant LEE (alanine aminotransferase
>5 x upper limit of normal, or 3 x upper limit of normal if
symptomatic) [105107]. Occasionally, more severe liver
dysfunction can develop, leading to hepatic decompensation
and fulminant hepatic failure [108, 109].
There are several possible causes of LEE in HBV/HCV
co-infected patients, the most important being DILI (due to
ART or other drugs) and immune-mediated flares related to
IRIS directed at the hepatitis virus [3, 110112]. Differenti-
ating these conditions can be difficult. While conversion of
serological markers (including HepBeAg and HepBsAg)
and changes in HBV-DNA viral load have been associated
with HBV-IRIS flares, findings have not been consistent and
not studied in large enough numbers to establish their diag-
nostic utility [110, 113115]. If significant LEE occurs, a
pragmatic approach is to stop non-ART hepatotoxic drugs,
exclude alternative causes, and alter ART to minimize ex-
posure to agents with the highest risk for hepatotoxicity
(particularly nevirapine) [111]. Any change in ART regimen
in HBV co-infected patients must ensure that anti-HBV
activity is maintained [116]. Liver function tests and clinical
status should be monitored closely and liver biopsy consid-
ered if there is no improvement [110, 112]. If hepatic de-
compensation develops then ART must be temporarily
halted. In patients with HBV co-infection an HBV active
drug should be continued to prevent viral rebound and
further deterioration. A re-trial of ART should be considered
when liver enzymes are normalizing and HBV-DNA is
falling [111].
The use of corticosteroids or other immunosuppressive
agents is not advised, as they have been associated with
increased viral replication and worsening of hepatic func-
tion. In the most extreme instances this has led to fulminant
hepatic failure requiring liver transplantation [117119].
Some authors have proposed controlling HBV replication
prior to ART to prevent IRIS in high-risk patients (eg, those
with underlying cirrhosis or high HBV viral loads) [108,
111, 120]. Care must be taken to avoid the generation of
HIV resistance with HBV agents with such a strategy.
Future Directions in IRIS Treatment and Research
While symptom benefit from corticosteroids and NSAIDs is
reported for many forms of IRIS, their mechanism of action
likely reflects suppression of effector responses [30] not an
alteration of the underlying pathogenic process or natural
history. Often when these treatments are discontinued IRIS
symptoms relapse [11, 28, 48]. Corticosteroids are not
always effective [121]. Other treatments remain experi-
mental. A number of other immunomodulatory agents
have been used to treat IRIS in limited numbers of
patients, including thalidomide, pentoxifylline, hydroxy-
chloroquine, montelukast, and azathioprine, with variable
reports of benefit [64, 122]. In the case of prolonged IRIS
such treatments could spare patients the cumulative adverse
effects of corticosteroids [64].
TB-IRIS has been associated with elevations of a range
of proinflammatory cytokines and chemokines of both lym-
phoid and myeloid origin, most consistently IL-6, TNF-,
and IFN- [123], and cryptococcal-IRIS with elevations of
IL-6, IL-7, IL-8, IL-17, IFN-, G-CSF, and granulocyte-
macrophage colony-stimulating factor [7]. It has been
suggested that these cytokines play a role in pathogenesis
and that blocking pathways of the major cytokines implicat-
ed may be a therapeutic strategy. The TNF- blocker inflix-
imab has been used successfully in the treatment of
refractory CNS TB paradoxical reaction [124]. The IL-6
blocker tocilizumab is now used to treat rheumatoid arthritis
[125] and in theory might be beneficial in TB-IRIS given
the associated IL-6 elevation, but there are no case reports.
Cost and adverse effects related to immunosuppression are
issues that may prevent the use of biologicals for IRIS
treatment. There is a need for studies to define immunolog-
ical and pathogen factors associated with prolonged IRIS
that could help in targeting interventions aimed at prevent-
ing and treating prolonged IRIS.
The ongoing CADIRIS trial (http://clinicaltrials.gov/ct2/
show/NCT00988780) is investigating maraviroc (for its
chemokine receptor CCR5 blocking activity) as an IRIS
prevention strategy. It could be further investigated as an
IRIS treatment option as CCR5 blockade reduces leukocyte
recruitment to sites of inflammation including the CNS.
There is one case report of a patient with PML-IRIS
responding to the addition of maraviroc [126]. Statins have
been proposed as a potential treatment given their anti-
inflammatory effects on inflammatory signaling pathways
and mediators [127]. Further research to better understand
the immunopathogenesis of IRIS will help define novel
treatment strategies that could be taken forward to clinical
evaluation. More comparative clinical trials of IRIS man-
agement strategies are required.
Conclusions
Appropriate management of IRIS requires recognition of the
condition and exclusion of differential diagnoses, particu-
larly additional infections and OI drug resistance. Because
of the heterogeneity of IRIS in terms of the underlying
infection, clinical presentation, and severity, management
Curr HIV/AIDS Rep (2012) 9:238250 245
needs to be individualized. Treatment of the underlying OI
should be optimized. Corticosteroids and NSAIDs provide
symptom relief and there is clinical trial evidence demonstrat-
ing that prednisone reduces morbidity in paradoxical TB-IRIS.
Most clinicians use corticosteroids for life-threatening forms of
mycobacterial and fungal IRIS. We also use corticosteroids in
other cases of paradoxical TB-IRIS with significant symptoms
based on the findings of the randomized controlled trial. Cor-
ticosteroids are generally avoided in viral forms of IRIS.
