Académique Documents
Professionnel Documents
Culture Documents
Antrochoanal Polyp: Seung Kyu Chung, M.D
Transféré par
NurhafizahImfista0 évaluation0% ont trouvé ce document utile (0 vote)
52 vues4 pagesdefinition
Titre original
polip antrochoanal
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentdefinition
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
52 vues4 pagesAntrochoanal Polyp: Seung Kyu Chung, M.D
Transféré par
NurhafizahImfistadefinition
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
5
KISEP Review J Rhinol 7 1 , 2000
Antrochoanal Polyp
Seung Kyu Chung, M.D.
ABSTRACT
The antrochoanal polyps ACPs originate in the maxillary sinus, come to the nasal cavity usually through the accessory
opening of the maxillary sinus and extend into the nasopharynx. They occur in all ages, although show more frequency in
pediatric patients than in adults. The endoscopic removal is the modality of choice with reasonable success rate. If the ACPs
come through the accessory ostia, these openings should be connected with the natural openings.
KEY WORDS Maxillary sinusPolyp.
INTRODUCTION
Choanal polyp originated in a paranasal sinus, usually
in the maxillary sinus, and extends on a pedicle from the
middle meatus into the choana or nasopharynx, where
it may continue to enlarge. Apparently, it may arise from
any wall of the maxillary sinus and gains entrance to the
nasal fossa by way of an ostium, usually a large acces-
sory ostium. It is predominantly solitary and unilateral,
and higher incidence in pediatric population. The intra-
sinus portion is cystic, and the solid portion reaches the
nasopharynx. Two portions are connected with stalk,
which passes through the ostium. Therefore this polyps
look like a dumbbell. The cystic portion inside the sinus
may be multi-chambered.
HISTORY
A description of a polyp in the nasopharynx which
Palfyn observed in a girl in 1753 was one of the ear-
liest descriptions of the choanal polyps.
1)
In the 19th
century, a number of interesting observations of the po-
lyps in the nasopharynx were published by Semeleder
1866 , Scheck 1884 and Moldenhauer 1886 .
1)
In
1981, Zuckerkandl had an illustration of a pedicle, ori-
ginating in an antrum and passing into the nose through
a large accessory ostium, in his book. In 1906, Killian
presented a paper on the origin of the choanal polyp and
expressed the opinion that it arose from the maxillary
sinus and gained access to the nasal cavity through the
accessory ostium.
2)
In 1909, Kelly reported 15 cases of
nasoantral polyps and, in 11 of these, he opened the an-
trum using the Caldwell-Luc procedure and demonstr-
ated a connection between the lining membrane of the
sinus and the polyp.
3)
Kelly reported that in all instances
there were large accessory ostia providing ready com-
munication between the antrum and nasal fossa.
3)
EPIDEMIOLOGY
Generally, ACPs are reported to comprise 3% to 6%
of all nasal polyps.
4)
Stammberger reported that the an-
trochoanal polyps appeared to be rare, making up less
than 0.8% of all their polyp patients.
5)
Children made
up 70% of antrochoanal polyp patients in their series.
The incidence of the ACP is high in pediatric population,
as high as 28%.
6)
However, Cook, et al., reported an
incidence of 22.3% 33 of 148 of all nasal polyp pa-
tients on whom they operated during the same period. 7
Of their patients, 85% were adults. Although the ACPs
are found more often in children,
5)6)8-11)
some reports re-
veal that ACPs are more often found in adults.
1)4)7)12)13)
Cook, et al., reported the pathologic findings of the
polyps coexisting with antrochoanal polyps in adult pa-
tients. This means that the ACP may be present with
Department of Otorhinolaryngology, Head and Neck Surgery
Samsung Medical Center, Sungkyunkwan University School of
Medicine, Seoul, Korea
Address correspondence and reprint requests to Seung-Kyu
Chung, M.D., Department of Otorhinolaryngology, Samsung
Medical Center, Ilwondong 50, Kangnamku, Seoul 135-710,
Korea
Tel 82-2-3410-3572, Fax 82-2-3410-3789
E-mail skchung@smc.smsung.co.kr
Accepted for publication on May 7, 2000
6 / J Rhinol 7 1 , 2000
other polyps. If we were preoccupied with the fact that
the ACP is usually present as only one polyp, we can
miss the ACP cases that coexist with other polyposis.
