Académique Documents
Professionnel Documents
Culture Documents
Acog 1997
Transféré par
SAKAI69Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Acog 1997
Transféré par
SAKAI69Droits d'auteur :
Formats disponibles
0
P u r p o s e
~ O b j e c t i v e s
M e t h o d s
I n t e r n a t i o n a l 4 o u r n a l o l
GYNECOLOGY
& OBSTETRICS
Intemational Joumal of Gynecology & Obstetrics 60 (1998) 306-313
ACOG pr act i ce pat t er ns
Shoulder dystocia
Nu mb e r 7, Oc t obe r 1997
Shoulder dystocia is an obstetric emergency. Failure of the shoulders to deliver sponta-
neously i mmedi at el y places both the pregnant woman and fetus at risk for injury. Re-
ported incidence ranges from less than 1% to slightly more than 4% among vaginal
cephalic deliveries. Differences in reported rates are partly due to clinical variation in
describing shoulder dystocia. The diagnosis of shoulder dystocia has a subjective com-
ponent. Although severe cases are readily apparent, milder forms may be over- or un-
derestimated. As a result, researchers differ in their approaches to defining shoulder
dystocia. Some accept a clinician' s judgment, noted in the chart, that shoulder dystocia
occurred. Others require documentation of specific release maneuvers or other proce-
dures to substantiate a diagnosis of shoulder dystocia. As a result, incidence figures
vary. Over time, several maneuvers to release impacted shoulders have been devel-
oped, but the rarity and urgency of this event makes prospective studies to compare
them impractical. Prevention is largely confined to planned cesarean delivery for preg-
nancies considered to be most at risk for shoulder dystocia.
The purpose of this document is to provide information based on published studies
regarding the prediction, prevention, and management of deliveries complicated by
shoulder dystocia to assist obstetrician-gynecologists in providing care to their patients.
These practice guidelines will enable physicians to:
Determine whet her shoulder dystocia can be predicted
Identify strategies to manage shoulder dystocia
Determine whet her elective cesarean delivery is an effective strategy to prevent
shoulder dystocia
The MEDLINE database was used to conduct a literature search to locate relevant ar-
ticles published between 1985 and 1997. The search was restricted to articles published
in the English language. Articles reporting results of original research were given prior-
ity, although review articles and commentaries were consulted as well. Abstracts of
research presented at symposia and scientific conferences were not considered adequate
for inclusion in this document. Guidelines published by organizations or institutions
such as the National Institutes of Health and the Ameri can College of Obstetricians and
Gynecologists were reviewed, and additional studies were located by reviewing bibli-
ographies of articles l ocat ed via MEDLINE. Studies were col l ect ed and grouped
according to topic. In most cases, studies involving fewer than 50 subjects were not
evaluated. When reliable research was not available, expert opinions from obstetri-
ci an-gynecol ogi st s were used.
ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313 307
St udi es wer e r evi ewed and eval uat ed f or qual i t y accor di ng t o t he met hod out l i ned
by t he U. S. Pr event i ve Ser vi ces Task For ce:
I Evi dence obt ai ned f r om at l east one pr oper l y desi gned r andomi zed cont r ol l ed
trial
II-1 Evi dence obt ai ned f r om wel l - desi gned cont r ol l ed trials wi t hout r andomi zat i on
II-2 Evi dence obt ai ned f r om wel l - desi gned cohor t or case- cont r ol anal yt i c st udi es,
pr ef er abl y f r om mor e t han one cent er or r esear ch gr oup
1I-3 Evi dence obt ai ned f r om mul t i pl e t i me seri es wi t h or wi t hout t he i nt er vent i on.
Dr amat i c resul t s in uncont r ol l ed exper i ment s coul d al so be r egar ded as this t ype
of evi der i ce
III Opi ni ons of r espect ed aut hori t i es, based on cl i ni cal exper i ence, descr i pt i ve st ud-
ies, or report s of exper t commi t t ees
Results Can shoulder dystocia be accurately predicted and prevented?
The i deal ma na ge me nt st r at egy f or shoul der dyst oci a is pr event i on. Theor et i cal l y, mos t
cases of shoul der dyst oci a coul d be avoi ded i f f et uses at ri sk wer e i dent i f i ed bef or e
l abor and sel ect ed f or el ect i ve cesar ean del i very. However , this st r at egy rel i es on sev-
eral under l yi ng assumpt i ons that, in reality, are not t rue. Thes e er r oneous assumpt i ons
are
Ri sk f act or s f or shoul der dyst oci a can al ways be i dent i f i ed pr i or t o labor.
The pr es ence of ri sk f act or s is hi ghl y pr edi ct i ve of shoul der dyst oci a.
