Académique Documents
Professionnel Documents
Culture Documents
Short-Course Prophylactic Zinc Supplementation For Diarrhea Morbidity in Infant 6-11 Month Children
Transféré par
listiarsasihDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Short-Course Prophylactic Zinc Supplementation For Diarrhea Morbidity in Infant 6-11 Month Children
Transféré par
listiarsasihDroits d'auteur :
Formats disponibles
DOI: 10.1542/peds.
2012-2980
; originally published online June 3, 2013; 2013;132;e46 Pediatrics
Akash Malik, Davendra K. Taneja, Niveditha Devasenapathy and K. Rajeshwari
Infants of 6 to 11 Months
Short-Course Prophylactic Zinc Supplementation for Diarrhea Morbidity in
http://pediatrics.aappublications.org/content/132/1/e46.full.html
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Boulevard, Elk Grove Village, Illinois, 60007. Copyright 2013 by the American Academy
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
publication, it has been published continuously since 1948. PEDIATRICS is owned,
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
Short-Course Prophylactic Zinc Supplementation for
Diarrhea Morbidity in Infants of 6 to 11 Months
WHATS KNOWN ON THIS SUBJECT: Randomized controlled trials
have shown that zinc supplementation during diarrhea
substantially reduces the incidence and severity. However, the
effect of short-course prophylactic zinc supplementation has been
observed only in children .12 months of age.
WHAT THIS STUDY ADDS: The current study was able to show that
short-course prophylactic zinc supplementation signicantly
reduced diarrhea morbidity in apparently healthy infants of 6 to
11 months even after 5 months of follow-up.
abstract
BACKGROUND: Zinc supplementation during diarrhea substantially
reduces the incidence and severity of diarrhea. However, the effect
of short-course zinc prophylaxis has been observed only in children
.12 months of age. Because the incidence of diarrhea is comparatively
high in children aged 6 to 11 months, we assessed the prophylactic
effect of zinc on incidence and duration of diarrhea in this age group.
METHODS: In this randomized, double-blind, placebo-controlled trial, we
enrolled infants aged 6 to 11 months froman urban resettlement colony in
Delhi, India, between January 1, 2011, and January 15, 2012. We randomly
assigned 272 infants to receive either 20 mg of zinc or a placebo
suspension orally every day for 2 weeks. The primary outcome was
the incidence of diarrhea per child-year. All analyses were done by
intention-to-treat.
RESULTS: A total of 134 infants in the zinc and 124 in the placebo groups
were assessed for the incidence of diarrhea. There was a 39% reduction
(crude incident rate ratio [IRR] 0.61, 95% condence interval [CI] 0.53
0.71) in episodes of diarrhea, 39% (adjusted IRR 0.61, 95% CI 0.540.69)
in the total number of days that a child suffered from diarrhea, and
reduction of 36% in duration per episode of diarrhea (IRR 0.64, 95% CI
0.560.74) during the 5 months of follow-up.
CONCLUSIONS: Short-course prophylactic zinc supplementation for
2 weeks may reduce diarrhea morbidity in infants of 6 to 11 months
for up to 5 months, in populations with high prevalence of wasting
and stunting. Pediatrics 2013;132:e46e52
AUTHORS: Akash Malik, MBBS,
a
Davendra K. Taneja, MD,
a
Niveditha Devasenapathy, MBBS, MSc,
b
and K. Rajeshwari,
MD
c
Departments of
a
Community Medicine, and
c
Paediatrics, Maulana
Azad Medical College, New Delhi, India; and
b
Indian Institute of
Public Health-Delhi, Public Health Foundation of India, New Delhi,
India
KEY WORDS
zinc, diarrhea, infants, randomized control trial
ABBREVIATIONS
CIcondence interval
IRRincident rate ratio
RRrate ratio
Dr Malik formulated the research question and contributed to
designing the study, wrote the research grants, carried out the
eld investigations, carried out the initial data analyses, and
drafted the initial manuscript; Dr Taneja contributed to
designing the study, contributed to developing the standard
operating procedures, implemented randomization and blinding,
and reviewed and revised the manuscript; Dr Devasenapathy
supervised the data collection and managed the data, analyzed
the data, and interpreted the ndings; Dr Rajeshwari supervised
the clinical data collection and management, and contributed to
developing the standard operating procedures; and all authors
approved the nal manuscript as submitted.
This trial was registered with the Clinical Trial Registry-India, No.
CTRI/2010/091/001417.
The Indian Council of Medical Research, Department of Health
Research (Ministry of Health and Family Welfare), Government of
India, which funded the study, had no role in the study design,
data collection, analysis, interpretation of results, or decision to
publish this research. AK, DKT, ND and KR had full access to all
the data in the study and had nal responsibility for the decision
to submit for publication.
www.pediatrics.org/cgi/doi/10.1542/peds.2012-2980
doi:10.1542/peds.2012-2980
Accepted for publication Mar 25, 2013
Address correspondence to Akash Malik, MBBS, Department of
Community Medicine, Maulana Azad Medical College and
Associated Hospitals, Bahadur Shah Zafar Marg, New Delhi, India.
E-mail: drakashmalik28@gmail.com
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright 2013 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have
no nancial relationships relevant to this article to disclose.
FUNDING: Supported by the Indian Council of Medical Research,
Department of Health Research (Ministry of Health and Family
Welfare), Government of India. Reference No. 3/2/2011/PG-thesis-
MPD-10.
e46 MALIK et al
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
Zinc is required for multiple cellular
tasks and the immune system depends
on the sufcient availability of this es-
sential trace element.