Male preponderance was noted in nore than 70% of
the reports
Usually ACPs are present as a unilateral polyp, with
bilateral or unilateral nasal obstruction. However three
bilateral ACPs were reported out of 74 patients.
8)
Two
other bilateral cases were reported.
11)13)
PATHOPHYSIOLOGY
Killian found the ACP has root within the maxillary
sinus and coming through the large accessory ostium of
the maxillary sinus, with a dumbbell-like shape because
of the relatively small size of the accessory ostium.
2)
He
proposed that the ACP was at first a simple antral polyp.
Occasionally, as a result of blowing the nose, part of
ACP finds its way through the wide accessory opening
into the middle meatus. The growing stalk of the polyp
presses in turn upon the walls of the accessory ositum
and widens this entrance.
2)
There is some evidence that the lesion may start with
a cyst from the posterior wall of the maxillary sinus,
filling the maxillary sinus and eroding the medial sinus
wall by pressure, before reaching the nose usually thr-
ough the posterior fontanelle region with a stalk.
14)
They
exhibited a histologic finding of the ACPs identical to
the structure of the common intramural cyst of the ma-
xillary sinus. They suggested that the choanal polyp de-
veloped from the expanding intramural cyst protruding
through the maxillary ostium and into the nasal cavity.
The histologic finding that the ACP contains less sub-
mucous gland favors this suggestion.
4)9)
Since reports made by Killian and Kelly in the early
1900s, there have been no debates on the exact exit site
of the ACP from the maxillary sinus. After the introdu-
ction of endoscopic sinus surgery in the mid-1980s, a de-
tailed examination on the exit site was made possible.
15)
Kamel reported that the polyp passed through the main
ostium in 20 patients from 22 patients.
16)
However, 14
out of 22 64% of his patients were revision cases, and
confirming the exact location of the ostium was consi-
dered to be difficult due to postoperative changes. In a
study on pediatric cases, Wooley found that the exact
exit site was the accessory ostium of the maxillary sinus
in 3 from the 7 patients.
10)
Stammberger described that,
in over 80% of their cases, the polyp reached the nose
via the posterior fontanelle and not through the natural
ostium of the maxillary sinus.
5)
According to a number
of reports, in most or many cases, ACPs reached the na-
sal cavity through the accessory ostium of the maxillary
sinus.
17)18)
Regarding correlation with allergic diseases, most of
the reports denied the correlations,
4)9)18)
while Cook, et
al., reported that the association of allergic disease with
ACPs to be statistically significant.
7)
Seventy% 23 of
the 33 of their patients were diagnosed as having all-
ergic rhinitis.
DIAGNOSIS
The usual complaint was unilateral or bilateral nasal
obstruction. Rhinorrhea was another common presenta-
tion.
6)
Other symptoms include bleeding, snoring, halit-
osis and foreign body sensation. On examination, anterior
rhinoscopy revealed a unilateral intranasal polypoid ma-
ss of pale, fleshy quality.
6)
When accompanied by the hypertrophy of the inferior
turbinate was, ACPs may be easily missed. In the adult
patients, ACP was accompanied with other polyposis.
7)
The presence of polyps in the nasal cavity and nasoph-
arynx can be confirmed with endoscopes easily.
Simple radiographic findings of the ACP were dimi-
nished aeration of the involved maxillary antrum, and
the expansion of the antrum.
19)20)
But there were reports
saying that bony erosion was not observed.
6)10)
CT sh-
owed polyp from posterior fontanelle.
12)
In general, ACPs are unilateral lesion. With simple
roentgenogram, ipsilateral involvement of the inflam-
mation was noted in 57.6% of the patients and bilateral
involvement was noted in 42.6%.
4)
Observing through
a radiologic examination, bilateral sinus involvement was
shown in 31 50% of patients.
6)8)18)
Soft tissue mass in
the nasopharynx on lateral view was seen in 57% 8
out of 14 of patients.
