Académique Documents
Professionnel Documents
Culture Documents
The Skin in General Medicine
Transféré par
micheal19600 évaluation0% ont trouvé ce document utile (0 vote)
22 vues6 pagesMedical
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentMedical
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
22 vues6 pagesThe Skin in General Medicine
Transféré par
micheal1960Medical
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 6
11 Heidary N, Naik H, Burgin S.
Chemotherapeutic agents and the skin: an
update. J Am Acad Dermatol
2008;58:54570.
12 Robert C, Soria JC, Spatz A et al.
Cutaneous side-effects of kinase inhibitors
and blocking antibodies. Lancet Oncol
2005;6:491500.
13 Agero AL, Dusza SW, Benvenuto-Andrade
C et al. Dermatologic side effects associated
with the epidermal growth factor receptor
inhibitors. J Am Acad Dermatol
2006;55:65770.
14 Hu JC, Sadeghi P, Pinter-Brown LC, Yashar
S, Chiu MW. Cutaneous side effects of epi-
dermal growth factor receptor inhibitors:
clinical presentation, pathogenesis, and
management. J Am Acad Dermatol
2007;56:31726.
Address for correspondence:
Dr E Topham, Brighton and Sussex
University Hospitals NHS Trust,
Brighton General Hospital, Elm
Grove, Brighton BN2 3EW.
Email: emma.topham@bsuh.nhs.uk
Sasha Dhoat, Locum Consultant
Dermatologist; Malcolm Rustin,
Consultant Dermatologist
Royal Free Hospital, London
KEY WORDS: skin, lyme disease,
Kawasaki disease, hand, foot and
mouth disease
Cutaneous manifestations of systemic
disorders are common in general medi-
cine and can be important presenting
features of internal disease.
1,2
This
review is not comprehensive but high-
lights the most frequent and important
entities.
Infections
Lyme disease (or borreliosis)
The most common tick-borne disease in
the northern hemisphere is lyme disease.
It is transmitted to humans through the
bite of an ixodes tick infected with spiro-
chetes Borrelia afzelii or Borrelia garinii
(most commonly in Europe) or Borrelia
burgdorfei (in the USA). Cases of lyme
disease confirmed by UK laboratories
have increased tenfold since records
began in 1986. Several hundred cases are
reported every year, mainly in the south-
western regions of the country during
summer months. The disease develops in
three stages:
1st stage: in 5075% of patients the
classical rash of erythema chronicum
migrans occurs up to four weeks
after the tick bite (Fig 1). The
annular erythema gradually spreads
outwards from the site of the bite; it
is usually at least 5 cm in diameter
and may develop central clearing,
bruising or necrosis.
2nd stage: this may be followed by
lesions of multiple secondary ery-
thema migrans, musculoskeletal
symptoms (60%) (often migratory
joint pain with or without joint
swelling), neurological manifesta-
tions (15%) (meningitis, facial cra-
nial nerve paralysis and radicular
neuropathies) or, less commonly,
cardiovascular complications (8%),
including varying degrees of atri-
oventricular block).
3rd stage: in 60% of untreated cases
the next stage begins at least seven
months after the primary infection. It
can manifest as intermittent pain and
swelling of the knees and hips, which
may progress to chronic arthritis
(10%). Occasionally, polyneuropathy
or encephalopathy may develop.
Diagnosis and treatment. The history of
a tick bite and skin eruption is highly
characteristic and the diagnosis is pri-
marily clinical.
3
Serological testing
(ELISA and Western blot) is sensitive,
but not specific; both tests may be neg-
ative early in the disease and they do not
accurately distinguish active from past
infection. Lyme disease can be con-
firmed only by culture, although this is
a low yield procedure. Treatment with
doxycycline 200 mg od for one month
should be initiated early to prevent
complications.
Tuberculides
Tuberculides are cutaneous hypersensi-
tivity reactions to tuberculosis (TB)
Royal College of Physicians, 2009. All rights reserved. 379
Clinical Medicine 2009, Vol 9, No 4: 37984
The skin in general medicine
Fig 1. Erythema chronicum migrans.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 379
elsewhere in the body.