Ri sks associ at ed wi t h shoul der dyst oci a are gr eat er t han ri sks associ at ed wi t h
pl anned cesar ean del i ver i es t o avoi d shoul der dyst oci a.
Cost s associ at ed wi t h pl anned cesar ean del i ver i es t o avoi d shoul der dyst oci a
are less t han t he cost s associ at ed wi t h shoul der dyst oci a- r el at ed injuries.
Predictors of shoulder dystocia
Ther e have been ma ny effort s t o i dent i f y ri sk fact ors. Ma c r os omi a and mat er nal di abe-
tes consi st ent l y appear across many st udi es as t he t wo ri sk f act or s mos t st r ongl y associ -
at ed wi t h shoul der dyst oci a ( Level II-2: 1- 5) ( Level II-3: 6). Pr egnant wome n who
have di abet es are t wo t o six t i mes mor e l i kel y t o exper i ence shoul der dyst oci a t han
wome n who do not have di abet es ( Level I1-2: 1, 3, 5). The i nci dence of shoul der dyst o-
ci a i ncr eases i n di r ect pr opor t i on t o i nf ant bi rt h wei ght whet her or not t he woman has
di abet es, al t hough wome n who have di abet es exper i ence si gni f i cant l y gr eat er rat es of
shoul der dyst oci a in each wei ght gr oup ( Level 11-2: 2, 4, 5, 7- 9) (see Tabl es 1 and 2).
TABLE 1. Risk o f Sho u l der Dysto cia Acco r din g to Dia betic Sta tu s
Author Increase in Risk Associated with Diabetic Status
Acker et a 119851
Ba ha r 1996 ~
La n ger et a l 1991 ~
Sa n dmir e et a l 19884
Ra te r a tio 5.2
Odds r a tio 4 .3; 95% CI 2.2-8.3
Rel a tive r isk <4 ,000 g 2.6; 95% CI 1.29-5.34
Rel a tive r isk >4 ,000 g 3.6; 95% CI 2.37-4 .76
Rel a tive r isk 6.5; 95% CI 1.5-27.1
308
ACOG practice patterns /International Journal of Gynecology & Obstetrics 60 (1998) 306-313
TABLE 2. Ra te o f Sho u l der Dysto cia Rel a ted to Bir th Weight a n d Dia bet!c Sta tu s
Birth Weight (g) Women Without Diabetes ( %) Women wi th Diabetes ( %)
<4 ,000 0.1-1.1 0.6-3.7
4 ,000-4 ,4 4 9 1.1-10.0 4 .9-23.1
_>4,500 4 .1-22.6 20.0-50.0
So u r ces: Acker DB, Sa chs BP, Fr iedma n EA. Risk fa cto r s fo r sho u l der dysto cia . Obstet Gyn eco l 1985;66:762-768;
a I-Na ja shi S, a I-Su l eima n SA, eI-Ya hia A, Ra hma n MS, Ra hma n J. Sho u l der dysto cia : a cl in ica l stu dy o f 56 ca ses. Au st N
Z J Obstet Gyn a eco 11989;29:129-132; La n ger 0, Ber ku s MD, Hu ff RW, Sa mu el o ff A. Sho u l der dysto cia : sho u l d the fetu s
weighin g __4 ,000 gr a ms be del iver ed by cesa r ea n sectio n ? Am J Obstet Gyn eco 11991 ;165:831--837.
Although risk increases with birth weight and diabetic status, a substantial propor-
tion of cases occur among women who do not have diabetes and among infants with
birth weights of less than 4,000 g. Predicting which patients are likely to experience
shoulder dystocia based on the presence of risk factors has been unsuccessful. Acker et
al reported a low sensitivity when diabetes mellitus and macrosomi a were used to pre-
dict cases of shoulder dystocia; the presence of these risk factors accurately predicted
onl y 55% of cases (Level II-2: 1). Additional studies failed to find any combination of
risk fact ors that could predict which pregnancies would be complicated by shoulder
dystocia (Level II-2: 3, 4, 7, 8, 10). In each case, risk factors could be identified, but
their predictive value was not high enough to be useful in a clinical setting.
Planned cesarean deli very
Because identification of antenatal risk factors has not proved useful in preventing shoul-
der dystocia, a broad policy of planned cesarean delivery for macrosomic fetuses has
been suggested. This strategy seeks to prevent shoulder dystocia by identifying a sub-
group with a known risk factor, macrosomia, and selecting those fetuses for cesarean
delivery. To be successful, several elements must exist. There must be a high correla-
tion between macrosomia and shoulder dystocia, as well as a reliable met hod for iden-
tifying fetal macrosomia. In addition, the risks associated with shoulder dystocia must
be greater than the risks associated with the additional cesarean deliveries resulting
from the policy.
