Académique Documents
Professionnel Documents
Culture Documents
Glaucoma
Transféré par
kristel_nicole18yahoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Glaucoma
Transféré par
kristel_nicole18yahoDroits d'auteur :
Formats disponibles
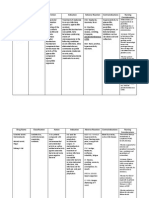
Modifiable Factors
Frequent use of
steroids
Previous Eye Injury
MYOPIA
Non-Modifiable Factors
Age
Genetics
Race
Lens hardens and inc in size,
with old age, trabecular
meshwork cells works less
efficiently
Resulting to build up
aqueous humour within
the anterior chamber of
the eye
Blocks aqueous flow
Predisposes to raise
intraocular pressure
Cells and ganglions
nerves of the retina
dries off
Retinal Ganglion
Ischemia due to
compression of
blood vessels of
retina
Deprivation of
nutrients to the eye
Diagnostic Exams:
1. Comprehensive
gaucoma exam
2. Tonometry
3. Gonioscopy
4. Opthalmoscopy
Results to clinically
progressive loss of
peripheral visual fields
GLAUCOMA
Glaucoma is a disease that damages the eyes optic nerve. The optic nerve is connected to the retina
a layer of light-sensitive tissue lining the back of the eye and is made up of many nerve fibers, like an
electric cable is made up of many wires. It is the optic nerve that sends signals from your retina to your
brain, where these signals are interpreted as the images you see.
CLASSIFICATIONS
1. Open-angle glaucoma
The most common form of glaucoma is called primary open-angle glaucoma. It occurs when the
trabecular meshwork of the eye gradually becomes less efficient at draining fluid. As this happens, your
eye pressure, called intraocular pressure (IOP), rises. Raised eye pressure leads to damage of the optic
nerve
Symptoms:
1. Tunnel Vision
2. Gradual Peripheral Vision loss
3. Gradual vision loss
2. Close-Angle Glaucoma
A less common form of glaucoma is closed angle (or narrow-angle glaucoma or angle-closure
glaucoma). Closed-angle glaucoma occurs when the drainage angle of the eye becomes blocked. The
pressure rises because the iris the colored part of the eye partially or completely blocks off the
drainage angle
Symptoms:
1. Severe eye or brow pain
2. Redness of the eye
3. Decreased or blurred vision
4. Seeing colored rainbows or halos
5. Headache
6. Nausea
7. Vomiting
GLAUCOMA
Normal-Tension Glaucoma
Their eye pressure is consistently below 21 mm Hg, but optic nerve damage and visual field
loss still occur. People with normal-tension glaucoma typically receive the same methods of
treatment used for open-angle glaucoma.
Chronic open-angle glaucoma
No early symptoms
Insidious visual impairment, blurring
Diminished accommodation
Gradual loss of peripheral vision (tunnel vision)
Mildly aching eyes
Halos around lights later with elevated IOP
Acute closed-angle glaucoma
Transitory attacks of diminished visual acuity
Colored halos around lights
Reddened eye with excruciating pain
Headache
Nausea and vomiting
Laboratory and diagnostic study findings
Tonometry detects elevated IOP (>10 to 20 mmHg)
Slit-lamp examination reveals abnormalities in the anterior vitreous humor.
What Causes Glaucoma:
Eye injury;
Inflammation of the eye;
Abnormal blood vessel formation from diabetes or retinal blood vessel blockage;
Use of steroid-containing medications (pills, eyedrops, sprays); or
Pigment dispersion, where tiny fragments or granules from the iris (the colored part of the eye)
can circulate in the aqueous humor (the fluid within the front portion of the eye) and block the
trabecular meshwork, the tiny drain for the eyes aqueous humor.
