Académique Documents
Professionnel Documents
Culture Documents
Print 16
Transféré par
Mahmoud SelimDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Print 16
Transféré par
Mahmoud SelimDroits d'auteur :
Formats disponibles
How to reverse warfarin
Index: Anticoagulation
Original article by: Michael Tam
Warfarin is an increasingly commonly used medication in Australia. It is invaluable as an oral
anticoagulant and until the oral direct antithrombin agents (e.g., ximelagatran) (1) are
released, it is the only oral medication that can provide therapeutic levels of anticoagulation.
Unfortunately, with its increased use, over-anticoagulation has become a common presentation
to the emergency department. A high INR with or without bleeding complication is not an
uncommon scenario for hospital inpatients as well (IMHO due in part due to poor warfarin
initiation and management).
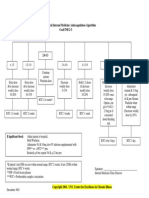
Guideline for raised INR (adapted from the consensus guidelines) (2):
Resources
Warfarin reversal: consensus guidelines, on behalf of the
Australasian Society of Thrombosis and Haemostasis
[Position Statement]
Clinical setting Action
INR higher than the
therapeutic range but <
5.0; bleeding absent
Lower the dose or omit the next dose of warfarin.
Resume therapy at a lower dose when the INR
approaches therapeutic range.
If the INR is only minimally above therapeutic
range (up to 10%), dose reduction may not be
necessary.
INR 5.09.0; bleeding
absent
Cease warfarin therapy; consider reasons for
elevated INR and patient-specific factors.
If bleeding risk is high, give vitamin K (1.02.0
mg orally or 0.51.0 mg intravenously).
Measure INR within 24 hours, resume warfarin at
a reduced dose once INR is in therapeutic range.
INR > 9.0; bleeding
absent
Where there is a low risk of bleeding, cease
warfarin therapy, give 2.55.0 mg vitamin K orally
or 1.0 mg intravenously. Measure INR in 612
hours, resume warfarin therapy at a reduced dose
once INR < 5.0.
Where there is high risk of bleeding, cease
warfarin therapy, give 1.0 mg vitamin K1
Page 1of 5
Prevention: reduce the risk of high INR
The best way to avoid warfarin reversal is to try to prevent the scenarios that lead to a high
INR. The following should be considered:
As per my article on how to start warfarin therapy avoid loading doses of warfarin and
initiation schemes designed to reach an INR of 2.0 as quickly as possible for discharge; it
is a sure fire recipe for a high INR one to two weeks post discharge in the community (3).
Patience is importance unless there is a very good reason, INR need only be tested no
more than once a week and each dosage change should be small and well considered.
Continuing patient education is important.
Ensure medication compliance before increasing the dose.
Aim for an INR of 2.5 (the therapeutic range for most conditions is between 2.0 and 3.0
and for mechanical heart valves 2.5 to 3.5 either way, aiming for 2.5 covers both
bases).
There has recently been some discussion about low-intensity warfarin therapy with a target INR
of 1.5 to 2.0. However, the Extended Low-Intensity Anticoagulation for Thrombo-Embolism
Investigators found in 2003 that low-intensity warfarinisation was not as good as standard
warfarinisation and did not reduce the rate of bleeding complications (4). As such this practice
cannot be recommended.
What to do for INR < 3.5
The increased risk of bleeding is around twice that of an INR from 2.0-3.0. Keep this in
intravenously. Consider Prothrombinex-HT (2550
IU/kg) and fresh frozen plasma (150300 mL),
measure INR in 612 hours, resume warfarin
therapy at a reduced dose once INR < 5.0.
Any clinically significant
bleeding where warfarin-
induced coagulopathy is
considered a contributing
factor
Cease warfarin therapy, give 5.010.0 mg vitamin
K intravenously, as well as Prothrombinex-HT (25
50 IU/kg) and fresh frozen plasma (150300 mL),
assess patient continuously until INR < 5.0, and
bleeding stops.
or
If fresh frozen plasma is unavailable, cease
warfarin therapy, give 5.010.0 mg vitamin K
intravenously, and Prothrombinex-HT (2550
IU/kg), assess patient continuously until INR <
5.0, and bleeding stops.
or
If Prothrombinex-HT is unavailable, cease warfarin
therapy, give 5.010.0 mg vitamin K
intravenously, and 1015 mL/kg of fresh frozen
plasma, assess patient continuously until INR <
5.0, and bleeding stops.