4,5
Immunity is
usually high, leading to destruction of
bacilli which are therefore not usually
demonstrable on skin lesions.
Erythema induratum
Erythema induratum presents as red,
painful warm nodules on the lower limbs,
often associated with fever and joint pains.
Unlike erythema nodosum, lesions may
ulcerate and they do not resolve sponta-
neously. Although no overt focus of TB
may be found, the Mantoux and ELISpot
tests are strongly positive and the skin
changes usually respond to antitubercu-
lous therapy. Histology is characterised
by a lobular panniculitis and vasculitis.
Scrofuloderma
Scrofuloderma results from breakdown
of skin overlying a tuberculous focus,
usually at a lymph node. It presents as
firm, painless, subcutaneous nodules
that gradually enlarge and suppurate
forming ulcers and sinus tracts in over-
lying skin. Tubercle bacilli can usually be
isolated from the purulent discharge.
Lupus vulgaris
Lupus vulgaris, the most common form
of cutaneous TB, presents as a solitary
reddish-brown plaque, often on the face,
which shows an apple-jelly colour when
pressed with a glass spatula (diascopy).
Lesions occur due to direct extension of
underlying tuberculous foci, lymphatic
or haematogenous spread, after primary
inoculation, BCG vaccination or in scars
of old scrofuloderma. Affected individ-
uals have a moderate or high degree of
immunity and so isolation of acid-fast
bacilli is rare.
Bacillary angiomatosis
Bacillary angiomatosis presents as mul-
tiple angiomas, primarily in patients with
AIDS, due to bacteria of the Bartonella
genus. Bartonella henselae is most often
transmitted through a cat scratch or bite
but also by ticks and fleas. Bartonella
quintana is usually transmitted by lice.
Kawasaki disease
The most common vasculitic disorder of
childhood worldwide is Kawasaki disease.
It is the leading cause of acquired heart
disease among children in developed
countries. It presents with high spiking
fever lasting at least five days and at least
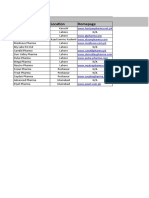
five of the following six symptoms (Fig 2):
bilateral conjunctivitis
red, dry cracked lips
red oral and pharyngeal mucosa
strawberry tongue
widespread polymorphous rash
red swollen hands and, later, desqua-
mation of the fingers, toes, palms and
soles.
Up to one-fifth of untreated children
develop coronary artery aneurysms
which can be associated with mortality.
Early recognition of this syndrome allows
initiation of high-dose intravenous (iv)
immunoglobulin (Ig) (2 gm/kg single
dose) and aspirin (7580 mg/kg/day ini-
tially, followed by aspirin 35 mg/kg/day
in the convalescent phase). This is essential
to prevent cardiovascular complications.
Hand, foot and mouth disease
A disease of childhood, hand, foot and
mouth disease, is caused by infection
380 Royal College of Physicians, 2009. All rights reserved.
CME Dermatology
Fig 2. Manifestations
of Kawasaki disease.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 380
with non-polio enteroviruses, such as
coxsackie virus A16 and enterovirus 71.
It is transmitted via contact with infected
saliva and fluid from blisters or stool.
After an incubation period of 37 days,
oval vesicles with a slightly grey centre
develop in the mouth and on the hands
and feet. Fever, malaise, sore throat,
vomiting and/or diarrhoea may occur.
Symptoms usually resolve within 10
days and more than two-thirds of
infected cases remain asymptomatic.
Polymerase chain reaction can be used to
identify enterovirus 71 which may cause
severe neurological disease (including
viral meningitis, encephalitis or acute
flaccid paralysis), as well as pulmonary
oedema/haemorrhage and myocarditis.
Treatment is supportive.
Gastrointestinal disease
Inflammatory bowel disease
Erythema nodosum may be associated
with inflammatory bowel disease. There
are crops of acute tender, red smooth
nodules, usually over the extensor sur-
faces of the shins, possibly accompanied
by mild fever, malaise and joint pains.
Lesions may reach a diameter of 34 cm.
Later they become mauve and last one to
two weeks. It often reflects active bowel
disease but may precede it. The whole
episode may resolve within six weeks.