1
Zinc deciency
is common in several developing coun-
tries, including India. This is because the
commonly consumed staple foods have
lowzinc contents andare richinphytates,
which inhibit the absorption and utiliza-
tion of zinc.
2
Randomized controlled trials
have shown that zinc supplementation
during acute diarrhea reduces the du-
ration and severity, as well as the
incidence of subsequent diarrheal epi-
sodes.
37
However, recently published
meta-analyses conclude that pro-
phylactic zinc supplementation signi-
cantly reduces the incidence of diarrhea
only in children .12 months of age.
810
Because the incidence of diarrhea is
comparatively high in children 6 to 12
months of age (4.8 episode per year),
11
coinciding with the starting of comple-
mentary feeding, the current study
aimed to evaluate whether zinc pro-
phylaxis for a short duration has any
role in reducing the morbidity due to
diarrhea in this age group. Although the
original trial included additional out-
comes, such as acute respiratory tract
infections and growth, the results of
these will be reported separately.
METHODS
Study Setting and Participants
This is a community-based, randomized,
double-blind, parallel-arm placebo-
controlled trial, conducted from Jan-
uary 1, 2011, to January 15, 2012. We
included all children 6 to 11 months of
age residing in Gokulpuri, an urban
resettlement colony in the northeast dis-
trict of Delhi, India, who were likely to stay
until thecompletionof thestudy. Gokulpuri
has 2500 houses dividedinto 4 blocks, A,
B, C, and D, with a predominantly migrant
population of 23 000. Most of the pop-
ulation belongs to the middle and lower
socioeconomic strata. To achieve the -
nal sample size, additional children were
recruited from the similar adjacent area
of Gangavihar. The study was approvedby
the Institutional Ethical Committee of
Maulana Azad Medical College, NewDelhi,
and Associated Lok Nayak Hospitals. The
trial is registered with the Clinical Trial
Registry-India, number CTRI/2010/091/
001417.
We hypothesized that zinc prophylaxis
for 2 weeks would reduce the incidence
of diarrhea in subsequent months.
Thus, we excluded any child receiving
zinc supplement at the time of study or
who had received it in the preceding
3 months, those who were severely
malnourished, immune-decient, cur-
rently on steroid therapy, severely ill
requiring hospitalization, or of families
likely to migrate from the study area. A
house-to-house survey was done at the
beginning of the study to identify and
recruit the eligible infants. The study
purposewasexplainedtothefamilyand
aninformedconsent wasobtainedfrom
parents of all infants before they were
included in the trial. The recruitment
was done during the rst 2 weeks of
JanuaryandJuly, followedbysubsequent
5 months of follow-up, respectively. This
ensured the assessment of outcomes for
a complete year from January 2011 to
January 2012, to minimize the effect of
seasonality.
Randomization and Blinding
Random sequence was generated by
simple randomization method using
computer-generated random numbers
(Excel 2010). The bottles were labeled
with serial numbers in the Department
of Community Medicine, Maulana Azad
Medical College, by DKT, without the
knowledge of the eld investigator (AM).
The eld investigator and parents were
blinded to the treatment allocation and
unblinding was done at the end of the
follow-up period for all 272 infants.
Intervention
The zinc and placebo syrups were pre-
pared by Abyss Pharma (Delhi, India).
Each 5 mL of the preparation containing
placebo (syrup base) or zinc (20 mg
elemental zinc as zinc sulfate) was
packed in similar-looking bottles. The
syrups were of similar color, taste, and
consistency. During the survey, after
ascertainingthe eligibility andobtaining
informed consent, the infants were en-
rolled sequentially. The mother received
the bottles with prelabeled serial num-
bers. Theeldinvestigatoradministered
the rst dose of the intervention at the
time of enrollment and advised the
mother to give 5 mL of syrup (using
a standard 5-mL plastic spoon) daily to
the infant for the remaining 13 days.
Subsequently, visits were made on the
7th and the 14th days to ensure com-
pliance. If the syrup had not been given
regularly, a maximum of 1 week was
given to complete the dosages. We col-
lected data for any possible side effects
as reported by the caregivers during
these visits. To ensure that the childdid
not receive additional doses of zinc, we
provided mothers with identity cards
indicating the study title and that the
infants had received zinc syrup. These
cards were to be produced whenever
the child was taken to any medical
practitioner.
Outcomes and Follow-up
Theprimary outcomewas theincidence
of diarrhea per child-year. Diarrhea
was dened as 3 or more loose, liquid,
or watery stools or any change in
consistency or frequency of stools or
at least 1 loose stool containing blood
in a 24-hour period.
12
Secondary out-
comes included incidence density of
acute diarrhea, dysentery, and persis-
tent diarrhea; duration of diarrhea;
and side effects. Acute diarrhea was
dened as an episode of diarrhea
lasting up to 14 days. If an episode
lasted for .14 days, it was dened as
persistent diarrhea.
12
The episode was
classied as dysentery if the stool con-
tained blood.
12
Duration was assessed
as the number of days with diarrhea
ARTICLE
PEDIATRICS Volume 132, Number 1, July 2013 e47
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
and as mean number of days a di-
arrheal episode lasted. A baseline as-
sessment (Table 1) was done at the time
of recruitment, which included weight
and length measurements using a
Salter weighing scale (up to 100 g
[Model no. 235 6M; Salter India Ltd,
Daryaganj, New Delhi, India]) and an
Infantometer (up to 1 mm[model no: AM
1744; ATICO Medical Pvt Ltd, Haryana,
India]) respectively. All the outcomes
were assessed by a trained eld
investigator.
