Académique Documents
Professionnel Documents
Culture Documents
Morport 8 Juni 2014
Transféré par
Agustina Anggraeni PurnomoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Morport 8 Juni 2014
Transféré par
Agustina Anggraeni PurnomoDroits d'auteur :
Formats disponibles
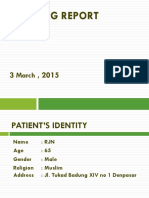
Mr.
MR, 24 YO
Cawang
CC : Vomit Sunday, June 8
th
2014, 2 PM
Findings Assesment Therapy Planning
Nausea
Loss of appetite
Patient came with vomiting since 1 week ago.The vomiting of food and
mucus.Patient said when he eat some food, he felt nausea. Two days ago, he
had fever. Patient already consumed lanzoprazole, donperidone, ondansentron,
and Pantoprazol, but the complain doesnt better.
Appearance : moderate illness, GCS E4V5M6, BP : 130/80 mmHg, PR :64 x/min,
RR : 20x/min, T : 36C
Eye : hyperemic conjunctiva -/-, icteric sclera -/-
THT : normal
Mouth : coated tongue +, tremor -
Neck : lymph nodes not enlarge, JVP : 5-2 cmH2O
Thorax
Ins : symmetric
Pal : vocal fremitus sound symmetric
Per : symmetric sonor sound
Aus : basic sound of breath vesicular, wheezing -/-, ronchi +/+. Heart sound I&II
regular, murmur -, gallop -
Abdominal
Ins : flat
Aus : bowel sound 8x/min
Pal : no tenderness, liver and spleen not palpable enlarged
Per : no percution pain
Extremities : warm acral, CRT < 2, edema +
- -
- -
Typhoid fever
Pro Hospitalized
Diet : Soft
IVFD : II RL
I Futrolit / 24hrs
Mm/
Levofloxacin 1x500 mg
Omeperazole 2x40 mg
Ondansentron 3x1c
- H2TL
LAB FINDING
Hemoglobin : 15,5 g/dl
Hematocrit : 38,5 %
Leukocyte : 3400 /ul
Platelet: 175.000 /ul
Widal test
S. Typhose H +1/320
S. Paratyphi A H -
S. Paratyphi B H +1/160
S. Paratyphi C H +1/160
S. Typhose O -
S. Paratyphi A O +1/160
S. Paratyphi B O +1/160
S. Paratyphi C O +1/160
Findings Assessment Therapy Planning
Appearance: moderate illness, GCS : E4V5M6, BP: 130/80 mmHg, PR :
80 x/min (adequate,regullar) RR : 22 x/min, T: 36,5 C
Eye : conjuntiva not pale, Sklera icteric -/-
Ear, Nose, Throat: normal
Neck : lymph nodes did not enlarged, venous distention -
THORAX
Insp : symmetric, ictus cordis (-)
Pal : vf symmetric, ictus cordis palpable
Per : symmetric, sonor sound
RHB ICS V lin. sternal dext, LHB ICS V lin.
Midclavicula sin
Aus : vesicular rh -/-,wh -/-
S1 single, S2 single, regular, murmur (-) gallop (-)
ABDOMINAL
Ins : stomach looks flat
Ausc : bowel sounds + 4x/m,
Palp : Pressure Pain - in epigastrium
Undulation(-)
Per : timpany, shifting dulness (-),
Extremitas : warm acral, CR<2, edema
LAB FINDING:
Complete Perifer Blood :
Hb : 12,3 gr/dl Leu : 9.500/ul ; Ht : 39,8%
Unstable Angina Pectoris
DD/ Dyspepsia
Pro Hospitelize
IVFD : I RL/ 24 hour
Diit : soft meal
Mm/
ISDN 3x2,5mg SL
OMZ 2x40mg IV
Clopidogrel 1x75mg PO
Domperidon 3x10mg PO AC 30
minutes
Sulcrafat 3x1C PO
Observation 48 hours with
serial EKG.