Exceptions are local corticosteroids for CMV IRU and system-
ic corticosteroids for life-threatening PML-IRIS complicated
by cerebral edema. Corticosteroids have potential complica-
tions and should only be used when the diagnosis of IRIS is
certain; otherwise, their use should be deferred pending further
investigation given that most IRIS is self-limiting. NSAIDs are
largely used for milder IRIS. ARTshould be interrupted only if
IRIS is imminently life-threatening.
Acknowledgments G. Meintjes was funded in part through a
Fogarty International Center South African TB/AIDS Training Award
(NIH/FIC 1U2RTW007373-01A1, U2RTW007370 ICORTA). J.
Scriven, G. Meintjes and Suzaan Marais are funded by the Wellcome
Trust.
Disclosure Conflicts of interest: G. Meintjes is a senior clinical
consultant for the Aid for AIDS Managed Care Group and has received
a lecture fee paid by Sanofi-Aventis; J. Scriven: none; S. Marais: none.
References
Papers of particular interest, published recently, have been
highlighted as:
Of importance
Of major importance
1. French MA, Lenzo N, John M, et al. Immune restoration disease
after the treatment of immunodeficient HIV-infected patients with
highly active antiretroviral therapy. HIV Med. 2000;1:10715.
2. Haddow LJ, Easterbrook PJ, Mosam A, et al. Defining immune
reconstitution inflammatory syndrome: evaluation of expert opin-
ion versus 2 case definitions in a South African cohort. Clin
Infect Dis. 2009;49:142432.
3. Ratnam I, Chiu C, Kandala NB, Easterbrook PJ. Incidence and
risk factors for immune reconstitution inflammatory syndrome in
an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis.
2006;42:41827.
4. Haddow LJ, Colebunders R, Meintjes G, et al. Cryptococcal
immune reconstitution inflammatory syndrome in HIV-1-infected
individuals: proposed clinical case definitions. Lancet Infect Dis.
2010;10:791802. Consenus case definitions for diagnosing
cryptococcal IRIS proposed by the International Network for
the Study of HIV-associated IRIS (INSHI).
5. Meintjes G, Lawn SD, Scano F, et al. Tuberculosis-associated
immune reconstitution inflammatory syndrome: case definitions
for use in resource-limited settings. Lancet Infect Dis.
2008;8:51623.
6. Burman W, Weis S, Vernon A, et al. Frequency, severity and
duration of immune reconstitution events in HIV-related tubercu-
losis. Int J Tuberc Lung Dis. 2007;11:12829.
7. Boulware DR, Meya DB, Bergemann TL, et al. Clinical
features and serum biomarkers in HIV immune reconstitution
inflammatory syndrome after cryptococcal meningitis: a pro-
spective cohort study. PLoS Med. 2010;7:e1000384. A prospec-
tive cohort study conducted in Uganda of patients with CM. A
total of 45 % developed paradoxical cryptococcal IRIS after
starting ART. The risk of mortality was doubled in those who
developed IRIS. A detailed analysis of biomarkers predictive of
and associated with IRIS was performed.
8. Muller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M.
Immune reconstitution inflammatory syndrome in patients start-
ing antiretroviral therapy for HIV infection: a systematic review
and meta-analysis. Lancet Infect Dis. 2010;10:25161.
9. Pepper DJ, Marais S, Maartens G, et al. Neurologic manifes-
tations of paradoxical tuberculosis-associated immune reconsti-
tution inflammatory syndrome: a case series. Clin Infect Dis.
2009;48:e96107.
10. Lawn SD, Meintjes G. Pathogenesis and prevention of immune
reconstitution disease during antiretroviral therapy. Expert Rev
Anti Infect Ther. 2011;9:41530. A recently published review
article that covered the immunopathogenesis of IRIS and strat-
egies to prevent both unmasking and paradoxical forms of
IRIS. The review focused particularly on IRIS associated with
mycobacterial infections, cryptococcosis, and CMV.
11. Meintjes G, Wilkinson RJ, Morroni C, et al. Randomized
placebo-controlled trial of prednisone for paradoxical
tuberculosis-associated immune reconstitution inflammatory syn-
drome. AIDS. 2010;24:238190. The first clinical trial to assess a
treatment for IRIS. A total of 110 patients with paradoxical TB-IRIS
were enrolled in this randomised placebo-controlled trial of a 4-
week course of prednisone. Prednisone resulted in reduction in
hospitalization and outpatient therapeutic procedures without
an excess of severe infections or metabolic complications.
12. Lehloenya R, Meintjes G. Dermatologic manifestations of the
immune reconstitution inflammatory syndrome. Dermatol Clin.
2006;24:54970. vii.
13. Meintjes G, Rangaka MX, Maartens G, et al. Novel relationship
between tuberculosis immune reconstitution inflammatory syn-
drome and antitubercular drug resistance. Clin Infect Dis.
2009;48:66776.
14. Adcock IM. Glucocorticoid-regulated transcription factors. Pulm
Pharmacol Ther. 2001;14:2119.
15. Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids
new mechanisms for old drugs. N Eng J Med. 2005;353:171123.
16. Payne DN, Adcock IM. Molecular mechanisms of corticosteroid
actions. Paediatr Respir Rev. 2001;2:14550.
17. Zen M, Canova M, Campana C, et al. The kaleidoscope of glucorti-
coid effects on immune system. Autoimmun Rev. 2011;10:30510.
18. Briel M, Bucher HC, Boscacci R, Furrer H. Adjunctive cortico-
steroids for Pneumocystis jiroveci pneumonia in patients with
HIV-infection. Cochrane Database Syst Rev 2006:CD006150.
