Académique Documents
Professionnel Documents
Culture Documents
Pour Guideline
Transféré par
api-2456727840 évaluation0% ont trouvé ce document utile (0 vote)
106 vues4 pagesTitre original
pour guideline
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
106 vues4 pagesPour Guideline
Transféré par
api-245672784Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
Voiding Algorithm for
Preventing Postoperative Urinary Retention (POUR)
in Phase II Patients
Related Policies and Procedures:
Insertion, Removal and Care of an Indwelling Foley Catheter
Pediatric Post Anesthesia Care
Post Anesthesia Care
Bladder Scan Use in the Post Anesthesia Care Units
Approved By:
Owner: Perioperative Quality and Patient Safety Council
Submitted by: Raelyn Nicholson, RN, BSN, PCCN
Date updated/reviewed: 6/10/2014
Perioperative Guideline Task Force review date: (PGTF will review every two
years following PPPPC)
Purpose:
The purpose of this unit based guideline (UBG) is to provide the post anesthesia nurse
with clear and concise direction on preventing postoperative urinary retention (POUR) in
patients being discharged the day of surgery by utilizing an evidence based algorithm.
Sources:
Baldini, G., Bagry, H., Aprikian, A., & Carli, F. (2009). Postoperative urinary retention:
anesthetic and perioperative considerations. Anesthesiology, 110(5), 1139-1157. (Level
I)
Beatty, A.M., Martin, D.E., Couch, M., & Long, N. (1997). Relevance of oral intake an
necessity to void as ambulatory surgical discharge criteria. Journal of PeriAnesthesia
Nursing, 12(6), 413-421. (Level VI)
Buchko, B.L. & Robinson, L.E. (2012). An evidence-based approach to decrease early
post-operative urinary retention following urogynecologic surgery. Urologic Nursing,
32(5), 260-273. (Level VI)
Buchko, B.L., Robinson, L.E., & Bell, T.D. (2013). Translating an evidence-based
algorithm to decrease early post-operative urinary retention after urogynecologic surgery.
Urologic Nursing, 33(1), 24-32. doi: 10.7257/1053-816X2013.33.1.24 (Level VI)
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
DiBlasi, S.M. (2013). Planned cesarean delivery and urinary retention associated with
spinal morphine. Journal of PeriAnesthesia Nursing, 28(3), 128-135. doi:
10.1016/jopan.2012.07.012 (Level III)
Dreijer, B., Moller, M.H., & Bartholdy, J. (2011). Post-operative urinary retention in a
general surgical population. European Journal of Anaesthesiology, 28(3), 190-194. doi:
10.1097/EJA.0b013e328341ac3b (Level IV)
Hansen, B.S., Soreide, E., Warland, A.M., & Nilsen, O.B. (2011). Risk factors of post-
operative urinary retention in hospitalised patients. Acta Anaesthesiologica Scandinavica,
55, 545-548. doi: 10.1111/j.1399-6576.2011.02416.x (Level IV)
Feliciano, T., Montero, J., McCarthy, M., & Priester, M. (2008). A retrospective,
descriptive, exploratory study evaluating incidence of postoperative urinary retention
after spinal anesthesia and its effect on PACU discharge. Journal of PeriAnesthesia
Nursing, 23(6), 394-400. doi: 10.1016/j.jopan.2008.09.006 (Level VI)
McLeod, L., Southerland, K., & Bond, J. (2013). A clinical audit of postoperative urinary
retention in the postanesthesia care unit. Journal of PeriAnesthesia Nursing, 28(4), 210-
216. doi: 10.1016/j.jopan.2013.10.0006 (Level VII)
Warner, A.J., Phillips, S., Riske, K., Haubert, M., & Lash, N. (2000). Postoperative
bladder distension: Measurement with bladder ultrasonography. Journal of
PeriAnesthesia Nursing, 15(1), 20-25. (Level VII)
Definitions:
PACU- Post Anesthesia Care Unit
POUR - Postoperative Urinary Retention
Phase II Patient - Patient going home the day of surgery who meets post anesthesia
discharge criteria
Guideline
A. Definition: Postoperative urinary retention (POUR) is defined as a bladder
volume greater than 400 ml and the inability to void.