6)
Choanal polyps usually originate from the maxillary
sinus, however they also originate from the sphenoid si-
nus, anterior ethmoid sinus or posterior ethmoid sinus.
21)
Polypoid mass should be differentiated with inverted pa-
pilloma.
21)
LOCATION
The ACPs originated most frequently from the post-
erior wall, followed by the inferior , lateral, and medial
Chung Antrochoanal Polyp / 7
wall.
9)
This finding is consistent with that reported by
Kubo.
1)
Lee, et al. Reported that the floor of the maxil-
lary sinus was the most frequent site of origin, followed
by lateral wall, medial wall and roof in his 74 patients.
8)
PATHOLOGY
Grossly, ACPs have a characteristic dumbbell shape.
4)
Earlier reports have indicated that the histology of the
ACP does not differ significantly from that of nasal po-
lyps. Tissue eosinophilia occurs less frequently in ACPs
than in the nasal polyps.
4)
Min, et al., reported that in
ACP, eosinophilic infiltration is less severe than in the
allergic polyp group.
9)
The presence of submucous gla-
nds was significantly less pronounced than in the ordi-
nary nasal polyp group.
4)9)
These findings indicate that
the ACP has little causal relationship with nasal allergy,
but is all the more intimately associated with inflamm-
atory processes.
9)
On the other hand, there was a contrasting report
saying in 90% of patients 27 out of 33 , abundant
eosinophils or plasma cells are noted in the nasal polyp
coexisting with ACPs.
7)
TREATMENT
For therapy, surgery is the modality of choice. The cy-
stic portion coming out of the maxillary sinus must tot-
ally be removed.
For the removal of the polyps, removal by snare, ev-
ulsion polypectomy, intranasal antrostomy, or Caldwell-
Luc operation were tried in 1950s.
1)
A good result may
be expected in 80% of person without chronic sinusitis
following removal of the polyps by snare and avulsion.
1)4)
The radical external sinus operation is probably the
procedure of choice when there is chronic suppurative
inflammatory disease of the lining membrane of the si-
nus from which the polyp arose. Recurrence followed in
approximately 5.5% of cases in which the external ap-
proach was used.
One recurrence was found in a patient treated with
the C-L approach, out of 12, during an 18 months fol-
low up period.
6)
Lee, et al., reported no recurrence of
ACP with Caldwell-Luc approach, however, a 33% re-
currence rate with endoscopic technique, and 66% with
simple avulsion.
8)
Functional endoscopic sinus surgery has been repor-
ted to be useful in the surgery of the ACPs.
12)16)
Endo-
scopic sinus surgery is useful particularly in obviating
the need for a standard Caldwell-Luc approach to the
antrum.
7)
During the operation, the ostia through which
the ACPs comes to the nasal cavity should be confirmed
carefully. If these opening are the accessory ostia, these
opening should be connected with natural opening of the
maxillary sinus. For the revision cases, ACP may come
through the surgically created middle meatal antrostomy
site or inferior meatal antrostomy site.
16)
Loury reported an 80% success rate with endoscopic
sinus surgery technique for 5 patients.
12)
No recurrence
of ACPs with ESS technique were reported in 22 pati-
ents during 20 months
16)
and in 33 patients during 24
months of follow up period.
7)
Choo, et al., reported that
he treated the ACPs in pediatric patients with endosco-
pic technique and no recurrence of polyps in 85% within
a one year period.
22)
Lee, et al., compared the endoscopic technique for 15
patients and 10 osteoplastic Caldwell-Luc approach.
23)
He did not observe any recurrence of ACP with endo-
scopic technique for 24 months. Same results were ob-
tained with Kim for his 21 cases of ACP.
11)
So now the
endoscopic removal is the method of choice.
23)
Corticosterioid is not effective, which possibly related
to the fact that few inflammatory cells, and no eosinop-
hils, are encountered in histological sections.
5)
REFERENCES
1) Hardy G. The choanal polyp. Ann Otol Rhinol Laryngol 1957;66:
306-26.
2) Killian G. The origin of choanal polypi. Lancet 1906;2:81-2.
