Académique Documents
Professionnel Documents
Culture Documents
Nephrology Quiz Questionnaire - 2
Transféré par
Lp Saikumar DoradlaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Nephrology Quiz Questionnaire - 2
Transféré par
Lp Saikumar DoradlaDroits d'auteur :
Formats disponibles
Special Feature
Nephrology Quiz and Questionnaire: Transplantation
Donald E. Hricik (Discussant),* Richard J. Glassock (Co-Moderator),
and Anthony J. Bleyer (Co-Moderator)
Summary
Presentation of the Nephrology Quiz and Questionnaire (NQQ) has become an annual tradition at the meetings of
the American Society of Nephrology. It is a very popular session judged by consistently large attendance. Members of
the audience test their knowledge and judgment on a series of case-oriented questions prepared and discussed by
experts. They can also compare their answers in real time, using audience response devices, to those of program
directors of nephrology training programs in the United States, acquired through an Internet-based questionnaire.
Topics presented here include transplantation issues. These cases, along with single best answer questions, were
prepared by Dr. Hricik. After the audience responses, the correct and incorrect answers were then briey
discussed and the results of the questionnaire were displayed. This article aims to recapitulate the session and re-
produce its educational value for a larger audiencethat of the readers of the Clinical Journal of the AmericanSociety
of Nephrology. Have fun.
Clin J Am Soc Nephrol 0: cccccc, 2012. doi: 10.2215/CJN.01730212
Case 1: Donald E. Hricik (Discussant)
A 53-year-old man with ESRD secondary to IgA
nephropathy received a kidney transplant from a
deceased donor 6 months ago. The patient received
induction antibody therapy with rabbit antithymo-
cyte globulin. Serum creatinine concentrations ranged
between 1.3 and 1.6 mg/dl during the previous 4
months. Maintenance immunosuppression consisted
of tacrolimus, mycophenolate mofetil, and prednisone.
Other medications include metoprolol, trimethoprim-
sulfamethoxazole, omeprazole, and ergocalciferol. One
week earlier, a serum creatinine concentration was 1.8
mg/dl and a repeat level was 2.0 mg/dl. Results on
surveillance blood PCR for BK polyoma virus were
negative 3 months after transplantation but now show
a viral level of 5000 copies/mL. The patient is entirely
asymptomatic. On examination, his body temperature is
37.2C and his BP is 138/88 mmHg. There is no allo-
graft tenderness. Doppler ultrasonography of the trans-
planted kidney shows no hydronephrosis and mildly
increased resistive indices. A biopsy of the trans-
planted kidney is performed. The pathologist reviews
the light microscopic ndings and notes lymphocytic
inltrates in 20% of the core, as well as mild tubulitis.
Findings are Banff grade suspicious for acute rejec-
tion. No glomerular abnormalities are present.
Question 1A
An immunostain of the transplant renal biopsy to
which ONE of the following antigens would be MOST
helpful in guiding subsequent management (see Figure 1)?
A. C4d complement
B. IgA
C. Simian virus 40 (SV40)
D. JC polyomavirus
E. C3 complement
Discussion of Case 1 (Question 1A)
The best choice is C. The detection of BK polyoma
viremia in a kidney transplant recipient with an in-
creasing serum creatinine concentration raises a
serious concern for BK polyoma virus nephropathy.
Transplant renal biopsy represents the gold standard
for diagnosis of BK polyoma virus nephropathy. How-
ever, in the early stages of this disorder, classic cyto-
pathic changes in epithelial cells may be minimal, and
interstitial inammation, including tubulitis, can be
confused with acute cellular rejection (1,2).
The polyoma viruses are a group of species-specic
small-DNA viruses that include human pathogens
(BK and JC viruses) and the primate pathogen (SV40)
(1). The BK virus shares 70% of DNA sequence ho-
mology with SV40, and immunostaining against the
latter virus forms the basis for the immunohistochem-
ical diagnosis of BK polyoma nephropathy. Antibodies
to BK polyoma virus can be detected in approximately
80% of adults. Viral infection typically occurs in child-
hood and is then followed by a latent state with viral
presence in the uroepithelium, lymphoid tissues, and
brain (3). In the rst year after transplantation, 10%20%
of kidney transplant recipients develop BK viremia.