Other associations include:
pyoderma gangrenosum (which may
not reflect bowel disease activity)
urticaria
vasculitis (small vessel type and cuta-
neous polyarteritis nodosa)
oral lesions, including ulcers, angular
stomatitis, pyostomatitis vegetans (a
mucosal variant of pyoderma gan-
grenosum), granulomatous infil-
trates of the lips (only Crohns
disease) and acquired enteropathica-
like lesions.
Acrodermatitis enteropathica
Associated with zinc deficiency is acroder-
matitis enteropathica, a triad of circum-
orificial and acral dermatitis, alopecia and
diarrhoea. It is an autosomal recessive dis-
order which presents within a few days or
weeks of life. The vesiculobullous lesions,
which crust and erode, occur around the
eyes, mouth, ears, nose, anus and geni-
talia, and on the fingers and toes.
A similar eruption can be seen with
inadequate zinc intake due to anorexia
nervosa, vegetarian diets or parenteral
nutrition, and with reduced zinc absorp-
tion in coeliac disease, pancreatic insuffi-
ciency, cystic fibrosis, severe infantile
diarrhoea and alcoholism.
Dermatitis herpetiformis
6
This is an extremely itchy, vesicu-
lopapular eruption, usually associated
with gluten-sensitive enteropathy.
Grouped vesicles symmetrically involve
the buttocks, knees, elbows and scalp
(Fig 3). Urticarial lesions and excoria-
tions due to intense pruritus are
common (hence vesicles are often diffi-
cult to detect). Mucous membranes are
occasionally involved.
Overt malabsorption is very rare, except
in patients with associated coeliac disease,
prevalence 3.711.1%, so intestinal biop-
sies are not performed in asymptomatic
patients. There is a small increased risk of
gastrointestinal (GI) malignancy, espe-
cially lymphoma (incidence 2%) and
some evidence to suggest a protective role
of a gluten-free diet (GFD).
Anti-endomysial antibodies are pre-
sent in 52100% of patients (tissue trans-
glutaminase sensitivity 100%, specificity
80%), providing a helpful method to
assess adherence to a GFD. Diagnosis is
confirmed by demonstration of granular
IgA deposits at the dermo-epidermal
junction in perilesional or normal skin
(sensitivity 92.4%).
Liver disease
Mixed cryoglobulinaemia
It is estimated that 7090% of patients
with mixed cryoglobulinaemia (circu-
lating Igs complexed with other Igs that
reversibly precipitate in the cold) have
hepatitis C. A triad of palpable purpura
on the lower extremities (Fig 4),
glomerulonephritis (26%) and periph-
eral neuropathy (8%) should prompt a
screen for hepatitis C infection and
serum IgM and IgG cryoglobulins.
Lesions usually arise after cold exposure
or prolonged standing or sitting, last
310 days and can be associated with
arthralgia (21%).
Polyarteritis nodosa
Also sometimes associated with hepatitis
B and C infection is polyarteritis nodosa,
a multisystem segmental necrotising
Royal College of Physicians, 2009. All rights reserved. 381
CME Dermatology
Fig 3. Excoriated papules and vesicles in dermatitis herpetiformis.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 381
vasculitis of small and medium vessels
with end-organ damage due to
ischaemia, infarcts and haemorrhage.
Painful nodules on the lower legs along
the course of the superficial arteries,
livedo reticularis, digital infarction and
large ulcers may be accompanied by
paraesthaesiae, renal disease, hyperten-
sion, arthralgias and myalgias. Skin or
muscle/nerve biopsy may be helpful
and an arteriogram demonstrates
aneurysms or occlusions of the visceral
arteries.
Acquired porphyria cutanea tarda
A photosensitivite disorder, acquired
porphyria cutanea tarda, is caused by
inhibition of the liver enzyme uropor-
phyrin decarboxylase, a step in the
pathway of haem synthesis. Inhibitors
of the enzyme are formed in the
presence of iron and reactive oxygen
species, such as in hepatitis C,
haemochromatosis, alcohol and oestrogen
intake. The resultant accumulation of
uroporphyrins and coproporphyrins is
hepatotoxic; it may cause liver cir-
rhosis and in some cases hepatocel-
lular carcinoma.