For women who do not have diabetes, the policy is unfeasible. Although there is a
greater incidence of shoulder dystocia among macrosomic infants, most do not experi-
ence this complication. Consequently, i f all fetuses suspected of being macrosomic
underwent cesarean delivery, there would be a disproportionate impact on the increased
cesarean rate compared with the reduction in rate of shoulder dystocia (Level II-2: 5, 8)
(Level II-3:11). For example, Gross et al projected a 27% increase in the total cesarean
rate (rising from 15.1% to 19.1%) i f cesarean deliveries were performed for all patients
with fetuses that weighed 4,000 g or more; unfortunately, the number of shoulder dys-
tocia cases would be reduced by only 42% (Level II-2: 8). Delpapa et al reported simi-
lar results among fetuses with estimated birth weights of 4,000 g or more; in their study,
an additional 76 cesarean deliveries would have prevented onl y five cases of shoulder
dystocia, none of which resulted in permanent injury (Level II-3:11). A recently pub-
lished decision analysis estimated an additional 2,345 cesarean deliveries would be
required, at a cost of $4.9 million annually, to prevent one permanent injury resulting
from shoulder dystocia i f all fetuses suspected of weighing 4,000 g or more underwent
cesarean delivery (Level III: 12).
ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313 309
Even i f the weight threshold were increased to 4,500 g, the pol i cy remains ques-
tionable. Opinion is divided over whether the benefits out wei gh the risks. More cases
of shoulder dyst oci a woul d be prevented, but the impact on the cesarean del i very rate
woul d also be greater. Dependi ng on the distribution of shoulder dyst oci a cases within
a given population, planned cesarean delivery may provide more benefits than risks.
Two investigators reported more than 50% of their cases occurred among infants weigh-
ing 4,500 g or more, but this finding was unusual (Level I1-3: 6, 13). Others report that
20% or less of shoulder dyst oci a cases coul d be prevented by cesarean del i very for
infants with birth weights of 4,500 g or more (Level 11-2: 1, 5, 7) (Level I1-3:14).
Gross et al argued that despite preventing fewer cases overall, infants weighing
4,500 g or more coul d benefit from planned cesarean delivery wi t hout adversely affect-
ing the cesarean delivery rate; within the population studied, 20 cases of shoulder dys-
tocia woul d have been prevented among 42 spontaneous vaginal deliveries with birth
weights of 4,500 g or greater, and the cesarean delivery rate woul d only have increased
from 15.1% to 15.7% (Level 1I-2: 8). Another investigator supporting routine cesarean
delivery for birth weights greater than 4,500 g calculated the pol i cy woul d reduce the
incidence of shoulder dyst oci a by more than 50% while increasing the cesarean rate by
only 1.7% (Level 11-3: 6). At the other end of the spectrum, Baskett et al project ed that
implementing the pol i cy within their study population woul d have resulted in an addi-
tional 817 cesarean deliveries while preventing only 69 cases of shoulder dyst oci a and
15 cases of brachial plexus pal sy (Level 11-2: 7). A separate study of 590 vaginal deliv-
eries of infants weighing 4,500 g or more found only 54 cases of shoulder dystocia,
with fi ve brachial palsies, three fractured clavicles, and no permanent injuries (Level
11-3: 15). According to a decision analysis, the national impact of this policy woul d be
$8.7 million annually, with an additional 3,695 cesarean deliveries required to prevent
one permanent injury (Level 111: 12). The cesarean del i very rate woul d be projected to
rise from 19.1% to 27.6% (Level 111: 12). According to the evidence, the costs associ-
ated with routine cesarean delivery for estimated fetal weights of 4,500 g or more woul d
be costly without commensurat e benefits.
Among women with diabetes, shoulder dyst oci a cases are more concentrated within
the heavier birth weight classes (Level I1-2: 1, 2, 5). Approximately 70% of cases among
women with diabetes occur at infant birth weights of 4, 000 g or more, compared with
50% among those of women without diabetes. Therefore, a pol i cy of planned cesarean
delivery is more likely to prevent shoulder dyst oci a cases among pregnant women with
diabetes. The evi dence confirms this finding. Acker et al reported that almost 55% of
shoulder dystocia among women with diabetes could be prevented i f fetuses that weighed
4,000 g or more underwent cesarean delivery (Level 11-2: 1). Langer et al found that
76% of shoulder dyst oci a cases among pregnant women with diabetes could be pre-
vented i f fetuses weighing 4, 250 g or more underwent cesarean del i very (Level II-2: 5).
