Académique Documents
Professionnel Documents
Culture Documents
DFGHJK
Transféré par
cliffwinskyTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
DFGHJK
Transféré par
cliffwinskyDroits d'auteur :
Formats disponibles
J Ayub Med Coll Abbottabad 2010;22(3)
http://www.ayubmed.edu.pk/JAMC/PAST/22-3/Zahid.pdf 179
ORIGINAL ARTICLE
EARLY VERSUS LATE ARTERIO-VENOUS FISTULAE:
IMPACT ON FAILURE RATE
Zahid Farooq, Arshad Mehmood*, Shahzad Saeed, Khalid Mehmood Raja*,
Malik Nadeem Azam Khan, Badar Murtaza*
Military Hospital, *Armed Forces Institute of Urology, Rawalpindi, Pakistan
Background: Haemodialysis is the primary mode of renal replacement therapy for patients of end
stage renal disease. The most important determinant for effective haemodialysis is a reliable vascular
access. Arterio-venous (AV) fistula is the closest to be an ideal long-term haemodialysis vascular
access. The creation of fistulas or grafts is recommended before starting haemodialysis, this study was
undertaken to determine
the impact of timing of AV fistula creation on its failure rate. Methods: It is a
descriptive study. All patients with chronic kidney disease (CKD) reporting to Armed Forces Institute
of Urology (AFIU) and Military Hospital (MH) Rawalpindi from January 2008 to October 2009 in
whom vascular access was created were included. The patients were followed prospectively and a
complete data about their haemodialysis and vascular access was maintained. Results: A total of 168
permanent accesses were created in 112 patients in this study. The mean duration of follow-up was
14.054.45 months. Early access creation group included 23 patients and late access creation group
included 89 patients. Out of 168 fistulas that were created, 54 fistulas failed with 45 (83.3%) of these
from patients of late access creation group. Age, gender and diabetes mellitus (DM) had no significant
affect on failure rate of fistulas. Conclusion: Timely referral to nephrologists and early creation of
permanent vascular access by dedicated team work can improve the success rate of AV fistulae so
enhancing quality of life of patients of end stage renal disease.
Keywords: Nephrology consultation, Haemodialysis, Arterio-venous fistula
INTRODUCTION
Early pre-dialysis nephrology care is essential in patients
with chronic kidney disease, as it has shown to slow the
progression of kidney disease and reduce morbidity and
mortality.
16
One of the most important aspects of pre-
dialysis care is the timely creation
of vascular access.
National Kidney Foundation Kidney Disease Outcome
Quality Initiative (KDOQI) guidelines
recommend that
vascular access should be created when a patients
creatinine clearance is less than 25 ml/min, or when their
serum
creatinine is greater than 4 mg/dl (353 mol/L), or
within
1 yr of expected start of haemodialysis.
7
Another
target set by these guidelines is
that fistulas should be
created at least 34 months before use. Despite these
recommendations, even in developed countries
approximately one third of persons starting
chronic
haemodialysis therapy are referred late for pre-dialysis
care, and between 3060% use a double lumen catheter
as their initial
vascular access.
8,9
Use of double lumen
catheters for haemodialysis is a consistent risk factor for
sepsis.
10,11
The situation in Pakistan is even worse, most
of the patients are referred late to nephrologists and even
those who are under nephrologists care are unwilling for
AV access creation.
12
So AV fistulae in majority of
cases are created after institution of haemodialysis. The
objective of this study was to determine
the impact of
timing of AV fistula creation on its maturation and
failure.
PATIENTS AND METHOD
This is a descriptive study conducted in prospective
design, in patients with chronic kidney disease (CKD) in
whom permanent vascular access was created. All
patients reporting to nephrology out patient department
or emergency reception of Armed forces Institute of
Urology (AFIU) and Military Hospital (MH) Rawalpindi
from January 2008 to July 2009 were included in this
study. After a thorough history, complete physical
examination and investigations, the patients were treated
depending on their condition and then referred for
vascular access creation. As per protocol the patients
with chronic kidney disease were referred for vascular
access creation as early as possible after stabilisation of
their condition. The patients presenting acutely were
biopsy confirmed or followed up for three months before
referring them for vascular access creation. A complete
data about their haemodialysis and vascular access was
maintained. This included their demographic
information, likely cause of CKD, details about
haemodialysis and vascular access. Vascular access
information included its site of formation, time relation
to haemodialysis and details of surgeon.