19. Hakim JG, Ternouth I, Mushangi E, Siziya S, Robertson V,
Malin A. Double blind randomised placebo controlled trial of
adjunctive prednisolone in the treatment of effusive tubercu-
lous pericarditis in HIV seropositive patients. Heart.
2000;84:1838.
20. Achenbach CJ, Harrington RD, Dhanireddy S, Crane HM, Casper
C, Kitahata MM. Paradoxical immune reconstitution inflammatory
syndrome in HIV-infected patients treated with combination anti-
retroviral therapy after AIDS-defining opportunistic infection. Clin
Infect Dis. 2012;54:42433. A retrospective cohort study of 196
patients who started ART after a diagnosis of an AIDS-defining OI
in the US. A total of 11 % developed paradoxical IRIS. Treatment
246 Curr HIV/AIDS Rep (2012) 9:238250
and outcome are reported. Morbidity and mortality were highest in
those with visceral KS-IRIS.
21. Kumarasamy N, Chaguturu S, Mayer KH, et al. Incidence of
immune reconstitution syndrome in HIV/tuberculosis-coinfected
patients after initiation of generic antiretroviral therapy in India. J
Acquir Immune Defic Syndr. 2004;37:15746.
22. Manfredi R, Pieri F, Pileri SA, Chiodo F. The changing face of
AIDS-related opportunism: cryptococcosis in the highly active
antiretroviral therapy (HAART) era. Case reports and literature
review. Mycopathologia. 1999;148:738.
23. Kaplan JE, Benson C, Holmes KH, Brooks JT, Pau A, Masur H.
Guidelines for prevention and treatment of opportunistic infec-
tions in HIV-infected adults and adolescents: recommendations
from CDC, the National Institutes of Health, and the HIV Med-
icine Association of the Infectious Diseases Society of America.
MMWR Recomm Rep. 2009;58:1207.
24. Nelson MR, Katlama C, Montaner JS, et al. The safety of
tenofovir disoproxil fumarate for the treatment of HIV infection
in adults: the first 4 years. AIDS. 2007;21:127381.
25. Morelle J, Labriola L, Lambert M, Cosyns JP, Jouret F, Jadoul M.
Tenofovir-related acute kidney injury and proximal tubule dys-
function precipitated by diclofenac: a case of drug-drug interac-
tion. Clin Nephrol. 2009;71:56770.
26. Thwaites GE, Nguyen DB, Nguyen HD, et al. Dexamethasone for
the treatment of tuberculous meningitis in adolescents and adults.
N Engl J Med. 2004;351:174151.
27. Strang JI, Kakaza HH, Gibson DG, Girling DJ, Nunn AJ, Fox W.
Controlled trial of prednisolone as adjuvant in treatment of tuber-
culous constrictive pericarditis in Transkei. Lancet. 1987;2:1418
22.
28. Breen RA, Smith CJ, Bettinson H, et al. Paradoxical reactions
during tuberculosis treatment in patients with and without HIV
co-infection. Thorax. 2004;59:7047.
29. McAllister WA, Thompson PJ, Al-Habet SM, Rogers HJ. Rifampicin
reduces effectiveness and bioavailability of prednisolone. Br Med J
(Clin Res Ed). 1983;286:9235.
30. Meintjes G, Skolimowska KH, Wilkinson KA, Matthews K,
Tadokera R, Conesa-Botella A, Seldon R, Rangaka MX, Rebe
K, Pepper DJ, Morroni C, Colebunders R, Maartens G, Wilkinson
RJ. Corticosteroid modulated immune activation in the TB immune
reconstitution inflammatory syndrome. AmJ Respir Crit Care Med.
2012. doi:10.1164/rccm.201201-00940c.
31. Michailidis C, Pozniak AL, Mandalia S, Basnayake S, Nel-
son MR, Gazzard BG. Clinical characteristics of IRIS syn-
drome in patients with HIV and tuberculosis. Antivir Ther.
2005;10:41722.
32. Olalla J, Pulido F, Rubio R, et al. Paradoxical responses in a
cohort of HIV-1-infected patients with mycobacterial disease. Int
J Tuberc Lung Dis. 2002;6:715.
33. Breton G, Duval X, Estellat C, et al. Determinants of immune
reconstitution inflammatory syndrome in HIV type 1-infected
patients with tuberculosis after initiation of antiretroviral therapy.
Clin Infect Dis. 2004;39:170912.
34. Lawn SD, Wood R. Hepatic involvement with tuberculosis-
associated immune reconstitution disease. AIDS. 2007;21:23623.
35. Meintjes G, Sonderup MW. A practical approach to the diagnosis
and management of paradoxical tuberculosis immune reconstitution
inflammatory syndrome. Contin Med Educ. 2011;29(10):4107.
36. Torok ME, Yen NT, Chau TT, et al. Timing of initiation of
antiretroviral therapy in human immunodeficiency virus (HIV)
associated tuberculous meningitis. Clin Infect Dis. 2011;52:1374
83. This is the only published randomised controlled trial to com-
pare early versus delayed ART in patients with HIV-associated
TBM. Mortality was ~60 % and no different in the two arms of
the trial (those who started ART within 7 days of TB treatment and
those who started ARTafter 2 months of TB treatment). Participants
in both arms of the trial received adjunctive dexamethasone for 6
8 weeks.
37. Asselman V, Thienemann F, Pepper DJ, et al. Central nervous
system disorders after starting antiretroviral therapy in South
Africa. AIDS. 2010;24:28716.