Reduction of immunosuppression is the mainstay of
therapy (4). With aggressive surveillance protocols,
aimed to detect viremia before the development of
impaired kidney function, graft loss now occurs in less
than 5% of viremic patients. The risk for graft loss is
related to histologic stage, starting with mild inam-
mation (tubulitis), increasing to cytopathic changes in
tubular epithelial cells, and followed by progressive
brosis.
Immunostaining for IgA and C3 would be of some
interest in this patient with underlying IgA nephrop-
athy. However, the absence of glomerular abnor-
malities rules against recurrent IgA nephropathy.
*Division of
Nephrology and
Hypertension,
Department of
Medicine, University
Hospitals Case
Medical Center,
Cleveland, Ohio;
David Geffen School
of Medicine at UCLA,
Los Angeles,
California; and
Section on
Nephrology, Wake
Forest Medical
School, Winston-
Salem, North Carolina
Correspondence: Dr.
Anthony J. Bleyer,
Section on Nephrology,
Wake Forest University
School of Medicine,
Medical Center
Boulevard, Winston-
Salem, NC 27157.
Email: ableyer@
wakehealth.edu
www.cjasn.org Vol 0 , 2012 Copyright 2012 by the American Society of Nephrology 1
. Published on May 17, 2012 as doi: 10.2215/CJN.01730212 CJASN ePress
Furthermore, recurrence of the original disease would
probably not account for marked interstitial inammation
noted on light microscopy. The detection of C4d deposits in
peritubular capillaries represents the histopathologic hall-
mark of acute humoral rejection (5). Unless the pathologist
noted peritubular capillaritis on light microscopy, acute
humoral rejection would not be a serious concern in this
case at this point. The presence of BK viremia, with or
without overt nephropathy, is generally believed to reect
overimmunosuppression (4), in which concurrent cellular
or humoral rejection would be distinctly unusual.
Case 1, continued
Tacrolimus treatment was discontinued and the dose of
mycophenolate mofetil was reduced by 25%. One month
later, results of blood PCR for BK polyoma virus were
negative and the serum creatinine level decreased slightly
to 1.7 mg/dl. Two months later, routine laboratory testing
revealed a serum creatinine concentration of 3.2 mg/dl.
Repeat biopsy showed acute humoral rejection with pos-
itive staining for C4d. Two donor-specic antibodies were
detectable in high titers. Tacrolimus treatment was renewed.
Despite a trial of pulse steroid therapy, plasmapheresis, and
intravenous immunoglobulin, the patient exhibited pro-
gressive renal dysfunction and returned to dialysis treat-
ment 6 months later. One month later, the patient tells you
that a friend from his church wishes to be evaluated as a
possible living donor (Figure 2). He continues to receive
tacrolimus and prednisone.
Question 1B
What is your BEST advice regarding retransplantation
with a living unrelated donor?
A. The rst transplanted kidney is a reservoir for BK polyoma
virus and must be removed before a second transplant.
B. Deceased-donor transplantation is preferred because the
risk for recurrent BK polyoma virus nephropathy is lower
than that with a related donor.
Figure 1. | Responses to question 1A: Immunostaining against which antibody is most likely to guide subsequent management? (Correct
answer: C.)
Figure 2. | Responses to question 1B: What is the best advice regarding re-transplantation with a living unrelated donor? (Correct answer: C.)
2 Clinical Journal of the American Society of Nephrology
C. Repeat BKpolyoma blood PCRshould be performed. If result
is negative, he should continue current immunosuppression
until the second transplantation is performed.
D. Irrespective of the current BKviral load, tacrolimus must be
weaned and discontinued before a second transplant.