Follow-up for diarrhea began on the
15th day after intervention. Each child
was followed-up fortnightly 63 days
and the follow-up continued for 5
months after the completion of zinc/
placebo supplementation. At each
follow-up, the mother/caregiver was
asked about the occurrence of di-
arrhea during the previous 15 days.
Recovery from a diarrheal episode was
considered when the last day of di-
arrhea was followed by a 72-hour
diarrhea-free period.
6
Subsequent epi-
sodes were considered to be new di-
arrheal episodes.
Sample Size
The sample size was calculated taking
into account 4 primary outcomes: de-
crease in incidence of diarrhea, acute
respiratory tract infections, and in-
crease in length and weight. For di-
arrhea, previous studies in similar
populations estimated an incidence of
9.1 episodes (SD = 4.5) per child-year.
7,9
Thus, for a 20% reduction in the
incidence of diarrhea (a = 0.05 and
power 80%), we required 90 infants in
each group. However, the largest
sample size required (for acute re-
spiratory tract infection) was 258; thus,
we recruited the entire population of
216 infants from Gokulpuri and an
additional 56 infants from Gangavihar
(total = 272). The outcomes for di-
arrhea were assessed for all recruited
infants.
Statistical Analysis
Thedatawerecollectedandcheckedfor
accuracy on a daily basis and entered
into SPSS version 16 (IBM SPSS Sta-
tistics, IBM Corporation, Chicago, IL).
The incidence density was expressedas
episodes per child per year. The counts
were expressed by means and SD.
Difference between means was tested
using t-test, for normally distributed
data, or Mann-Whitney U test, for skewed
data.
Generalized estimating equations were
used to obtain an incident rate ratio
(IRR) with 95% condence intervals
(CIs), to compare monthwise number
of episodes and duration of diarrhea
using Poisson log linear distribution,
by intention-to-treat analysis. The ex-
changeable working correlation matrix
was selected for all the outcomes. We
included all children who had taken at
least 2 doses of the intervention for the
analyses. The follow-up visits for which
the infant outcomes were not available
were imputed using the worst-case (2
episodes of diarrhea) and best-case
scenarios (no episodes). However, this
did not change the study results; thus,
we present in this article results from
complete data set analysis. We decided
to adjust the IRRs for covariates that
appeared to be different at baseline in
the 2 groups. We also decided to com-
pare the monthwise mean episodes of
diarrhea in the 2 groups.
Socioeconomic status was assessed by
using the Modied Kuppuswamy Scale
(based on education and occupation of
family head and total family income)
modied for Consumer Price Index for
industrial workers of India for 2011.
13
The z-scores for length and weight were
calculated by using World Health Orga-
nization reference tables for length and
weight.
14,15
Observation and Results
From a total of 3155 households iden-
tied during the house to house survey,
we assessed 272 infants for eligibility
(Fig 1). As there were no exclusions and
refusals, all the infants were recruited.
A total of 141 infants received zinc
and 131 received placebo. Both groups
shared similar baseline characteristics
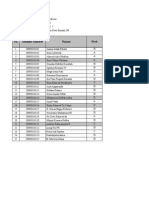
TABLE 1 Baseline Characteristics of the Study Subjects at the Time of Recruitment
Characteristic Zinc (n = 141) Placebo (n = 131)
Gender, n (%)
Male 67 (47.5) 68 (51.9)
Female 74 (52.5) 63 (48.1)
Age, mo, mean 6 SD 8.77 6 1.73 8.76 6 1.86
Socioeconomic status, n (%)
Upper 4 (2.8) 4 (3.1)
Upper Middle 39 (27.7) 30 (22.9)
Lower Middle 65 (46.1) 58 (44.3)
Lower 33 (23.4) 39 (29.8)
Average oor space per person, square meters 6 SD 7.75 6 4.13 8.26 6 5.21
Household water purication device, n (%)
Yes 31 (22.0) 23 (17.6)
No 110 (78.0) 108 (82.4)
Feeding type, n (%)
Exclusive breastfeeding 13 (9.2) 16 (12.2)
Complementary feeding 12 (8.5) 11 (8.4)
Both 116 (82.3) 104 (79.4)
Length, cm, mean 6 SD 67.4 6 3.86 67.6 6 3.82
Mean z score 21.76 6 1.46 21.69 6 1.48
Stunted (,2Z WHO) , n (%) 51 (36.0) 54 (41.0)
Weight, kg, mean 6 SD 7.26 6 1.1 7.21 6 1.2
Mean Z score 21.50 6 1.15 21.58 6 1.21
Wasted (,2Z WHO) , n (%) 44 (31.2) 53 (41.0)
WHO, World Health Organization.
e48 MALIK et al
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
(Table 1). Seven families (n = 4 in the
zinc group and n = 3 in the placebo
group, respectively) migrated during
the study period. The mean number of
follow-ups was 10 in each group (zinc:
10.0 6 0.75, placebo: 10.0 6 0.76, P =
.721). The nal analyses included 134
infants in the zinc group and 124 in the
placebo group, who had completed the
study. A total of 19 infants (13.5%) in
the zinc group and 26 infants (20%)
in the placebo group were given an
additional 1 week to complete the in-
tervention, as they were found to be
initially noncompliant.
