Académique Documents
Professionnel Documents
Culture Documents
24584823
Transféré par
Pascalis Adhi KurniawanCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
24584823
Transféré par
Pascalis Adhi KurniawanDroits d'auteur :
Formats disponibles
Current Pharmaceutical Design, 2007, 13, 793-800 793
1381-6128/07 $50.00+.00 2007 Bentham Science Publishers Ltd.
Casein Phosphopeptides in Oral Health - Chemistry and Clinical
Applications
K.J. Cross, N.L. Huq and E.C. Reynolds
*
Centre for Oral Health Science, School of Dental Science, The University of Melbourne, 720 Swanston Street, Victoria,
3000, Australia
Abstract: The casein phosphopeptides (CPP) are derived from the milk protein casein by tryptic digestion. The CPP, con-
taining the sequence -Pse-Pse-Pse-Glu-Glu- where Pse is a phosphoseryl residue, stabilize calcium and phosphate ions in
aqueous solution and make these essential nutrients bioavailable. Under alkaline conditions the calcium phosphate is pre-
sent as an alkaline amorphous phase complexed by the CPP, referred to as casein phosphopeptide-amorphous calcium
phosphate (CPP-ACP). The CPP-ACP complexes readily incorporate fluoride ions forming casein phosphopeptide-
amorphous calcium fluoride phosphate (CPP-ACFP). A mechanism is discussed which provides a rationale for the ability
of the CPP-ACP to remineralize carious lesions in dental enamel. Clinical applications of the CPP-ACP as agents in the
treatment of dental caries and other hypomineralized conditions are reviewed. It is concluded that the CPP are a safe and
novel carrier for calcium, phosphate and hydroxide (fluoride) ions to promote enamel remineralization with application in
oral care products, dental professional products and foodstuffs.
Key Words: Anticariogenic casein phosphopeptides, calcium phosphate delivery vehicle, structure, clinical studies nanocom-
plex.
BACKGROUND
Dental Caries
Dental caries is the most prevalent human disease of bac-
terial origin and is still a major public health problem, par-
ticularly in low socio-economic groups [1]. The disease
process is initiated via the demineralization of tooth hard
tissue by organic acids that result from the fermentation of
dietary sugar by dental plaque odontopathogenic bacteria [2].
Even though in most developed countries the prevalence of
dental caries has decreased through the use of fluorides, the
disease remains a major public health problem [1]. The re-
cently published [1] Child Dental Health Survey, Australia
1996 provides an insight into the scale of this public health
problem. The survey found 40.2% of 6 yr-olds showed signs
of dental caries [decayed, missing (due to caries) or filled
teeth] and 48.6% of 12 yr-olds showed signs of the disease.
Untreated clinically detectable decay in the combined de-
ciduous and permanent dentition was present for 35.3% of
children in the age range 5 to 15 years with the greatest se-
verity occurring in the youngest ages (e.g. 9.1% of 5 year-
olds had 4 or more teeth with untreated decay). The level of
disease in these high-risk children has decreased only
slightly in recent years, (e.g. the proportion of 6 yr-olds with
4 or more decayed, missing or filled teeth reduced by only
3.7% between 1989 and 1996). Therefore, although the car-
ies experience of the general population of children has im-
proved significantly, a significant percentage of high-risk
children remains that require further targeting. Recent dental
*Address correspondence to this author at the Centre for Oral Health Sci-
ence, School of Dental Science, The University of Melbourne, 720
Swanston Street, Victoria, 3000, Australia; Tel: +61 3 9341 1548; Fax: +61
3 9341 1596; E-mail: e.reynolds@unimelb.edu.au
health surveys [1] in young and older adults have indicated
that the gains in oral health made in childhood are not neces-
sarily carried into later years as these age cohorts exhibit
higher percentages of high caries-risk individuals. For exam-
ple, 78% of young adults selected from the electoral roll in
Adelaide, a city with fluoridated reticulated water, showed
signs of tooth decay with a mean decayed, missing and filled
tooth (DMFT) index of 3.66, with over 10% of these indi-
viduals exhibiting a DMFT of 8 or more [1]. Demographic
changes and changing patterns of oral disease are resulting in
larger numbers of older Australians who are increasingly
dentate and at high risk of dental caries. A recent survey of
Adelaide nursing home residents [1] showed that 34% of the
residents were dentate with 41% of their teeth showing signs
of active decay with a mean DMFT of 23.7. The total cost of
providing dental services in Australia in 1998 was estimated
[1] at $2.6 billion with over 50% being attributed to treating
the consequences of dental caries. This economic burden is
higher than for any other dietary related disease including
coronary heart disease, hypertension or stroke [1, 3]. Recent
studies have highlighted a number of socio-demographic
variables associated with caries risk: high risk being associ-
ated with ethnicity and low socio-economic status [4]. The
level of high-risk individuals of all ages has remained rela-
tively constant even though the overall severity and preva-
lence of disease in the community has decreased [1, 4]. Den-
tal caries is therefore still a major public health problem in
Australia, particularly in recent migrants and lower socio-
economic groups who tend not to use dental services. Dental
caries is also becoming a concern in developing countries as
the consumption of more highly processed foods increases
[5]. This highlights the requirement for the development of a
non-toxic, anticariogenic agent that could supplement the
effects of fluoride in an approach to further lower caries ex-
perience.
794 Current Pharmaceutical Design, 2007, Vol. 13, No. 8 Cross et al.
Fluoride
Fluoride is currently regarded as an effective topical
agent for the prevention of caries by promoting enamel
remineralization with fluorapatite [6]. Topical fluoride has
been recommended for the non-invasive treatment of incipi-
ent enamel subsurface lesions, especially if the risk factors of
poor oral hygiene and high-caries-risk diet are also ad-
dressed.
A problem with fluoride ions is their low solubility in the
presence of salivary calcium and phosphate ions and hence
their rapid deposition with these ions in the surface layer of
the enamel lesion. This deposition in the surface layer then
blocks further ion penetration into the body of the carious
lesion thus limiting deeper remineralization [7].
Furthermore, for fluoride ions to remineralize enamel
subsurface lesions with fluorapatite, with a unit cell
stoichiometry of Ca
10
(PO
4
)
6
F
2
, 2 mol fluoride ions, are re-
quired for every 10 mol of calcium and 6 mol of phosphate
ions. Hence for many applications of topical fluorides the
level of calcium and phosphate ions will be the limiting fac-
tor for remineralization.
The clinical use of calcium phosphates to promote
enamel remineralization has not been successful. Soluble
calcium ions are not retained on the tooth surface in high
enough concentrations to promote diffusion into the subsur-
face enamel [8]. Insoluble calcium phosphates are also not
retained to any significant extent on the tooth surface and do
not provide bioavailable ions to promote enamel reminerali-
zation. A new technology has now been developed involving
phosphopeptides from the milk protein casein that localize
calcium and phosphate ions at the tooth surface and promote
enamel remineralization. The casein phosphopeptides (CPP)
stabilize calcium, phosphate and hydroxide (fluoride) ions
preventing spontaneous precipitation of hydroxyapatite
(fluorapatite). The CPP stabilized calcium, phosphate and
hydroxide (fluoride) ions substantially promote remineraliza-
tion of enamel subsurface lesions and therefore have the po-
tential as a superior form of fluoride for the prevention and
remineralization of incipient carious lesions and for the
remineralization of hypomineralized enamel lesions gener-
ally.