Discussion of Case 1 (Question 1B)
The best choice is C. The clinical predicament presented
by this case brings up two controversial management issues:
(1) the role of transplant nephrectomy before retransplanta-
tion in a patient with a previous graft loss due to BK poly-
oma nephropathy and (2) general management of a patient
with a previously failed allograft.
Because BK polyoma virus can become latent in uro-
epithelial tissues, there is a logical concern that retention of
the failed allograft will create a reservoir for re-infection
of a new graft. However, there is some evidence that BK
present in the donor kidney may serve as the source of the
infection in the recipient, at least in the rst year after
transplantation (3). Moreover, clinical experience has sug-
gested that the risk for BK polyoma nephropathy in a sec-
ond transplant is not inuenced by removal of a previous
graft (6,7). In a recent retrospective study of 31 patients
undergoing retransplantation within a median of 6 months
after graft failure from BK nephropathy, 35% developed
recurrent BK viremia but only 6% developed overt ne-
phropathy (7). Clearance of previous BK viremia was the
only factor associated with lack of recurrence, and the ef-
fects of prior nephrectomy were not signicant.
Controversies regarding the general management of the
patient with a failed graft focus on practices for weaning
immunosuppression and on the role of transplant nephrec-
tomy (8). It is generally recognized that complete weaning
of immunosuppression can lead to increased generation of
anti-HLA antibodies that may limit opportunities for re-
transplantation. However, for patients requiring long
waiting times for deceased-donor kidney transplantation,
continued immunosuppression will increase the risk for
infection. Retrospective studies suggest that removal of a
failed allograft and discontinuation of immunosuppression
may decrease mortality rates and increase the chances of
retransplantation (9). One theory behind these observations
is that the allograft tissue acts as a source of inammation.
However, such studies are fundamentally awed by retro-
spective designs that fail to consider important biases in the
selection of patients for transplant nephrectomy (10). More-
over, other studies suggest that removal of the allograft
actually increases the circulating levels of anti-HLA anti-
bodies (11). The theory here is that the allograft tissue acts
as a sponge for circulating antibodies. There is no con-
sensus about the optimal timing of nephrectomy and wean-
ing of immunosuppression after graft failure. However, in
this case, the availability of a live donor will allow for rel-
atively rapid retransplantation, and one can make a strong
argument to continue immunosuppression to prevent HLA
sensitization, so long as BK viremia is under control. Donor
source (i.e., living versus deceased donor) has not been
identied as a risk factor for BK polyoma viremia after
kidney retransplantation (12).
Case 2: Donald E. Hricik (Discussant)
A 65-year-old man with ESRD due to chronic GN (of
unknown nature) had a previous kidney transplant that
failed 3 years ago. He then began receiving long-term
hemodialysis and was on the waiting list for another kidney
transplant. He continued to work full-time as an attorney. Two
years ago, he was hospitalized for an upper gastrointestinal
hemorrhage resulting from gastric erosions and received 6
units of packed red blood cells. He is now highly sensitized
against HLA antigens; recent ow cytometrymeasured
panel-reactive antibody levels were 92% for class I antigens
Figure 3. | Responses to question 2: Which fact concerning donors after cardiac death is correct? (Correct answer: C.)
Table 1. Criteria for dening an expanded-criteria donor
1. Deceased donor age . 60 yr
OR
2. Deceaseddonor age 5059 yr with $2 of the following:
history of hypertension
terminal serum creatinine concentration .1.5 mg/dl
death from cerebral vascular accident
Clin J Am Soc Nephrol 0: cccccc, , 2012 Nephrology Quiz and Questionnaire: Transplantation, Hricik et al. 3
and 94% for class II antigens. He had previously signed a
consent form agreeing to consider an expanded-criteria
donor (ECD). The patient has been allocated a kidney allo-
graft from a donor after cardiac death (DCD), a 49-year-old
male drowning victim (Figure 3).