Page 2of 5
perspective. If there is a 1% per annum risk of serious bleed, an INR of 3.5 means
approximately 2% per annum risk; or a miniscule risk that they will have a serious bleed within
the next week.
What you will do somewhat depends on the scenario.
If someones INR is known to fluctuate up and down but has otherwise been fairly stable
on a particular dose, then it would not be unreasonable to keep them on the current dose
and repeat the INR in a week.
Similarly, if there is a good reason for the increase (e.g., commencement of a short
course of oral antibiotics), then there is no particular reason to change the existing dose.
If it appears that the raised INR is likely to remain raised on their current maintenance
dose of warfarin, then it would be reasonable to reduce the regular dose to what is
estimated to be the correct dose (example, approximately a 10-20% dose reduction) and
then recheck the INR in 1-2 weeks.
Avoid the (IMHO, bad) practice of withholding doses at this INR range.
What to do for INR 3.5 5.0
The risk of bleeding is up to quadrupled from an INR of 2.0-3.0. Again keep this in perspective.
The absolute risk of a serious bleed in the next few days to week when you will be managing it
is very low if the patient doesnt have risk factors.
Consider precipitating factors, e.g., drug interactions, medication compliance issues. If
the INR of 5.0 was unexpected, then it may be reasonable to repeat the INR daily for the
next few days to monitor the trend.
If the patient is otherwise relatively stable, reduce the dose to what would be expected to
be the correct dose (approximately 20% dose reduction) and check again in a week.
For some patients who may have higher risk, it is reasonable to repeat the INR on a daily
basis and withholding warfarin until the INR falls to below 3.5. At that time, restart at
what is estimated as the appropriate dose.
What to do for INR 5.0 9.0
The risk of acute bleeding is now raised significantly enough that warfarin should be ceased
immediately. The cause of the raised INR should be carefully considered.
I would advise daily INRs and restarting warfarin once the INR is below 3.5. The dose
chosen should be the estimated maintenance dose.
Try to avoid the inevitable INR undershoot by restarting warfarin sooner rather than
later once the INR trend is clearly downwards.
If bleeding risk is high, give a low dose of vitamin K:
1-2 mg orally or;
0.5-1.0 mg intravenously.
Avoid high doses of vitamin K as it results in resistance during re-warfarinisation. Even
a small dose intravenously often leads to completely reversal.
If INR is sub-therapeutic after reversal, then remember to provide alternate forms of
anticoagulation (e.g., with low molecular weight heparin) if indicated.
What to do for INR > 9.0
Page 3of 5
There is marked increased risk for acute bleeding at this level.
Again, consider why the INR is raised.
Immediately cease warfarin therapy.
Where bleeding risk is low, give vitamin K:
2.5-5.0 mg orally or;
1 mg intravenously.
Where bleeding risk is high:
vitamin K 1 mg intravenously or;
Prothrombinex 25-50 units/kg intravenously or;
fresh frozen plasma (FFP) 150-300 mL (1 unit) intravenously.
Check the INR in 6 hours and monitor with daily INRs for the next few days.
Restart warfarin at the estimated appropriate dose for maintenance when the INR < 5.0.
How to give intravenous vitamin K
In the hospitals I worked in, phytomenadione (vitamin K) (Konakion) tablets were simply not
stocked. However, intravenous vitamin K is almost universally available.
Be aware that intravenous vitamin K (also Konakion) comes in both paediatric (2 mg/0.2 mL)
and adult (10 mg/1 mL) sizes.
Firstly, insert an intravenous cannula, preferable 21 gauge or larger. Make sure that the line is
patent by giving it a flush with sterile saline.
Secondly, ensure that resuscitation equipment is available as intravenous vitamin K can
provoke anaphylactic reactions.
Now, the usual dose for intravenous vitamin K is 1 mg, or 0.1 mL. That is impossible to infuse
slowly. So:
Afterwards, flush with 5-10 mL of saline again, slowly over 30-60 seconds. For larger doses of
vitamin K, infuse the appropriate amount. When diluted up to 10 mL, the concentration of
vitamin K is 1 mg/mL.