In contrast, Keller et al found no justification for a 4,000-g threshold among women
with gestational diabetes because more than half the cases occurred in infants weighing
less than 4,000 g and the ultrasound estimates of fetal weight were inaccurate (Level II-
2: 9). A decision analysis project ed that a 4,500-g threshold for fetuses of women with
diabetes woul d require an additional 443 procedures to prevent one permanent brachial
plexus injury, at a cost of $930, 000 (Level 111: 12). The studies indicate that for preg-
nant women with diabetes who are suspected of carrying macrosomi c fetuses, a planned
cesarean del i very may be a reasonable course of action, depending on the incidence of
shoulder dystocia, the accuracy of predicting macrosomia, and the cesarean del i very
rate within a specific population.
310 ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313
The policy of planned cesarean delivery relies also on accurate estimates of fetal
weight. Fetal weights are calculated from measurement s taken during ultrasound ex-
aminations. Ultrasonography is an inaccurate predictor of macrosomia. Among the gen-
eral population, ultrasonography could correctly identify macrosomi a only about 60%
of the time, according to a pooled estimate of 13 studies (Level III: 12). Within the
diabetic population, ultrasonography has provided mi xed results. There is evidence of
accelerated fetal growth, most notably in the abdominal ci rcumference and chest-to-
head ratio (Level 11-2: 16-18). However, the clinical usefulness of this information has
been limited. One study correctly predicted 88.8% of macrosomi a cases among preg-
nant women with diabetes, based on measurement s of abdominal ci rcumference and
estimated fetal weight (Level 11-2: 17). However, there are no studies document i ng the
usefulness of identifying macrosomi c fetuses for pl anned cesarean delivery among
women with diabetes.
How often does shoulder dystocia result in an injury to the newborn?
Brachial plexus injuries and fractures of the clavicle and humerus are associated with
shoulder dystocia. The most potentially serious, brachial plexus injuries, can be caused
by ext reme amounts of traction and flexion exert ed on the infant' s neck. These injuries
may result in permanent disability. The reported i nci dence of brachial plexus injuries
following a delivery complicated by shoulder dystocia varies widely from 4% to 40%
(1,2, 6-9, 13, 14, 19-22). Fortunately, most cases resolve without permanent disability.
Reports indicate bet ween 9% and 25% of brachial plexus injuries persist (2, 7, 9, 14).
Placed in perspective, fewer than 10% of all shoulder dystocia cases result in a persis-
tent brachial plexus injury (2, 7, 9, 14). Moreover, brachial plexus injuries can occur
without shoulder dystocia and at birth weights of less than 4,000 g (23).
Are any of the maneuvers used to release impacted shoulders either more
likely to cause injuries or more likely to be successful?
Because of the rarity and urgency of shoulder dystocia, only a limited amount of data
exists comparing management techniques. Two separate studies confi rm that the com-
bination of traction and fundal pressure is associated with brachial plexus injuries as
well as with fractures of the humerus and clavicle (Level II-2: 7) (Level II-3: 20). There
is no indication, however, that any particular management technique is superior to an-
other once shoulder dystocia occurs.
There is evidence that injuries might and do occur despite application of appropri-
ate obstetric maneuvers (Level 11-3: 24). During a series of deliveries, the obstetrician
wore a tactile-sensing device that recorded the peak and duration of forces applied to
the head and neck of the fetus. During the study, t wo cases of shoulder dystocia oc-
curred to infants with similar birth weights and obstetric protocols. One infant sus-
tained a shoulder dystocia-related injury and the ot her did not (Level II-3: 24).
The McRoberts maneuver relies on maternal manipulation and is reported to be
effective (Level 11-2: 7, 19) (Level 11-3: 25). Successful use of the McRoberts maneu-
ver is document ed in the scientific literature. The maneuver involves sharply flexing
the patient' s legs against her abdomen. Results from a laboratory study using model s of
the maternal pelvis, fetal head, and fetal shoulders demonstrated that less force was
required to deliver fetuses using the McRoberts maneuver compared with the standard
lithotomy position (26).
ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313 311
Summary and Bas ed on t hi s hi ghest l evel of evi dence f ound in t he dat a, t he f ol l owi ng r e c o mme n da -
Recommendations t i ons ar e pr ovi ded and gr aded accor di ng t o t he f ol l owi ng cat egor i es:
A The r e is good evi dence t o s uppor t t he r e c omme nda t i on.
B The r e is f ai r evi dence t o suppor t t he r e c omme nda t i on.
C Ther e is i nsuf f i ci ent evi dence t o s uppor t t he r e c omme nda t i on; however , t he r ec-
omme nda t i on ma y be ma de on ot her gr ounds.
Prediction and prevention of shoulder dystocia
Mos t cases of s houl der dys t oci a cannot be pr edi ct ed or pr e ve nt e d be c a us e accur at e
me t hods f or i dent i f yi ng whi ch f et uses wi l l exper i ence this compl i cat i on do not exi st ,
and per f or mi ng cesar ean del i ver i es f or all wo me n suspect ed of car r yi ng a ma c r os omi c
f et us is not appr opr i at e (B: 11-2).