ANTICARIOGENIC FOODSTUFFS
Dairy Products
The food group most recognized as exhibiting anticaries
activity is dairy products (milk, milk concentrates, powders
and cheeses) [9]. Using in vitro, animal and in situ caries
models, the components largely responsible for this anticari-
ogenic activity have been identified as casein, calcium and
phosphate [9-15]. The bovine milk phosphoprotein, casein,
which is known to interact with calcium and phosphate [16]
and is a natural food component, is an obvious candidate for
an anticariogenic food and toothpaste additive, however this
is precluded by organoleptic properties and the very high
levels required for activity [9, 13, 15]. Using a human intra-
oral caries model, Reynolds [14] showed that digestion of
caseinate with trypsin did not destroy the protein's ability to
prevent enamel sub-surface demineralization. Tryptic pep-
tides of casein were found incorporated into the intra-oral
appliance plaque and were associated with a substantial in-
crease in the plaque's content of calcium and phosphate. It
was concluded that the tryptic peptides that were responsible
for the anticariogenic activity were the calcium phosphate
sequestering phosphopeptides.
Anticariogenic Casein Phosphopeptides
The major casein phosphopeptides (CPP) released by
trypsin that sequester calcium phosphate are Bos
S1
-casein
X-5P (f59-79) [1], Bos -casein X-4P (f1-25) [2], Bos
S2
-
casein X-4P (f46-70) [3] and Bos
S2
-casein X-4P (f1-21)
[4]. Using the three-letter code Pse to represent an O-phos-
phoseryl residue, the sequences of these peptides are:
[1] Gln
59
-Met-Glu-Ala-Glu-Pse-Ile-Pse-Pse-Pse-Glu-Glu-
Ile-Val-Pro-Asn-Pse-Val-Glu-Gln-Lys
79
S1
-casein(f59-79)
[2] Arg
1
-Glu-Leu-Glu-Glu-Leu-Asn-Val-Pro-Gly-Glu-Ile-
Val-Glu-Pse-Leu-Pse-Pse-Pse-Glu-Glu-Ser-Ile-Thr-
Arg
25
-casein(f1-25).
[3] Asn
46
-Ala-Asn-Glu-Glu-Glu-Tyr-Ser-Ile-Gly-Pse-Pse-
Pse-Glu-Glu-Pse-Ala-Glu-Val-Ala-Thr-Glu-Glu-Val-
Lys
70
S2
-casein(f46-70)
[4] Lys
1
-Asn-Thr-Met-Glu-His-Val-Pse-Pse-Pse-Glu-Glu-
Ser-Ile-Ile-Pse-Gln-Glu-Thr-Tyr-Lys
21
S2
-casein(f1-21)
These peptides are approximately 10% w/w of caseinate
and through their multiple phosphoseryl residues they se-
quester calcium and phosphate ions to form colloidal com-
plexes. Since the CPP are not associated with the unpalat-
ability [17] or allergenicity [18, 19] of the caseins and fur-
thermore have the potential for a specific anticariogenicity at
least ten times greater on a weight basis, their potential as a
food and toothpaste additive is considerably better than that
of the intact proteins. The CPP can be isolated from a tryptic
digest of caseinate using selective precipitation involving
calcium ions and ethanol [20]. The peptides produced by this
procedure have been comprehensively characterized [20].
The major peptides of the preparation are
S1
(59-79) [1] and
its deamidated forms, (1-25) [2], with smaller amounts of
S2
(46-70) [3], and
S2
(1-21) [4]. All the peptides contain
the sequence motif -Pse-Pse-Pse-Glu-Glu-. The individual
peptides of the preparation were identified by amino acid
composition and sequence analyses after purification to ho-
mogeneity by anion exchange FPLC and reversed-phase
HPLC [20]. Prior to sequence analysis the labile phos-
phoseryl residues were converted to S-ethyl cysteinyl resi-
dues by -elimination [20]. This CPP preparation has been
used as a 1% w/v CPP colloidal solution together with 60
mmol/L CaCl
2
and 36 mmol/L sodium phosphate pH 7.0 to
characterize its anticariogenic potential. The CPP in the
presence of 60 mmol/L CaCl
2
and 36 mmol/L sodium phos-
phate at pH 7.0 forms a random, cross-linked network re-
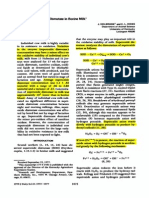
ferred to as open complexes (Fig. 1). This colloidal solu-
tion containing 1.0% w/v CPP and 60 mmol/L CaCl
2
and 36
mmol/L sodium phosphate at pH 7.0 has been tested in a
variety of caries models [9, 21, 22].
Casein Phosphopeptides in Oral Health Current Pharmaceutical Design, 2007, Vol. 13, No. 8 795
Fig. (1). A schematic representation of the open complexes of CPP
in which the peptides are cross-linked in a random network by cal-
cium ions and calcium phosphate ion clusters.
EFFICACY STUDIES
Anticariogenicity of CPP-CP in the Rat
The ability of open complex casein-phosphopeptide cal-
cium phosphate solutions at pH 7.0 (CPP-CP) to reduce car-
ies activity was investigated using specific-pathogen-free
rats orally infected with Streptococcus sobrinus 6715WT-13
[23]. CPP-CP solutions at pH 7.0, were applied to the ani-
mals teeth twice daily, and significantly reduced caries ac-
tivity with 1.0% w/v CPP containing 60 mmol/L CaCl
2
and
36 mmol/L sodium phosphate at pH 7.0 producing a 55%
reduction relative to the distilled water control. CPP at 0.5%
w/v containing 30 mmol/L CaCl
2
and 18 mmol/L sodium
phosphate pH 7.0 produced a reduction in caries activity
similar to that of the 500 ppm F
-
solution. The anticario-
genicity of CPP-CP and fluoride were additive as animals
receiving 0.5% CPP-CP plus positive control, 500 ppm F
-
had significantly lower caries activity than those animals
receiving either CPP-CP or fluoride alone.
Enamel Demineralization In Situ Study
The ability of a 1.0% w/v CPP solution containing 60
mmol/L CaCl
2
and 36 mmol/L sodium phosphate at pH 7.0
to prevent enamel demineralization has been studied in a
human in situ caries model [9, 22]. In this model two expo-
sures of the CPP-CP solution per day produced a 51 19%
reduction in enamel mineral loss relative to the control
enamel and increased plaque calcium and inorganic phos-
phate contents by 143% and 160% respectively. CPP was
also found in the treated plaque at a level of 2.4 0.7 mg/g.
The level of the CPP was determined by competitive ELISA
using an antibody that recognizes both
s1
(59-79) and (1-
25). Electron micrographs of immunocytochemically stained
sections of the plaque revealed localization of the peptide
predominantly on the surface of microorganisms but also in
the extracellular matrix.