For AV fistula formation patient were
examined clinically regarding condition of his vessels
and in doubtful cases Doppler ultrasound mapping was
carried out. End-to-side anastomosis was carried out and
patency checked clinically by thrill. The fistula was
examined next day for patency clinically. In doubtful
cases Doppler ultrasound was carried out and fistula
J Ayub Med Coll Abbottabad 2010;22(3)
http://www.ayubmed.edu.pk/JAMC/PAST/22-3/Zahid.pdf 180
reopened in case of failure. Fistulas were allowed to
mature for more than 46 weeks before use and
cannulated when considered fit after examination. Radio
cephalic (wrist) fistula is the preferred site followed by
brachio-cephalic (elbow) fistula. In the absence of
suitable vessels or after failure of fistulas at these sites,
brachio-basilic fistula with anterior transposition of vein
was preferred over prosthetic graft. Local anaesthesia
was used for conventional fistulas while Brachio-basilic
fistulas and prosthetic grafts were done under general
anaesthesia.
A fistula was considered to have had a primary
failure when it never matured adequately to be used
successfully
for dialysis. The fistulae were categorized
as early if created more than one month before
institution of haemodialysis and late if it was formed
within one month before or after starting haemodialysis.
The outcome of the study was defined as successful use
of fistula for haemodialysis after maturation. Based on
early and late access creation, patients were divided into
2 groups. After comparison of demographic features, the
rate of failure was compared between two groups.
RESULTS
In this study, 125 patients with CKD in whom vascular
access was created, were included. Out of these 5
patients were lost during follow-up and the rest 114
patients were followed prospectively. Eight patients
died during study period, so a total of 112 patients were
included in this study with a mean duration of follow-up
of 14.054.45 months.
A total of 168 permanent accesses were
created in these 112 patients. Out of these 68.8% had
received one permanent access, 18.8% received two and
12.5% received three or more permanent access. Early
access creation group (E-group) included 23 patients
and late creation group (L-group) included 89 patients.
Patients in L-group were relatively younger as
compared to E-group. Males outnumbered females in
both groups with over 60% males in both groups
(p=0.36). There were more patients with diabetes
mellitus (DM) in E-group as compared to L-group
(p=0.557) (Table-1).
Time of nephrology consultation varied a lot
with majority of patients of E-group reporting to a
nephrologist 4 months or earlier to start of
haemodialysis (p<0.001). In L-group 46% cases
reported to nephrologist at the initiation of
haemodialysis or less than one month prior to
haemodialysis and 36 % cases more than 4 months prior
to starting haemodialysis (Table-1).
The majority of patients had a permanent
access created just before or after starting haemodialysis
(62.5%), creating a bell shaped distribution when
plotting persons in monthly interval (Figure-1). Double-
lumen temporary catheter (DL) use increased when
access was created late relative to start of haemodialysis
or in patients with multiple fistulae failure (p<0.001).
First haemodialysis through a double lumen catheter
was carried out in 31% patients from E-group and 98%
patients of the L-group (p<0.001). The mean time of use
of DL catheter in patients starting haemodialysis
without permanent vascular access was 8.3 weeks (58
days). The mean time between referral to surgeon and
first access creation was 2.47 weeks (17 days). Most of
the vascular access operators were urologists in our
setup, followed by vascular surgeons. Time between
AVF creation and cannulation is more than 4 weeks,
with 20.5% cases having cannulation after 4 weeks,
45.5% after 5 weeks and 34% after 6 or more weeks.
Out of 168 fistulae that were created 54
fistulas failed, with significant proportion of these i.e.
83.3% (n=45) from patients of L-group (p-value 0.005).