The INR should always be checked after 6 hours to ensure adequate reversal of anticoagulation.
Reference articles
(1) Brighton TA. The direct thrombin inhibitor melagatran/ximelagatran. MJA 2004; 181: 432
437 [download PDF :: 344 Kb]
Draw 10 mg (1 mL) of vitamin K into a 10 mL syringe
Then draw up sterile 0.9% NaCl solution into the syringe to make
up 10 mL
Slowly infuse 1 mg (1 mL) of the diluted solution through the
cannula over 30-60 seconds
Page 4of 5
(2) Baker RI., Coughlin PB., Gallus AS., et al.; the Warfarin Reversal Consensus Group.
Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis
and Haemostasis [Position Statement]. MJA 2004; 181 (9): 492-497 [download PDF :: 183 Kb]
(3) Tam M. How to start warfarin therapy [electronic article]. The Medicine Box. Last updated
20 July 2006. [Link]
(4) Kearon C., Ginsberg JS., Kovacs MJ., et al.; Extended Low-Intensity Anticoagulation for
Thrombo-Embolism Investigators. Comparison of low-intensity warfarin therapy with
conventional-intensity warfarin therapy for long-term prevention of recurrent venous
thromboembolism. New England Journal of Medicine. 349(7):631-9, 2003 Aug 14 [download
PDF :: 910 Kb]
Please read the disclaimer
Page 5of 5
Vous aimerez peut-être aussi
- Heparin Drip ProtocolDocument16 pagesHeparin Drip Protocolapi-277534147100% (1)
- Mini Warfarin GuidelinesDocument2 pagesMini Warfarin GuidelinesPeunn NattaphatPas encore d'évaluation
- JMO Solutions 2008Document4 pagesJMO Solutions 2008ichkhuyPas encore d'évaluation
- Coumadin Dosing GuideDocument3 pagesCoumadin Dosing Guidemorale28Pas encore d'évaluation
- Surgical Finals Passing The Clinical PDFDocument40 pagesSurgical Finals Passing The Clinical PDFnetradeep67% (3)
- LTE 3GPP Band13 Test Entrance CriteriaDocument130 pagesLTE 3GPP Band13 Test Entrance CriteriaBuchi Reddy0% (1)
- Rightship Ship Inspection Questionnaire RISQDocument177 pagesRightship Ship Inspection Questionnaire RISQИгорь100% (3)
- Warfarin NOTESDocument8 pagesWarfarin NOTESSarah :-)Pas encore d'évaluation
- AntidotesDocument36 pagesAntidotesMohamed Haggag100% (1)
- GP 24-21 - Fire Hazard AnalysisDocument53 pagesGP 24-21 - Fire Hazard AnalysisJohn DryPas encore d'évaluation
- Drugs To Watch With WARFARINDocument3 pagesDrugs To Watch With WARFARINRajendra RaiPas encore d'évaluation
- MRCS Essential ListDocument18 pagesMRCS Essential ListMahmoud Selim100% (1)
- Warfarin Therapy Management: ScopeDocument9 pagesWarfarin Therapy Management: ScopesastiraPas encore d'évaluation
- Post Test MS RleDocument15 pagesPost Test MS RleAngel YN Patricio FlorentinoPas encore d'évaluation
- Microscopio Olympus CX31 Serv PDFDocument36 pagesMicroscopio Olympus CX31 Serv PDFalejandra0% (1)
- Overdose and PoisoningDocument4 pagesOverdose and PoisoningMahmoud SelimPas encore d'évaluation
- Warfarin GuidelinesDocument9 pagesWarfarin Guidelinesmarto langPas encore d'évaluation
- Vit KguidelinesDocument2 pagesVit KguidelinesMayer Rosenberg100% (1)
- JajajaDocument1 pageJajajaFian AldyPas encore d'évaluation
- Warfarin Therapy in MalaysiaDocument34 pagesWarfarin Therapy in MalaysiaDaniel RajPas encore d'évaluation
- dietary DI Warfarin Clinical Practice Guideline Care Process ModelDocument12 pagesdietary DI Warfarin Clinical Practice Guideline Care Process Modeltl drPas encore d'évaluation
- A NTICOAGULANTDocument48 pagesA NTICOAGULANTSharliza S100% (1)
- UHS Anticoagulation Therapy Guideline Y12 04Document7 pagesUHS Anticoagulation Therapy Guideline Y12 04staylor235Pas encore d'évaluation