In Vitro Remineralization of Enamel Lesions by CPP-CP
We have developed an in vitro model system [24] to
study remineralization of artificial lesions in human third
molars. Using this system the association between the activi-
ties of the various calcium phosphate species in various
CPP-CP solutions and the rate of enamel lesion remineraliza-
tion was studied. The1% CPP solution containing 60 mmol/L
calcium chloride and 36 mmol/L sodium phosphate at pH 7.0
produced the highest enamel remineralisation in vitro with
the higher pH solutions producing very poor remineralisa-
tion. The activity of the neutral ion species CaHPO
4
0
in the
various remineralizing solutions was found to be highly cor-
related with the rate of lesion remineralization [24]. At the
time it was speculated that free calcium and phosphate ions
eg. CaHPO
4
0
would diffuse into the enamel lesion and in-
crease the degree of saturation with respect to hydroxyapa-
tite. These results strongly suggested that free calcium and
phosphate ions, and not CPP-bound calcium phosphate, were
important for remineralisation activity and that the optimal
pH for stabilisation of free calcium and phosphate ions was
pH 7.0.
CHEMISTRY
Interaction of CPP with Calcium Phosphate
The CPP have a marked ability to stabilize calcium phos-
phate ions in solution [25]. Under alkaline conditions (eg.
pH 9.0) the CPP bind high amounts of calcium, phosphate
and hydroxide ions to produce specific nanocomplexes. Fur-
thermore, there is an interdependence of bound calcium to
bound phosphate indicating that a specific alkaline amor-
phous calcium phosphate phase is being bound by the CPP,
referred to as CPP-ACP.
The number of peptide chains participating in the forma-
tion of the CPP-ACP nanocomplexes was investigated by
using glutaraldehyde to cross-link the C-terminal lysyl resi-
dues and the N-terminal amines of
S1
(59-79) in complexes
with either calcium alone or in a CPP-ACP complex. Native
polyacrylamide gel electrophoresis was then performed on
the cross-linked peptides using 1 mm thick 20% gels and
stained overnight with Stains All [26]. A maximum of six
bands could be counted on the gel, suggesting that the com-
plexes contain a maximum of six peptide chains [27]. In con-
trol experiments, in which the peptide
S1
(59-79) was incu-
bated alone or in the presence of phosphate ions with glu-
taraldehyde, the highest molecular weight band formed cor-
responded to a dimer.
The ion activity products for the various calcium phos-
phate phases [hydroxyapatite (HA); octacalcium phosphate
(OCP); tricalcium phosphate (TCP); amorphous calcium
phosphate (ACP); and dicalcium phosphate dihydrate
(DCPD)] were determined from the free calcium and phos-
phate concentrations in these studies [25] using an iterative
computational procedure [28]. This iterative procedure cal-
culates the ion activity coefficients using the expanded De-
796 Current Pharmaceutical Design, 2007, Vol. 13, No. 8 Cross et al.
bye-Hckel equation and takes into account the ion pairs
CaHPO
4
0
, CaH
2
PO
4
+
, CaPO
4
-
and CaOH
+
, the dissociation of
H
3
PO
4
and H
2
O and the ionic strength. Analysis of the pH
dependence of the calcium and phosphate binding by
S1
(59-
79) over a range of pH values from 7.0 to 9.0 has shown that
the ion activity product of an alkaline ACP [Ca
3.0877
(PO
4
)
2
(OH)
0.1754
.xH
2
O] best correlated with the observed calcium
and phosphate binding behaviour [25]. Because hydroxyl
and fluoride ions have similar charges and sizes, fluoride
ions and hydroxyl ions readily replace each other in solid-
state phases, thus the presence of hydroxyl ions in the CPP-
ACP complex provides a rationale for the ready incorpora-
tion of fluoride into these complexes.
It was concluded that the stabilized nanocomplexes have
unit formulof [
s1
(59-79)(ACP)
7
]
6
and [(1-25)(ACP)
8
]
6
[25] from the stoichiometric and cross-linking analyses [27].
In alkaline supersaturated calcium phosphate solutions,
clusters of alkaline ACP, [Ca
3
(PO
4
)
2
/Ca
2
(PO
4
)OH] nuclei
form spontaneously. It is proposed that the CPP bind to the
forming alkaline ACP nanoclusters, producing a metastable
solution thereby preventing ACP growth to the critical size
required for nucleation and precipitation. The ACP appears
to be amorphous rather than simply microcrystalline as gen-
tle heating converts the ACP to an apatitic form of calcium
phosphate [25]. The heat-treated CPP-ACP has a broad-line,
X-ray powder diffraction spectrum characteristic of a mi-
crocrystalline solid. Interestingly, the calcium and phosphate
in the heat treated CPP-ACP is not as readily bioavailable as
that in the native CPP-ACP [25].
The interaction between phosphopeptides and hydroxya-
patite surfaces has been studied by computer simulation
techniques [29]. A model peptide (-Pse-Pse-Pse-Glu-Glu-)
corresponding to the calcium-binding motif of the caseins
was docked in random conformations against various crystal
faces of hydroxyapatite and allowed to relax in situ. The
lowest energy conformations of the peptide docked on each
of the a, b, and c faces of hydroxyapatite were then exam-
ined. The study concluded that the lowest energy conforma-
tions were characterized by having all the charged side-
chains in proximity to calcium ions in the crystal faces. The
study also concluded that the peptides were significantly
more strongly bound to the a and b faces than to the c face, a
result in agreement with the experimental observations using
other multiphosphorylated proteins [30]. The reduced affin-
ity of the peptide for the c face resulted from the inability of
the peptide to adopt a low-energy conformation that also
allowed the side-chains to interact with the calcium ions in
the crystal surface.
Structure of the Anticariogenic Casein Phosphopeptides
The conformations of the peptide moiety in the calcium
ion complexes of the CPP, and related peptides, have been
investigated using
1
H NMR techniques [31-39]. These stud-
ies have, in general, found significant secondary shifts of the
NH and H resonances indicative of a non-random coil con-
formation for the peptides. However, only those studies by
Cross, Huq and co-workers have identified medium-range
nOes that characterize the secondary structure of the peptides
in these complexes. In general, the structures are character-
ized by loops and turns although the structure of
S2
(1-21),
in its calcium ion complex, appears to contain a nascent -
helical region [40]. The study of (1-25) in complexes with
calcium, sodium, and ammonium ions and of the dephos-
phorylated peptide in the presence of sodium ions, suggests
that the peptide adopts a non-random coil conformation in
response to the binding of calcium ions [37].
Using 2D
1
H NMR, an analysis of
s1
(59-79) and (1-25)
in the presence of calcium ions indicated conformational
preferences [36, 37]. Two structured regions were identified
in
s1
(59-79): a -turn from Val
72
to Val
76
, and a loop-type
structure from Glu
61
to Pse
67
[36]. Four structured regions
were identified in (1-25): Arg
1
to Glu
4
form a loop, Val
8
to
Glu
11
, Pse
18
to Glu
20
, and Ser
22
to Thr
24
are in tight turns
[37]. The peptide conformation in region of the Pse-Pse-Pse-
Glu-Glu calcium-binding motif is different in these two pep-
tides. Molecular modeling of both
s1
(59-79) and (1-25)
using the constraints derived from NMR spectroscopy have
indicated that the peptides adopt conformations that allow
the glutamyl and phosphoseryl side chains to interact collec-
tively with calcium ions [25, 36].
The biological significance of the structural motifs identi-
fied in (1-25) has been examined by Ferraretto et al. [41,
42] who studied the uptake of calcium ions by HT-29 tumour
cells in the presence of (1-25) and chimeric peptides based
on the structural motifs identified by NMR techniques [37].