B. Signs and symptoms: restlessness, confusion, anxiety, hypertension, tachycardia
or bradycardia, and tachypnea. The patient may also be asymptomatic.
C. Risk factors for POUR:
1) Spinal Blocks
a. Depresses the ability to sense bladder fullness and lack of
voluntary muscle coordination to consciously initiate voiding.
Once the dermatome is L5 or lower, detrusor contractions return,
meaning patient
should be able to void.
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
2) Gynecologic, urologic, rectal (i.e. hemorrhoidectomies), and pelvic
procedures (i.e. inguinal hernia repairs).
a. The local anesthetics in these procedures can cause a lack of
voluntary muscle coordination to consciously initiate voiding.
These procedures also have the potential to inflame the perineum,
obstructing the urethra or damaging nerves that innervate the
bladder
3) Medications:
a. Opioids decrease the urge sensation, which increases bladder
capacity.
b. Anticholinergics (glycopyrrolate, atropine, ditropan) block
detrusor contractions causing bladder hypotonia
c. Sympathomimetics increase urethral resistance.
d. Beta blockers reduce sphincter tone; blocking that may cause
retention
4) Length of procedure greater than 60 minutes.
5) Intraoperative fluid greater than 1000 ml.
6) History of benign prostatic hyperplasia (BPH) and/or urinary retention.
7) 65 years old or greater due to neuronal degeneration leading to bladder
dysfunction.
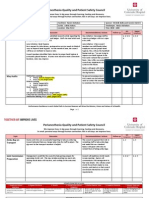
D. POUR Algorithm: To reduce the incidences of POUR in the Phase II patient, the
post anesthesia nurse uses an algorithm. Using the algorithm decreases urinary
retention, frequency of catheterization, duration of Foley catheter, in addition to
improving patient safety, satisfaction, and outcomes.
E. How to use the Algorithm:
1. The post anesthesia nurse identifies phase II patients with a high risk for
developing POUR.
a. Important Note: According to the risk factors, every patient could
be at risk for developing POUR. This does not indicate that every
patient should void prior to discharge.
b. A patient is only required to void prior to discharge if there is an
MD order. Without an order, the PACU nurse must use his/her
critical thinking skills to assess the patients risk and whether or
not the patient should be required to void before discharge.
2. Phase II patients with no risk factors are discharged and advised to call if
they are unable to void within 8 hours of last void.
3. Phase II patients with risk factors must void at least 150 ml.
4. If the patient is unable to void or voids less than 150 ml, the PACU nurse
assesses the patients volume by bladder scan.
5. For bladder volumes greater than 400 ml, the nurse calls the surgical team
for further orders.
6. For bladder volumes less than 400 ml, the PACU nurse may discharge the
patient if appropriate.
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
Is patient at risk
for POUR?