- Anticoagulant Pocket GuideDocument8 pagesAnticoagulant Pocket GuideDrew John Minardi100% (2)
- CH 26 Evolve QuestionsDocument4 pagesCH 26 Evolve QuestionsjoannePas encore d'évaluation
- How To Start Warfarin TherapyDocument4 pagesHow To Start Warfarin TherapyMahmoud SelimPas encore d'évaluation
- Vitamin K Antagonists: American College of Pharmacology and Management of TheDocument41 pagesVitamin K Antagonists: American College of Pharmacology and Management of TheCatalina VallejoPas encore d'évaluation
- Appendix B: Phytonadione (Vitamin K) Dosing GuidelinesDocument2 pagesAppendix B: Phytonadione (Vitamin K) Dosing GuidelinesWill TohallinoPas encore d'évaluation
- Deep Vein ThrombosisDocument4 pagesDeep Vein ThrombosisStefania CristinaPas encore d'évaluation
- Chest Guidelines - WarfarinDocument41 pagesChest Guidelines - Warfarinkedaw100% (1)
- Anticoagulation Workshop 7-8 August 2010: Case StudiesDocument11 pagesAnticoagulation Workshop 7-8 August 2010: Case Studieskhangsiean89Pas encore d'évaluation
- Nclex 3 With RationaleDocument13 pagesNclex 3 With RationaleMsPocketbook HoarderPas encore d'évaluation
- Procoagulantes Guias PDFDocument30 pagesProcoagulantes Guias PDFtsntbPas encore d'évaluation
- Anticoagulation Protocol For PostDocument8 pagesAnticoagulation Protocol For PostMohammed IbrahimPas encore d'évaluation
- Guideline On The Management of Bleeding in Patients On Antithrombotic Agents.Document10 pagesGuideline On The Management of Bleeding in Patients On Antithrombotic Agents.Madalina TalpauPas encore d'évaluation
- Agatha Christie - Craciunul Lui PoirotDocument14 pagesAgatha Christie - Craciunul Lui PoirotIokan DanPas encore d'évaluation
- Warfarin Therapy - Evolving Strategies in AnticoagulationDocument10 pagesWarfarin Therapy - Evolving Strategies in AnticoagulationarbetaPas encore d'évaluation
- Warfarin Dosing ProtocolDocument2 pagesWarfarin Dosing Protocolkiondoon100% (1)
- Drug Interactions: Warfarin and Antiplatelet DrugsDocument4 pagesDrug Interactions: Warfarin and Antiplatelet DrugsAyesha AhmadPas encore d'évaluation
- Hydralazine For Severe PIHDocument4 pagesHydralazine For Severe PIHYwagar YwagarPas encore d'évaluation
- Ambulatory 2 RadDocument58 pagesAmbulatory 2 RadAlaa ElsisiPas encore d'évaluation
- UNC General Internal Medicine Anticoagulation Algorithm Goal INR 2-3Document1 pageUNC General Internal Medicine Anticoagulation Algorithm Goal INR 2-3Fajar NugrahaPas encore d'évaluation
- Chest Suppl 22sDocument17 pagesChest Suppl 22sMoisés PoncePas encore d'évaluation
- Deep Vein ThrombosisDocument5 pagesDeep Vein ThrombosisSiva Malar GanasenPas encore d'évaluation
- Anticoagulation Related Bleeding - Guideline Summary: Click On The Appropriate Link BelowDocument19 pagesAnticoagulation Related Bleeding - Guideline Summary: Click On The Appropriate Link BelowIrenePas encore d'évaluation
- Dosing and Administration Guide: IndicationDocument12 pagesDosing and Administration Guide: IndicationenggajbPas encore d'évaluation
- Anticoag GuidelinesDocument22 pagesAnticoag Guidelinesyusuf100% (1)
- Case Consult Paper 1Document3 pagesCase Consult Paper 1api-665600383Pas encore d'évaluation
- Name of The Medicinal Product: Prescribing Information Coumadin TabletsDocument13 pagesName of The Medicinal Product: Prescribing Information Coumadin Tabletsddandan_2Pas encore d'évaluation
- Hemostan, Methergine CA Gluconate2Document4 pagesHemostan, Methergine CA Gluconate2Stacy MC PelitoPas encore d'évaluation
- WarfarinDocument4 pagesWarfarinekramPas encore d'évaluation