38. Torok ME, Kambugu A, Wright E. Immune reconstitution dis-
ease of the central nervous system. Curr Opin HIV AIDS.
2008;3:43845.
39. Dautremer J, Pacanowski J, Girard PM, Lalande V, Sivignon
F, Meynard JL. A new presentation of immune reconstitution
inflammatory syndrome followed by a severe paradoxical reaction
in an HIV-1-infected patient with tuberculous meningitis. AIDS.
2007;21:3812.
40. Tuon FF, Mulatti GC, Pinto WP, de Siqueira Franca FO,
Gryschek RC. Immune reconstitution inflammatory syndrome
associated with disseminated mycobacterial infection in
pa t i ent s wi t h AI DS. AI DS Pa t i e nt Ca r e STDS.
2007;21:52732.
41. Lee CH, Lui CC, Liu JW. Immune reconstitution syndrome in a
patient with AIDS with paradoxically deteriorating brain tuber-
culoma. AIDS Patient Care STDS. 2007;21:2349.
42. Manosuthi W, Kiertiburanakul S, Phoorisri T, Sungkanuparph S.
Immune reconstitution inflammatory syndrome of tuberculosis
among HIV-infected patients receiving antituberculous and anti-
retroviral therapy. J Infect. 2006;53:35763.
43. Rajeswaran G, Becker JL, Michailidis C, Pozniak AL, Padley SP.
The radiology of IRIS (immune reconstitution inflammatory syn-
drome) in patients with mycobacterial tuberculosis and HIV co-
infection: appearances in 11 patients. Clin Radiol. 2006;61:833
43.
44. Crump JA, Tyrer MJ, Lloyd-Owen SJ, Han LY, Lipman MC,
Johnson MA. Miliary tuberculosis with paradoxical expansion of
intracranial tuberculomas complicating human immunodeficien-
cy virus infection in a patient receiving highly active antiretrovi-
ral therapy. Clin Infect Dis. 1998;26:10089.
45. Vidal JE, Cimerman S, Schiavon Nogueira R, et al. Paradox-
ical reaction during treatment of tuberculous brain abscess in
a patient with AIDS. Rev Inst Med Trop Sao Paulo.
2003;45:1778.
46. Lipman M, Breen R. Immune reconstitution inflammatory syn-
drome in HIV. Curr Opin Infect Dis. 2006;19:205.
47. World Health Organisation. Improving the diagnosis and treat-
ment of smear-negative pulmonary and extrapulmonary tubercu-
losis among adults and adolescents. Recommendations for HIV-
prevalent resource-constrained settings. Geneva: WHO Press;
2006.
48. Phillips P, Bonner S, Gataric N, et al. Nontuberculous mycobac-
terial immune reconstitution syndrome in HIV-infected patients:
spectrum of disease and long-term follow-up. Clin Infect Dis.
2005;41:148397.
49. Riddell J, Kaul DR, Karakousis PC, Gallant JE, Mitty J, Kazanjian
PH. Mycobacterium avium complex immune reconstitution
inflammatory syndrome: long term outcomes. J Transl Med.
2007;5:50.
50. Desimone Jr JA, Babinchak TJ, Kaulback KR, Pomerantz RJ.
Treatment of Mycobacterium avium complex immune reconsti-
tution disease in HIV-1-infected individuals. AIDS Patient Care
STDS. 2003;17:61722.
51. Benson CA, Williams PL, Currier JS, et al. A prospective, ran-
domized trial examining the efficacy and safety of clarithromycin
in combination with ethambutol, rifabutin, or both for the treat-
ment of disseminated Mycobacterium avium complex disease in
persons with acquired immunodeficiency syndrome. Clin Infect
Dis. 2003;37:123443.
52. Cinti SK, Kaul DR, Sax PE, Crane LR, Kazanjian PH. Recurrence
of Mycobacterium avium infection in patients receiving highly
Curr HIV/AIDS Rep (2012) 9:238250 247
active antiretroviral therapy and antimycobacterial agents. Clin
Infect Dis. 2000;30:5114.
53. Lee YC, Lu CL, Lai CC, Tseng YT, Sun HY, Hung CC. Myco-
bacterium avium complex infection-related immune reconstitu-
tion inflammatory syndrome of the central nervous system in an
HIV-infected patient: Case report and review. J Microbiol Immu-
nol Infect. 2012 Jan 6. [Epub ahead of print].
54. Jenny-Avital ER. A patient with refractory disseminated Myco-
bacterium avium after immune-reconstitution localized MAC.
AIDS Clin Care. 2003;15:246.
55. Sungkanuparph S, Filler Scott G, Chetchotisakd P, et al.
Cryptococcal immune reconstitution inflammatory syndrome
after antiretroviral therapy in AIDS patients with cryptococcal
meningitis: a prospective multicenter study. Clin Infect Dis.
2009;49:9314.
56. Shelburne SA, Darcourt J, White AC, et al. The role of immune
reconstitution inflammatory syndrome in AIDS-related Crypto-
coccus neoformans disease in the era of highly active antiretro-
viral therapy. Clin Infect Dis. 2005;40:104952.
57. Bicanic T, Meintjes G, Rebe K, et al. Immune reconstitution
inflammatory syndrome in HIV-associated cryptococcal meningitis:
a prospective study. J Acquir Immune Defic Syndr. 2009;51:1304.
A prospective cohort study of CMpatients in South Africa reporting
an IRIS incidence of 17 %. IRIS management and patient outcomes
are described. In this study CM-IRIS was not associated with excess
mortality.