Tro : 231.000/ul ; random blood sugar: 104; Troponin T -; CPK 140;
CKMB 26; ureum 28; creatinin 0,85
Vous aimerez peut-être aussi
- Team 1 Morpot - 13 Juni 2014 (B)Document2 pagesTeam 1 Morpot - 13 Juni 2014 (B)Armando HalauwetPas encore d'évaluation
- Findings Assesment Therapy Planning: Abdominal PainDocument2 pagesFindings Assesment Therapy Planning: Abdominal PainAgustina Anggraeni PurnomoPas encore d'évaluation
- Mrs. Amelia Manurung, 42years Ugd Rs Uki Cawang CC: Abdominal Pain Monday, July 07 2014, 17:45:01PMDocument2 pagesMrs. Amelia Manurung, 42years Ugd Rs Uki Cawang CC: Abdominal Pain Monday, July 07 2014, 17:45:01PMFerjiRPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument12 pagesMorning Report: Department of Internal MedicineandrirombePas encore d'évaluation
- Morning Report: Departement of Surgery February 15rd 2017Document17 pagesMorning Report: Departement of Surgery February 15rd 2017Deasy Arindi PutriPas encore d'évaluation
- Tetralogy of FallotDocument30 pagesTetralogy of FallotRiYa SHreePas encore d'évaluation
- Physical Examination Generalised StatusDocument10 pagesPhysical Examination Generalised StatusregarskidPas encore d'évaluation
- Team 1 Morpot 24 Mei 2014Document13 pagesTeam 1 Morpot 24 Mei 2014FerjiRPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument19 pagesMorning Report: Department of Internal MedicinedwityanoviariPas encore d'évaluation
- Team 1 Morpot - 05 Juni 2014Document2 pagesTeam 1 Morpot - 05 Juni 2014Armando HalauwetPas encore d'évaluation
- Final CaseDocument45 pagesFinal Case_carido_Pas encore d'évaluation
- Mrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningDocument2 pagesMrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningAgustina Anggraeni PurnomoPas encore d'évaluation
- Morning Report Case: MarchDocument20 pagesMorning Report Case: Marchputri meiliawatiPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument11 pagesMorning Report: Department of Internal MedicineAyunita PermataPas encore d'évaluation
- Morning Report Tuesday Night Shift, FEBRUARY 12, 2019: Dr. / Dr. / Dr. / Dr. /dr. Dr. Dr. / DRDocument32 pagesMorning Report Tuesday Night Shift, FEBRUARY 12, 2019: Dr. / Dr. / Dr. / Dr. /dr. Dr. Dr. / DRHafizhan MuhammadPas encore d'évaluation
- Morport Kel 1 - A PrintDocument12 pagesMorport Kel 1 - A PrintAdhityaWPutraPas encore d'évaluation
- Jehan El Aher, Male, 27 YO, TI: Fever Since 4 Days AgoDocument10 pagesJehan El Aher, Male, 27 YO, TI: Fever Since 4 Days AgoFajri AanPas encore d'évaluation
- Morning Report Gastroenteritis CaseDocument12 pagesMorning Report Gastroenteritis CasezakyalfathuPas encore d'évaluation
- Boy, 14 Vomits and Abdominal Pain After AppendectomyDocument15 pagesBoy, 14 Vomits and Abdominal Pain After AppendectomyLodewyk Kefas JoshoaPas encore d'évaluation
- SLE Case Report on 15-Year-Old GirlDocument38 pagesSLE Case Report on 15-Year-Old GirlDiLa NandaRiPas encore d'évaluation
- Morport 12 Juni 2014Document12 pagesMorport 12 Juni 2014Agustina Anggraeni PurnomoPas encore d'évaluation
- Morning Report June 10, 2017 Dept of Internal Medicine G26Document21 pagesMorning Report June 10, 2017 Dept of Internal Medicine G26Deasy Arindi PutriPas encore d'évaluation
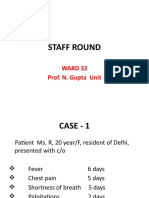
- Staff Round: Ward 32 Prof. N. Gupta UnitDocument22 pagesStaff Round: Ward 32 Prof. N. Gupta UnitSaroj SahooPas encore d'évaluation
- Morning Report: Dr. Satya Leads Hospital TeamsDocument42 pagesMorning Report: Dr. Satya Leads Hospital TeamsPramudia DeniPas encore d'évaluation
- ConsultsDocument16 pagesConsultsRaq KhoPas encore d'évaluation
- 91-Year-Old Patient Report with Gastrointestinal BleedingDocument17 pages91-Year-Old Patient Report with Gastrointestinal BleedingPuteri Diah RahtiniPas encore d'évaluation