Age, gender and DM had no significant affect on failure
rate of fistulas. Radio-cephalic site was the major site of
failed fistulae with over 85% of failed fistulas from this
site, followed by brachio-cephalic fistulae. Primary
failure due to thrombosis was the commonest cause
(83%), followed by secondary thrombosis and infection
of AV fistulas. The major site of working fistulae was
also Radiocephalic site (50%) followed by Brachio-
cephalic (36.6%).
Figure-2 shows a young patient from L-group
who had multiple AV fistulae failed and also had a
failed Prosthetic graft. He had multiple life threatening
episodes of septicaemia. Presently he is on
haemodialysis through right brachio-cephalic fistula and
is being worked up for renal transplantation.
Table-1: Comparison of early and late access
creation groups
Variables
Early access
creation group
(n=23)
Late access
creation group
(n=89)
Age (Yr), (MeanSD) 51.218.058 46.216.958
Gender (Male:Female) 40:60 33:67
Cause of ESRD (DM:ND) 52:48 24:76
Time of Nephrology
consultation
<1 month
14 months
>4 months
Nil
8.6%
91.4%
46%
18%
36%
1
st
haemodialysis through DL 31% 98%
ESRD=end stage renal disease, DM:ND=diabetics:non-diabetics,
DL=double-lumen
8
15 18
52
10 9
0
10
20
30
40
50
60
3- 2- 1- 1+ 2+ 3+
Time in months with reference to hemodialysis
Figure-1: Time of formation of AV fistulas with
reference to starting haemodialysis
J Ayub Med Coll Abbottabad 2010;22(3)
http://www.ayubmed.edu.pk/JAMC/PAST/22-3/Zahid.pdf 181
Figure-2: Multiple failed AV fistulae and a failed
prosthetic graft
DISCUSSION
Only 23.5% of patients included in our study had
permanent access created early before starting
haemodialysis. More age in patients of E-group is likely
due to different causes of CKD in two groups. The
patients suffering from chronic diseases like diabetes and
hypertension get an early nephrologist care due to slow
progression of kidney disease and are in E-group, while
in late access creation group we have more patients with
diseases presenting acutely like glomerulonephritis. This
observation is supported in our data with DM more
common in E-group. Male predominance can likely be
due to entitlement in our setup.
In our study 47% cases had early nephrologists
care which in comparison to other countries is very low,
i.e., 6079% patients seeing a nephrologists >4 months
before haemodialysis and 6988% seeing nephrologists
>1 month before starting dialysis.
13
Time of nephrology
consultation is an important factor and had significant
impact on vascular access creation and failure. But even
in late access creation group in our study 36% of patients
had an early nephrology consultation but in them fistula
was formed late. The reasons in these patients are varied
and include poor education status, low income to support
future haemodialysis, haemodialysis phobia and wrong
claims of quacks and non-conventional practicing
physicians to remain dialysis free with their treatment.
So despite thorough counselling these patients are
unwilling to get vascular access created. As a result of
this most of the vascular access created is just before or
after haemodialysis and majority of patients (81.3%) had
first haemodialysis through double lumen. In comparison
for patients having seen a
nephrologist >4 months prior
to ESRD onset, catheter use
varied from 10% in Japan to
around 50% in Canada, USA and UK.
13
Time of referral to surgeon and time taken by
surgeon for access creation also has impact on likelihood
of starting haemodialysis through catheter and thus
fistula failure. With lesser time there is more possibility
of starting haemodialysis through AV fistula. The mean
time from referral to vascular access creation is 17 days
in our study and in other countries median time
calculated varies from 5 to 6 days in Italy, Japan and
Germany, and from 40 to 43 days in Canada and UK.
13
Time between AVF creation and cannulation in
our setup is more than 4 weeks as in most countries. In a
few countries,
a high proportion of units (>60%) have
their AVF first cannulated
within 4 weeks after AVF
creation.
13
CONCLUSION
The creation of vascular access and its maintenance will
remain a challenge in nephrology. Timely referral to
nephrologists and early creation of permanent vascular
access by dedicated team work and development of
expertise can improve success rate of AV fistula and so
improving quality of life of patients with end stage renal
disease. Whenever possible AV fistula should be
created at least 4 months before starting haemodialysis.