- Vitamin K1: Dosage Forms & StrengthsDocument4 pagesVitamin K1: Dosage Forms & StrengthsErnesto Fer FdezPas encore d'évaluation
- Dokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedDocument54 pagesDokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedMahmoud FathyPas encore d'évaluation
- NCLEX Practice QuestionsDocument12 pagesNCLEX Practice QuestionsDane WrightPas encore d'évaluation
- How Would You Manage A Patient Who Was Taking WarfarinDocument6 pagesHow Would You Manage A Patient Who Was Taking WarfarinKen KwongPas encore d'évaluation
- Anx 124974 enDocument87 pagesAnx 124974 encuba11Pas encore d'évaluation
- Annex I Summary of Product CharacteristicsDocument182 pagesAnnex I Summary of Product Characteristicsadrip234Pas encore d'évaluation
- KC Journal 04 2015Document20 pagesKC Journal 04 2015Delly Dellima RPas encore d'évaluation
- DVT TreatmentDocument24 pagesDVT TreatmentphoechoexPas encore d'évaluation
- MIL Vol 5 No 8 (Initiating Oral Anticoagulation)Document3 pagesMIL Vol 5 No 8 (Initiating Oral Anticoagulation)garywall.ukPas encore d'évaluation
- Hypertension Management of Acute 51118Document10 pagesHypertension Management of Acute 51118MuathPas encore d'évaluation
- Current Cardiovascular Therapy Pharmacological-229-246Document18 pagesCurrent Cardiovascular Therapy Pharmacological-229-246Yulian 53Pas encore d'évaluation
- Labetalol GuodlinesDocument6 pagesLabetalol GuodlinesSundusPas encore d'évaluation
- LMWH QML 06Document7 pagesLMWH QML 06pd7qmlPas encore d'évaluation
- Oral Anticoagulants 2001Document14 pagesOral Anticoagulants 2001Napoleon Gonzalez GilPas encore d'évaluation
- Suture TypesDocument2 pagesSuture TypesMahmoud SelimPas encore d'évaluation
- Factors Associated With The High Cost of Liver Transplantation in AdultsDocument10 pagesFactors Associated With The High Cost of Liver Transplantation in AdultsMahmoud SelimPas encore d'évaluation
- Left Versus Right Lobe Liver Donation: EditorialDocument2 pagesLeft Versus Right Lobe Liver Donation: EditorialMahmoud SelimPas encore d'évaluation
- How To Start Warfarin TherapyDocument4 pagesHow To Start Warfarin TherapyMahmoud SelimPas encore d'évaluation
- "Maintenance" IV Fluids in Euvolaemic Adults: Intravenous Fluid Therapy Michael TamDocument4 pages"Maintenance" IV Fluids in Euvolaemic Adults: Intravenous Fluid Therapy Michael TamMahmoud SelimPas encore d'évaluation
- How To Stop Warfarin For Surgery: Low Thromboembolic RiskDocument3 pagesHow To Stop Warfarin For Surgery: Low Thromboembolic RiskMahmoud SelimPas encore d'évaluation
- Print 18Document4 pagesPrint 18Mahmoud SelimPas encore d'évaluation
- Donor Liver Steatosis and Graft Selection For Liver Transplantation: A Short ReviewDocument3 pagesDonor Liver Steatosis and Graft Selection For Liver Transplantation: A Short ReviewMahmoud SelimPas encore d'évaluation
- How To Reverse Low Molecular Weight HeparinDocument2 pagesHow To Reverse Low Molecular Weight HeparinMahmoud SelimPas encore d'évaluation
- Clinical Features of Serotonin SyndromeDocument2 pagesClinical Features of Serotonin SyndromeMahmoud SelimPas encore d'évaluation
- Clin Diabetes 2001 Plodkowski 92 5Document4 pagesClin Diabetes 2001 Plodkowski 92 5Mahmoud SelimPas encore d'évaluation
- ASTS Recommended Practice Guidelines For Controlled Donation After Cardiac Death Organ Procurement and TransplantationDocument8 pagesASTS Recommended Practice Guidelines For Controlled Donation After Cardiac Death Organ Procurement and TransplantationMahmoud SelimPas encore d'évaluation