Question 2
The patients concerns about accepting this allograft would
BEST be allayed by which ONE of the following facts?
A. Kidneys fromDCDdonors exhibit rates of allograft survival
equivalent to those from ECDs.
B. Kidneys from DCD donors exhibit rates of delayed graft
function similar to those from standard-criteria donors
(SCDs).
C. Kidneys from DCD donors exhibit allograft survival rates
equivalent to those from SCDs.
D. Kidneys from DCD donors exhibit rates of primary non-
function lower than those from ECDs.
Discussion of Case 2 (Question 2)
The correct choice is C, given data from the Scientic
Registry for Transplant Recipients. The denition of an
ECD (Table 1) was derived from a large multivariate
analysis that sought to identify risk factors that collec-
tively posed a 70% increase in the relative risk for graft
loss compared with relatively healthy, younger donors,
also known as SCDs (13). DCDs are donors with terminal
illnesses but intact brain function. Organs from DCDs are
harvested quickly after declaration of asystole. Because
varying degrees of warm ischemia are involved in the
harvesting of DCD organs, it is no surprise that recipients
of these organs experience relatively high rates of delayed
graft function or even primary nonfunction (14). How-
ever, long-term follow-up of patients receiving kidneys
from DCDs indicate that both patient and graft survival
are similar to those achieved with brain-dead donors (15)
(Figure 4), whereas graft survival of DCD recipients is
actually superior to that of ECD recipients (15).
Disclosures
None.
References
1. Wiseman AC: Polyomavirus nephropathy: A current perspec-
tive and clinical considerations. Am J Kidney Dis 54: 131142,
2009
2. Drachenberg CB, Papadimitriou JC: Polyomavirus-associated
nephropathy: Update in diagnosis. Transpl Infect Dis 8: 6875,
2006
3. Bohl DL, Storch GA, Ryschkewitsch C, Gaudreault-Keener M,
Schnitzler MA, Major EO, Brennan DC: Donor origin of BK virus
in renal transplantation and role of HLA C7 in susceptibility to
sustained BK viremia. Am J Transplant 5: 22132221, 2005
4. Babel N, Fendt J, Karaivanov S, Bold G, Arnold S, Sefrin A, Lieske
E, Hoffzimmer M, Dziubianau M, Bethke N, Meisel C, Gru tz G,
Reinke P: Sustained BK viruria as an early marker for the de-
velopment of BKV-associated nephropathy: Analysis of 4128
urine and serum samples. Transplantation 88: 8995, 2009
5. Colvin RB: Antibody-mediated renal allograft rejection: Di-
agnosis and pathogenesis. J Am Soc Nephrol 18: 10461056,
2007
6. Hirsch HH, Ramos E: Retransplantation after polyomavirus-
associated nephropathy: Just do it? Am J Transplant 6: 79, 2006
7. Geetha D, Sozio SM, Ghanta M, Josephson M, Shapiro R,
Dadhania D, Hariharan S: Results of repeat renal transplantation
after graft loss from BK virus nephropathy. Transplantation 92:
781786, 2011
8. Gill JS: Managing patients with a failed kidney transplant: How
can we do better? Curr Opin Nephrol Hypertens 20: 616621,
2011
9. Ayus JC, Achinger SG, Lee S, Sayegh MH, Go AS: Transplant
nephrectomy improves survival following a failed renal allograft.
J Am Soc Nephrol 21: 374380, 2010
10. Schaefer HM, Helderman JH: Allograft nephrectomy after
transplant failure: should it be performed in all patients returning
to dialysis? J Am Soc Nephrol 21: 207208, 2010
Figure 4. | Allograft and patient survival after kidney transplantation using donors after cardiac death (DCD) and donors after brain death
(DBD). Data obtained from reference 14.