58. Boulware DR, Bonham SC, Meya DB, et al. Paucity of initial
cerebrospinal fluid inflammation in cryptococcal meningitis is
associated with subsequent immune reconstitution inflammatory
syndrome. J Infect Dis. 2010;202:96270.
59. Lawn SD, Bekker L-G, Myer L, Orrell C, Wood R. Cryptococcocal
immune reconstitution disease: a major cause of early mortality in a
South African antiretroviral programme. AIDS. 2005;19:20502.
60. Perfect John R, Dismukes William E, Dromer F, et al. Clinical
practice guidelines for the management of cryptococcal disease:
2010 update by the infectious diseases society of America. Clin
Infect Dis. 2010;50:291322. The most recent Infectious Dis-
eases Society of America guidelines for managing cryptococcal
disease. These include recommendations on the management of
elevated intracranial pressure in CM and use of corticosteroids in
IRIS.
61. King MD, Perlino CA, Cinnamon J, Jernigan JA. Paradoxical
recurrent meningitis following therapy of cryptococcal meningi-
tis: an immune reconstitution syndrome after initiation of highly
active antiretroviral therapy. Int J STD AIDS. 2002;13:7246.
62. Lortholary O, Fontanet A, Mmain N, et al. Incidence and
risk factors of immune reconstitution inflammatory syndrome
complicating HIV-associated cryptococcosis in France. AIDS.
2005;19:10439.
63. Venkataramana A, Pardo CA, McArthur JC, et al. Immune re-
constitution inflammatory syndrome in the CNS of HIV-infected
patients. Neurology. 2006;67:3838.
64. Scourfield A, Waters L, Tittle V, Martin T, Rockwood N, Gazzard
B, Bower M, Nelson M. Azathioprine use as a novel treatment for
cryptococcal immune reconstitution and inflammatory syndrome
in HIV. 17th Annual Conference of the British HIVAssociation,
Bournmouth, 2011, abstract P92.
65. Muller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger
M. Immune reconstitution inflammatory syndrome in patients
starting antiretroviral therapy for HIV infection: a systematic
review and meta-analysis. Lancet Infect Dis. 2010;10:25161. A
systematic review and meta-analysis of the incidence and mor-
tality associated with IRIS. A total of 16 % of unselected patients
who started ART developed any kind of IRIS. The highest inci-
dence of paradoxical IRIS was in patients with CMV retinitis at
ART initiation. IRIS was associated with 21 % mortality in CM.
66. Stewart MW. Optimal management of cytomegalovirus retinitis in
patients with AIDS. Clin Ophthalmol. 2010;4:28599. A compre-
hensive review of the currently available treatments for CMV reti-
nitis. Advantages and disadvantages of various treatment options as
well as their use in different socioeconomic settings are discussed.
67. El-Bradey MH, Cheng L, Song MK, Torriani FJ, Freeman WR.
Long-term results of treatment of macular complications in eyes
with immune recovery uveitis using a graded treatment approach.
Retina. 2004;24:37682.
68. Karavellas MP, Azen SP, MacDonald JC, et al. Immune recovery
vitritis and uveitis in AIDS: clinical predictors, sequelae, and
treatment outcomes. Retina. 2001;21:19.
69. Henderson HW, Mitchell SM. Treatment of immune recovery
vitritis with local steroids. Br J Ophthalmol. 1999;83:5405.
70. Karavellas MP, Lowder CY, Macdonald C, Avila Jr CP, Freeman
WR. Immune recovery vitritis associated with inactive cytomega-
lovirus retinitis: a newsyndrome. Arch Ophthalmol. 1998;116:169
75.
71. Arevalo JF, Mendoza AJ, Ferretti Y. Immune recovery uveitis in
AIDS patients with cytomegalovirus retinitis treated with highly
active antiretroviral therapy in Venezuela. Retina. 2003;23:495
502.
72. Zegans ME, Walton RC, Holland GN, ODonnell JJ, Jacobson MA,
Margolis TP. Transient vitreous inflammatory reactions associated
with combination antiretroviral therapy in patients with AIDS and
cytomegalovirus retinitis. Am J Ophthalmol. 1998;125:292300.
73. Lin YC, Yang CH, Lin CP, et al. Cytomegalovirus retinitis and
immune recovery uveitis in AIDS patients treated with highly
active antiretroviral therapy in Taiwanese. Ocul Immunol Inflamm.
2008;16:837.
74. Morrison VL, Kozak I, LaBree LD, Azen SP, Kayicioglu OO,
Freeman WR. Intravitreal triamcinolone acetonide for the treat-
ment of immune recovery uveitis macular edema. Ophthalmol-
ogy. 2007;114:3349.
75. Sirimaharaj M, Robinson MR, Zhu M, et al. Intravitreal injection
of triamcinolone acetonide for immune recovery uveitis. Retina.
2006;26:57880.
76. Hu J, Coassin M, Stewart JM. Fluocinolone acetonide implant
(Retisert) for chronic cystoid macular edema in two patients with
AIDS and a history of cytomegalovirus retinitis. Ocul Immunol
Inflamm. 2011;19:2069.
77. Ufret-Vincenty RL, Singh RP, Lowder CY, Kaiser PK. Cytomega-
lovirus retinitis after fluocinolone acetonide (Retisert) implant. Am
J Ophthalmol. 2007;143:3345.