Calcium uptake by the HT-29 cells was shown to require the
presence of the N-terminal region of the (1-25) peptide and
the phosphorylated calcium-ion binding motif. The synthetic
peptide corresponding to the calcium-ion binding motif was
observed to be ineffective in inducing calcium ion uptake
[41] even though such a peptide is expected to bind almost
as much calcium phosphate as the (1-25) peptide [25]. A
peptide in which residues 1-4 of (1-25) were swapped with
residues 8-11 of (1-25) was ineffective at inducing calcium
ion uptake by HT-29 cells [41]. In our model of the calcium
phosphate complex of (1-25) [25, 27], residues 8-11 of (1-
25) were shown to be involved in the formation of a hydro-
phobic patch on the surface of the nanocomplex. The hydro-
phobic patch is possibly the point at which the CPP-ACP
interacts with the hydrophobic cell membrane in order to
accomplish their biological role as calcium phosphate deliv-
ery vehicles.
The
1
H NMR solution spectra of (1-25) complexed with
alkaline amorphous calcium phosphate [(1-25)-ACP] have
recently been reported [27]. The spectra displayed sharp
lines, with
3
J
NH
coupling constants readily measurable in the
amide region (in contrast to the broader resonances observed
with the (1-25)-calcium complex). The signals were intense
with no evidence for a broadened component underlying the
spectrum as would be expected for aggregated species. We
have recorded Double Quantum Filtered Correlation Spec-
troscopy (DQF-COSY), Total Spectroscopy (TOCSY) and
Nuclear Overhauser Enhanced Spectroscopy (NOESY) spec-
tra of the (1-25)-ACP complex in 90% H
2
O/ 10% D
2
O so-
lution at a temperature of 25C. We have been able to com-
plete a sequential assignment of the spectra, and chemical
shifts of resonances show significant shifts away from ran-
dom coil values and differences compared with the shifts of
the (1-25)-calcium complex [36]. Using the stored Longi-
tudinal Encode Decode (sLED) technique [43] we have de-
Casein Phosphopeptides in Oral Health Current Pharmaceutical Design, 2007, Vol. 13, No. 8 797
termined the translational diffusion coefficient for (1-25)
ACP as a function of pH at a sample concentration of 1 mM
[27]. The Stoke's-Einstein equation was used to estimate the
hydrodynamic radii of the particles giving rise to the ob-
served
1
H NMR spectra of (1-25) ACP. The decay of the
echo amplitude due to translational diffusion was single-
exponential. Using the rate of decay of the HDO peak and a
hydrodynamic radius of 1.40 for the water molecule, we
have estimated hydrodynamic radii of 1.526 0.044 nm at
pH 6.0 increasing to 1.923 0.082 nm at pH 9.0 for the (1-
25)-ACP complex. These particle dimensions are consistent
with the predicted size of the [(1-25)(ACP)
8
]
6
nanoclusters
using molecular modeling. Using the sLED technique [43],
we have recently characterized
s1
-casein(f59-79)(ACFP)
nanocomplexes and demonstrated that they are slightly
larger than the -casein(f1-25)(ACP) complexes suggesting
that the incorporation of fluoride ions enhances the forma-
tion and the stabilization of the complexes [44].
The Closed Complex Structure of CPP-ACP
It has been unexpectedly difficult to determine the di-
mensions of the CPP-ACP nanocomplex. After exhaustive
deproteination of casein micelles through the use of hydra-
zine solutions, McGann et al. [45] were able to image the
resulting calcium phosphate particles using electron micros-
copy. They reported that The Ca phosphate exhibits a
very fine and uniform granularity when examined by elec-
tron microscopy; the small particles have a true diameter of
approximately 2.5 nm.
A structure of (1-25) with an acidic calcium phosphate
has been proposed by Holt et al. based on small-angle X-ray
scattering and neutron diffraction studies [46] performed on
samples having 10 mg ml
-1
of (1-25)-casein peptide. The
model consists of an inner sphere of acidic calcium phos-
phate (as CaHPO
4
.2H
2
O) with a radius of 2.30 0.05 nm
surrounded by a tightly packed shell consisting of 49 4
peptide chains with an outer radius of 4.04 0.15 nm. Inter-
estingly, the authors reported scattering with a subsidiary
maximum at about Q 1.6 nm
-1
suggesting the presence of
structure at a finer scale than explained by their model. The
authors suggest that these results were consistent with those
of McGann et al. [45], but McGann et al. reported a diameter
of 2.5 nm rather than a radius. Secondly, the thickness of the
peptide coat (1.74 0.20 nm) is a substantial portion of the
length of a fully extended (1-25) peptide chain. Assuming
that the calcium-binding motif, -Pse-Pse-Pse-Glu-Glu-,
interacts with the acidic calcium phosphate core, then the
low-energy conformation of the complex would be charac-
terized by many of the peptides charged residues not inter-
acting with the calcium phosphate core. Not only is this dif-
ficult to understand from the point of view of electrostatics,
but the model does not provide an explanation of why pep-
tide length is a determinant of the amount of calcium phos-
phate bound by analogs of the CPP [25].
A model of (1-25) complexed with alkaline amorphous
calcium phosphate has recently been proposed [25, 27].
The model is referred to as a closed complex structure
(Fig. 2) and is based on several lines of experimental evi-
dence including chemical cross-linking of peptides in the
S1
(59-79)-ACP complex, electron microscopy and X-ray
diffraction analysis. The (1-25)-ACP complex was shown
to have a hydrodynamic radius of 1.526 0.044 nm at
pH 6.0 increasing to 1.923 0.082 nm at pH 9.0. This model
shows all the charged residues having a significant interac-
tion with the alkaline calcium phosphate core particle, thus
rationalizing the observation [25] that shorter CPP analogues
bind less calcium phosphate than the full-length CPP. Re-
cently a method for routine preparation of the closed com-
plex CPP-ACP has been developed involving careful titra-
tion of calcium ions, phosphate ions and hydroxide ions at
pH 9.0 to produce a high molar ratio of Ca and phosphate
ions to CPP [47]. This results in the loading of the CPP with
calcium, phosphate and hydroxide ions in closed complexes
that are very stable and can be purified by filtration and
dried. This alkaline, stable and highly soluble CPP-ACP has
been trademarked as Recaldent
TM
and has now been com-
mercialised in sugar-free gum and mints and in dental pro-
fessional products (Tooth Mousse
TM
).
Fig. (2). The closed complex structure of the CPP-ACP nanocom-
plex.