4 Clinical Journal of the American Society of Nephrology
11. Knight MG, Tiong HY, Li J, Pidwell D, Goldfarb D: Transplant
nephrectomy after allograft failure is associated with allosensi-
tization. Urology 78: 314318, 2011
12. Dharnidharka VR, Cherikh WS, Neff R, Cheng Y, Abbott KC: Re-
transplantation after BKvirus nephropathy in prior kidney transplant:
An OPTNdatabase analysis. Am J Transplant 10: 13121315, 2010
13. Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon
TE, Metzger RA, Ojo AO, Port FK: Deceased-donor character-
istics and the survival benet of kidney transplantation. JAMA
294: 27262733, 2005
14. Cohen DJ, St Martin L, Christensen LL, Bloom RD, Sung
RS: Kidney and pancreas transplantation in the United
States, 1995-2004. Am J Transplant 6[suppl 2]: 11531169,
2006
15. Rao PS, Ojo A: The alphabet soup of kidney transplantation: SCD,
DCD, ECDfundamentals for the practicing nephrologist. Clin
J Am Soc Nephrol 4: 18271831, 2009
Published online ahead of print. Publication date available at www.
cjasn.org.
Clin J Am Soc Nephrol 0: cccccc, , 2012 Nephrology Quiz and Questionnaire: Transplantation, Hricik et al. 5
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- S2 Sample1Document5 pagesS2 Sample1Lp Saikumar DoradlaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Critical Care Emergency Medicine 03Document5 pagesCritical Care Emergency Medicine 03Cynthia CameliaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Kidney BiopsyDocument6 pagesKidney BiopsyLp Saikumar DoradlaPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Itas2010 - Indiantakayasu'S Arteritis Activity ScoreDocument2 pagesItas2010 - Indiantakayasu'S Arteritis Activity ScoreLp Saikumar DoradlaPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Polymixin Vs ColistinDocument2 pagesPolymixin Vs ColistinLp Saikumar DoradlaPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Vascular AccessDocument6 pagesVascular AccessLp Saikumar DoradlaPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
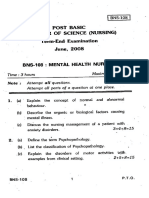
- Post Basic Bachelor of Sctence (Nursing) ' Term-End Examination June, 2OO8Document2 pagesPost Basic Bachelor of Sctence (Nursing) ' Term-End Examination June, 2OO8Lp Saikumar DoradlaPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Indian CKD GuidelinesDocument63 pagesIndian CKD GuidelinesLp Saikumar DoradlaPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- First Clinical Guidelines On Acute Kidney Injury Issued (Printer-Friendly)Document3 pagesFirst Clinical Guidelines On Acute Kidney Injury Issued (Printer-Friendly)Lp Saikumar DoradlaPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Electrolyte Quiz 2008Document38 pagesElectrolyte Quiz 2008Lp Saikumar Doradla100% (2)
- AKI BiomarkersDocument6 pagesAKI BiomarkersLp Saikumar DoradlaPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- 2014 DM MCH ProspectusDocument22 pages2014 DM MCH ProspectusLp Saikumar DoradlaPas encore d'évaluation
- DM MCH 14 Bhu NotificationDocument4 pagesDM MCH 14 Bhu NotificationLp Saikumar DoradlaPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- UrologyDocument22 pagesUrologyLp Saikumar DoradlaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Indian CKD GuidelinesDocument63 pagesIndian CKD GuidelinesLp Saikumar DoradlaPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- CardiologyDocument30 pagesCardiologyLp Saikumar DoradlaPas encore d'évaluation
- IrcDocument129 pagesIrcFreddy RojasPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Renal BiopsyDocument11 pagesRenal BiopsyKiess11Pas encore d'évaluation