78. Dalessandro L, Bottaro E. Reactivation of CMV retinitis after
treatment with subtenon corticosteroids for immune recovery
uveitis in a patient with AIDS. Scand J Infect Dis. 2002;34:7802.
79. Tan CS, Koralnik IJ. Progressive multifocal leukoencephalopathy
and other disorders caused by JC virus: clinical features and
pathogenesis. Lancet Neurol. 2010;9:42537.
80. Harrison DM, Newsome SD, Skolasky RL, McArthur JC, Nath
A. Immune reconstitution is not a prognostic factor in progressive
multifocal leukoencephalopathy. J Neuroimmunol. 2011;238:81
6.
81. Tan K, Roda R, Ostrow L, McArthur J, Nath A. PML-IRIS in
patients with HIV infection: clinical manifestations and treatment
with steroids. Neurology. 2009;72:145864. A case series and
retrospective review of the literature reporting 54 patients with
PML-IRIS. The clinical manifestations and outcomes of patients
treated with and without corticosteroids are reported.
82. Tantisiriwat W, Tebas P, Clifford DB, Powderly WG, Fichtenbaum
CJ. Progressive multifocal leukoencephalopathy in patients with
AIDS receiving highly active antiretroviral therapy. Clin Infect
Dis. 1999;28:11524.
83. Thurnher MM, Post MJ, Rieger A, Kleibl-Popov C, Loewe C,
Schindler E. Initial and follow-up MR imaging findings in AIDS-
248 Curr HIV/AIDS Rep (2012) 9:238250
related progressive multifocal leukoencephalopathy treated with
highly active antiretroviral therapy. Am J Neuroradiol.
2001;22:97784.
84. Falco V, Olmo M, del Saz SV, et al. Influence of HAART on
the clinical course of HIV-1-infected patients with progressive
multifocal leukoencephalopathy: results of an observational
mul t i cent er st udy. J Acqui r Immune Def i c Syndr.
2008;49:2631.
85. Miralles P, Berenguer J, Lacruz C, et al. Inflammatory reactions
in progressive multifocal leukoencephalopathy after highly active
antiretroviral therapy. AIDS. 2001;15:19002.
86. Hoffmann C, Horst HA, Albrecht H, Schlote W. Progressive
multifocal leucoencephalopathy with unusual inflammatory re-
sponse during antiretroviral treatment. J Neurol Neurosurg Psy-
chiatry. 2003;74:11424.
87. Marshall LJ, Major EO. Molecular regulation of JC virus
tropism: insights into potential therapeutic targets for progressive
multifocal leukoencephalopathy. J Neuroimmune Pharmacol.
2010;5:40417.
88. Martinez JV, Mazziotti JV, Efron ED, et al. Immune re-
constitution inflammatory syndrome associated with PML
in AIDS: a treatable disorder. Neurology. 2006;67:1692
4.
89. Berger JR. Steroids for PML-IRIS: a double-edged sword?
Neurology. 2009;72:14545. An editorial that summarizes the
pros and cons of corticosteroid treatment for PML-IRIS.
90. Cinque P, Koralnik IJ, Gerevini S, Miro JM, Price RW. Progres-
sive multifocal leukoencephalopathy in HIV-1 infection. Lancet
Infect Dis. 2009;9:62536.
91. Berger JR, Levy RM, Flomenhoft D, Dobbs M. Predictive factors
for prolonged survival in acquired immunodeficiency syndrome-
associated progressive multifocal leukoencephalopathy. Ann
Neurol. 1998;44:3419.
92. Kotecha N, George MJ, Smith TW, Corvi F, Litofsky NS.
Enhancing progressive multifocal leukoencephalopathy: an
indicator of improved immune status? Am J Med. 1998;105:541
3.
93. Du Pasquier RA, Koralnik IJ. Inflammatory reaction in progres-
sive multifocal leukoencephalopathy: harmful or beneficial? J
Neurovirol. 2003;9 Suppl 1:2531.
94. Cattelan AM, Calabr ML, Gasperini P, et al. Acquired im-
munodeficiency syndrome-related Kaposis sarcoma regres-
sion after highly active antiretroviral therapy: biologic
correlates of clinical outcome. J Natl Cancer Inst Monographs
2001;449.
95. Bower M, Nelson M, Young AM, et al. Immune reconstitution
inflammatory syndrome associated with Kaposis sarcoma. J Clin
Oncol. 2005;23:52248.
96. Connick E, Kane MA, White IE, Ryder J, Campbell TB. Immune
reconstitution inflammatory syndrome associated with Kaposi
sarcoma during potent antiretroviral therapy. Clin Infect Dis.
2004;39:18525.
97. Weir A, Wansbrough-Jones M. Mucosal Kaposis sarcoma fol-
lowing protease inhibitor therapy in an HIV-infected patient.
AIDS. 1997;11:18956.
98. Letang E, Almeida JM, Mir JM, et al. Predictors of immune
reconstitution inflammatory syndrome-associated with kaposi
sarcoma in mozambique: a prospective study. J Acquir Immune
Defic Syndr. 2010;53:58997. A prospective cohort study con-
ducted in Mozambique that reports the incidence, risk factors,
management, and outcomes of KS-IRIS. The mortality in patients
with KS-IRIS was 25 %.
99. Leidner RS, Aboulafia DM. Recrudescent Kaposis sarcoma
after initiation of HAART: a manifestation of immune recon-
stitution syndrome. AIDS Patient Care STDS. 2005;19:635
44.
100. Crane HM, Deubner H, Huang JC, Swanson PE, Harrington RD.
Fatal Kaposis sarcoma-associated immune reconstitution follow-
ing HAART initiation. Int J STD AIDS. 2005;16:803.