Clinical Studies with CPP-ACP
CPP-ACP closed complexes (Recaldent
TM
) have supe-
rior anticariogenic potential to CPP-CP open complexes as
the closed complexes carry more calcium and phosphate ions
as well as hydroxide ions which help prevent enamel demin-
eralisation and promote enamel remineralisation. In fact, the
ability of CPP-ACP added to sugar-free chewing gum to
remineralise enamel subsurface lesions has been demon-
strated in several randomised, double-blind, in situ clinical
trials [48-50]. The subjects of the trials were healthy adults
ranging in age from 22 to 44 years and exhibited normal
salivary flow rates [48-50]. The sugar-free gums were
chewed for either 20 min, four times per day or for five min,
seven times per day. After 14 days microradiographic analy-
ses demonstrated that gum containing 18.8 mg and 56.4 mg
of CPP-ACP chewed for 20 min four times per day increased
enamel subsurface remineralisation by 101% and 151% re-
spectively relative to the control sugar-free gum [48]. In an-
798 Current Pharmaceutical Design, 2007, Vol. 13, No. 8 Cross et al.
other in situ clinical study CPP-ACP was shown to be supe-
rior in remineralisation of subsurface enamel lesions to other
forms of calcium phosphate [49]. In a further in situ clinical
study CPP-ACP remineralised enamel was shown to be more
acid resistant than normal tooth enamel, which is a calcium-
deficient carbonated apatite [50]. These results suggest that
CPP-ACP remineralised enamel should be relatively more
resistant to caries than normal tooth enamel. A dental profes-
sional crme (Tooth Mousse
TM
) containing 10% w/w CPP-
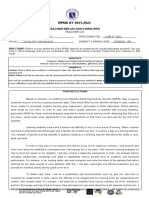
ACP has been used clinically for the non-invasive treatment
of mild to moderate fluorotic (hypomineralised) tooth
enamel (Fig. 3). The crme was applied in the dental surgery
and then by the patient nightly before retiring for six weeks
[51].
Fig. (3). Treatment of mild to moderate fluorosis (hypomineralized
enamel) with Tooth Mousse
TM
containing CPP-ACP. A) Before
treatment and B) After 6 weeks treatment.
Interaction of CPP-ACP with Fluoride
Fluoride ion in the presence of CPP-ACP incorporates
into the amorphous calcium phosphate phase to produce a
novel amorphous calcium fluoride phosphate phase. Analy-
sis of the crystallinity of the calcium fluoride phosphate
phase stabilized by the CPP using powder X-ray diffraction
and TEM-EDAX confirmed that the phase was amorphous
[44]. A detailed stoichiometric analysis of the calcium,
phosphate and fluoride ions bound by the CPP at different
pH values suggested that two phases were stabilized by the
CPP, ACP [Ca
3
(PO
4
)
2
.xH
2
O] and ACFP [Ca
2
FPO
4
.xH
2
O].
The ratio of the two phases stabilized depended upon the
molar ratio of the calcium, phosphate and fluoride ions
added and the solution pH. A 1:1 ACP:ACFP molar ratio of
the two phases [i.e. Ca
3
(PO
4
)
2
xH
2
O : Ca
2
FPO
4
xH
2
O] pro-
duces a stoichiometry of Ca
5
(PO
4
)
3
F, the same as that of
fluorapatite. Typically at neutral pH the molar ratio is 2:1
ACP:ACFP producing a stoichiometry of Ca
8
(PO
4
)
5
F
x
H
2
O.
The identification of the novel amorphous calcium fluoride
phosphate (ACFP) phase has led to the speculation that the
formation of this phase is responsible for the observed addi-
tive anticariogenic effect of CPP-ACP and F. The anticario-
genic mechanism of fluoride is now proposed to be the local-
ization of the fluoride ion at the tooth surface, particularly in
plaque in the presence of calcium and phosphate ions [6].
This localization increases the degree of saturation with re-
spect to fluorapatite (FA) thus promoting remineralization of
enamel with FA [6]. It is clear that for the formation of FA
[Ca
10
(PO
4
)
6
F
2
], calcium and phosphate ions must be co-
localized at the tooth surface with the fluoride ion. The addi-
tive anticariogenic effect of CPP-ACP and F [21] may there-
fore be attributable to the localization of ACFP at the tooth
surface by the CPP which in effect would co-localize Ca, Pi
and F.
We have recently demonstrated the remineralization of
fluorotic (hypomineralized) lesions of enamel with 2% CPP-
ACFP at pH 7.0 by up to 80% in an in vitro study. The CPP-
ACFP prevented the rapid precipitation of fluorapatite in the
surface layer of the hypomineralized lesion by slowly releas-
ing the calcium, phosphate and fluoride ions. The localiza-
tion of high amounts of CPP-ACFP at the tooth surface and
the slow release of the calcium, phosphate and fluoride ions
results in remineralization deep into the lesion. However, for
the remineralized phase to be of benefit in preventing future
caries development at that site, it is desirable that the depos-
ited mineral is fluorapatite (i.e. Ca:P:F of 5:3:1).
CLINICAL APPLICATIONS
A recent clinical trial has demonstrated that the tooth
enamel mineral formed by CPP-ACP is relatively resistant to
acid challenge. This study compared a sugar-free gum con-
taining 18.8 mg CPP-ACP with a sugar-free gum not con-
taining CPP-ACP [50]. Subjects wore removable palatal ap-
pliances with insets of human enamel containing demineral-
ized subsurface lesions and chewed the gum for 20 minutes
four times per day for a total of 14 days. After each treat-
ment the enamel slabs were removed from the appliances
and half of each lesion was challenged with acid in vitro for
8 or 16 hours. The strength and acid resistance of the remin-
eralized enamel depends on the nature of the calcium phos-
phate phase and its crystallinity. The lesions that were acid
challenged after in situ remineralisation by the CPP-ACP-
containing gum, showed demineralization beneath the
remineralized zone, indicating that the remineralized mineral
was more resistant to subsequent acid challenge. The results
showed that sugar-free gum containing CPP-ACP is superior
to an equivalent gum not containing CPP-ACP in reminerali-
zation of enamel subsurface lesions in situ with mineral that
was more resistant to subsequent acid challenge.
Dental caries is a chronic disease that requires prolonged
therapy to repair enamel. With any oral therapeutic agent
applied periodically, long term activity or high substantiv-
ity is a desirable property. A recent study of CPP-ACP re-
tention in plaque [49] showed that significant levels of CPP
Casein Phosphopeptides in Oral Health Current Pharmaceutical Design, 2007, Vol. 13, No. 8 799
could be detected in supragingival plaque up to three hours
after chewing a Recaldent pellet gum containing 9.5 mg of
CPP-ACP per piece. Interactions between salivary proteins
that form the dental pellicle and CPP have been demon-
strated by Ung et al. [52]. These interactions would be ex-
pected to give the CPP-ACP high oral substantivity even in
the absence of significant dental plaque.
The consumption of highly acidic sports drinks and soft
drinks can lead to tooth erosion. A recent study demonstrated
that at concentrations of 0.09% w/v or greater in a typical
sports drink CPP-ACP was effective in preventing tooth ero-
sion in vitro [53]. As part of this study, a taste panel was set
up to investigate whether the addition of CPP-ACP had any
deleterious taste effects in this application. The authors re-
ported that tasters in the test panel could not distinquish be-
tween the sports drink and the sports drink containing
0.125% w/w of CPP-ACP.
A recent novel clinical application of the CPP-ACP tech-
nology is as a component of a self-curing, glass ionomer
cement (GIC) [54]. Because GICs are water-based and tooth-
coloured, they are used as an adhesive material in dental
restorations, a usage that demands high bond strength and
compressive strength. By incorporating 1.56% w/w of CPP-
ACP into the GIC a material was produced that when cured
had significantly greater microtensile bond strength and
compressive strength. The curing time of the modified-GIC
increased by 40 seconds compared with the control, but was
still acceptable for clinical application. A major problem
with any dental restorative is the occurrence of micro-
leakage around the edges of the restoration, which can result
in caries lesions underneath the restoration. The CPP-ACP
incorporated into the GIC released calcium, phosphate, and
fluoride into the surrounding medium under acidic and neu-
tral conditions. The modified GIC was observed to provide
significant protection to the adjacent dentin from deminerali-
zation during acid challenge in vitro.