Adults present with tense blisters on
sun-exposed sites, especially the back of
the hands and face, skin fragility and
healing with scars and milia. There may
be hypertrichosis, hyperpigmentation
and morphoea. Urine and blood/faeces
samples demonstrate an excess of uro-
porphyrins (samples must be protected
from light and transported in black
opaque bags).
Primary biliary cirrhosis
Primary biliary cirrhosis (PBC) is com-
monly associated with generalised pru-
ritus (70%), diffuse hyperpigmentation
and xanthomata (eruptive, planar and
occasionally tuberous). There is also a
more frequent association with lichen
planus, scleroderma and CREST
syndrome (calcinosis, Raynauds phe-
nomenon, sclerodactyly, oesophageal
involvement, telangiectasia). In one
series, the dermatological lesion was the
presenting symptom or sign leading to
the diagnosis in more than a third of
patients. The diagnosis is confirmed by
demonstration of M2 antimitochon-
drial antibodies (present in 95%
patients).
Endocrine disease
Pretibial myxoedema
This condition presents as red to skin
coloured, purple/brown or yellowish
waxy indurated plaques on the anterolat-
eral aspect of the lower legs or feet, char-
acteristically with a peau dorange
appearance. It may also manifest as a dif-
fuse non-pitting oedema. There may be
localised hypertrichosis and hyper-
hidrosis. It is due to mucin deposition,
often associated with hyperthyroidism
(Graves disease patients 1.5%, exoph-
thalmos 25%), but can appear following
treatment of thyroid disease.
Hirsutism
The growth of terminal hair (hirsutism)
in females in normally non-hairy sites
can be racial or due to:
increased production of ovarian
androgens (polycystic ovaries,
ovarian tumours)
increased production of adrenal
androgens (adrenal tumour/
hyperplasia or hyperpituitarism)
ovarian failure (postmenopausal or
post-oophorectomy)
androgenic drugs (testosterone, sys-
temic steroids, danazol).
Acne can also be androgen driven and
may coexist. Screening tests may include
plasma testosterone, sex hormone
binding globulin, prolactin, luteinising
and follicular stimulating hormone
levels, 17-hydroxyprogesterone, dehy-
droepiandrosterone sulphate and
androstenedione.
382 Royal College of Physicians, 2009. All rights reserved.
CME Dermatology
Fig 4. Vasculitic rash of
mixed cryoglobulinaemia.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 382
Metabolic disease
Fabry disease
A rare X-linked disorder of males, Fabry
disease, due to a deficiency of -galac-
tosidase A, causes deposition of glycol-
ipid in small blood vessels of the skin,
kidneys, heart and brain. Soon after
puberty, red or black telangiectatic mac-
ules and papules up to 0.5 cm in diam-
eter arise diffusely around the umbilicus
and lower trunk, over the hips, buttocks,
thighs and genitalia. Angiokeratomas of
the skin may occur in heterozygote
female carriers who are usually asympto-
matic. Periodic bouts of excruciating
burning pain in the extremities associ-
ated with fever are characteristic.
Diagnosis by skin biopsy is vital as
replacement of the missing enzyme by iv
infusion prevents life-threatening renal
failure, myocardial infarction and cere-
brovascular accident.
Xanthomatoses
Xanthomatoses are characterised by lipid
deposition in the skin due to hyperlipi-
daemia either from a primary genetic
defect or secondary to defective metabo-
lism. They may present as:
xanthelasmata: flat yellow papules
around the eyes which can occur
both in disorders of cholestasis (ie
PBC) and in normolipaemic states
eruptive xanthomata: sudden profuse
onset of yellow papules over the but-
tocks, often associated with triglyceride
excess due to uncontrolled diabetes,
alcohol excess, oestrogens or, rarely,
primary hyperlipidaemia (Fig 5)
xanthoma planum: yellow macules of
slightly palpable papules occur in the
creases of the hands and are virtually
diagnostic of type 3 familial dysbe-
talipoproteinaemia
xanthoma tendinosum: nodules over
the elbows and knees or along ten-
dons (especially the back of the
hands and Achilles tendon), often
seen in heterozygous familial hyperc-
holesterolaemia
diffuse plane xanthomata: present as
widespread yellow/orange patches,
chiefly over the trunk and sides of the
neck in normolipaemic patients.