- TGA Letter of Demand - 4 July 2023Document30 pagesTGA Letter of Demand - 4 July 2023Tim BrownPas encore d'évaluation
- Oncogenic VirusesDocument83 pagesOncogenic VirusespthamainiPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Midterm Micro-2 Virology Lesson-2Document3 pagesMidterm Micro-2 Virology Lesson-2MYLENE POSTREMOPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Oncogenic VirusesDocument25 pagesOncogenic VirusesMedicina 19Pas encore d'évaluation
- Enveloped and Non Enveloped VirusDocument10 pagesEnveloped and Non Enveloped ViruspixholicPas encore d'évaluation
- Viral OncogenesisDocument36 pagesViral OncogenesisyuanlupePas encore d'évaluation
- Oncogene: Viral OncogenesDocument12 pagesOncogene: Viral OncogenesIlyas Khan AurakzaiPas encore d'évaluation
- Viro 1Document6 pagesViro 1Elsa YuniaPas encore d'évaluation
- 16 Oncogenic Viruses)Document32 pages16 Oncogenic Viruses)Ahmed EisaPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- PapovavirusesDocument25 pagesPapovavirusesIGA ABRAHAMPas encore d'évaluation
- COMPREHENSIVE MycoviroDocument208 pagesCOMPREHENSIVE MycoviroMartin JustoPas encore d'évaluation
- Simian Virus 40 Infection in Humans and Association With Human Diseases: Results and HypothesesDocument9 pagesSimian Virus 40 Infection in Humans and Association With Human Diseases: Results and HypothesesMilan PetrikPas encore d'évaluation
- Malaria and Some Polyomaviruses (Sv40, BK, JC, and Merkel Cell Viruses)Document365 pagesMalaria and Some Polyomaviruses (Sv40, BK, JC, and Merkel Cell Viruses)zahidPas encore d'évaluation
- MCQs in Medical MicrobiologyDocument14 pagesMCQs in Medical Microbiologysidharta_chatterjee100% (8)
- សំណួរត្រៀមDocument1 480 pagesសំណួរត្រៀមNobel PelPas encore d'évaluation
- WartsDocument167 pagesWartseva yustianaPas encore d'évaluation
- Diagnosis of Viral Infections in Animal TissuesDocument3 pagesDiagnosis of Viral Infections in Animal TissuesRandy Butternubs100% (2)
- Horowitz Aids and EbolaDocument11 pagesHorowitz Aids and EboladeliriousheterotopiasPas encore d'évaluation
- Poliomavirus BKDocument30 pagesPoliomavirus BKRobin Gonzalez100% (1)
- Virus-Klasifikasi, Sifat, GenetikaDocument24 pagesVirus-Klasifikasi, Sifat, GenetikaRamano Untoro PutroPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Viral Oncogenesis DR - Fokam-JosephDocument31 pagesViral Oncogenesis DR - Fokam-JosephRosemary FuanyiPas encore d'évaluation
- Understanding Genitourinary System CytologyDocument130 pagesUnderstanding Genitourinary System Cytologyaaes2Pas encore d'évaluation
- 4-Week UFAPS With FA 2021Document2 pages4-Week UFAPS With FA 2021susannahshinyPas encore d'évaluation
- Cam4 5 1239Document12 pagesCam4 5 1239kadiksuhPas encore d'évaluation
- Virus-Klasifikasi, Sifat, GenetikaDocument26 pagesVirus-Klasifikasi, Sifat, Genetikanovia putriPas encore d'évaluation
- Polyomavirus LectureDocument60 pagesPolyomavirus Lecturerggefrm75% (4)
- French Molt Disease: Nasih Hamad Ali College of Veterinary Medicine University of SulaimaniDocument12 pagesFrench Molt Disease: Nasih Hamad Ali College of Veterinary Medicine University of Sulaimaninasih hamadPas encore d'évaluation
- Pox, Parvo, Adeno and Papova VirusesDocument33 pagesPox, Parvo, Adeno and Papova VirusesmicroperadeniyaPas encore d'évaluation
- Clinical Virology Manual (PDFDrive)Document639 pagesClinical Virology Manual (PDFDrive)Shweta KumariPas encore d'évaluation
- Cancer Associated Viruses, (2012) (UnitedVRG)Document868 pagesCancer Associated Viruses, (2012) (UnitedVRG)anon ankon100% (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)