CONCLUSION
The potential anticariogenicity of the CPP-ACP has been
demonstrated in various caries models and short-term clini-
cal trials. The material appears to be very safe for human use
in oral care products, dental professional products and food-
stuffs. In animal and in vitro experiments the CPP-ACP and
fluoride have been shown to have an additive effect in reduc-
ing caries experience and remineralizing enamel subsurface
lesions. The fluoride ion incorporates into a novel amor-
phous calcium fluoride phosphate phase (ACFP) which is
stabilized by the CPP and localized at the tooth surface, sug-
gesting that the CPP may be an excellent delivery vehicle to
co-localize Ca, F, and phosphate ions at the tooth surface in
a slow-release amorphous form producing superior anticaries
efficacy.
REFERENCES
References 55-57 are related articles recently published in
Current Pharmaceutical Design.
[1] Armfield J , Roberts-Thomson K, Spencer A. Australia's Health
2000: the seventh biennial health report of the Australian Institute
of Health & Welfare. Canberra 2000.
[2] Loesche W. Role of Streptococcus mutans in human dental decay.
Microbiol Revs 1986; 50: 353-80.
[3] Crowley S, Antioch K, Crater R, Conway L, Matheis C. The eco-
nomic burden of diet-related disease in Australia. Centre for Health
Program Evaluation and the Aust Inst Health 1992.
[4] Spencer AJ , Wright FAC, Brown LM, Brown LP. Changing caries
experience and risk factors in five- and six-year-old Melbourne
children. Aust Dent J 1986; 34: 160-5.
[5] Liljemark WF, Bloomquist C. Human oral microbial ecology and
dental caries and periodontal diseases. Crit Rev Oral Biol Med
1996; 7: 180-98.
[6] Thylstrup A, Fejerskov O. Textbook of cariology. In: Munksgaard;
1986; 196-201.
[7] Chang HS, Walsh LJ , Freer TJ . Enamel demineralization during
orthodontic treatment. Aetiology and prevention. Aust Dent J 1997;
42: 322-7.
[8] Reynolds EC, Black CL, Cai F, Cross KJ , Eakins D, Huq NL, et al.
Advances in enamel remineralization: casein phosphopeptide-
amorphous calcium phosphate. J Clin Dent 1999; 10: 86-8.
[9] Reynolds EC. Anticariogenic complexes of amorphous calcium
phosphate stabilized by casein phosphopeptides: a review. Spec
Care Dentist 1998; 18: 8-16.
[10] Reynolds E, J ohnson I. Effect of milk on caries incidence and
bacterial composition of dental plaque in the rat. Arch Oral Biol
1981; 26: 445-51.
[11] Reynolds E, del Rio A. Effects of casein and whey-protein solu-
tions on caries experience and feeding patterns of the rat. Arch Oral
Biol 1984; 29: 927-33.
[12] Reynolds E, Black C. Confectionery composition and rat caries.
Caries Res 1987; 21: 238-45.
[13] Reynolds E, Black C. The reduction of chocolate's cariogenicity by
supplementation with sodium caseinate. Caries Res 1987; 21: 445-
51.
[14] Reynolds E. The prevention of sub-surface demineralization of
bovine enamel and change in plaque composition by casein in an
intra-oral model. J Dent Res 1987; 26: 1120-7.
[15] Reynolds E, Black C. Cariogenicity of a confection supplemented
with sodium caseinate at a palatable level. Caries Res 1989; 23:
368-70.
[16] Reeves R, Latour N. Calcium phosphate sequestering phosphopep-
tide from casein. Science 1958; 128: 472.
[17] Swaisgood HE. Chemistry of Milk Protein. In: Fox PF Ed, Devel-
opments In dairy chemistry - 1. London: Applied Science Publish-
ers 1982; 1-43.
[18] Ametani A, Kaminogawa S, Shimizu M, Yamauchi K. Rapid
screening of antigenically reactive fragments of s1-casein using
HPLC and ELISA. J Biochem (Tokyo, J apan) 1987; 102: 421-5.
[19] Park O-J , Allen J C. Antigenicity of casein phosphopeptides pre-
pared with immobilized glutamic acid-specific endopeptidase or
trypsin. Nutr Res 2000; 20: 359-70.
[20] Reynolds EC, Riley PF, Adamson NJ . A selective precipitation
procedure for the purification of multiple-phosphoseryl containing
peptides and their identification. Anal Biochem 1994; 217: 277-84.
[21] Reynolds EC, Cain CJ , Webber FL, Black CL, Riley PF, J ohnson
IH, et al. Anticariogenicity of calcium phosphate complexes of
tryptic casein phosphopeptides in the rat. J Dent Res 1995; 74:
1272-9.
[22] Reynolds E. Anticariogenic phosphopeptides. US Patent No
5015628. 1991.
[23] Reynolds EC, Cain CJ , Webber FL, Black CL, Riley PF, J ohnson
IH, et al. Anticariogenicity of calcium phosphate complexes of
tryptic casein phosphopeptides in the rat. J Dent Res 1995; 74:
1272-9.
[24] Reynolds EC. Remineralization of enamel subsurface lesions by
casein phosphopeptide-stabilized calcium phosphate solutions. J
Dent Res 1997; 76: 1587-95.
[25] Cross KJ , Huq NL, Palamara J , Perich J W, Reynolds EC. Physico-
chemical characterization of casein phosphopeptide-amorphous
calcium phosphate nanocomplexes. J Biol Chem 2005; 280: 15362-
9.
[26] Green MR, Pastewska J V, Peacock AC. Differential staining of
phosphoproteins on polyacrylamide gels with a cationic carbo-
cyanine dye. Anal Biochem 1973; 56: 43-51.
[27] Cross KJ , Huq NL, Reynolds EC. Anticariogenic peptides. In:
Mine Y, Shahidi F Eds, Nutraceutical proteins and peptides in
health and disease: CRC Press 2005; 335-51.
[28] Marsh ME. Binding of calcium and phosphate ions to dentin phos-
phophoryn. Biochemistry 1989; 28: 346-52.
800 Current Pharmaceutical Design, 2007, Vol. 13, No. 8 Cross et al.
[29] Huq NL, Cross KJ , Reynolds EC. Molecular modelling of a mul-
tiphosphorylated sequence motif bound to hydroxyapatite surfaces.
J Mol Model 2000; 6: 35-47.
[30] Fujisawa R, Kuboki Y. Preferential adsorption of dentin and bone
acidic proteins on the (100) face of hydroxyapatite crystals. Bio-
chim Biophys Acta 1991; 1075: 56-60.
[31] Tsuda S, Niki R, Kuwata T, Tanaka I, Hikichi K. Proton NMR
study of casein phosphopeptide (1-25): Assignment and conforma-
tion. Magn Reson Chem 1991; 28: 1097-102.
[32] Wahlgren NM, Dejmek P, Drakenberg T. Secondary structures in
the -casein peptide 1-42. J Dairy Sci 1993; 1-9.
[33] Wahlgren NM, Leonil J , Dejmek P, Drakenberg T. Calcium in-
duced structural changes in the -casein peptide 1-25. A two-
dimensional nuclear magnetic resonance study. J Dairy Sci 1993:
1-9.