They can be associated with disor-
ders of the reticuloendothelial
system and may precede systemic
manifestations by several years.
Therefore, careful follow-up is
advisable, with periodic laboratory
investigations to screen for lympho-
proliferative disease.
Pseudoxanthoma elasticum
A rare group of inherited disorders of
elastic and collagen fibres, pseudoxan-
thoma elasticum, manifests as yellow
papules and loose thickened skin in
the flexures, in combination with ocular
and vascular abnormalities (Fig 6).
Cracking of Bruchs membrane,
resulting in angioid streaks, should be
sought by slit-lamp examination of the
eyes. Vascular involvement can cause GI
or urinary tract haemorrhage, hyperten-
sion (through calcification of renal
arteries) and angina. A skin biopsy
demonstrates fragmentation and
clumping of elastic fibres in the mid-
and lower dermis.
Ehlers-Danlos syndrome
Ehlers-Danlos syndrome is a group of
abnormalities of collagen biosynthesis
which result in hyperextensible skin and
joints, poor wound healing, easy bruising
and occasional fragility of large blood
vessels and viscera. Skin is thin, velvety
and fragile, heals with tissue paper scars,
later becoming pendulous especially over
palms and soles. Pseudotumours (herni-
ations of fat through the dermis) are
common, particularly over knees and
elbows. Serious complications include
rupture of a large aneurysm or blood
vessel and GI perforation.
Royal College of Physicians, 2009. All rights reserved. 383
CME Dermatology
Fig 5. Eruptive
xanthomata.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 383
References
1 Cox NH, Graham RM. Systemic disease and
the skin. In: Burns DA, Breathnach SM, Cox
NH et al. (eds). Rooks textbook of derma-
tology (7th edn). Oxford: Blackwell, 2004.
2 Callen J. Dermatologic signs of systemic
diseases. In: Bologna J, Jorizzo JL, Rapini
RP (eds). Dermatology. St Louis, Mosby,
2003:7123.
3 Bratton RL, Whiteside JW, Hovan MJ,
Engle RL, Edwards FD. Diagnosis and
treatment of lyme disease. Mayo Clin Proc
2008;83:56671.
4 Lai-Cheong JE, Perez A, Tang G et al.
Cutaneous manifestations of tuberculosis.
Clin Exp Dermatol 2007;32:4616.
5 Umapathy KC, Begum R, Ravichandran G
et al. Comprehensive findings on clinical,
bacteriological, histopathological and ther-
apeutic aspects of cutaneous tuberculosis.
Trop Med Int Health 2006;11:15218.
6 Alonso-Llamazares J, Gibson LE, Rogers
RS 3rd. Clinical, pathologic, and
immunopathologic features of dermatitis
herpetiformis: review of the Mayo Clinic
experience. Int J Dermatol 2007;46:9109.
7 Koulentaki M, Ioannidou D, Stefanidou M
et al. Dermatological manifestations in
primary biliary cirrhosis patients: a case
control study. Am J Gastroenterol
2006;101:5416.
Address for correspondence: Dr S
Dhoat, Royal Free Hospital, Pond
Street, London NW3 2QG. Email:
sasha.dhoat@royalfree.nhs.uk
384 Royal College of Physicians, 2009. All rights reserved.
CME Dermatology
Fig 6. Yellow papules of pseudoxanthoma elasticum.