Ul t r as onogr aphi c me a s ur e me nt s t o es t i mat e ma c r o s o mi a ha ve l i mi t ed accur acy (B:
1I-2).
Pl anned ces ar ean del i ver y on t he basi s of s us pect ed ma c r o s o mi a i n t he gener al popu-
l at i on is not a r eas onabl e s t r at egy be c a us e t he numbe r and cost o f addi t i onal cesar -
ean del i ver i es r equi r ed t o pr event one pe r ma ne nt i nj ur y is exces s i ve (B: I1-2).
Pl anned ces ar ean del i ver y ma y be a r eas onabl e st r at egy f or di abet i c pr egnant wo me n
wi t h es t i mat ed fet al wei ght s exceedi ng 4, 250--4, 500 g (B: 1/-2).
Shoulder dystocia as a cause of i nj ury to newborns
I nj ur i es are a c o mmo n out c ome as s oci at ed wi t h s houl der dys t oci a and ma y oc c ur
despi t e use of appr opr i at e st andar d obst et r i c ma ne uve r s (B: I1-3). Br achi al pl exus
i nj uri es, f r act ur es of t he humer us , and f r act ur es o f t he cl avi cl e ar e t he mos t c om-
mo n l y r epor t ed i nj uri es as s oci at ed wi t h s houl der dys t oci a (A: 11-2).
Fe we r t han 10% of all del i ver i es c ompl i c a t e d by s houl der dys t oci a wi l l r esul t in a
per si st ent br achi al pl exus i nj ury ( A: I I - 2) .
References
Release techniques
Ther e is no evi dence t hat any one ma n e u ve r is s uper i or to anot her in r el eas i ng an
i mpa c t e d shoul der or r educi ng t he chance of injury. Howe ve r , t he Mc Robe r t s ma -
ne uve r is easi l y f aci l i t at ed and has a hi gh success r at e wi t hout an as s oci at ed i ncr eas e
in r i s k o f i nj ury t o the ne wbor n (B: 1I-2).
Tr act i on c ombi ne d wi t h f undal pr es s ur e has been associ at ed wi t h a hi gh r at e o f br a-
chi al pl exus i nj uri es and f r act ur es (B: 1I-2).
I. Acker DB, Sachs BP, Friedman EA. Risk factors for shoulder dystocia. Obstet Gynecol 1985;66:762-
768
2. al-Najashi S, al-Suleiman SA, el-Yahia A, Rahman MS, Rahman J. Shoulder dystocia: a clinical study
of 56 cases. Aust N Z J Obstet Gynaecol 1989;29:129-132
3. Bahar AM. Risk factors and fetal outcome in cases of shoulder dystocia compared with normal deliv-
eries of a similar birthweight. Br J Obstet Gynaecol 1996;103:868-872
4. Sandmire HF, O'Halloin TJ. Shoulder dystocia: its incidence and associated risk factors. Int J Gynaecol
Obstet 1988;26:65-73
5. Langer O, Berkus MD, Huff RW, Samueloff A. Shoulder dystocia: should the fetus weighing >4000
grams be delivered by cesarean section? Am J Obstet Gynecol 1991;165:831-837
6. el Madany AA, Jallad KB, Radi FA, el Hamdan H, O'deh HM. Shoulder dystocia: anticipation and