Outpatient with
no risk factors
for POUR
Discharge
Outpatient with
risk factors
for POUR
Unable
to void
Assess volume by
bladder scan
Bladder volume
> 400 ml
Call MD for
catheterization
order
Bladder volume
< 400 ml
Discharge
Advise patient
to seek medical
assistance if
unable to void
within 8 hours
Void
< 150 ml > 150 ml
POUR Algorithm
Vous aimerez peut-être aussi
- Pour Pretest GraphsDocument10 pagesPour Pretest Graphsapi-245672784Pas encore d'évaluation
- Focuspdca Pour1Document5 pagesFocuspdca Pour1api-245672784Pas encore d'évaluation
- PscannualcompetencyDocument2 pagesPscannualcompetencyapi-245672784Pas encore d'évaluation
- Ekg DefibrhythmstemplateDocument1 pageEkg Defibrhythmstemplateapi-245672784Pas encore d'évaluation
- JcahosynopsistemplateDocument1 pageJcahosynopsistemplateapi-245672784Pas encore d'évaluation
- CnaannualcompetencyDocument3 pagesCnaannualcompetencyapi-245672784Pas encore d'évaluation
- RnannualcompetencyDocument3 pagesRnannualcompetencyapi-245672784Pas encore d'évaluation
- CompetencyemailsDocument3 pagesCompetencyemailsapi-245672784Pas encore d'évaluation
- Jcaho EmailsDocument8 pagesJcaho Emailsapi-245672784Pas encore d'évaluation
- Ekg EmailsDocument5 pagesEkg Emailsapi-245672784Pas encore d'évaluation
- Code BlueDocument5 pagesCode Blueapi-245672784Pas encore d'évaluation
- TimelineDocument1 pageTimelineapi-245672784Pas encore d'évaluation
- Ekg Scenario TemplateDocument2 pagesEkg Scenario Templateapi-245672784Pas encore d'évaluation
- PACU Joint Commission Compliance Outcomes Board - PEER REVIEWDocument1 pagePACU Joint Commission Compliance Outcomes Board - PEER REVIEWapi-245672784Pas encore d'évaluation
- JcahopreparationtemplateDocument1 pageJcahopreparationtemplateapi-245672784Pas encore d'évaluation
- CatchabugDocument1 pageCatchabugapi-245672784Pas encore d'évaluation
- JcahomockvisittemplateDocument1 pageJcahomockvisittemplateapi-245672784Pas encore d'évaluation
- Joint Commission Compliance Powerpoint Post-TestDocument2 pagesJoint Commission Compliance Powerpoint Post-Testapi-245672784Pas encore d'évaluation
- Qps Min 5-28Document2 pagesQps Min 5-28api-245672784Pas encore d'évaluation
- 2015 Yearly Joint Commission Compliance CompetencyDocument1 page2015 Yearly Joint Commission Compliance Competencyapi-245672784Pas encore d'évaluation
- Ekg Share Point TesttemplateDocument2 pagesEkg Share Point Testtemplateapi-245672784Pas encore d'évaluation
- JointcommissionDocument27 pagesJointcommissionapi-245672784Pas encore d'évaluation
- Ekg Ulearn ClasstemplateDocument1 pageEkg Ulearn Classtemplateapi-245672784Pas encore d'évaluation
- Perianesthesia Quality and Patient Safety Council CharterDocument2 pagesPerianesthesia Quality and Patient Safety Council Charterapi-245672784Pas encore d'évaluation
- Ekg NursedysrhythmiatesttemplateDocument1 pageEkg Nursedysrhythmiatesttemplateapi-245672784Pas encore d'évaluation
- StrokecontributionDocument3 pagesStrokecontributionapi-245672784Pas encore d'évaluation
- Ekg InterpretationDocument1 pageEkg Interpretationapi-245672784Pas encore d'évaluation
- Stroke Alert Powerpoint EmailsDocument5 pagesStroke Alert Powerpoint Emailsapi-245672784Pas encore d'évaluation
- Pourguideline 1 STDocument3 pagesPourguideline 1 STapi-245672784Pas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- ETHICS & CommunityDocument47 pagesETHICS & CommunityShuaib AhmedPas encore d'évaluation
- Implement WHO surgical safety checklistDocument28 pagesImplement WHO surgical safety checklistAmeng GosimPas encore d'évaluation
- Pre Anesthesia Management and Premedication: Dr. Santosh Khadka Assistant Prof Naihs 2073/11/26Document27 pagesPre Anesthesia Management and Premedication: Dr. Santosh Khadka Assistant Prof Naihs 2073/11/26Manish ShresthaPas encore d'évaluation