CMJ0904-CME.Groves.qxd 7/25/09 5:18 PM Page 384
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- ABX Common Effects of Antibiotics On Other Drugs MMDocument3 pagesABX Common Effects of Antibiotics On Other Drugs MMmicheal1960Pas encore d'évaluation
- Kid StonesDocument5 pagesKid Stonesmicheal1960Pas encore d'évaluation
- A Better Test Than HbA1c Oct 19, 2016Document5 pagesA Better Test Than HbA1c Oct 19, 2016micheal1960Pas encore d'évaluation
- Ezetimibe Simvastatin Post-Acute Coronary SyndromeDocument12 pagesEzetimibe Simvastatin Post-Acute Coronary Syndromemicheal1960Pas encore d'évaluation
- MBF2306162Document137 pagesMBF2306162DrHassan Ahmed ShaikhPas encore d'évaluation
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangPas encore d'évaluation
- Lipid Lowering With Statin Is Better Than Adding Other AgentDocument1 pageLipid Lowering With Statin Is Better Than Adding Other Agentmicheal1960Pas encore d'évaluation
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangPas encore d'évaluation
- Simple Depression Anxiety 2 Simple Screenin QuestionsDocument2 pagesSimple Depression Anxiety 2 Simple Screenin Questionsmicheal1960Pas encore d'évaluation
- New Guidelines On Nonstatin Lipid Lowering 2016-8-16Document7 pagesNew Guidelines On Nonstatin Lipid Lowering 2016-8-16micheal1960Pas encore d'évaluation
- 13 Can'T-Miss Findings On Pediatric Imaging 2015-12-2Document29 pages13 Can'T-Miss Findings On Pediatric Imaging 2015-12-2micheal1960Pas encore d'évaluation
- AKI MGMT 2005-11-1 AAFP p1739Document8 pagesAKI MGMT 2005-11-1 AAFP p1739micheal1960Pas encore d'évaluation
- Taylors.10 Minute - Diagnosis.manual - Symptoms.and - Signs.in - The.time Limited - Encounter.Document656 pagesTaylors.10 Minute - Diagnosis.manual - Symptoms.and - Signs.in - The.time Limited - Encounter.micheal1960Pas encore d'évaluation
- Serotonin SyndromeDocument5 pagesSerotonin Syndromemicheal1960Pas encore d'évaluation
- Tests Distinguish Pneumonia Types in MinutesDocument3 pagesTests Distinguish Pneumonia Types in Minutesmicheal1960100% (1)
- Iron Deficiency Anemia 2007-3-1 AAFP p671Document8 pagesIron Deficiency Anemia 2007-3-1 AAFP p671micheal1960Pas encore d'évaluation
- Low SodiumDocument4 pagesLow Sodiummicheal1960Pas encore d'évaluation
- AF & Oral Anticoagulants 2016Document11 pagesAF & Oral Anticoagulants 2016micheal1960100% (1)
- Clinical Challenge Bright Plaques, Papules On The ThumbDocument4 pagesClinical Challenge Bright Plaques, Papules On The Thumbmicheal1960Pas encore d'évaluation
- Nail Diseases, Hand in Diagnosis, Terry's NailDocument35 pagesNail Diseases, Hand in Diagnosis, Terry's Nailmicheal1960Pas encore d'évaluation
- RaynaudDocument11 pagesRaynaudmicheal1960Pas encore d'évaluation
- Cold Agglutinin Disease 2015-4-28Document9 pagesCold Agglutinin Disease 2015-4-28micheal1960Pas encore d'évaluation
- Trigeminal N Tables SummaryDocument14 pagesTrigeminal N Tables Summarymicheal1960Pas encore d'évaluation
- Anal Cancer 2016-2-9Document17 pagesAnal Cancer 2016-2-9micheal1960Pas encore d'évaluation
- Rheumatoid Arthritis 2015-6-9Document22 pagesRheumatoid Arthritis 2015-6-9micheal1960Pas encore d'évaluation
- RaynaudDocument11 pagesRaynaudmicheal1960Pas encore d'évaluation
- Prostate Cancer 2015-5-7Document27 pagesProstate Cancer 2015-5-7micheal1960Pas encore d'évaluation
- Athlete's Heart or Cardiomyopathy 2016-3-1Document2 pagesAthlete's Heart or Cardiomyopathy 2016-3-1micheal1960Pas encore d'évaluation