- Findings Assessment Therapy PlanningDocument23 pagesFindings Assessment Therapy PlanningAdeliaPas encore d'évaluation
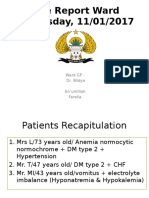
- Case Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaDocument39 pagesCase Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaFarella KartikaPas encore d'évaluation
- Case Report: Kwashiorkor: BY: JAYA DEV (110100465) Supervisor: Dr. Hj. Tiangsa Sembiring, M.Ked (Ped), Sp.A (K)Document49 pagesCase Report: Kwashiorkor: BY: JAYA DEV (110100465) Supervisor: Dr. Hj. Tiangsa Sembiring, M.Ked (Ped), Sp.A (K)Izaac JdevPas encore d'évaluation
- Ibu 9 JanDocument12 pagesIbu 9 JanYanti syahuri lubisPas encore d'évaluation
- Emergency Case Report December, 18 - , 19 2013: Resident On Duty: Dr. Alex Chief On Duty: Galih RahmanDocument66 pagesEmergency Case Report December, 18 - , 19 2013: Resident On Duty: Dr. Alex Chief On Duty: Galih Rahmangalihrahman51Pas encore d'évaluation
- Laporan Kasus AppendicitisDocument21 pagesLaporan Kasus AppendicitisjessicaPas encore d'évaluation
- Case Conference Saturday Night Shift, APRIL 6 TH, 2019Document46 pagesCase Conference Saturday Night Shift, APRIL 6 TH, 2019delfiaPas encore d'évaluation
- RSA SN Sabtu Pagi 6 JuliDocument12 pagesRSA SN Sabtu Pagi 6 JulimariaPas encore d'évaluation
- Morning Report: Case Resume Normal Labor - Pathology LaborDocument7 pagesMorning Report: Case Resume Normal Labor - Pathology LabormelatiigdPas encore d'évaluation
- MR GoutyDocument25 pagesMR GoutyArvindan SubramaniamPas encore d'évaluation
- Lapjag 10 Feb 2016 - AnemiaDocument25 pagesLapjag 10 Feb 2016 - AnemiamyoganoPas encore d'évaluation
- Morpot BilliDocument12 pagesMorpot BilliKadek Widhiana UtamiPas encore d'évaluation
- Nurul Hayati DR AgungDocument17 pagesNurul Hayati DR AgungAgung Pratama YudhaPas encore d'évaluation
- Duty Report, SuhayatiDocument9 pagesDuty Report, SuhayatiRudiErwinKurniawanPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument11 pagesMorning Report: Department of Internal MedicineSharly Ayu PuspitaPas encore d'évaluation
- Dengue Haemorrhagic Fever: Case ReportDocument37 pagesDengue Haemorrhagic Fever: Case ReportmhimiPas encore d'évaluation
- Morpot InternaDocument14 pagesMorpot InternaZega AgustianPas encore d'évaluation
- Case Report: Acute Post-Streptococcal GlomerulonephritisDocument57 pagesCase Report: Acute Post-Streptococcal Glomerulonephritistitis sariPas encore d'évaluation
- Tn. Ngadiran, r25Document21 pagesTn. Ngadiran, r25alanaaluPas encore d'évaluation
- Shock SepticDocument35 pagesShock SepticAkbar SyarialPas encore d'évaluation
- Morning Report: Date: 1 June 2019Document15 pagesMorning Report: Date: 1 June 2019Erwin HidayatPas encore d'évaluation
- MR Interna Intoksikasi MetanolDocument17 pagesMR Interna Intoksikasi Metanolvina_vermillionPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument13 pagesMorning Report: Department of Internal MedicineBungas ArisudanaPas encore d'évaluation
- Acute Abdominal Pain Case ConferenceDocument26 pagesAcute Abdominal Pain Case ConferenceEfan StiawanPas encore d'évaluation
- Case Report of a 7-Year-Old Girl with Diabetic Ketoacidosis and Acute Kidney InjuryDocument17 pagesCase Report of a 7-Year-Old Girl with Diabetic Ketoacidosis and Acute Kidney InjurySaravana Selvi SanmugamPas encore d'évaluation
- Morning Report: Monday, July 3, 2018Document25 pagesMorning Report: Monday, July 3, 2018Nur FarinahPas encore d'évaluation
- Morning Report Case: June 19, 2014Document23 pagesMorning Report Case: June 19, 2014Sri DashiniePas encore d'évaluation
- DUTY Report: 64yo Male with BreathlessnessDocument12 pagesDUTY Report: 64yo Male with BreathlessnessAnonymous C7LSjfPas encore d'évaluation