3) Kelly AB. Naso-antral polypus. Lancet 1909;2:89-91.
4) Heck WE, Hallberg OE, Williams HL. Antrochoanal polyp. Arch
Oto 1950;52:538-48.
5) Stammberger H. Examination and endoscopy of the nose and pa-
ranasal sinuses. In: Mygind N, Lildholdt T, editors. Nasal polypo-
sis. An inflammatory disease and its treatment. 1st ed. Copenhagen:
Munksgaard;1997. P.120-36.
6) Chen JM, Schloss MD, Azouz ME. Antro-choanal polyp: A 10
year retrospective stufy in the pediatric population with a review
of the literature. J Otolaryngol 1989;18:168-72.
7) Cook PR, Davis WE, McDonald R, McKinsey JP. Antrochoanal po-
lyposis: A review of 33 cases. Ear Nose Throat J 1993;72:401-10 .
8) Lee BJ, Kim JH, Kim HC, Yang DS, Chu KC. Antrochoanal polyps:
Analysis of 74 surgical cases. Korean J Rhinol 1994;1:54-62.
9) Min YG, Chung JW, Chi JG. Histologic structure of antrochoanal
polyps. Acta Otolaryngol 1995;115:543-7.
10) Woolley AL, Clary RA, Lusk RP. Antrochoanal polyps in children.
Am J Otolaryngol 1996;17:368-373.
11) Kim YD, Bai CH, Kim JW, Chung YS, Suh JS, Song KW. Endos-
copic sinus surgery for antrochoanal polyp. Korean J Otollaryngol
1998;41:208-212.
12) Loury MC, Hinkley DK, Wong W. Endoscopic transnasal antroc-
8 / J Rhinol 7 1 , 2000
hoanal polypectomy: An alternative to the transantral approach.
South Med J 1993;86:18-22.
13) Myatt HM, Cabrera M. Bilateral antrochoanal polyps in a child: A
case report. J Layngol Otol 1996;110:272-4.
14) Berg O, Carenfelt C, Silfversward C, Sobin A. Origin of the choa-
nal polyp. Arch Otolaryngol Head Neck Surg 1988;114:1270-1.
15) Kennedy DW, Zinreich SJ, Rosenbaum A, Johns ME. Functional
endoscopic sinus surgery: Theory and diagnosis. Arch Otolaryngol
1985;111:576-582.
16) Kamel R. Endoscopic transnasal surgery in antrochoanal polyp.
Arch Otolaryngol Head Neck Surg 1990;116:841-3.
17) Basak S, Karaman CZ, Akdilli A, Metin KK. Surgical approaches
to antrochoanal polyps in children. Int J Pediatr Otorhinolaryngol
1998;46:197-205.
18) Aktas D, Yetiser S, Gerek M, Kurnaz A, Can C, Kahramanyo M.
Antrochoanal polyps: Analysis of 16 cases. Rhinology 1998;26:
81-5.
19) Crowe JE, Sumner TE, Ramquist NA, Koufman JA. Antrochoanal
polyps. South Med J 1982;75:674-6.
20) Towbin R, Dunbar JS, Bove K. Antrochoanal polyps. AJR Am J
Roentgenol 1979;132:27-31.
21) Lopatin A, Bykova V, Piskunov G. Choanal polyps: One entity, one
surgical approach? Rhinology 1997;35:79-83.
22) Choo MJ, Kim JW, Lee KH, Choi YS, Shin SO. Endoscopic sinus
surgery for treatment of antrochoanal polyp. Korean J Rhinol 1996;
3:54-7.
23) Lee CH, Lee SJ. Treatment of antrochoanal polyp: Conservative
surgery using nasal endoscope. Korean J Otolaryngol 1996;39:
1253-9.