[34] Wahlgren NM, Leonil J , Dejmek P, Drakenberg T. Two-
dimensional nuclear magnetic resonance study of the -casein pep-
tide 1-25: resonance assignments and secondary structure. Biochim
Biophys Acta 1993; 1202: 121-8.
[35] Wahlgren NM, Dejmek P, Drakenberg T. Secondary structures in
the -casein peptide 1-42: A two dimensional nuclear magnetic
resonance study. J Dairy Res 1994; 61: 495-506.
[36] Huq NL, Cross KJ , Reynolds EC. A
1
H-NMR study of the casein
phosphopeptide S1-casein(59-79). Biochim Biophys Acta 1995;
1247: 201-8.
[37] Cross KJ , Huq NL, Bicknell W, Reynolds EC. Cation-dependent
structural features of -casein-(1-25). BiochemJ 2001; 356: 277-
86.
[38] Huq NL, Cross KJ , Reynolds EC. Nascent helix in the multiphos-
phorylated peptide S2-casein(2-20). J Pept Sci 2003; 9: 386-92.
[39] Huq NL, Cross KJ , Reynolds EC. Molecular modelling of the
multiphosphorylated casein phosphopeptide S1-casein(59-79)
based on NMR constraints. J Dairy Res 2004; 71: 28-32.
[40] Huq NL, Cross KJ , Reynolds EC. A
1
H NMR study of the casein
phosphopeptide S2-casein(1-21). J Dent Res 1995; 74: 579.
[41] Ferraretto A, Gravaghi C, Fiorilli A, Tettamanti G. Casein-derived
bioactive phosphopeptides: role of phosphorylation and primary
structure in promoting calcium uptake by HT-29 tumor cells. FEBS
Lett 2003; 551: 92-8.
[42] Ferraretto A, Gravaghi C, Fiorilli A, Tettamanti G. Casein-derived
bioactive phosphopeptides: role of phosphorylation and primary
structure in promoting calcium uptake by HT-29 tumor cells. FEBS
Lett 2003; 553: 218.
[43] Altieri A, Hinton D, Byrd R. Association of biomolecular systems
via pulsed field gradient NMR self-diffusion measurements. J Am
Chem Soc 1995; 117: 7566-7.
[44] Cross KJ , Huq NL, Stanton DP, Sum M, Reynolds EC. NMR stud-
ies of a novel calcium, phosphate and fluoride delivery vehicle-S1-
casein(59-79) by stabilized amorphous calcium fluoride phosphate
nanocomplexes. Biomaterials 2004; 25: 5061-9.
[45] McGann TC, Kearney RD, Buchheim W, Posner AS, Betts F,
Blumenthal NC. Amorphous calcium phosphate in casein micelles
of bovine milk. Calcif Tissue Int 1983; 35: 821-33.
[46] Holt C, Timmins PA, Errington N, Leaver J . A core-shell model of
calcium phosphate nanoclusters stabilized by -casein phosphopep-
tides, derived from sedimentation equilibrium and small-angle x-
ray and neutron-scattering measurements. Eur J Biochem 1998;
252: 73-8.
[47] Reynolds E. Calcium phosphopeptide complexes. US Patent
6780844. 1997.
[48] Shen P, Cai F, Nowicki A, Vincent J , Reynolds EC. Remineraliza-
tion of enamel subsurface lesions by sugar-free chewing gumcon-
taining casein phosphopeptide-amorphous calcium phosphate. J
Dent Res 2001; 80: 2066-70.
[49] Reynolds EC, Cai F, Shen P, Walker GD. Retention in plaque and
remineralization of enamel lesions by various forms of calcium in a
mouthrinse or sugar-free chewing gum. J Dent Res 2003; 82: 206-
11.
[50] Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC.
Acid resistance of enamel subsurface lesions remineralized by a
sugar-free chewing gum containing casein phosphopeptide-
amorphous calcium phosphate. Caries Res 2004; 38: 551-6.
[51] Reynolds EC, Walsh L. Additional aids to remineralisation of tooth
strucuture. In: Mount G, Hume W Eds, Preservation and restoration
of tooth structure. 2nd ed. Brisbane: Knoweldge Books and Soft-
ware 2005; 109-16.
[52] Ung M, Huq NL, Cross KJ , Reynolds EC. Characterisation of the
binding of anticariogenic casein phosphopeptide complexes to the
enamel pellicle proteins. Aust Dent J 2004; 49: S19-20.
[53] Ramalingam L, Messer LB, Reynolds EC. Adding casein phos-
phopeptide-amorphous calcium phosphate to sports drinks to
eliminate in vitro erosion. Pediatr Dent 2005; 27: 61-7.
[54] Mazzaoui SA, Burrow MF, Tyas MJ , Dashper SG, Eakins D, Rey-
nolds EC. Incorporation of casein phosphopeptide-amorphous cal-
cium phosphate into a glass-ionomer cement. J Dent Res 2003; 82:
914-8.
[55] Salvi GE, Lang NP. The effects of non-steroidal anti-inflammatory
drugs (selective and non-selective) on the treatment of periodontal
diseases. Curr Pharm Des 2005; 11(14): 1757-69.
[56] Wycoff KL. Secretory IgA antibodies from plants. Curr Pharm Des
2005; 11(19): 2429-37.