101. Volkow PF, Cornejo P, Zinser JW, Ormsby CE, Reyes-Tern G.
Life-threatening exacerbation of Kaposis sarcoma after predni-
sone treatment for immune reconstitution inflammatory syn-
drome. AIDS. 2008;22:6635.
102. Elliott AM, Luzze H, Quigley MA, et al. A randomized, double-
blind, placebo-controlled trial of the use of prednisolone as an
adjunct to treatment in HIV-1-associated pleural tuberculosis. J
Infect Dis. 2004;190:86978.
103. Gill PS, Loureiro C, Bernstein-Singer M, Rarick MU, Sattler F,
Levine AM. Clinical effect of glucocorticoids on Kaposi sarcoma
related to the acquired immunodeficiency syndrome (AIDS). Ann
Intern Med. 1989;110:93740.
104. Ueno T, Mitsuishi T, Kimura Y, et al. Immune reconstitution
inflammatory syndrome associated with Kaposis sarcoma:
successful treatment with interferon-alpha. Eur J Dermatol.
2007;17:53940.
105. den Brinker M, Wit FW, Wertheim-van Dillen PM, et al. Hepatitis
B and C virus co-infection and the risk for hepatotoxicity of
highly active antiretroviral therapy in HIV-1 infection. AIDS.
2000;14:2895902.
106. Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hep-
atotoxicity associated with antiretroviral therapy in adults
infected with human immunodeficiency virus and the role
of hepatitis C or B virus infection. JAMA. 2000;283:74
80.
107. Wit FWNM, Weverling GJ, Weel J, Jurriaans S, Lange JMA.
Incidence of and risk factors for severe hepatotoxicity asso-
ciated with antiretroviral combination therapy. J Infect Dis.
2002;186:2331.
108. Drake A, Mijch A, Sasadeusz J. Immune reconstitution hepatitis
in HIVand hepatitis B coinfection, despite lamivudine therapy as
part of HAART. Clin Infect Dis. 2004;39:12932.
109. Murcia JM, Boix V, Merino E, Manso MI, Portilla J. Drug
toxicity or syndrome of immune restoration causing fulminant
cirrhosis after HAART-induced immune recovery. Eur J Clin
Micro Infect Dis. 2002;21:1535.
110. Carr A, Cooper DA. Restoration of immunity to chronic hepatitis
B infection in HIV-infected patient on protease inhibitor. Lancet.
1997;349:9956.
111. Crane M, Matthews G, Lewin SR. Hepatitis virus immune resto-
ration disease of the liver. Curr Opin HIVAIDS. 2008;3:44652.
112. John M, Flexman J, French MA. Hepatitis C virus-associated
hepatitis following treatment of HIV-infected patients with HIV
protease inhibitors: an immune restoration disease? AIDS.
1998;12:228993.
113. Manegold C, Hannoun C, Wywiol A, et al. Reactivation of
hepatitis B virus replication accompanied by acute hepatitis in
patients receiving highly active antiretroviral therapy. Clin Infect
Dis. 2001;32:1448.
114. Rouanet I, Peyriere H, Mauboussin JM, Terrail N, Vincent
D. Acute clinical hepatitis by immune restoration in a human
immunodeficiency virus/hepatitis B virus co-infected patient
receiving antiretroviral therapy. Eur J Gastroenterol Hepatol.
2003;15:957.
115. Velasco M, Moran A, Tellez MJ. Resolution of chronic hepatitis
B after ritonavir treatment in an HIV-infected patient. N Eng J
Med. 1999;340:17656.
116. Nesch R, Ananworanich J, Srasuebkul P, et al. Interruptions
of tenofovir/emtricitabine-based antiretroviral therapy in
patients with HIV/hepatitis B virus co-infection. AIDS.
2008;22:1524.
117. Calabrese LH, Zein NN, Vassilopoulos D. Hepatitis B virus
(HBV) reactivation with immunosuppressive therapy in rheumatic
Curr HIV/AIDS Rep (2012) 9:238250 249
diseases: assessment and preventive strategies. Ann Rheum Dis.
2006;65:9839.
118. Sagnelli E, Manzillo G, Maio G, et al. Serum levels of
hepatitis B surface and core antigens during immunosuppres-
sive treatment of HBsAg-positive chronic active hepatitis.
Lancet. 1980;2:3957.
119. McGee S, Hirschmann J. Use of corticosteroids in treating infec-
tious diseases. Arch Intern Med. 2008;168:103446.
120. Baker JV, Boulware DR, Bohjanen PR. A case for treating high
hepatitis B DNA levels before starting HIV therapy. AIDS.
2006;20:24023.
121. Hardwick C, White D, Morris E, Monteiro EF, Breen RA, Lip-
man M. Montelukast in the treatment of HIVassociated immune
reconstitution disease. Sex Transm Infect. 2006;82:5134.
122. Marais S, Wilkinson RJ, Pepper DJ, Meintjes G. Management of
patients with the immune reconstitution inflammatory syndrome.
Curr HIV/AIDS Rep. 2009;6:16271.
123. Tadokera R, Meintjes G, Skolimowska KH, et al. Hypercytokinaemia
accompanies HIV-tuberculosis immune reconstitution inflam-
matory syndrome. Eur Resp J. 2011;37:124859.
124. Blackmore TK, Manning L, Taylor WJ, Wallis RS. Therapeutic use
of infliximab in tuberculosis to control severe paradoxical reaction
of the brain and lymph nodes. Clin Infect Dis. 2008;47:e835.