Vous aimerez peut-être aussi
- Bilateral Antrochoanal Polyps in an Adult Case ReportDocument3 pagesBilateral Antrochoanal Polyps in an Adult Case ReportCut Nanda FitriPas encore d'évaluation
- 0392-100X 29 021 PDFDocument6 pages0392-100X 29 021 PDFCut Nanda FitriPas encore d'évaluation
- Antrochoanal Polyp in Pediatric Age Group PDFDocument5 pagesAntrochoanal Polyp in Pediatric Age Group PDFCut Nanda FitriPas encore d'évaluation
- Ena 1Document4 pagesEna 1haneefmdfPas encore d'évaluation
- Ac PolypDocument8 pagesAc PolypDr. T. BalasubramanianPas encore d'évaluation
- 12.bilateral Antrochoanal Polyp inDocument4 pages12.bilateral Antrochoanal Polyp inDR K C MALLIK0% (1)
- Eosinophilic Angiocentric Fibrosis of The Nasal Septum: Case ReportDocument15 pagesEosinophilic Angiocentric Fibrosis of The Nasal Septum: Case ReportPriskila Marlen YoltuwuPas encore d'évaluation
- Bilateral Nasolabial Cyst MarcoviceanuDocument4 pagesBilateral Nasolabial Cyst MarcoviceanubamsusiloPas encore d'évaluation
- Articles Fernand Montreuil1949 Cyst of The Nasal VestibuleDocument8 pagesArticles Fernand Montreuil1949 Cyst of The Nasal Vestibuledieynaba baPas encore d'évaluation
- A Huge Epiglottic Cyst Causing Airway Obstruction in An AdultDocument4 pagesA Huge Epiglottic Cyst Causing Airway Obstruction in An AdultWaleed KerPas encore d'évaluation
- Ceo 3 110 PDFDocument5 pagesCeo 3 110 PDFCut Nanda FitriPas encore d'évaluation
- Nasal Polyps OriginateDocument5 pagesNasal Polyps OriginateMr.ZeddPas encore d'évaluation
- Preauricular Sinus and Its ManagmentDocument12 pagesPreauricular Sinus and Its ManagmentDr. T. Balasubramanian100% (7)
- Polip 1Document5 pagesPolip 1Nurzanah C PrimadanisPas encore d'évaluation
- Bab 2Document3 pagesBab 2Ratna WindyaningrumPas encore d'évaluation
- Edinbmedj74325 0089Document5 pagesEdinbmedj74325 0089anandadigdoyo44Pas encore d'évaluation
- Antrocoanal THTDocument6 pagesAntrocoanal THTNIGHTCORE NATIONPas encore d'évaluation
- Ijgmp - Medicine - Clinic-Pathological Profile of Sinonasal MassesDocument12 pagesIjgmp - Medicine - Clinic-Pathological Profile of Sinonasal Massesiaset123Pas encore d'évaluation
- Chapter 17 - Antrochoanal Polyp: Patient SelectionDocument4 pagesChapter 17 - Antrochoanal Polyp: Patient Selectionedohermendy_32666011Pas encore d'évaluation
- Surgery For Nasal Dermoids PDFDocument8 pagesSurgery For Nasal Dermoids PDFRirin PurbaPas encore d'évaluation
- Rare Nasal Alar ChondromaDocument4 pagesRare Nasal Alar Chondromaanitaabreu123Pas encore d'évaluation
- The Pathophysiology of Antrochoanal PolypsDocument6 pagesThe Pathophysiology of Antrochoanal PolypsAzuhra AnnisaPas encore d'évaluation
- Abcese FistuleDocument8 pagesAbcese FistuleDenis StoicaPas encore d'évaluation
- 2022 Nasal Pyriform Aperture StenosisDocument2 pages2022 Nasal Pyriform Aperture StenosisNicolien van der PoelPas encore d'évaluation
- Veterinary Dermatology - 2022 - T Pfer - Brachycephaly in French Bulldogs and Pugs Is Associated With Narrow Ear CanalsDocument8 pagesVeterinary Dermatology - 2022 - T Pfer - Brachycephaly in French Bulldogs and Pugs Is Associated With Narrow Ear CanalsJose Vargas GarciaPas encore d'évaluation
- Choanal Atresia PDFDocument8 pagesChoanal Atresia PDFMonna Medani LysabellaPas encore d'évaluation
- Sino Nasal Polyposis SsDocument42 pagesSino Nasal Polyposis SsJeffrinPas encore d'évaluation