- Atralex InjectionDocument20 pagesAtralex InjectionNor ZahidahPas encore d'évaluation
- Negi 2014Document14 pagesNegi 2014Olivia LimPas encore d'évaluation
- Mepivacaine HydrochlorideDocument2 pagesMepivacaine HydrochloridetzuquinoPas encore d'évaluation
- Saudi Prometric Latest Questions AndanswerDocument67 pagesSaudi Prometric Latest Questions AndanswerGloria Jaison100% (4)
- Advanced Blueprint 1Document3 pagesAdvanced Blueprint 1api-728237431Pas encore d'évaluation
- IfU Perseus A500 SW 1.1n EN 9054101Document272 pagesIfU Perseus A500 SW 1.1n EN 9054101Антон ПашаевPas encore d'évaluation
- Lecture 14 Pharmacology Dr. Noor Al HasaniDocument10 pagesLecture 14 Pharmacology Dr. Noor Al Hasaniعلي الاسديPas encore d'évaluation
- Immediate Post-Anaesthesia Recovery 2013Document20 pagesImmediate Post-Anaesthesia Recovery 2013Lee SungjongPas encore d'évaluation
- 192 Pulmonary Aspiration of Gastric Contents - 2Document6 pages192 Pulmonary Aspiration of Gastric Contents - 2ade_liaPas encore d'évaluation
- EnglishDocument56 pagesEnglishPankaj SharmaPas encore d'évaluation
- @anesthesia Books 2020 Oxford Specialist Handbooks in AnaesthesiaDocument705 pages@anesthesia Books 2020 Oxford Specialist Handbooks in AnaesthesiaMarina SolansPas encore d'évaluation
- Brazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Document25 pagesBrazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Renata Araújo Borges XavierPas encore d'évaluation
- Anaesthesia For BurnsDocument51 pagesAnaesthesia For BurnsAnulatkPas encore d'évaluation
- Management of Severe Pre-Eclampsia and Eclampsia Update 2009Document6 pagesManagement of Severe Pre-Eclampsia and Eclampsia Update 2009Praveen RadhakrishnanPas encore d'évaluation
- Teaser BullsDocument11 pagesTeaser BullsEsthefanny Romero HilariónPas encore d'évaluation
- Final FRCApastpapersDocument20 pagesFinal FRCApastpapersRavi Vishnu50% (2)
- Complications of Bimaxillary Orthognathic SurgeryDocument18 pagesComplications of Bimaxillary Orthognathic SurgeryVarun AroraPas encore d'évaluation
- PSARJ180002Document3 pagesPSARJ180002William OmarPas encore d'évaluation
- Normal Parturition and Management of Dystocia in Dogs and CatsDocument7 pagesNormal Parturition and Management of Dystocia in Dogs and Catsmcs.vet8473Pas encore d'évaluation
- State of Vermont Department of Mental Health Redstone Building 26 Terrace Street Phone 802-828-3824 Montpelier, VT 05609-1101 Fax 802-828-3823 WWW - Mentalhealth.vermont - Gov 800-253-0191Document15 pagesState of Vermont Department of Mental Health Redstone Building 26 Terrace Street Phone 802-828-3824 Montpelier, VT 05609-1101 Fax 802-828-3823 WWW - Mentalhealth.vermont - Gov 800-253-0191Titik Dyah AgustiniPas encore d'évaluation
- Operation TheatreDocument22 pagesOperation TheatreAbirami100% (1)
- Daftar Nama Obat & Alkes Yang Diperlukan Tiap Jenis Tindakannya (Untuk Paket), Revisi K'2Document8 pagesDaftar Nama Obat & Alkes Yang Diperlukan Tiap Jenis Tindakannya (Untuk Paket), Revisi K'2Muhammad Ekopranoto100% (1)
- Jciamb4th Standards OnlyDocument25 pagesJciamb4th Standards OnlyZeeshan AliPas encore d'évaluation
- Management of The Difficult Airway in The Pediatric PatientDocument11 pagesManagement of The Difficult Airway in The Pediatric PatientDaniel GallegoPas encore d'évaluation
- Basic Care and ComfortDocument74 pagesBasic Care and ComfortNikko PabicoPas encore d'évaluation
- Perioperative NursingDocument8 pagesPerioperative NursinglovethestarPas encore d'évaluation
- Here Are A List of Some Anaesthetic Drugs For Veterinary UseDocument2 pagesHere Are A List of Some Anaesthetic Drugs For Veterinary UseSapana YadavPas encore d'évaluation