125. Hennigan S, Kavanaugh A. Interleukin-6 inhibitors in the treatment
of rheumatoid arthritis. Ther Clin Risk Manag. 2008;4:76775.
126. Martin-Blondel G, Cuzin L, Delobel P, et al. Is maraviroc bene-
ficial in paradoxical progressive multifocal leukoencephalopathy-
immune reconstitution inflammatory syndrome management?
AIDS. 2009;23:25456.
127. Sun HY, Singh N. Potential role of statins for the management of
immune reconstitution syndrome. Med Hypotheses. 2011;76:30710.
128. Gallant JE, Chaisson RE, Moore RD. The effect of adjunctive corti-
costeroids for the treatment of Pneumocystis carinii pneumonia on
mortality and subsequent complications. Chest. 1998;114:125863.
250 Curr HIV/AIDS Rep (2012) 9:238250
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Emergency Rescue DrillDocument13 pagesEmergency Rescue DrillbalasubramaniamPas encore d'évaluation
- Orchestral Tools - The Orchestral Grands ManualDocument12 pagesOrchestral Tools - The Orchestral Grands ManualPiotr Weisthor RóżyckiPas encore d'évaluation
- Hoc Volume1Document46 pagesHoc Volume1nordurljosPas encore d'évaluation
- EFL Listeners' Strategy Development and Listening Problems: A Process-Based StudyDocument22 pagesEFL Listeners' Strategy Development and Listening Problems: A Process-Based StudyCom DigfulPas encore d'évaluation
- How To Use The ActionDocument3 pagesHow To Use The Actioncizgiaz cizgiPas encore d'évaluation
- LECTURE 1.COMMUNICATION PROCESSES, PRINCIPLES, AND ETHICS - Ver 2Document24 pagesLECTURE 1.COMMUNICATION PROCESSES, PRINCIPLES, AND ETHICS - Ver 2Trixia Nicole De LeonPas encore d'évaluation
- Agitha Diva Winampi - Childhood MemoriesDocument2 pagesAgitha Diva Winampi - Childhood MemoriesAgitha Diva WinampiPas encore d'évaluation
- Venue:: Alberta Electrical System Alberta Electrical System OperatorDocument48 pagesVenue:: Alberta Electrical System Alberta Electrical System OperatorOmar fethiPas encore d'évaluation
- Why The American Ruling Class Betrays Its Race and CivilizationDocument39 pagesWhy The American Ruling Class Betrays Its Race and CivilizationNinthCircleOfHellPas encore d'évaluation
- PEDIA OPD RubricsDocument11 pagesPEDIA OPD RubricsKylle AlimosaPas encore d'évaluation
- Analysis of Pipe FlowDocument14 pagesAnalysis of Pipe FlowRizwan FaridPas encore d'évaluation
- Did Angels Have WingsDocument14 pagesDid Angels Have WingsArnaldo Esteves HofileñaPas encore d'évaluation
- Black Body RadiationDocument46 pagesBlack Body RadiationKryptosPas encore d'évaluation
- 755th RSBDocument32 pages755th RSBNancy CunninghamPas encore d'évaluation
- IAB Digital Ad Operations Certification Study Guide August 2017Document48 pagesIAB Digital Ad Operations Certification Study Guide August 2017vinayakrishnaPas encore d'évaluation
- January Payslip 2023.pdf - 1-2Document1 pageJanuary Payslip 2023.pdf - 1-2Arbaz KhanPas encore d'évaluation
- Mutants & Masterminds 3e - Power Profile - Death PowersDocument6 pagesMutants & Masterminds 3e - Power Profile - Death PowersMichael MorganPas encore d'évaluation
- Propht William Marrion Branham Vist IndiaDocument68 pagesPropht William Marrion Branham Vist IndiaJoshuva Daniel86% (7)
- Living in IT Era OutputDocument6 pagesLiving in IT Era OutputDanica Rose SaludarPas encore d'évaluation
- Robert FrostDocument15 pagesRobert FrostRishi JainPas encore d'évaluation
- Channels of CommunicationDocument3 pagesChannels of CommunicationIrin ChhinchaniPas encore d'évaluation
- Danese and Romano (2011) ModerationDocument14 pagesDanese and Romano (2011) ModerationUmer NaseemPas encore d'évaluation
- Sorsogon State College: Republic of The Philippines Bulan Campus Bulan, SorsogonDocument4 pagesSorsogon State College: Republic of The Philippines Bulan Campus Bulan, Sorsogonerickson hernanPas encore d'évaluation
- Linux Command Enigma2Document3 pagesLinux Command Enigma2Hassan Mody TotaPas encore d'évaluation
- Army War College PDFDocument282 pagesArmy War College PDFWill100% (1)
- The Civil Mutinies of Romeo and Juliet: Glenn ClarkDocument21 pagesThe Civil Mutinies of Romeo and Juliet: Glenn ClarkmilcahPas encore d'évaluation
- Things in The Classroom WorksheetDocument2 pagesThings in The Classroom WorksheetElizabeth AstaizaPas encore d'évaluation
- Civil Engineering Interview QuestionsDocument19 pagesCivil Engineering Interview QuestionsSrivardhanSrbPas encore d'évaluation
- Especificação - PneusDocument10 pagesEspecificação - Pneusmarcos eduPas encore d'évaluation
- Jesus Hold My Hand EbDocument2 pagesJesus Hold My Hand EbGregg100% (3)