Risk Factors of Glaucoma
Age
Family history of glaucoma
African or Hispanic ancestry
Farsightedness or nearsightedness
Elevated eye pressure
Past eye injury
Having a thinner central cornea (the clear, front part of the eye covering the pupil and colored
iris)
Not having eye examinations when they are recommended
Conditions that affect blood flow, such as migraines, diabetes and low blood pressure
Medical Treatment
B Beta Blockers (Timolol)
It is thought that beta-blockers reduce intraocular pressure by slowing down the production of aqueous
humour in your eye. They are used once or twice a day and can cause side effects such as:
a stinging or burning sensation in your eye
dry eyes
itchy eyes
A Anhydrase Inhibitors
Carbonic anhydrase inhibitors reduce the amount of aqueous humour produced in your eye, which
reduces intraocular pressure. These drops are used two or three times a day and may cause:
a bitter taste in your mouth
nausea (feeling sick)
a dry mouth
eye irritation
Some types of carbonic anhydrase inhibitors you may be prescribed include:
brinzolamide
dorzolamide
H HyperOsmotics
Reduces the rate of formation of fluid
Some type of hyperosmotic drug:
Mannitol
M Miotics
Miotics facilitate the outflow of aqueous humour
Example: Pilocarpine
Sugical Treatment
1. Laser trabeculoplasty
A surgery called laser trabeculoplasty is often used to treat open-angle glaucoma. There are two types
of trabeculoplasty surgery: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty
(SLT).
During ALT surgery, a laser makes tiny, evenly spaced burns in the trabecular meshwork. The laser
does not create new drainage holes, but rather stimulates the drain to function more efficiently.
2. Laser iridotomy
Laser iridotomy is recommended for treating people with closed-angle glaucoma and those with very
narrow drainage angles. A laser creates a small hole about the size of a pinhead through the top part
of the iris to improve the flow of aqueous fluid to the drainage angle.
3. Peripheral iridectomy
When laser iridotomy is unable to stop an acute closed-angle glaucoma attack, or is not possible for
other reasons, a peripheral iridectomy may be performed
4. Trabeculectomy
In trabeculectomy, a small flap is made in the sclera (the outer white coating of your eye). A filtration
bleb, or reservoir, is created under the conjunctiva the thin, filmy membrane that covers the white
part of your eye.
5. Aqueous shunt surgery
If trabeculectomy cannot be performed, aqueous shunt surgery is usually successful in lowering eye
pressure.
An aqueous shunt is a small plastic tube or valve connected on one end to a reservoir (a roundish or
oval plate). The shunt is an artificial drainage device and is implanted in the eye through a tiny
incision.
Nursing Management for Glaucoma
Provide information regarding management of glaucoma
Discuss preoperative and postoperative teaching for immediate surgical opening of the eye chamber.
Prepare to administer carbonic anhydrase inhibitors IV or IM, to restrict production of aqueous humor.
Prepare to administer osmotic agents.
Discuss and prepare the client for surgical or laser peripheral iridectomy after the acute episode is
relieved.
Provide information about laser trabeculoplasty, if medication therapy proves ineffective.
Teach the client about specific safety precautions.
Instruct the client to avoid mydriatics such as atropine, which may precipitate acute glaucoma in a
client with closed-angle glaucoma.
Instruct the client to carry prescribed medications at all times.
Instruct the client to carry a medical identification card or wear a bracelet stating his type of glaucoma
and need for medication.