[57] Yalcin AS. Emerging therapeutic potential of whey proteins and
peptides. Curr Pharm Des 2006; 12(13): 1637-43.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Root Canal TreatmentDocument7 pagesRoot Canal TreatmentHilda LiemPas encore d'évaluation
- 2 PB PDFDocument8 pages2 PB PDFPascalis Adhi KurniawanPas encore d'évaluation
- 230 2702 1 PBDocument5 pages230 2702 1 PBSTEFFI MIFTAPas encore d'évaluation
- Esprit de Corps and Quality Making The Case ForDocument5 pagesEsprit de Corps and Quality Making The Case ForPascalis Adhi KurniawanPas encore d'évaluation
- Critical AppraisalDocument6 pagesCritical AppraisalAmanda Diah MaharaniPas encore d'évaluation
- The Relationship of Hospital CEO CharacteristicsDocument12 pagesThe Relationship of Hospital CEO CharacteristicsPascalis Adhi KurniawanPas encore d'évaluation
- Esprit de Corps and Quality Making The Case ForDocument5 pagesEsprit de Corps and Quality Making The Case ForPascalis Adhi KurniawanPas encore d'évaluation
- Analysing qualitative health dataDocument22 pagesAnalysing qualitative health dataPascalis Adhi KurniawanPas encore d'évaluation
- Exploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsDocument16 pagesExploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsPascalis Adhi KurniawanPas encore d'évaluation
- A Future-Focused Approach ToDocument3 pagesA Future-Focused Approach ToPascalis Adhi KurniawanPas encore d'évaluation
- Sustained Hospital Performance On HospitalDocument14 pagesSustained Hospital Performance On HospitalPascalis Adhi KurniawanPas encore d'évaluation
- Hospital Value-Based Purchasing PerformanceDocument18 pagesHospital Value-Based Purchasing PerformancePascalis Adhi KurniawanPas encore d'évaluation
- Exploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsDocument16 pagesExploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsPascalis Adhi KurniawanPas encore d'évaluation
- A Future-Focused Approach ToDocument3 pagesA Future-Focused Approach ToPascalis Adhi KurniawanPas encore d'évaluation
- Diagnosis and Treatment of Gummy SmileDocument6 pagesDiagnosis and Treatment of Gummy SmilePascalis Adhi KurniawanPas encore d'évaluation
- Gummy Smile Correction Case Report 1000103 PDFDocument3 pagesGummy Smile Correction Case Report 1000103 PDFPascalis Adhi KurniawanPas encore d'évaluation
- Antioxidants ActivityDocument15 pagesAntioxidants ActivityPascalis Adhi KurniawanPas encore d'évaluation
- Exploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsDocument16 pagesExploring The Divide Between Output and Outcome Measures in Health Care Conceptual and Empirical InsightsPascalis Adhi KurniawanPas encore d'évaluation
- Variation of Superoxide Dismutase in Bovine MilkDocument6 pagesVariation of Superoxide Dismutase in Bovine MilkPascalis Adhi KurniawanPas encore d'évaluation
- Antioxidative Status of Saliva Before and After PDFDocument6 pagesAntioxidative Status of Saliva Before and After PDFPascalis Adhi KurniawanPas encore d'évaluation
- 62113463Document9 pages62113463Pascalis Adhi KurniawanPas encore d'évaluation
- Antioxidative Status of Saliva Before and After PDFDocument6 pagesAntioxidative Status of Saliva Before and After PDFPascalis Adhi KurniawanPas encore d'évaluation
- Konser JossDocument7 pagesKonser JossPascalis Adhi KurniawanPas encore d'évaluation
- Superoxide Dismutase Enzyme and Thiol Antioxidants in GingivalDocument8 pagesSuperoxide Dismutase Enzyme and Thiol Antioxidants in GingivalPascalis Adhi KurniawanPas encore d'évaluation
- Takushige Retreat J LSTRDocument5 pagesTakushige Retreat J LSTRPascalis Adhi KurniawanPas encore d'évaluation
- Coll 10 03Document7 pagesColl 10 03Pascalis Adhi KurniawanPas encore d'évaluation
- 25 713 PDFDocument6 pages25 713 PDFPascalis Adhi KurniawanPas encore d'évaluation
- Konser JossDocument7 pagesKonser JossPascalis Adhi KurniawanPas encore d'évaluation
- Antibiotics in Endodntics FINALDocument91 pagesAntibiotics in Endodntics FINALPascalis Adhi KurniawanPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Comparison of the Fully Automated Urinalysis Analyzers UX-2000 and Cobas 6500Document10 pagesComparison of the Fully Automated Urinalysis Analyzers UX-2000 and Cobas 6500Sethulakshmi PharmacistPas encore d'évaluation
- Development of The Planet EarthDocument14 pagesDevelopment of The Planet EarthHana CpnplnPas encore d'évaluation
- 2 Part 1Document99 pages2 Part 1m_luchianPas encore d'évaluation
- 01 MDCAT SOS Regular Session (5th June-2023) With LR..Document5 pages01 MDCAT SOS Regular Session (5th June-2023) With LR..bakhtawarsrkPas encore d'évaluation
- Population Size, Density, & Dispersal: Demography: Describing Populations and How They ChangeDocument4 pagesPopulation Size, Density, & Dispersal: Demography: Describing Populations and How They ChangeAllan Jr. Agao-AgaoPas encore d'évaluation
- Summary of Qualitative Tests (Pharmacognosy)Document8 pagesSummary of Qualitative Tests (Pharmacognosy)kidsaintfinePas encore d'évaluation
- Cell Membrane: A Selective BarrierDocument23 pagesCell Membrane: A Selective BarrierHama JamalPas encore d'évaluation
- JCM 08 00217 v3Document23 pagesJCM 08 00217 v3Sumit BediPas encore d'évaluation
- Ssac 2104Document100 pagesSsac 2104Amrutha amrPas encore d'évaluation
- Introspect For DealersDocument13 pagesIntrospect For DealersOBERON-INTROSPECT-BIOSPECTPas encore d'évaluation
- Plant Transport - IGCSE Biology Notes (2020)Document6 pagesPlant Transport - IGCSE Biology Notes (2020)Zhi En LeePas encore d'évaluation
- Dna Finger PrintingDocument23 pagesDna Finger PrintingSanjay KumarPas encore d'évaluation
- Regular Evaluation Test I Maths+Sc IXDocument7 pagesRegular Evaluation Test I Maths+Sc IXB.L. Indo Anglian Public School, Aurngabad, BiharPas encore d'évaluation
- Pemphigus Subtypes Clinical Features Diagnosis andDocument23 pagesPemphigus Subtypes Clinical Features Diagnosis andAnonymous bdFllrgorzPas encore d'évaluation
- Cooling Tower Operation - 030129Document8 pagesCooling Tower Operation - 030129Sekar CmPas encore d'évaluation
- Human Dimensions of Late Pleistocene/Holocene Arid Events in Southern South AmericaDocument13 pagesHuman Dimensions of Late Pleistocene/Holocene Arid Events in Southern South AmericaKaren RochaPas encore d'évaluation
- Student Exploration: Building DNADocument4 pagesStudent Exploration: Building DNAMia Smith100% (1)
- A Review of The Environmental Fate, Effects, and Exposures of Bisphenol A PDFDocument25 pagesA Review of The Environmental Fate, Effects, and Exposures of Bisphenol A PDFTiago TorresPas encore d'évaluation
- Effects of Different Fermentation Temperatures On Metabolites of KimchiDocument7 pagesEffects of Different Fermentation Temperatures On Metabolites of KimchiAngela ValdiviesoPas encore d'évaluation
- Reproductive Biology and Phylogeny of Birds PDFDocument624 pagesReproductive Biology and Phylogeny of Birds PDFFabricio GZPas encore d'évaluation
- Agilent ASMS 2019 ThP762 PosterDocument4 pagesAgilent ASMS 2019 ThP762 PostersppPas encore d'évaluation
- Natamycin Story - What You Need to KnowDocument13 pagesNatamycin Story - What You Need to KnowCharles MardiniPas encore d'évaluation
- COT TRF Science G8 - Food ChainDocument8 pagesCOT TRF Science G8 - Food ChainRAMIR BECOYPas encore d'évaluation
- Biology of Implant OsseointegrationDocument11 pagesBiology of Implant OsseointegrationAmIrPas encore d'évaluation
- Artigo Sobre Nutrigenômica e Nutrigenética PDFDocument18 pagesArtigo Sobre Nutrigenômica e Nutrigenética PDFDiogo JuniorPas encore d'évaluation
- MYCOVIRODocument11 pagesMYCOVIROPau SorianoPas encore d'évaluation
- C Specialized GeneralBiology1 Sem1 Clas3 CellsinPlantand-AnimalTissue v2Document14 pagesC Specialized GeneralBiology1 Sem1 Clas3 CellsinPlantand-AnimalTissue v2ダギア メイ アニアPas encore d'évaluation
- Everyday Sports Injuries The Essential Step-By-Step Guide To Prevention, Diagnosis, and TreatmentDocument274 pagesEveryday Sports Injuries The Essential Step-By-Step Guide To Prevention, Diagnosis, and TreatmentAnonymous f6goFflg3T100% (10)
- Warlock of The Magus World - Arc 2Document808 pagesWarlock of The Magus World - Arc 2Hitsuin MoviesPas encore d'évaluation
- DNA TimelineDocument2 pagesDNA TimelineMinaMilićPas encore d'évaluation