Académique Documents
Professionnel Documents
Culture Documents
Case Study Presentation - Spring 2013
Transféré par
api-252001755Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Case Study Presentation - Spring 2013
Transféré par
api-252001755Droits d'auteur :
Formats disponibles
PULMONARY
FIBROSIS
OBJECTIVES
Understand the basic pathophysiology of pulmonary
fibrosis
Identify presenting symptoms of the disease
Know what diagnostic tests are performed to confirm
the diagnosis
Discuss some of the treatment options
PATHOPHYSIOLOG
Y
Excess scar tissue build
up in the lungs
Decreases the ability of
the lungs to expand
Causes less oxygen to
be exchanged in the
lungs
Leads to hypoventilation
and hypercapnia
(Huether, 2012)
VIDEO
http://www.youtube.com/watch?v=Gh2Ovh0uAss
PRESENTING SYMPTOMS
Dyspnea on exertion
Diffuse inspiratory crackles
Cough
Hypoxemia
At rest and worsens with activity
Clubbing
Chronic hypoxemia as the disease progresses
(King, 2011)
PREVELANCE
Usually seen in middle-aged to elderly adults
Range 55-75 years old
2/3 of people diagnosed are over 60 (Rafii, 2013)
13-20/100,000
Men are diagnosed more often than women
(King, 2011)
DIAGNOSITC TESTS
CT
PFT
CXR
Lung biopsy
(King, 2011)
RISK FACTORS
Smoking
Exposure to metal and wood dust
Taking amiodarone
Genetic link
Only in 0.5-3.5% of cases
Hx of pulmonary diseases
Acute respiratory distress syndrome, TB, sarcoidosis,
rheumatoid arthritis
(King, 2011)
TREATMENT
No current cure
Oxygen
Corticosteroids
Cytotoxic drugs
Clinical trials in progress
Lung transplant
Only treatment that prolongs life in patients with pulmonary
fibrosis
Most die waiting for transplant
Should be referred at diagnosis for best chances of receiving
lung transplant
(King, 2011)
SURVIVAL RATE
Average survival rate is around 3-5 years after
diagnosis
Prognosis is worse with
Hx of smoking
Age >70
Low BMI
Pulmonary hypertension
(King, 2011)
PATIENT SCENARIO- HPI
The patient is a 76 year-old white male who came into
the ER complaining of shortness of breath during
minimal activity and a persistent cough. Noticed
increasing difficulty breathing for past 3 months.
Relaxing with no activity decreases symptoms. On
assessment auscultated diffuse crackles in the lungs
LABS/TESTS
Patient had CT scan and lung biopsy
Both indicated pulmonary fibrosis
Doctor ordered PFT to determine current respiratory
function and to track the progress of the disease in the
future
NURSING DIAGNOSES
Impaired gas exchange r/t excess scar tissue in the
lungs secondary to pulmonary fibrosis aeb shortness of
breath with exertion
Activity intolerance r/t imbalance between oxygen
supply/demand aeb patient inability to walk short
distances
Powerlessness r/t effects of illness and oncoming death
aeb no motivation in activities or events
NCLEX QUESTION #1
Which of the following diagnostic
tests is required to make the final
diagnosis?
A. PFT
B. CXR
C. ABG
D. CT
NCLEX QUESTION #2
Which of the following is not a
presenting symptom of pulmonary
fibrosis?
A. dyspnea on exertion
B. chest pain
C. cough
D. diffuse crackles
REFERENCES
Ackley, B. J., Ladwig, G. B. (2011). Nursing diagnosis handbook. St.
Louis, MO. Mosby, Inc.