- Case ReportDocument34 pagesCase ReportMiftahul JannahPas encore d'évaluation
- EncephalitisDocument27 pagesEncephalitisHasRoni Fathurrahman100% (1)
- "Morning Report": Christian University of IndonesiaDocument12 pages"Morning Report": Christian University of IndonesialettasamudraPas encore d'évaluation
- Breathless 56yo man with CKD stage VDocument12 pagesBreathless 56yo man with CKD stage VherlizarefrianiPas encore d'évaluation
- Morning Report: Department of Internal MedicineDocument11 pagesMorning Report: Department of Internal MedicineAyunita PermataPas encore d'évaluation
- Anaesthesia and cognitive changes in elderly patientsDocument4 pagesAnaesthesia and cognitive changes in elderly patientsdocbinPas encore d'évaluation
- 4Document11 pages4Agustina Anggraeni PurnomoPas encore d'évaluation
- Anesthesia & Analgesia Volume 114 Issue 2 2012 (Doi 10.1213/ane.0b013e31823b2602) Zhang, Bin Tian, Ming Zhen, Yu Yue, Yun Sherman, Janet Zhen - The Effects of Isoflurane and Desflurane On CognDocument6 pagesAnesthesia & Analgesia Volume 114 Issue 2 2012 (Doi 10.1213/ane.0b013e31823b2602) Zhang, Bin Tian, Ming Zhen, Yu Yue, Yun Sherman, Janet Zhen - The Effects of Isoflurane and Desflurane On CognAgustina Anggraeni PurnomoPas encore d'évaluation
- 26854Document13 pages26854Agustina Anggraeni PurnomoPas encore d'évaluation
- 6Document5 pages6Agustina Anggraeni PurnomoPas encore d'évaluation
- JapanDocument9 pagesJapanAgustina Anggraeni PurnomoPas encore d'évaluation
- Postoperative Cognitive Deficit After Cardiopulmonary Bypass With Preserved Cerebral Oxygenation: A Prospective Observational Pilot StudyDocument6 pagesPostoperative Cognitive Deficit After Cardiopulmonary Bypass With Preserved Cerebral Oxygenation: A Prospective Observational Pilot StudyAgustina Anggraeni PurnomoPas encore d'évaluation
- 2011 Gauge AmulreeDocument20 pages2011 Gauge AmulreeAgustina Anggraeni PurnomoPas encore d'évaluation
- Tens Compared To Opioids in Postoperative Analgesic Therapy After Major Spinal Surgery With Regard To Cognitive FunctionDocument8 pagesTens Compared To Opioids in Postoperative Analgesic Therapy After Major Spinal Surgery With Regard To Cognitive FunctionAgustina Anggraeni PurnomoPas encore d'évaluation
- Incidental Finding of Uterine Adenomyosis in A Bitch With Reproductive Disorders: A Case ReportDocument5 pagesIncidental Finding of Uterine Adenomyosis in A Bitch With Reproductive Disorders: A Case ReportAgustina Anggraeni PurnomoPas encore d'évaluation
- Post-Operative Cognitive Functions After General Anesthesia With Sevoflurane and Desflurane in South Asian ElderlyDocument6 pagesPost-Operative Cognitive Functions After General Anesthesia With Sevoflurane and Desflurane in South Asian ElderlyAgustina Anggraeni PurnomoPas encore d'évaluation
- Siriraj Stroke ScoreDocument2 pagesSiriraj Stroke ScoreUlil Fuad100% (4)
- Journal ObstetriDocument4 pagesJournal ObstetriDhiyah HarahapPas encore d'évaluation
- Interpreting Category II Fetal Heart Rate Tracings: Does Meconium Matter?Document8 pagesInterpreting Category II Fetal Heart Rate Tracings: Does Meconium Matter?Agustina Anggraeni PurnomoPas encore d'évaluation
- Osteoporosis PowerpointDocument45 pagesOsteoporosis PowerpointAgustina Anggraeni Purnomo100% (1)
- Management of Stroke in Older PeopleDocument11 pagesManagement of Stroke in Older PeopleAgustina Anggraeni PurnomoPas encore d'évaluation
- Mrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningDocument2 pagesMrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningAgustina Anggraeni PurnomoPas encore d'évaluation
- Morport 12 Juni 2014Document12 pagesMorport 12 Juni 2014Agustina Anggraeni PurnomoPas encore d'évaluation
- Valori Contract An. 2023 - Paraclinic - 20.09.2023Document21 pagesValori Contract An. 2023 - Paraclinic - 20.09.2023Matteo si Sofia vlog'sPas encore d'évaluation