outcome. Int J Gynecol Obstet 1990;34:7-12
7. Baskett TF, Allen AC. Perinatal implications of shoulder dystocia. Obstet Gynecol 1995;86:14-17
312 ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313
8. Gross TL, Sokol RJ, Williams T, Thompson K. Shoulder dystocia: a fetal-p.hysician risk. Am J Obstet
Gynecol 1987;156:1408-1418
9. Keller JD, Lopez-Zeno JA, Dooley SL, Socol ML. Shoulder dystocia and birth trauma in gestational
diabetes: a five-year experience. Am J Obstet Gynecol 1991;165:928-930
10. Nocon JJ, McKenzie DK, Thomas LJ, Hansell RS. Shoulder dystocia: an analysis of risks and obstetric
maneuvers. Am J Obstet Gynecol 1993;168:1732-1739
11. Delpapa EH, Mueller-Heubach E. Pregnancy outcome following ultrasound diagnosis of macrosomia.
Obstet Gynecol 1991;78:340-343
12. Rouse DJ, Owen J, Goldenberg RL, Cliver SP. The effectiveness and costs of elective cesarean deliv-
ery for fetal macrosomia diagnosed by ultrasound. JAMA 1996;276:1480-1486
13. Hassan AA. Shoulder dystocia: risk factors and prevention. Aust N Z J Obstet Gynaecol 1988;28:107-
109
14. Mordson JC, Sanders JR, Magann EF, Wiser WL. The diagnosis and management of dystocia of the
shoulder. Surg Gynecol Obstet 1992;175:515-522
15. Menticoglou SM, Manning FA, Morrison I, Harman CR. Must macrosomic fetuses be delivered by a
cesarean section? A review of outcome for 786 babies greater than or equal to 4,500 g. Aust N Z J
Obstet Gynaecol 1992;32:100-103
16. Bracero LA, Baxi LV, Rey HR, Yeh MN. Use of ultrasound in antenatal diagnosis of large-for-gesta-
tional age infants in diabetic gravid patients. Am J Obstet Gynecol 1985;152:43-47
17. Tamura RK, Sabbagha RE, Depp R, Dooley SL, Socol ML. Diabetic macrosomia: accuracy of third
trimester ultrasound. Obstet Gynecol 1986;67:828-832
18. Modanlou HD, Komatsu G, Dorchester W, Freeman RK, Bosu SK. Large-for-gestational-age neo-
nates: anthropometric reasons for shoulder dystocia. Obstet Gynecol 1982;60:417-423
19. Gonik B, Hollyer L, Allen R. Shoulder dystocia recognition: differences in neonatal risks for injury.
Am J Perinatol 1991 ;8:31-34
20. Gross SJ, Shime J, Farine D. Shoulder dystocia: predictors and outcome. A five-year review. Am J
Obstet Gynecol 1987; 156:334-336
21. Hopwood HG Jr. Shoulder dystocia: fifteen years' experience in a community hospital. Am J Obstet
Gynecol 1982;144:162-166
22. Lurie S, Insler V, Hagay ZJ. Induction of labor at 38 to 39 weeks of gestation reduces the incidence of
shoulder dystocia in gestational diabetic patients class A2. Am J Perinatol 1996;13:293-296
23. Graham EM, Forouzan I, Morgan MA. A retrospective analysis of Erb's palsy cases and their relation
to birth weight and trauma at delivery. J Matern Fetal Med 1997;6:1-5
24. Allen R, Sorah J, Gonik B. Risk factors for shoulder dystocia: an engineering study of clinician-
applied forces. Obstet Gynecol 1991 ;77:352-355
25. Smeltzer JS. Prevention and management of shoulder dystocia. Clin Obstet Gynecol 1986;29:299-308
26. Gonik B, Allen R, Sorab J. Objective evaluation of the shoulder dystocia phenomenon: effect of mater-
nal pelvic orientation on force reduction. Obstet Gynecol 1989;74:44-48
ACOG practice patterns / International Journal of Gynecology & Obstetrics 60 (1998) 306-313 313
Practice Patterns are clinical practice guidelines developed by The American College of Obstetricians and
Gynecologists (ACOG) to assist practitioners and patients in making decisions about appropriate obstetric
and gynecologic care. Each Practice Pattern focuses on a clinical issue and is based on a review and
analysis of the scientific literature. The information and recommendations reflect scientific and clinical
knowledge current as of the publication date and are subject to change as advances in diagnostic tech-
niques and treatments emerge. In addition, variations of practice, taking into account the needs of the
individual patient, resources, and limitations unique to the institution or type of practice, may warrant
alternative treatment or procedures to the recommendations outlined in this document. Therefore, these
guidelines should not be construed as dictating an exclusive course of treatment or procedure.
Copyright 1997 The American College of Obstetricians and Gynecologists, 409 l~2th Street, SW, PO
Box 96920, Washington, DC 20090-6920. Requests for authorization to make photocopies should be di-
rected to the Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923; telephone (508)
750-8400.