- UNAS 2022 Juni (Ke-62) Larfar 1-23, Al-Im 1-4Document51 pagesUNAS 2022 Juni (Ke-62) Larfar 1-23, Al-Im 1-4abubakar rizviPas encore d'évaluation
- 5+6. Nasal Polyp & DNS PDFDocument43 pages5+6. Nasal Polyp & DNS PDFJames StiltonPas encore d'évaluation
- A Prospective Study of Sinonasal and Nasopharyngeal Pathology in Chronic Otitis MediaDocument5 pagesA Prospective Study of Sinonasal and Nasopharyngeal Pathology in Chronic Otitis MediaAmalia OkvitariandariPas encore d'évaluation
- Bjorl: Congenital Laryngeal Saccular CystDocument1 pageBjorl: Congenital Laryngeal Saccular CystGuilherme AméricoPas encore d'évaluation
- Costa 2007Document7 pagesCosta 2007abeer alrofaeyPas encore d'évaluation
- Rare Nasal Hemangioma Causing Severe AnemiaDocument2 pagesRare Nasal Hemangioma Causing Severe AnemiaHerryAsu-songkoPas encore d'évaluation
- Nasopalatine Duct CystDocument4 pagesNasopalatine Duct CystVikneswaran Vîçký100% (1)
- Large Rhinolith Case Report with Granulation TissueDocument3 pagesLarge Rhinolith Case Report with Granulation TissueDea LeeteukPas encore d'évaluation
- Congenital Bilateral Choanal AtresiDocument5 pagesCongenital Bilateral Choanal AtresiMonna Medani LysabellaPas encore d'évaluation
- Juvenile Nasopharyngeal Angiofibroma (JNA)Document19 pagesJuvenile Nasopharyngeal Angiofibroma (JNA)YogiHadityaPas encore d'évaluation
- Nontraumatic Nasal Septal AbscessDocument2 pagesNontraumatic Nasal Septal AbscessrajaalfatihPas encore d'évaluation
- Case Report: Matin Ghazizade, Mahboobe Asadi and Pouyan DarbaniDocument4 pagesCase Report: Matin Ghazizade, Mahboobe Asadi and Pouyan DarbanirizkiaPas encore d'évaluation
- Choanal AtresiaDocument8 pagesChoanal AtresiaDantowaluyo NewPas encore d'évaluation
- 1 SMDocument4 pages1 SMLasauva YardhaPas encore d'évaluation
- JurnalDocument6 pagesJurnalYazid Eriansyah PradantaPas encore d'évaluation
- Giant Epidermoid Cyst of The Floor of Mouth: LT LTDocument3 pagesGiant Epidermoid Cyst of The Floor of Mouth: LT LTKharismaNisaPas encore d'évaluation
- Nasal polyposis, inflammation, and allergy connectionDocument6 pagesNasal polyposis, inflammation, and allergy connectionLena Wahyu SetianingsihPas encore d'évaluation
- Isolated nasopharyngeal aspergillosis caused by A flavusDocument3 pagesIsolated nasopharyngeal aspergillosis caused by A flavusHarshitPas encore d'évaluation
- Evaluation of Myiasis in Hospital Attending PopulaDocument4 pagesEvaluation of Myiasis in Hospital Attending PopulaVikrant VazePas encore d'évaluation
- New Documents ENDocument3 pagesNew Documents ENAjmal KunjumonPas encore d'évaluation
- Adult LaryngomlaciaDocument3 pagesAdult LaryngomlaciamitaPas encore d'évaluation
- Nasopalatine Duct Cyst-Manuscript Case Report Haji - MIODocument6 pagesNasopalatine Duct Cyst-Manuscript Case Report Haji - MIOdrg.montessoPas encore d'évaluation
- Dysphagia As A Unique Presentation PostersDocument1 pageDysphagia As A Unique Presentation Postershadzrie imanPas encore d'évaluation
- Nasolabial CystDocument7 pagesNasolabial CystathaPas encore d'évaluation
- Antro Choanal PolypDocument16 pagesAntro Choanal PolypSpencer100% (1)
- Nasal Polyp MedscapeDocument30 pagesNasal Polyp MedscapeMonissa ArrianiPas encore d'évaluation
- Rapid Diagnosis and Treatment of A Pleural Effusion in A 24-Year-Old ManDocument4 pagesRapid Diagnosis and Treatment of A Pleural Effusion in A 24-Year-Old ManJonathan EdbertPas encore d'évaluation