- Family MedicineDocument194 pagesFamily Medicineapi-3712326100% (2)
- Design and Management of Mettur Dam by Predicting Seepage Losses Using Remote SensingDocument10 pagesDesign and Management of Mettur Dam by Predicting Seepage Losses Using Remote SensingInternational Journal of Application or Innovation in Engineering & ManagementPas encore d'évaluation
- Learning Guide: Central Texas College Department of NursingDocument26 pagesLearning Guide: Central Texas College Department of Nursingapi-3697326Pas encore d'évaluation
- Suez Canal ReportDocument5 pagesSuez Canal ReportAnonymous Pc6LwfCPas encore d'évaluation
- Ficha-Tecnica-Tuberia MechDocument2 pagesFicha-Tecnica-Tuberia MechCarlos salazarPas encore d'évaluation
- Hydrostatic, Deviatoric StressesDocument7 pagesHydrostatic, Deviatoric StressespanbuPas encore d'évaluation
- A Duality Principle For The Entanglement Entropy of Free Fermion SystemsDocument12 pagesA Duality Principle For The Entanglement Entropy of Free Fermion SystemsCroco AliPas encore d'évaluation
- Baldor Motor TestDocument14 pagesBaldor Motor TestChecho BuenaventuraPas encore d'évaluation
- Smart Dust Technology Seminar ReportDocument32 pagesSmart Dust Technology Seminar ReportSushan Upadhyay67% (3)
- Servo Controlled FBW With Power Boost Control, Operations & Maint. ManualDocument126 pagesServo Controlled FBW With Power Boost Control, Operations & Maint. ManualKota NatarajanPas encore d'évaluation
- Dumel James Melchor DuayDocument3 pagesDumel James Melchor DuayBle DuayPas encore d'évaluation
- Module 5: Safety and Health at Work: Participant's HandbookDocument24 pagesModule 5: Safety and Health at Work: Participant's HandbookChristian Surio RamosPas encore d'évaluation
- Local AnesthesiaDocument55 pagesLocal AnesthesiaAhmed MagdyPas encore d'évaluation
- Long Quiz 1 Eim Tools, MaterialsDocument1 pageLong Quiz 1 Eim Tools, MaterialsLea Ann PalaciosPas encore d'évaluation
- Density-Based Methods: DBSCAN: Density-Based Clustering Based On Connected Regions With High DensityDocument3 pagesDensity-Based Methods: DBSCAN: Density-Based Clustering Based On Connected Regions With High DensityKingzlynPas encore d'évaluation
- Research Proposal PHDDocument19 pagesResearch Proposal PHDSuleiman Mukhtar100% (2)
- IJETR022563Document5 pagesIJETR022563erpublicationPas encore d'évaluation
- Genesis of KupferschieferDocument15 pagesGenesis of KupferschieferMaricela GarciaPas encore d'évaluation
- The DSG DQ200 LifespanDocument1 pageThe DSG DQ200 Lifespanqt99qzyhrbPas encore d'évaluation
- NMMT City Bus SystemDocument3 pagesNMMT City Bus Systemharish guptaPas encore d'évaluation
- Appetizer Summative TestDocument36 pagesAppetizer Summative TestArgelynPadolinaPedernalPas encore d'évaluation
- Band Structure Engineering in Gallium Sulfde NanostructuresDocument9 pagesBand Structure Engineering in Gallium Sulfde NanostructuresucimolfettaPas encore d'évaluation
- (WWW - Asianovel.com) - Quan Zhi Gao Shou Chapter 051 - Chapter 100Document310 pages(WWW - Asianovel.com) - Quan Zhi Gao Shou Chapter 051 - Chapter 100Exile0105Pas encore d'évaluation
- The Online Math Open Fall Contest December 4-15, 2020Document8 pagesThe Online Math Open Fall Contest December 4-15, 2020Raghav GoelPas encore d'évaluation
- National Railway Museum Annual Review 04-05Document40 pagesNational Railway Museum Annual Review 04-05sol.loredo1705530Pas encore d'évaluation
- The Six Types of Simple MachinesDocument4 pagesThe Six Types of Simple MachinesmarroPas encore d'évaluation