- Superficial Venous Insufficiency 2015-6-4Document16 pagesSuperficial Venous Insufficiency 2015-6-4micheal1960Pas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Abdominal UltrasoundDocument6 pagesAbdominal Ultrasounds0800841739100% (1)
- 6/27/2019 NO NAMA BARANG QTY UOM Batch EDDocument8 pages6/27/2019 NO NAMA BARANG QTY UOM Batch EDRedCazorlaPas encore d'évaluation
- Formulalrium PanduanDocument64 pagesFormulalrium Panduananon_939732770Pas encore d'évaluation
- End users' contact and product informationDocument3 pagesEnd users' contact and product informationمحمد ہاشمPas encore d'évaluation
- Joyetech Eroll Manual MultilanguageDocument9 pagesJoyetech Eroll Manual MultilanguagevanlilithPas encore d'évaluation
- Symposiumbooklet CareerDocument36 pagesSymposiumbooklet Careerroh009Pas encore d'évaluation
- Appsf 2007Document28 pagesAppsf 2007miangulPas encore d'évaluation
- Parallax Xray For Maxillary CanineDocument3 pagesParallax Xray For Maxillary Canineabdul samad noorPas encore d'évaluation
- Rectal Cancer Grossing Guide Optimizes Margin AssessmentDocument18 pagesRectal Cancer Grossing Guide Optimizes Margin Assessmentionut216100% (1)
- Aghamohammadi Et Al 2016 WEB OF SCIENCE Integrative Cancer TherapiesDocument9 pagesAghamohammadi Et Al 2016 WEB OF SCIENCE Integrative Cancer Therapiesemmanuelle leal capelliniPas encore d'évaluation
- Williams ObstetricsDocument2 pagesWilliams Obstetricsmely sandyPas encore d'évaluation
- Salivary GlandsDocument21 pagesSalivary GlandsHassan JaleelPas encore d'évaluation
- Cghs Rates BangaloreDocument26 pagesCghs Rates Bangaloregr_viswanathPas encore d'évaluation
- Material Safety Data Sheet: Tert-Amyl Alcohol MSDSDocument6 pagesMaterial Safety Data Sheet: Tert-Amyl Alcohol MSDSmicaziv4786Pas encore d'évaluation
- Sankar Ganguly - Pharma ManagerDocument2 pagesSankar Ganguly - Pharma Managersurojitsaha15094Pas encore d'évaluation
- AAO Glaucoma 2013 - GLA - Syllabus PDFDocument96 pagesAAO Glaucoma 2013 - GLA - Syllabus PDFrwdPas encore d'évaluation
- Neonatal Thrombocytopenia: An Overview of Etiologies and ManagementDocument21 pagesNeonatal Thrombocytopenia: An Overview of Etiologies and ManagementbidisPas encore d'évaluation
- Renal Regulation of Extracellular Fluid Potassium ConcentrationDocument32 pagesRenal Regulation of Extracellular Fluid Potassium ConcentrationDaniel AdamsPas encore d'évaluation
- AsepsisDocument6 pagesAsepsisMarcus, RN100% (5)
- Textbook of Clinical Occupational and Environmental MedicineDocument4 pagesTextbook of Clinical Occupational and Environmental MedicineAmos SiraitPas encore d'évaluation
- CAE-UOE Part1Document4 pagesCAE-UOE Part1nikitsaPas encore d'évaluation
- Resume Massage Therapist NtewDocument2 pagesResume Massage Therapist NtewPartheebanPas encore d'évaluation
- Seminar on Concepts and Foundations of RehabilitationDocument13 pagesSeminar on Concepts and Foundations of Rehabilitationamitesh_mpthPas encore d'évaluation
- Drug Study HydrocodoneDocument1 pageDrug Study HydrocodoneYlrenne DyPas encore d'évaluation
- Lab Test Results 7 2015Document3 pagesLab Test Results 7 2015Antzee Dancee0% (1)
- Sefcik Ashley Resume 2018Document1 pageSefcik Ashley Resume 2018api-394215168Pas encore d'évaluation
- IP Sterility TestingDocument6 pagesIP Sterility TestingVarghese100% (3)
- Embryology GenitalDocument53 pagesEmbryology GenitalDhonat Flash100% (1)
- About Critical Care NursingDocument7 pagesAbout Critical Care NursingaivynPas encore d'évaluation