ISSN 1083-3331 12345/10987
Vous aimerez peut-être aussi
- Diagnosis and Treatment of Medial Epicondylitis of The ElbowDocument13 pagesDiagnosis and Treatment of Medial Epicondylitis of The ElbowSAKAI69Pas encore d'évaluation
- Biomechanical Models For The Pathogenesis Upper Extremity DisordersDocument17 pagesBiomechanical Models For The Pathogenesis Upper Extremity DisordersSAKAI69Pas encore d'évaluation
- Psicosocial Factors and EpicondylitisDocument13 pagesPsicosocial Factors and EpicondylitisSAKAI69Pas encore d'évaluation
- Niosh Case MSDDocument590 pagesNiosh Case MSDAntonio NeiPas encore d'évaluation
- Lateral and Medial Epicondylitis Role of Occupational FactorsDocument15 pagesLateral and Medial Epicondylitis Role of Occupational FactorsSAKAI69Pas encore d'évaluation
- Cleary TendinitisDocument42 pagesCleary TendinitisSAKAI69Pas encore d'évaluation
- Biomechanical Models For The Pathogenesis Upper Extremity DisordersDocument17 pagesBiomechanical Models For The Pathogenesis Upper Extremity DisordersSAKAI69Pas encore d'évaluation
- Physical Examinations in Musculoskeletal Disorders of The ElbowDocument6 pagesPhysical Examinations in Musculoskeletal Disorders of The ElbowSAKAI69Pas encore d'évaluation
- JetlagDocument1 pageJetlagSAKAI69Pas encore d'évaluation
- Clinics in ObstetricsDocument770 pagesClinics in ObstetricsSAKAI69100% (3)
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaPas encore d'évaluation
- Understanding and Counteracting Fatigue in Flight Crews: Ames Research Center, Moffett Field, CaliforniaDocument1 pageUnderstanding and Counteracting Fatigue in Flight Crews: Ames Research Center, Moffett Field, CaliforniaSAKAI69Pas encore d'évaluation
- Jetlag PDFDocument6 pagesJetlag PDFSAKAI69Pas encore d'évaluation
- Dennerlein, Forearm LFF, AIHA2003Document8 pagesDennerlein, Forearm LFF, AIHA2003SAKAI69Pas encore d'évaluation
- 2012 - Potvin - An Equation To Predict Maximum Acceptable Loads For Repetitive Tasks Based On Duty Cycle - Evaluation With Lifting and Lowering TasksDocument5 pages2012 - Potvin - An Equation To Predict Maximum Acceptable Loads For Repetitive Tasks Based On Duty Cycle - Evaluation With Lifting and Lowering TasksSAKAI69Pas encore d'évaluation
- JoL Quality of Life MeasuresDocument12 pagesJoL Quality of Life MeasuresSAKAI69Pas encore d'évaluation
- Jet LagDocument98 pagesJet LagSAKAI69Pas encore d'évaluation
- NASA News: National Aeronautics and Space Administration Washington. DC 20546 AC 202 755-8370Document4 pagesNASA News: National Aeronautics and Space Administration Washington. DC 20546 AC 202 755-8370SAKAI69Pas encore d'évaluation
- 126999Document15 pages126999SAKAI69Pas encore d'évaluation
- Distocia de Hombro PDFDocument4 pagesDistocia de Hombro PDFSAKAI69Pas encore d'évaluation
- 1997 - Potvin & Bent - NIOSH Equation Horizontal Distances Associated With The Liberty Mutual (Snook) Lifting Table Box WidthsDocument7 pages1997 - Potvin & Bent - NIOSH Equation Horizontal Distances Associated With The Liberty Mutual (Snook) Lifting Table Box WidthsSAKAI69Pas encore d'évaluation
- Kurzbetriebsanleitung Junkers Ju 87 D-3 Für Den Flugzeugführer - EnglishDocument3 pagesKurzbetriebsanleitung Junkers Ju 87 D-3 Für Den Flugzeugführer - EnglishSAKAI69Pas encore d'évaluation
- LymphedemaDocument4 pagesLymphedemaSAKAI69Pas encore d'évaluation
- The Pathophysiology of LymphedemaDocument4 pagesThe Pathophysiology of LymphedemaSAKAI69Pas encore d'évaluation
- Kagero Asy Lotnictwa 02 Josef Priller, Hans Waldmann, Wolfgang SpateDocument30 pagesKagero Asy Lotnictwa 02 Josef Priller, Hans Waldmann, Wolfgang SpateRaul Garcia100% (5)
- Lymphedema: Clinical Picture, Diagnosis and Management: Tanja Planinšek Ru Čigaj and Vesna Tlaker ŽunterDocument17 pagesLymphedema: Clinical Picture, Diagnosis and Management: Tanja Planinšek Ru Čigaj and Vesna Tlaker ŽunterSAKAI69Pas encore d'évaluation
- Lymphedema 101: Part 1: Understanding The Pathology and DiagnosisDocument5 pagesLymphedema 101: Part 1: Understanding The Pathology and DiagnosisSAKAI69Pas encore d'évaluation
- Post Lymphedema 1Document7 pagesPost Lymphedema 1SAKAI69Pas encore d'évaluation