Effect on Diarrhea
Zincsupplementationfor14dayscaused
a signicant reduction in the number of
episodes of diarrhea. Of the total 829
episodes observed, 329 episodes oc-
curred in the zinc group and 500 in the
placebo group, accounting for an in-
cidence of 6.07 and 9.90 per child year
respectively, at the end of 5 months
(Table 2). Generalized estimating equa-
tion regression model showed that there
was a reduction of 39% (adjusted IRR
0.61, 95% CI 0.530.71) in episodes of
diarrhea in the zinc group as compared
with the placebo group after the model
was adjusted for wasting.
When types of diarrhea were analyzed
separately (Table 2), we found a signif-
icant decrease of 31% in the episodes
of acute diarrhea (adjusted IRR 0.69,
95% CI 0.590.81), 70% in the episodes
of persistent diarrhea (adjusted IRR
0.30, 95% CI 0.170.51), and more than
95% in the episodes of dysentery (ad-
justed IRR 0.03, 95% CI 0.010.24) in the
zinc group.
Zinc supplementation led to a signicant
reductionof 39%(adjustedrateratio[RR]
0.61, 95% CI 0.540.69) in overall days
with diarrhea. There was also a signi-
cant reduction of 36% in duration per
episode of diarrhea (adjusted RR 0.64,
95% CI 0.560.74) observed in the zinc
group (Table 3).
Zinc signicantly reduced the mean
episodes of diarrhea for each of the
5 months (Table 4). However, the level of
signicance decreased after the third
month.
Side Effects
Reported side effects were diarrhea,
vomiting, and constipation. The per-
centage of children reporting these
were 9.0%, 10.4%, and1.5%, respectively,
in the zinc group and 7.3%, 4.8%, and0%,
respectively, in the placebo group, and
the difference was nonsignicant in the
2 groups.
Onedeathduetodiarrheawasreportedin
thezincgroup3monthsafterrecruitment.
Verbal autopsy revealed severe de-
hydrationduetononadministrationof oral
rehydrationsolutionortheavailablehome
uids were the cause of death. The fact
that the death took place 3 months after
intervention, and the incorrect man-
agement revealed in the verbal autopsy,
rules out any possible role of zinc.
DISCUSSION
In the current trial, we report that
prophylactic zinc supplementation for
2 weeks signicantly reduced the in-
cidence and duration of diarrhea dur-
ing follow-up of 5 months. Although we
studied additional outcomes (ie, acute
respiratory tract infections andgrowth),
the results of these will be reported
separately.
Zinc depletion leads to upregulation of
neuropeptides, such as cyclic guanosine
monophosphate, and acute-phase reac-
tants, such as interleukin 1, which cre-
ates secretory conditions in the intestine
leading to diarrheal episodes.
16
Thus,
zinc prophylaxis in zinc-decient pop-
ulations reduces diarrheal morbidity.
The major limitation of this study is that
serum zinc levels were not done to as-
sess the deciency and the subsequent
effect onserumzinclevels. Nevertheless,
previous studies in similar populations
FIGURE 1
Trial Prole.
ARTICLE
PEDIATRICS Volume 132, Number 1, July 2013 e49
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
of Delhi have shown high prevalence of
zinc deciency (normal: 11.522.2 mM)
to the extent of 73.3% for values
,10.4 mM and 33.8% for values ,9.0
mM.
3
Moreover, in our study, the pro-
portion of stunted infants was .20%,
which suggests an elevated risk of zinc
deciency, because stunting is a proxy
indicator of zinc deciency in population
studies.
17
Also, baseline data on in-
cidence density of diarrhea in this age
group were not available.
Among the studies in which short-
course zinc prophylaxis of 2 weeks
was used, only 1 study had shown sig-
nicant reduction in the incidence
of diarrhea in a 12- to 35-month age
group.
18
Previous studies, which were
carried out in infants of 6 to 11 months,
have shown similar results to the
current trial but after continuous zinc
supplementation.
1922
One of these tri-
als was carried out in a cohort of low
birth weight infants.
20
Trials have also
shown the effectiveness of continuous
zinc prophylaxis among wider age groups
(641 months and 635 months, re-
spectively), but subgroup analysis for
children ,12 months of age was not
done.
23,24
In a large study done in a sim-
ilar population of Delhi as the current
trial, zinc prophylaxis of 4 months was
found to be effective only in children .12
months of age.
25
Thus, unlike the previous
studies, the current trial showed that
short-course zinc prophylaxis signi-
cantly reduced diarrheal incidence in an
age group of 6 to 11 months.
Zinc prophylaxis was shown to reduce
the incidence of diarrhea in both con-
tinuous as well as short-course sup-
plementationtrials, in2meta-analyses.
8,9
However, the benecial effect was lim-
ited to children .12 months of age.
In the current trial, a signicant re-
duction of days with diarrhea per child
and duration per episode of diarrhea
was observed. In contrast, results of 2
previous trials have shown no effect of
continuous zinc prophylaxis on the
duration of diarrhea. Of these, 1 study
was done in the age group of 6 to
9 months and another in the age group
of 18 to 36 months.
19,26
Of the 2 meta-
analyses, 1 with continuous zinc sup-
plementation trials showed fewer total
days with diarrhea,
27
whereas the other,
which included studies with continuous
and short-course zinc supplementa-
tion, showed no effect on duration of
diarrhea.
7
A signicant reduction in incidence
was seen when diarrhea was further
classied into acute diarrhea, persis-
tent diarrhea, and dysentery in the
current trial. In the past, only 1 study
concluded that the incidence of acute
diarrhea was reduced signicantly by
zinc supplementation, but in a wider
age group (635 months).
28
Three
studies, which had a similar age group
or analyzed results for children ,12
months of age, showed no signicant
decrease in persistent diarrhea in
the zinc group.