- CanaliculitisDocument12 pagesCanaliculitisSetiawan Arif WibowoPas encore d'évaluation
- Thorax00193 0009 PDFDocument10 pagesThorax00193 0009 PDFhotmart ventasPas encore d'évaluation
- APENDICITIS Maingots Abdominal Operations ING PDFDocument46 pagesAPENDICITIS Maingots Abdominal Operations ING PDFMichel RamirezPas encore d'évaluation
- E.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarDocument3 pagesE.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarJohn M. Hemsworth100% (1)
- Proceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964D'EverandProceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964Augusto CorradettiPas encore d'évaluation
- DAPUSDocument2 pagesDAPUSsyukrinaalviPas encore d'évaluation
- Treatment of Acute Low Back PainDocument17 pagesTreatment of Acute Low Back PainNurhafizahImfistaPas encore d'évaluation
- DafDocument1 pageDafNurhafizahImfistaPas encore d'évaluation
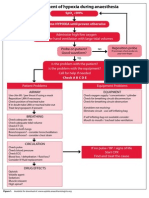
- Jurnal AnastesiDocument20 pagesJurnal AnastesiNurhafizahImfistaPas encore d'évaluation
- TreatmentDocument1 pageTreatmentNurhafizahImfistaPas encore d'évaluation
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Pyogenic GranulomaDocument6 pagesPyogenic GranulomaNurhafizahImfistaPas encore d'évaluation
- 4Document6 pages4NurhafizahImfistaPas encore d'évaluation
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Hospital in India. Journal of Gynecologic Surgery. Vol 22/no.4. 2006Document3 pagesHospital in India. Journal of Gynecologic Surgery. Vol 22/no.4. 2006NurhafizahImfistaPas encore d'évaluation
- Gagal GinjalDocument1 pageGagal GinjalNurhafizahImfistaPas encore d'évaluation
- Daftar PustakaDocument1 pageDaftar PustakaNurhafizahImfistaPas encore d'évaluation
- AntroChoanal Polyp SurgeryDocument14 pagesAntroChoanal Polyp SurgeryNurhafizahImfistaPas encore d'évaluation
- Vesicolithiasis With BPHDocument17 pagesVesicolithiasis With BPHNurhafizahImfistaPas encore d'évaluation
- HyperhidrosisDocument7 pagesHyperhidrosisNurhafizahImfistaPas encore d'évaluation
- A Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsDocument6 pagesA Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsNurhafizahImfistaPas encore d'évaluation
- OR1 Somchai TanawattanacharoenDocument6 pagesOR1 Somchai TanawattanacharoenNurhafizahImfistaPas encore d'évaluation
- Stres Dan KognitifDocument121 pagesStres Dan KognitifNurhafizahImfistaPas encore d'évaluation
- Education in Medicine Journal: Curricular Mapping: An Anti-Stress Tool For New Medical StudentsDocument7 pagesEducation in Medicine Journal: Curricular Mapping: An Anti-Stress Tool For New Medical StudentsNurhafizahImfistaPas encore d'évaluation
- Ciarrochi Deane PID Emotional Intelligence Moderates The Relationship Between Stress and Mental Health 2002Document13 pagesCiarrochi Deane PID Emotional Intelligence Moderates The Relationship Between Stress and Mental Health 2002NurhafizahImfistaPas encore d'évaluation
- A Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsDocument6 pagesA Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsNurhafizahImfistaPas encore d'évaluation
- Lower Gi Case Presentation PDFDocument35 pagesLower Gi Case Presentation PDFapi-448999672Pas encore d'évaluation