- Lymphedema ReviewDocument8 pagesLymphedema ReviewSAKAI69Pas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Preterm Rupture of MembranesDocument13 pagesPreterm Rupture of Membranesjoyrena ochondraPas encore d'évaluation
- Pamj 36 186Document9 pagesPamj 36 186PMKP RSIAANUGRAHPas encore d'évaluation
- Solutio Plasenta JournalDocument7 pagesSolutio Plasenta JournalAndi NatalonnaPas encore d'évaluation
- Breech PDFDocument4 pagesBreech PDFMiguel Cuevas Dolot100% (1)
- Impact of Preeclampsia On Birth Outcomes: Xu Xiong, MD, DRPHDocument15 pagesImpact of Preeclampsia On Birth Outcomes: Xu Xiong, MD, DRPHMichelle FortesPas encore d'évaluation
- PhilHealth ClaimForm3Document2 pagesPhilHealth ClaimForm3slyn_boneheadPas encore d'évaluation
- Please Fill This Story Below Into The Partogram CompletelyDocument1 pagePlease Fill This Story Below Into The Partogram CompletelydwindoksmPas encore d'évaluation
- Unsatisfactory Progress of LabourDocument13 pagesUnsatisfactory Progress of LabourQp NizamPas encore d'évaluation
- Characteristics of The Obstetric ForcepsDocument10 pagesCharacteristics of The Obstetric ForcepsNIRANJANA SHALINIPas encore d'évaluation
- RCOG Assisted Vaginal BirthDocument43 pagesRCOG Assisted Vaginal BirthMarPas encore d'évaluation
- MR Obgyn LMRDocument25 pagesMR Obgyn LMRRian Segal HidajatPas encore d'évaluation
- Cambridge Assessment International Education: Agriculture 5038/12 October/November 2017Document24 pagesCambridge Assessment International Education: Agriculture 5038/12 October/November 2017Ahmed NaserPas encore d'évaluation
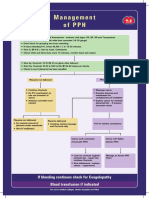
- Management of PPHDocument1 pageManagement of PPH098 U.KARTHIK SARAVANA KANTHPas encore d'évaluation
- (A.i) O&G PX Clerking TemplateDocument4 pages(A.i) O&G PX Clerking TemplateAfkar IshakPas encore d'évaluation
- NBZ Qobgy V01 092020Document3 pagesNBZ Qobgy V01 092020chong xue erPas encore d'évaluation
- 7 Moms Share What It's Really Like To Have A C-SectionDocument11 pages7 Moms Share What It's Really Like To Have A C-SectionLester Gene Villegas ArevaloPas encore d'évaluation
- 62-Article Text-58-1-10-20190528 PDFDocument5 pages62-Article Text-58-1-10-20190528 PDFputri vinia /ilove cutePas encore d'évaluation
- EINC Midterm ExamDocument12 pagesEINC Midterm ExamRettsu GamingPas encore d'évaluation
- Public Program On Sensitisation of Midwifery Educator TrainingDocument2 pagesPublic Program On Sensitisation of Midwifery Educator TrainingKUSH JOSHIPas encore d'évaluation
- Yemisi Chapter ThreeDocument10 pagesYemisi Chapter ThreeAbimbola OyarinuPas encore d'évaluation
- Pathophysiology of Postpartum HemorrhageDocument2 pagesPathophysiology of Postpartum HemorrhageroxaynnnPas encore d'évaluation
- Fdar HandleDocument2 pagesFdar HandleNicole Elma Caparas100% (4)
- Scenario of Neonatal Respiratory Distress in Tertiary HospitalDocument5 pagesScenario of Neonatal Respiratory Distress in Tertiary HospitalSulabh ShresthaPas encore d'évaluation
- Chapter 4.2 Maternal Care and Services 2022Document61 pagesChapter 4.2 Maternal Care and Services 2022Nicole Sales DiazPas encore d'évaluation
- Pengetahuan Ibu Tentang Mobilisasi Dini Pasca Persalinan Normal Pervaginam Di Wilayah Kerja Puskesmas Labuhan Rasoki Kecamatan Padangsidimpuan Tenggara Tahun 2018Document6 pagesPengetahuan Ibu Tentang Mobilisasi Dini Pasca Persalinan Normal Pervaginam Di Wilayah Kerja Puskesmas Labuhan Rasoki Kecamatan Padangsidimpuan Tenggara Tahun 2018Geuman ChajgoPas encore d'évaluation
- Memorandum of AgreementDocument5 pagesMemorandum of Agreementmacky symprano84% (25)
- Obsteric EmergenciesDocument10 pagesObsteric Emergenciestanmai nooluPas encore d'évaluation
- Neonatal Jaundice PDFDocument7 pagesNeonatal Jaundice PDFChp Luis Monterroso FloresPas encore d'évaluation
- BHW Summary of Services Reporting Form 1Document5 pagesBHW Summary of Services Reporting Form 1MOLINO II SOCIAL SERVICESPas encore d'évaluation
- Management of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055Document14 pagesManagement of Placenta Previa During Pregnancy: M Hadyan Syahputra 71 2016 055khaira_nPas encore d'évaluation