6,22,24
Although both
the meta-analyses show that risk of
persistent diarrhea did decrease
with zinc supplementation, subgroup
analysis for the 6 to 11 months
age group is not available.
9,27
Also
one of these meta-analyses included
studies with continuous zinc supple-
mentation only. Regarding dysentery,
only 1 study showed signicant re-
duction in incidence of dysentery fol-
lowing zinc supplementation, that too
in a wide age group of 6 to 35 months
with continuous supplementation.
24
TABLE 2 Effect of Zinc Supplementation on Incidence of Diarrhea on the Study Subjects
Intervention Child Years
Observed
Incidence
(Episodes Child
1
year
21
)
Crude IRR
(95% CI)
Adjusted IRR
a
(95% CI)
All forms of diarrhea
Zinc 54.08 6.07 0.61 (0.560.74) 0.61 (0.530.71)
Placebo 50.25 9.90 1.00 1.00
Acute diarrhea
Zinc 54.08 5.77 0.68 (0.570.83) 0.69 (0.590.81)
Placebo 50.25 8.33 1.00 1.00
Persistent diarrhea
Zinc 54.08 0.28 0.29 (0.170.51) 0.30 (0.180.53)
Placebo 50.25 1.01 1.00 1.00
Dysentery
Zinc 54.08 0.02 0.032 (0.0040.24) 0.030 (0.010.24)
Placebo 50.25 0.58 1.00 1.00
a
Adjusted for wasting.
TABLE 3 Effect of Zinc Supplementation on Days with Diarrhea and Duration per Episode of
Diarrhea
Duration Intervention P Value
b
Crude RR
(95% CI)
Adjusted RR
c
(95% CI)
Zinc
(n = 118)
a
Placebo
(n = 116)
a
Mean 6SD of days with diarrhea 10.10 6 7.06 23.19 6 13.8 ,.001 0.60 (0.530.76) 0.61 (0.540.69)
Mean 6 SD days per episode 3.60 6 2.23 5.34 6 2.16 ,.001 0.63 (0.550.77) 0.64 (0.560.74)
RRrate ratio.
a
The children with 0 episodes were excluded.
b
Mann-Whitney U test, P , .05 considered signicant.
c
Adjusted for wasting.
TABLE 4 Monthwise Episodes of Diarrhea in
the 2 Study Groups
Month Zinc Placebo P Value
a
Mean (SD) Mean (SD)
First 0.44 (0.60) 0.85 (0.84) ,.0001
Second 0.40 (0.56) 0.83 (0.87) ,.0001
Third 0.49 (0.65) 0.88 (0.77) ,.0001
Fourth 0.58 (0.65) 0.82 (0.78) .014
Fifth 0.61 (0.80) 0.77 (0.73) .037
a
Mann-Whitney U test, P , .05 considered signicant.
e50 MALIK et al
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
A study with short-course zinc sup-
plementation showed a nonsignicant
reduction in incidence of dysentery
in the age group of 12 to 35 months.
18
Of the 2 meta-analyses, 1 is in agree-
ment with the current trial, although
the age group is wide in this meta-
analysis and studies with only con-
tinuous zinc supplementation have
been included.
9,27
Among the previous studies in similar
populations, we found that 1 study
may have insufcient power to detect
a signicant decrease in diarrhea
morbidity in infants 6 to 11 months of
age.
25
In other studies, zinc pro-
phylaxis was given to a subset of the
population that had already received
therapeutic zinc for acute diarrhea,
which might have led to reduced ef-
fectiveness of the subsequent zinc
prophylaxis.
5,7,24,28
However, the cur-
rent study was done in a population
that had not received zinc supple-
mentation for the preceding 3 months,
was apparently healthy, and had
a high proportion of wasted and
stunted infants. This, coupled with the
fact that the maximum burden of di-
arrhea is seen in the age group of 6
to 11 months,
11
may have been re-
sponsible for such signicant results
in the current study.
CONCLUSIONS
Previous trials and meta-analyses have
shown the benecial effect of zinc
prophylaxis on diarrhea either by
continuous supplementation for a long
duration, ranging from 3 months to
1 year, or in age groups of .12 months.
The current study was able to show
signicant reduction in diarrhea mor-
bidity in infants of 6 to 11 months,
even 5 months after short-course zinc
prophylaxis.
The advantage of zinc given as a
community-based prophylactic interven-
tion is that all children in the target
population will be covered. This in turn
will reduce the overall incidence of
diarrhea in the community compared
with administration of zinc only to
children who seek treatment for di-
arrhea. This is because many children
suffering from diarrhea may not come
to a health facility, as is common in the
slum populations, and thus keep suf-
fering from repeated episodes of di-
arrhea. The difculty of having to give
zinc to apparently healthy children is
that the delivery strategy has to be
community based, thus requiring ad-
ditional time and work on the part
of the health workers/community
volunteers.
The results of this study have important
cost and operational implications, as
short-course prophylaxis of zinc in an
adequate dose might be more feasible
than continuous therapies.
The results of this study may be
extrapolated to similar zinc-decient
populations only. Future trials on the
effect of zinc prophylaxis on diarrhea
should concentrate on zinc-decient
pockets in both developed and de-
veloping countries. It is desirable that
such trials follow a standardized pro-
cedureregardingthedurationanddose
of zinc prophylaxis. This would ensure
that policy makers have reliable and
valid evidence to implement zinc pro-
phylaxis programs for those child
populations that will benet the most
from them.