- Sirwan Ali Enterohemorrhagic-Escherichia-coliDocument8 pagesSirwan Ali Enterohemorrhagic-Escherichia-coliDlzar AbubakrPas encore d'évaluation
- Z50 Transducer Ficha Tecnica SheetDocument3 pagesZ50 Transducer Ficha Tecnica SheetMarcos CharmeloPas encore d'évaluation
- Ismmidterm2018 MinDocument17 pagesIsmmidterm2018 Minapi-382001974Pas encore d'évaluation
- RICKETS and OSTEOGENESIS IMPERFRCTADocument11 pagesRICKETS and OSTEOGENESIS IMPERFRCTAFaith de la RosaPas encore d'évaluation
- Understanding Toxic Goiter and Its Nursing CareDocument22 pagesUnderstanding Toxic Goiter and Its Nursing CareJohn Matley Caampued100% (2)
- HSYLCSyllabus Beijing 2016Document5 pagesHSYLCSyllabus Beijing 2016Akshay SwaminathanPas encore d'évaluation
- Activity # 3 - Research JournalDocument3 pagesActivity # 3 - Research Journalcayla mae carlosPas encore d'évaluation
- 199-Article Text-1111-1-10-20230613Document7 pages199-Article Text-1111-1-10-20230613Yayu AngrianPas encore d'évaluation
- Clinical and Social Factors Associated With Violent Behavior in Persons With Schizophrenia Spectrum DisordersDocument6 pagesClinical and Social Factors Associated With Violent Behavior in Persons With Schizophrenia Spectrum DisordersIJAR JOURNALPas encore d'évaluation
- BEmONC - Training ManualDocument263 pagesBEmONC - Training ManualdiribaPas encore d'évaluation
- Clinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066Document1 pageClinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066kolintang1Pas encore d'évaluation
- DR Walsh Autism Ocd Pandas Depression MethylationDocument6 pagesDR Walsh Autism Ocd Pandas Depression MethylationAnupama PoulosePas encore d'évaluation
- Patient A (Click On The Link To "Complete Patient A's Karyotype")Document2 pagesPatient A (Click On The Link To "Complete Patient A's Karyotype")ZzaiRraPas encore d'évaluation
- Roselet Medical Lab Blood and Urine Test ResultsDocument6 pagesRoselet Medical Lab Blood and Urine Test ResultsDaniel DasPas encore d'évaluation
- Cga - 1Document19 pagesCga - 1Kenji Tolero100% (1)
- Critical Care Nurse Skills ChecklistDocument4 pagesCritical Care Nurse Skills Checklistspartacuslives100% (1)
- Endovac BrochureDocument8 pagesEndovac BrochureGeorge MK100% (1)
- Post TestDocument11 pagesPost Testoomculun100% (6)
- Endoscopic DacryocystorhinostomyDocument17 pagesEndoscopic Dacryocystorhinostomyapi-19500641Pas encore d'évaluation
- Hematology 2006 Young 72 7Document6 pagesHematology 2006 Young 72 7Indira DeviPas encore d'évaluation
- Factors Affecting Inter Individual Variations in Drug ResponseDocument10 pagesFactors Affecting Inter Individual Variations in Drug Responsehumera50% (4)
- Sciences Basic To PsychiatryDocument2 pagesSciences Basic To Psychiatrynisha chauhanPas encore d'évaluation
- Extrahepatic Biliary AtresiaDocument3 pagesExtrahepatic Biliary AtresiaTiti Afrianto100% (1)
- Summary Exercise 2Document2 pagesSummary Exercise 2SeanPas encore d'évaluation
- Trazissin® VASOPRESSIN INJECTION USP 20IU Per 1ml Solution For Injection Package Leaflet - Taj PharmaDocument1 pageTrazissin® VASOPRESSIN INJECTION USP 20IU Per 1ml Solution For Injection Package Leaflet - Taj PharmaTAJ PHARMA — A Health Care ProviderPas encore d'évaluation
- SBAR Communication GuidelinesDocument2 pagesSBAR Communication GuidelinesmonabertPas encore d'évaluation
- Case Study StrokeDocument5 pagesCase Study StrokelilutzuPas encore d'évaluation
- Understanding Borderline Personality DisorderDocument4 pagesUnderstanding Borderline Personality DisorderAbdul Hakim Abdul Kadir100% (1)
- Hydrocephalus AND Neural Tube DefectDocument7 pagesHydrocephalus AND Neural Tube DefectTherese ArellanoPas encore d'évaluation