- Endometrial PolypDocument1 pageEndometrial PolypEdalyn CapiliPas encore d'évaluation
- (545729767) Colonoscopy-ConsentDocument1 page(545729767) Colonoscopy-ConsentMañanaMatutinaPas encore d'évaluation
- ICD-9-CM Morphology of Neoplasms GuideDocument17 pagesICD-9-CM Morphology of Neoplasms GuideMaju_kasusPas encore d'évaluation
- (2020) Pearls and Pitfalls of Interpretation in CT ColonographyDocument9 pages(2020) Pearls and Pitfalls of Interpretation in CT ColonographyChristian ToalongoPas encore d'évaluation
- Sample Multiple choice questions Single best answersDocument26 pagesSample Multiple choice questions Single best answersrutendonormamapurisa100% (2)
- Case Analysis COLON CANCERDocument4 pagesCase Analysis COLON CANCERBelle A. Basilio50% (2)
- Ohtas 15 1Document39 pagesOhtas 15 1indahPas encore d'évaluation
- ASCIA PCC Nasal Polyps 2015Document1 pageASCIA PCC Nasal Polyps 2015ASGHAR ALIPas encore d'évaluation
- Diagnosis: Surgical Pathology ReportDocument2 pagesDiagnosis: Surgical Pathology ReportMHCNSPas encore d'évaluation
- Lower Gastrointestinal BleedingDocument18 pagesLower Gastrointestinal Bleedingosama nawaysehPas encore d'évaluation
- Final Interpretation of Endoscopic Gastrointestinal BiopsyDocument107 pagesFinal Interpretation of Endoscopic Gastrointestinal BiopsyyourinmyheartPas encore d'évaluation
- Base Excision Repair and CancerDocument17 pagesBase Excision Repair and CancerIonela Petronela Tarabuta BocanceaPas encore d'évaluation
- Curs Colon RectDocument96 pagesCurs Colon RectIoanaPas encore d'évaluation
- Vulva, VaginaDocument15 pagesVulva, VaginaBilly Darisma100% (1)
- Jurnal Polip EndometriumDocument4 pagesJurnal Polip EndometriumNamira AmmarinPas encore d'évaluation
- Medical Transcription HISTORY & PHYSICAL EXAMINATION (Emergency Services)Document4 pagesMedical Transcription HISTORY & PHYSICAL EXAMINATION (Emergency Services)Caitlin EsguerraPas encore d'évaluation
- AM - ICD-10-AM GuideDocument26 pagesAM - ICD-10-AM GuidedrrskhanPas encore d'évaluation
- Just One Voice - High Res Ebook PDFDocument92 pagesJust One Voice - High Res Ebook PDFmwi66399Pas encore d'évaluation
- Ac PolypDocument18 pagesAc PolypSusmi CmPas encore d'évaluation
- BHRUT Endoscopy Induction Pack v1.5 (Final)Document17 pagesBHRUT Endoscopy Induction Pack v1.5 (Final)vlad910Pas encore d'évaluation
- ENT Question PaperDocument12 pagesENT Question Paperasokk40% (5)
- Nasal Polyps: Causes, Symptoms and TreatmentDocument32 pagesNasal Polyps: Causes, Symptoms and TreatmentAkhnal SyaputraPas encore d'évaluation
- Colon, Rectum and AnusDocument121 pagesColon, Rectum and AnusCheng Mochi-MochikoPas encore d'évaluation
- Familial Adenomatous Polyposis Clinical Presentation History, Physical ExaminationDocument1 pageFamilial Adenomatous Polyposis Clinical Presentation History, Physical ExaminationUrooj Ahmed AbbasiPas encore d'évaluation
- Colorectal Cancer: - Dr. Suneet KhuranaDocument36 pagesColorectal Cancer: - Dr. Suneet KhuranaCarlo ToledooPas encore d'évaluation
- Vitasum PDFDocument22 pagesVitasum PDFHen8Pas encore d'évaluation
- ENT Scholar Volume 1Document93 pagesENT Scholar Volume 1Dr. T. BalasubramanianPas encore d'évaluation
- Robbins Ch15!16!17Document26 pagesRobbins Ch15!16!17jeskevandiemenPas encore d'évaluation
- Malignant Colorectal PolypDocument44 pagesMalignant Colorectal PolypHarsha VardhanPas encore d'évaluation