REFERENCES
1. Beisel WR. Single nutrients and immunity.
Am J Clin Nutr. 1982;35(suppl 2):417468
2. Black RE. Zinc deciency, immune function,
and morbidity and mortality from in-
fectious disease among children in de-
veloping countries. Food Nutr Bull. 2001;22:
155162
3. Baqui AH, Black RE, El Arifeen S, et al. Effect
of zinc supplementation started during
diarrhea on morbidity and mortality in
Bangladeshi children: community random-
ized trial. BMJ. 2002;325(7372):1059
4. Walker CL, Black RE. Zinc for the treatment
of diarrhoea: effect on diarrhoea morbid-
ity, mortality and incidence of future epi-
sodes. Int J Epidemiol. 2010;39(suppl 1):
i63i69
5. Sazawal S, Black RE, Bhan MK. Effect of zinc
supplementation during acute diarrhea on
duration and severity of the episode
a community based double-blind controlled
trial. N Engl J Med. 1995;333:839844
6. Sazawal S, Black RE, Bhan MK, et al. Zinc
supplementation reduces the incidence of
persistent diarrhea and dysentery among
low socioeconomic children in India. J Nutr.
1996;126(2):443450
7. Sazawal S, Black RE, Bhan MK, Jalla S,
Sinha A, Bhandari N. Efcacy of zinc sup-
plementation in reducing the incidence and
prevalence of acute diarrheaa community-
based, double-blind, controlled trial. Am J
Clin Nutr. 1997;66(2):413418
8. Brown KH, Peerson JM, Baker SK, Hess SY.
Preventive zinc supplementation among
infants, preschoolers, and older prepubertal
children. Food Nutr Bull. 2009;30(suppl 1):
S12S40
9. Bhutta ZA, Black RE, Brown KH, et al. Pre-
vention of diarrhea and pneumonia by zinc
supplementation in children in developing
countries: pooled analysis of randomized
controlled trials. Zinc Investigators Col-
laborative Group. J Pediatr. 1999;135(6):
689697
10. Brown KH, Rivera JA, Bhutta Z, et al; In-
ternational Zinc Nutrition Consultative
Group (IZiNCG). Assessment of the risk of
zinc deciency in populations. Food Nutr
Bull. 2004;25(1 suppl 2):S99S203
11. Kosek M, Bern C, Guerrant RL. The global
burden of diarrhoeal disease, as estimated
from studies published between 1992 and
2000. Bull World Health Organ. 2003;81:
197204
12. World Health Organization. Diarrhoeal dis-
ease. Available at: www.who.int/mediacentre/
ARTICLE
PEDIATRICS Volume 132, Number 1, July 2013 e51
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
factsheets/fs330/en/index.html. Accessed
October 7, 2010
13. Kuppuswamy B. Manual of Socioeconomic
Status (Urban). Delhi, India: Manasayan; 1981
14. World Health Organization. Child growth
standards. Weight-for-age. Available at: www.
who.int/childgrowth/standards/weight_for_
age/en/index.html. Accessed July 23, 2011
15. World Health Organization. Child growth
standards. Length/height-for-age. Available
at: www.who.int/childgrowth/standards/
height_for_age/en/index.html. Accessed
July 23, 2011
16. Wapnir RA. Zinc deciency, malnutrition
and the gastrointestinal tract. J Nutr. 2000;
130(suppl 5S):1388S1392S
17. de Benoist B, Darnton-Hill I, Davidsson L,
Fontaine O, Hotz C. Conclusions of the joint
WHO/UNICEF/IAEA/IZiNCG interagency meet-
ing on zinc status indicators. Food Nutr
Bull. 2007;28(suppl 3):S480S484
18. Rahman MM, Vermund SH, Wahed MA,
Fuchs GJ, Baqui AH, Alvarez JO. Simulta-
neous zinc and vitamin A supplementation
in Bangladeshi children: randomised dou-
ble blind controlled trial. BMJ. 2001;323
(7308):314318
19. Ruel MT, Rivera JA, Santizo MC, Lnnerdal B,
Brown KH. Impact of zinc supplementation
on morbidity from diarrhea and respiratory
infections among rural Guatemalan chil-
dren. Pediatrics. 1997;99(6):808813
20. Sur D, Gupta DN, Mondal SK, et al. Impact of
zinc supplementation on diarrheal mor-
bidity and growth pattern of low birth
weight infants in Kolkata, India: a ran-
domized, double-blind, placebo-controlled,
community-based study. Pediatrics. 2003;
112(6 pt 1):13271332
21. Brooks WA, Santosham M, Naheed A, et al.
Effect of weekly zinc supplements on in-
cidence of pneumonia and diarrhoea in
children younger than 2 years in an urban,
low-income population in Bangladesh:
randomised controlled trial. Lancet. 2005;
366(9490):9991004
22. Long KZ, Montoya Y, Hertzmark E, Santos JI,
Rosado JL. A double-blind, randomized,
clinical trial of the effect of vitamin A and
zinc supplementation on diarrheal disease
and respiratory tract infections in children
in Mexico City, Mexico. Am J Clin Nutr. 2006;
83(3):693700
23. Gupta DN, Mondal SK, Ghosh S, Rajendran
K, Sur D, Manna B. Impact of zinc supple-
mentation on diarrhoeal morbidity in rural
children of West Bengal, India. Acta Pae-
diatr. 2003;92(5):531536
24. Penny ME, Marin RM, Duran A, et al. Ran-
domized controlled trial of the effect of
daily supplementation with zinc or multiple
micronutrients on the morbidity, growth,
and micronutrient status of young Peruvian
children. Am J Clin Nutr. 2004;79(3):457
465
25. Bhandari N, Bahl R, Taneja S, et al. Sub-
stantial reduction in severe diarrheal mor-
bidity by daily zinc supplementation in
young north Indian children. Pediatrics.