Huether, S. E., & McCance, K. L. (2012).Understanding
Pathophysiology (5th ed.). St. Louis, MO: Mosby. ISBN: 978-
0-323-07891-7
King, T. E., Pardo, A., & Selman, M. (2011). Idiopathic pulmonary
fibrosis. The Lancet, 378(9087). Retrieved from http://
www.sciencedirect.com.ezproxy.lib.usf.edu/
science/article/pii/S0140673611600524
Rafii, R., Juarez, M. M., Albertson, T. E., & Chan, A. L. (2013). A
review of current and novel therapies for idiopathic pulmonary
fibrosis. Journal of Thoracic Disease, 5. Retrieved from http://
www.ncbi.nlm.nih.gov/pmc/articles/PMC3548009/
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Bronchiolitis PDFDocument7 pagesBronchiolitis PDFYoerizta RatuPas encore d'évaluation
- Care of The DyingDocument4 pagesCare of The Dyingprokuno89% (9)
- Manual Muscle TestingDocument29 pagesManual Muscle Testingcreat1Pas encore d'évaluation
- Are Traditional Midwives History ? පාරම්පරික වින්නඹු මාතාවන් ඉතිහාසයට එක්වේ ද? பாரம்பாpய மருத்துவ மாதா;கள் வரலாற்றில் இடம்பெறுவார்களா?Document98 pagesAre Traditional Midwives History ? පාරම්පරික වින්නඹු මාතාවන් ඉතිහාසයට එක්වේ ද? பாரம்பாpய மருத்துவ மாதா;கள் வரலாற்றில் இடம்பெறுவார்களா?wmcsrilanka100% (1)
- Nursing Care Plans All PresentationsDocument23 pagesNursing Care Plans All PresentationsKaren Joyce Costales Magtanong100% (3)
- Jurisprudence RevDocument48 pagesJurisprudence RevJoel JosePas encore d'évaluation
- Fundamentals of NursingDocument18 pagesFundamentals of NursingFreeNursingNotes78% (9)
- 9 The Post Anesthesia Care UnitDocument77 pages9 The Post Anesthesia Care Unitsanjivdas100% (1)
- Initial Nurse Patient InteractionDocument1 pageInitial Nurse Patient InteractionBryan Jay Carlo PañaPas encore d'évaluation
- Animal and Insect Bites DiseasesDocument28 pagesAnimal and Insect Bites DiseasesAditya PrabawaPas encore d'évaluation
- NRP CertificationDocument1 pageNRP Certificationapi-252001755Pas encore d'évaluation
- Kimberly Cremerius: ObjectiveDocument3 pagesKimberly Cremerius: Objectiveapi-252001755Pas encore d'évaluation
- Pat 2Document18 pagesPat 2api-252001755Pas encore d'évaluation
- Pat 2Document18 pagesPat 2api-252001755Pas encore d'évaluation
- CertificateDocument1 pageCertificateapi-252001755Pas encore d'évaluation
- Clinical ExemplarDocument4 pagesClinical Exemplarapi-252001755Pas encore d'évaluation
- Discharge Planning PaperDocument4 pagesDischarge Planning Paperapi-252001755100% (1)
- Synthesis Paper SummativeDocument11 pagesSynthesis Paper Summativeapi-252001755Pas encore d'évaluation
- Pharmacovigilance AssignmentDocument11 pagesPharmacovigilance Assignmentchandru sahanaPas encore d'évaluation
- The Global Nursing Shortage: An Overview of Issues and ActionsDocument6 pagesThe Global Nursing Shortage: An Overview of Issues and ActionsChristina Yolanda Putri EklesiaPas encore d'évaluation
- Disorders of Acid Base BalanceDocument1 pageDisorders of Acid Base BalanceLyn Domingo EllaquezPas encore d'évaluation
- Generalization & SpecializatiionmDocument6 pagesGeneralization & SpecializatiionmJennifer DixonPas encore d'évaluation
- Miliue Therapy Skill PDFDocument1 pageMiliue Therapy Skill PDFRosalinda SalvadorPas encore d'évaluation
- NCP NutritionDocument3 pagesNCP NutritionSol GregorioPas encore d'évaluation
- Communication Boards in Critical CareDocument9 pagesCommunication Boards in Critical CareSeresolPas encore d'évaluation
- Aree Di LindauerDocument4 pagesAree Di LindauerGianluca PinzarronePas encore d'évaluation
- Appendix Anatomy: SURGERY 2 - G.I. ModuleDocument2 pagesAppendix Anatomy: SURGERY 2 - G.I. ModuleFrances Isabella OlasimanPas encore d'évaluation
- Developmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsDocument71 pagesDevelopmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsvadimmadanPas encore d'évaluation
- Communication and Ethics in Pharmacy Practice: What Is To BeDocument23 pagesCommunication and Ethics in Pharmacy Practice: What Is To BeMuhammad RezaPas encore d'évaluation
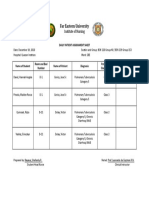
- Daily Patient Assignment SheetDocument1 pageDaily Patient Assignment SheetSheferely BayauaPas encore d'évaluation
- Paolo ManasanDocument5 pagesPaolo ManasanPaolo ManasanPas encore d'évaluation
- ADCHEM Percentage StohsDocument18 pagesADCHEM Percentage StohsMelvin CabonegroPas encore d'évaluation
- DR - Gold Created by SiraDocument26 pagesDR - Gold Created by SiraMohamed ElhabetPas encore d'évaluation
- Piperacillin MHRADocument46 pagesPiperacillin MHRAVaradha Raja PerumalPas encore d'évaluation
- Porcelain Fused To Metal (PFM) Crowns and Caries in Adjacent TeetDocument5 pagesPorcelain Fused To Metal (PFM) Crowns and Caries in Adjacent Teetbaiq rengganis dewiPas encore d'évaluation
- November 24, 2017 Strathmore TimesDocument32 pagesNovember 24, 2017 Strathmore TimesStrathmore TimesPas encore d'évaluation
- Acne HistoryDocument6 pagesAcne HistoryCristina SimaPas encore d'évaluation
- Chest Trauma: Dr. Sri Indah Aruminingsih, SP - RadDocument110 pagesChest Trauma: Dr. Sri Indah Aruminingsih, SP - Radvina zulfianiPas encore d'évaluation