Instruct the client to take extra precautions at night (e.g. use of handrails, provide extra lighting to
compensate for impaired pupil dilation from miotic use)
Vous aimerez peut-être aussi
- Monday, Tuesday, Thursday & Friday: St. Pio of Pietrelcina ChapelDocument2 pagesMonday, Tuesday, Thursday & Friday: St. Pio of Pietrelcina Chapelkristel_nicole18yahoPas encore d'évaluation
- Emergency & DisasterDocument1 pageEmergency & Disasterkristel_nicole18yahoPas encore d'évaluation
- Drug OrderDocument5 pagesDrug Orderkristel_nicole18yahoPas encore d'évaluation
- Diagram I Pathogenesis of Insulin Dependent DM (Type 1) : DiagramsDocument2 pagesDiagram I Pathogenesis of Insulin Dependent DM (Type 1) : Diagramskristel_nicole18yahoPas encore d'évaluation
- Drug StudyDocument8 pagesDrug Studykristel_nicole18yahoPas encore d'évaluation
- Vector Part 2 and 3Document18 pagesVector Part 2 and 3kristel_nicole18yahoPas encore d'évaluation
- Drug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaiseDocument3 pagesDrug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaisekristel_nicole18yahoPas encore d'évaluation
- NCPDXDocument3 pagesNCPDXkristel_nicole18yahoPas encore d'évaluation
- Addisons DiseaseDocument1 pageAddisons Diseasekristel_nicole18yahoPas encore d'évaluation
- Drug AnalysisDocument4 pagesDrug Analysiskristel_nicole18yahoPas encore d'évaluation
- 3NCPDocument4 pages3NCPkristel_nicole18yahoPas encore d'évaluation
- Drug AnalysisDocument4 pagesDrug Analysiskristel_nicole18yahoPas encore d'évaluation
- Nursing care plan for post-surgical gastric cancer patientDocument2 pagesNursing care plan for post-surgical gastric cancer patientkristel_nicole18yahoPas encore d'évaluation
- Chemistry Date: 04/29/14: Developed or Changed The Ranges From Her Chemistry LabDocument1 pageChemistry Date: 04/29/14: Developed or Changed The Ranges From Her Chemistry Labkristel_nicole18yahoPas encore d'évaluation
- Social History - Generativity vs StagnationDocument1 pageSocial History - Generativity vs Stagnationkristel_nicole18yahoPas encore d'évaluation
- 3rd NCP Risk For ConstipationDocument2 pages3rd NCP Risk For Constipationkristel_nicole18yaho100% (3)
- Gastric Adenocarcinoma Nursing CareDocument5 pagesGastric Adenocarcinoma Nursing Carekristel_nicole18yahoPas encore d'évaluation
- Addisons DiseaseDocument1 pageAddisons Diseasekristel_nicole18yahoPas encore d'évaluation
- Case Pres NCP HyperthermiaDocument2 pagesCase Pres NCP Hyperthermiakristel_nicole18yahoPas encore d'évaluation
- Drug OrderDocument5 pagesDrug Orderkristel_nicole18yahoPas encore d'évaluation
- Nursing care plan for post-surgical gastric cancer patientDocument2 pagesNursing care plan for post-surgical gastric cancer patientkristel_nicole18yahoPas encore d'évaluation
- Gastric Adenocarcinoma Nursing CareDocument5 pagesGastric Adenocarcinoma Nursing Carekristel_nicole18yahoPas encore d'évaluation
- Clinical Teaching Behavior Student'S Learning Response: Conceptual FrameworkDocument5 pagesClinical Teaching Behavior Student'S Learning Response: Conceptual Frameworkkristel_nicole18yahoPas encore d'évaluation
- DemoDocument6 pagesDemokristel_nicole18yahoPas encore d'évaluation
- Hinds & Gattuso, 1999Document1 pageHinds & Gattuso, 1999kristel_nicole18yahoPas encore d'évaluation
- Case Study PathoDocument4 pagesCase Study Pathokristel_nicole18yahoPas encore d'évaluation
- Hinds & Gattuso, 1999Document1 pageHinds & Gattuso, 1999kristel_nicole18yahoPas encore d'évaluation
- 10 17 1 PB PDFDocument14 pages10 17 1 PB PDFnylorjayPas encore d'évaluation
- Predisposing Factors Precipitating FactorsDocument1 pagePredisposing Factors Precipitating Factorskristel_nicole18yahoPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Gabriel Axel - Master Thesis - Vision The Art of Evolution (2010)Document41 pagesGabriel Axel - Master Thesis - Vision The Art of Evolution (2010)gabrielaxelPas encore d'évaluation