2002;109(6). Available at: www.pediatrics.
org/cgi/content/full/109/6/e86
26. Rosado JL, Lpez P, Muoz E, Martinez H,
Allen LH. Zinc supplementation reduced
morbidity, but neither zinc nor iron sup-
plementation affected growth or body
composition of Mexican preschoolers. Am J
Clin Nutr. 1997;65:1319
27. Aggarwal R, Sentz J, Miller MA. Role of zinc
administration in prevention of childhood
diarrhea and respiratory illnesses: a meta-
analysis. Pediatrics. 2007;119(6):11201130
28. Larson CP, Nasrin D, Saha A, Chowdhury MI,
Qadri F. The added benet of zinc supple-
mentation after zinc treatment of acute
childhood diarrhoea: a randomized, double-
blind eld trial. Trop Med Int Health. 2010;15
(6):754761
e52 MALIK et al
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
DOI: 10.1542/peds.2012-2980
; originally published online June 3, 2013; 2013;132;e46 Pediatrics
Akash Malik, Davendra K. Taneja, Niveditha Devasenapathy and K. Rajeshwari
Infants of 6 to 11 Months
Short-Course Prophylactic Zinc Supplementation for Diarrhea Morbidity in
Services
Updated Information &
ml
http://pediatrics.aappublications.org/content/132/1/e46.full.ht
including high resolution figures, can be found at:
References
ml#ref-list-1
http://pediatrics.aappublications.org/content/132/1/e46.full.ht
at:
This article cites 24 articles, 14 of which can be accessed free
Citations
ml#related-urls
http://pediatrics.aappublications.org/content/132/1/e46.full.ht
This article has been cited by 1 HighWire-hosted articles:
Subspecialty Collections
cs_sub
http://pediatrics.aappublications.org/cgi/collection/therapeuti
Therapeutics
ogy_sub
http://pediatrics.aappublications.org/cgi/collection/pharmacol
Pharmacology
rology_sub
http://pediatrics.aappublications.org/cgi/collection/gastroente
Gastroenterology
the following collection(s):
This article, along with others on similar topics, appears in
Permissions & Licensing
tml
http://pediatrics.aappublications.org/site/misc/Permissions.xh
tables) or in its entirety can be found online at:
Information about reproducing this article in parts (figures,
Reprints
http://pediatrics.aappublications.org/site/misc/reprints.xhtml
Information about ordering reprints can be found online:
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Grove Village, Illinois, 60007. Copyright 2013 by the American Academy of Pediatrics. All
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
at Indonesia:AAP Sponsored on April 17, 2014 pediatrics.aappublications.org Downloaded from
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Primary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyDocument7 pagesPrimary Surgery Versus Chemoradiotherapy For Advanced Oropharyngeal Cancers: A Longitudinal Population StudyLuvita Amallia SyadhatinPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Incident Reporting FormDocument1 pageIncident Reporting FormCollin NguPas encore d'évaluation
- Neuro AnatomyDocument26 pagesNeuro AnatomylistiarsasihPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Pimsleur - French III - Course TextDocument14 pagesPimsleur - French III - Course TextFlávio José LindolfoPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Meningitis (Hal 225) Daftar Pustaka: Penyakit Jilid 2Document2 pagesMeningitis (Hal 225) Daftar Pustaka: Penyakit Jilid 2listiarsasihPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The New FriendDocument1 pageThe New FriendlistiarsasihPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- 603-606 12.27 Saima Hafeez KhokharDocument4 pages603-606 12.27 Saima Hafeez KhokharlistiarsasihPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Critical Review Qual Form1Document4 pagesCritical Review Qual Form1Ekhy BarryPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Spiritual LeadershipDocument11 pagesSpiritual Leadershipmisy_musyPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Migra inDocument9 pagesMigra inlistiarsasihPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- English ScoreDocument1 pageEnglish ScorelistiarsasihPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Cardiopulmonary System: Blok 16Document1 pageCardiopulmonary System: Blok 16listiarsasihPas encore d'évaluation
- Jurnal BSC 6Document5 pagesJurnal BSC 6FazaKhilwanAmnaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Indonesia's Policy On CDM Implementation: Prasetyadi Utomo Ministry of Environment of IndonesiaDocument14 pagesIndonesia's Policy On CDM Implementation: Prasetyadi Utomo Ministry of Environment of IndonesialistiarsasihPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Blok 22Document1 pageBlok 22listiarsasihPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Fluid Resuscitation in Acute Illness PDFDocument2 pagesFluid Resuscitation in Acute Illness PDFlistiarsasihPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Role of Transrectal Ultrasound-Guided Biopsy in Diagnosis of Prostate CancerDocument7 pagesThe Role of Transrectal Ultrasound-Guided Biopsy in Diagnosis of Prostate CancerlistiarsasihPas encore d'évaluation
- Blok 24Document1 pageBlok 24listiarsasihPas encore d'évaluation
- Blok 22Document1 pageBlok 22listiarsasihPas encore d'évaluation
- 7 Ways To Love YourselfDocument7 pages7 Ways To Love YourselflistiarsasihPas encore d'évaluation
- Blok 21Document1 pageBlok 21listiarsasihPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elective Block of Research: Blok 20Document1 pageElective Block of Research: Blok 20listiarsasihPas encore d'évaluation
- Blok 19Document1 pageBlok 19listiarsasihPas encore d'évaluation
- CLASSROOM LANGUAGE - Creating A WorkshopDocument5 pagesCLASSROOM LANGUAGE - Creating A WorkshoplistiarsasihPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Public Health and Community Medicine: Blok 23Document1 pagePublic Health and Community Medicine: Blok 23listiarsasihPas encore d'évaluation
- Blok 12Document1 pageBlok 12listiarsasihPas encore d'évaluation
- Blok 14Document1 pageBlok 14listiarsasihPas encore d'évaluation
- Blok 24Document1 pageBlok 24listiarsasihPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Infection and Immunity: Blok 6Document1 pageInfection and Immunity: Blok 6listiarsasihPas encore d'évaluation
- Blok 18Document1 pageBlok 18listiarsasihPas encore d'évaluation
- Togaf Open Group Business ScenarioDocument40 pagesTogaf Open Group Business Scenariohmh97Pas encore d'évaluation
- Network Function Virtualization (NFV) : Presented By: Laith AbbasDocument30 pagesNetwork Function Virtualization (NFV) : Presented By: Laith AbbasBaraa EsamPas encore d'évaluation
- K3VG Spare Parts ListDocument1 pageK3VG Spare Parts ListMohammed AlryaniPas encore d'évaluation
- Special Warfare Ma AP 2009Document28 pagesSpecial Warfare Ma AP 2009paulmazziottaPas encore d'évaluation
- Gee 103 L3 Ay 22 23 PDFDocument34 pagesGee 103 L3 Ay 22 23 PDFlhyka nogalesPas encore d'évaluation
- What Is SCOPIC Clause - A Simple Overview - SailorinsightDocument8 pagesWhat Is SCOPIC Clause - A Simple Overview - SailorinsightJivan Jyoti RoutPas encore d'évaluation
- TEsis Doctoral en SuecoDocument312 pagesTEsis Doctoral en SuecoPruebaPas encore d'évaluation
- Final Module in Human BehaviorDocument60 pagesFinal Module in Human BehaviorNarag Krizza50% (2)
- Chain of CommandDocument6 pagesChain of CommandDale NaughtonPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Q & A Set 2 PDFDocument18 pagesQ & A Set 2 PDFBharathiraja MoorthyPas encore d'évaluation
- Laboratory Methodsin ImmnunologyDocument58 pagesLaboratory Methodsin Immnunologyadi pPas encore d'évaluation
- DMSCO Log Book Vol.25 1947Document49 pagesDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomPas encore d'évaluation
- List of Vocabulary C2Document43 pagesList of Vocabulary C2Lina LilyPas encore d'évaluation
- Introduction To Philosophy of The Human Person: Presented By: Mr. Melvin J. Reyes, LPTDocument27 pagesIntroduction To Philosophy of The Human Person: Presented By: Mr. Melvin J. Reyes, LPTMelvin J. Reyes100% (2)
- Gamboa Vs Chan 2012 Case DigestDocument2 pagesGamboa Vs Chan 2012 Case DigestKrissa Jennesca Tullo100% (2)
- Monastery in Buddhist ArchitectureDocument8 pagesMonastery in Buddhist ArchitectureabdulPas encore d'évaluation
- Pediatric ECG Survival Guide - 2nd - May 2019Document27 pagesPediatric ECG Survival Guide - 2nd - May 2019Marcos Chusin MontesdeocaPas encore d'évaluation
- SANDHU - AUTOMOBILES - PRIVATE - LIMITED - 2019-20 - Financial StatementDocument108 pagesSANDHU - AUTOMOBILES - PRIVATE - LIMITED - 2019-20 - Financial StatementHarsimranSinghPas encore d'évaluation
- Contoh RPH Ts 25 Engish (Ppki)Document1 pageContoh RPH Ts 25 Engish (Ppki)muhariz78Pas encore d'évaluation
- Answers To Quiz No 19Document5 pagesAnswers To Quiz No 19Your Public Profile100% (4)
- Outline - Criminal Law - RamirezDocument28 pagesOutline - Criminal Law - RamirezgiannaPas encore d'évaluation
- HTTP Parameter PollutionDocument45 pagesHTTP Parameter PollutionSpyDr ByTePas encore d'évaluation
- Entrep Bazaar Rating SheetDocument7 pagesEntrep Bazaar Rating SheetJupiter WhitesidePas encore d'évaluation
- Thomas Noochan Pokemon Review Final DraftDocument6 pagesThomas Noochan Pokemon Review Final Draftapi-608717016Pas encore d'évaluation
- Sample A: For Exchange Students: Student's NameDocument1 pageSample A: For Exchange Students: Student's NameSarah AuliaPas encore d'évaluation
- Wwe SVR 2006 07 08 09 10 11 IdsDocument10 pagesWwe SVR 2006 07 08 09 10 11 IdsAXELL ENRIQUE CLAUDIO MENDIETAPas encore d'évaluation
- MPU Self Reflection Peer ReviewDocument3 pagesMPU Self Reflection Peer ReviewysaPas encore d'évaluation
- RSA ChangeMakers - Identifying The Key People Driving Positive Change in Local AreasDocument29 pagesRSA ChangeMakers - Identifying The Key People Driving Positive Change in Local AreasThe RSAPas encore d'évaluation
- Scientific Errors in The QuranDocument32 pagesScientific Errors in The QuranjibranqqPas encore d'évaluation
- Government College of Engineering Jalgaon (M.S) : Examination Form (Approved)Document2 pagesGovernment College of Engineering Jalgaon (M.S) : Examination Form (Approved)Sachin Yadorao BisenPas encore d'évaluation