- The List by INDITEX. IV Edition - PDF SetasDocument37 pagesThe List by INDITEX. IV Edition - PDF SetasZOUARIPas encore d'évaluation
- IOL Calculation in Complex Corneal ConditionsDocument8 pagesIOL Calculation in Complex Corneal ConditionsShimaa MersalPas encore d'évaluation
- MANUAL VISIOMETRO VS-V - Universal - Manual - 2015Document23 pagesMANUAL VISIOMETRO VS-V - Universal - Manual - 2015ginalimartinezmuPas encore d'évaluation
- EyetgDocument19 pagesEyetgLissy JyothishPas encore d'évaluation
- Retina: Zarieh Dawn L. Novela Medicine 2Document50 pagesRetina: Zarieh Dawn L. Novela Medicine 2Zari NovelaPas encore d'évaluation
- Glaucoma: Direct Mechanical Theory - Suggests That HighDocument4 pagesGlaucoma: Direct Mechanical Theory - Suggests That HighMarissa AsimPas encore d'évaluation
- Human Eye: General PropertiesDocument10 pagesHuman Eye: General PropertiesVijay RajendiranPas encore d'évaluation
- DFV Diagnostic Product Guide ResourceDocument19 pagesDFV Diagnostic Product Guide ResourceSer NdcPas encore d'évaluation
- Brain Bee 2013 Study Guide FULLDocument12 pagesBrain Bee 2013 Study Guide FULLmsawickaPas encore d'évaluation
- Glaucoma: Pgmi Abadilla Angela MarieDocument29 pagesGlaucoma: Pgmi Abadilla Angela MarieAngel AbadillaPas encore d'évaluation
- Physiology Chapter 1 & 2 ReviewDocument193 pagesPhysiology Chapter 1 & 2 ReviewRichardPas encore d'évaluation
- Human Color Perception: Robert BoyntonDocument2 pagesHuman Color Perception: Robert BoyntonpauloPas encore d'évaluation
- UNIVERSITY OF MEDICAL SCIENCES"REZONANCA"-Halil Ajvazi/Ophthalmology/Prishtina/Republic of KosovaDocument98 pagesUNIVERSITY OF MEDICAL SCIENCES"REZONANCA"-Halil Ajvazi/Ophthalmology/Prishtina/Republic of KosovaHALIL Z.AJVAZI100% (1)
- Eyestar 900 BrochureDocument16 pagesEyestar 900 BrochureHaag-Streit UK (HS-UK)Pas encore d'évaluation
- 4 Lobes FunctionDocument4 pages4 Lobes FunctionAcharya PradeepPas encore d'évaluation
- Physiology Eye: of TheDocument164 pagesPhysiology Eye: of TheZZ Millania TitahPas encore d'évaluation
- Glaucoma Management and Target IOPDocument24 pagesGlaucoma Management and Target IOPElfi RisalmaPas encore d'évaluation
- Eye diseases: symptoms and conditionsDocument2 pagesEye diseases: symptoms and conditionsRaju ShresthaPas encore d'évaluation
- 13.2 Sense Organ - EyeDocument28 pages13.2 Sense Organ - EyeMuhammad Amin SuhaimiPas encore d'évaluation
- DPL 13 Feb 2023 - All IndiaDocument18 pagesDPL 13 Feb 2023 - All IndiaInfo UcsplPas encore d'évaluation
- Eyes - Ears - Mouth - Nose (Lecture 5)Document50 pagesEyes - Ears - Mouth - Nose (Lecture 5)اسامة محمد السيد رمضانPas encore d'évaluation
- Binocular Vision ScheimanDocument732 pagesBinocular Vision ScheimanOptom Dang100% (1)
- Manual de Técnicas Qx. en Oftalmología 14-10-22Document115 pagesManual de Técnicas Qx. en Oftalmología 14-10-22YAZMIN DEL JESUS LARA HUCHINPas encore d'évaluation
- Color and LightDocument1 pageColor and LightĐức ToànPas encore d'évaluation
- Vocab Quiz-Chap 4-Sens & PercDocument3 pagesVocab Quiz-Chap 4-Sens & PercJanie VandeBergPas encore d'évaluation
- Disturbance in Sensory PerceptionDocument48 pagesDisturbance in Sensory PerceptionKristine Louise JavierPas encore d'évaluation
- Common Retinal Diseases: FloatersDocument7 pagesCommon Retinal Diseases: FloatersDan-Dan Irika CentinoPas encore d'évaluation
- Optic Disc Abnormalities - Cheat SheetDocument6 pagesOptic Disc Abnormalities - Cheat SheetPaula EmyPas encore d'évaluation
- Contact Lenses 1: by Hatem S.H. Barhoom MHSC (Clinical Optometry) UKM - MalaysiaDocument250 pagesContact Lenses 1: by Hatem S.H. Barhoom MHSC (Clinical Optometry) UKM - MalaysiaHasan AnsariPas encore d'évaluation