REFERENCES
1. Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey
AS, et al. The timing of specialist evaluation in chronic kidney
disease and mortality. Ann Intern Med 2002;137:47986.
2. Arora P, Obrador GT, Ruthazer R, Kausz AT, Meyer KB,
Jenuleson CS, et al. Prevalence, predictors and consequences of
late nephrology referral at a tertiary care center. J Am Soc
Nephrol 1999;10:12816.
3. Schmidt RJ, Domico JR, Sorkin MI, Hobbs G. Early referral and
its impact on emergent first dialyses, health care costs, and
outcome. Am J Kidney Dis 1998;32:27883.
4. Ifudu O, Dawood M, Iofel Y, Valcourt JS, Friedman EA.
Delayed referral of black, Hispanic, and older patients with
chronic renal failure. Am J Kidney Dis 1999;33:72833.
5. Jungers P, Massy ZA, Khoa NT, Choukroun G, Robino C,
Fakhouri F, et al. Longer duration of predialysis nephrological
care is associated with improved long-term survival of dialysis
patients. Nephrol Dial Transplant 2001;16:235764.
6. Stack AG. Impact of timing of nephrology referral and pre-
ESRD care on mortality risk among new ESRD patients in the
United States. Am J Kidney Dis 2003;41:5057.
7. NKF-K/DOQI Clinical Practice Guidelines for Vascular Access:
Update 2000. Am J Kidney Dis 2001;37:S13781.
8. Reddan D, Klassen P, Frankenfield DL, Szczech L, Schwab S,
Coladonato J, et al. National profile of practice patterns for
hemodialysis vascular access in the United States. J Am Soc
Nephrol 2002;13;211724.
9. Pisoni RL, Young EW, Dykstra DM, Greenwood RN, Hecking
E, Gillespie B, et al. Vascular access use in Europe and the
United States: Results from the DOPPS. Kidney Int
2002;61:30516.
10. Hoen B, Dauphin PA, Hestin D, Kessler M. EPIBACDIAL: a
multicenter prospective study of risk factors for bacteremia in
chronic hemodialysis patients. J Am Soc Nephrol 1998;9:86976.
11. Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in
dialysis patients: incidence, risk factors, and prognosis. Kidney
Int 1999;55:108190.
12. Anees M, Mumtaz A, Nazir M, Ibrahim M, Rizwan SM, Kausar
T. Referral pattern of hemodialysis patients to nephrologists. J
Coll Phys Surg Pak 2007;17:6714.
13. Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T,
Akiba T, et al. Vascular access use and outcomes: an
international perspective from the dialysis outcomes and practice
patterns study. Nephrol Dial Transplant 2008;23:321926.
Address for Correspondence:
Maj. Zahid Farooq Baig, House No. 163, Street-14, Jinnahabad, Abbottabad, Pakistan. Cell: +92-323-5100221
Email: zhd.frq@gmail.com
Vous aimerez peut-être aussi
- European Best Practice Guidelines On Vascular Access 2007Document30 pagesEuropean Best Practice Guidelines On Vascular Access 2007Jim Dominguez RosalesPas encore d'évaluation
- Complications of Arteriovenous Fistula For Haemodialysis AccessDocument6 pagesComplications of Arteriovenous Fistula For Haemodialysis AccessAkiko Syawalidhany TahirPas encore d'évaluation
- Increased Minimum Vein Diameter On PreoperativeDocument40 pagesIncreased Minimum Vein Diameter On PreoperativeMikael AngelooPas encore d'évaluation
- DR Mohammed Ahmed, Assistant Professor, Department of Medicine, Bolan Medical CollegeDocument11 pagesDR Mohammed Ahmed, Assistant Professor, Department of Medicine, Bolan Medical CollegeMobin Ur Rehman KhanPas encore d'évaluation
- Quality Improvement Study: Romeo A. Lazarte JR., RN, CNNDocument26 pagesQuality Improvement Study: Romeo A. Lazarte JR., RN, CNNJohn Louie SolitarioPas encore d'évaluation
- A Study On Complications of Ventriculoperitoneal Shunt Surgery in Bir Hospital, Kathmandu, NepalDocument4 pagesA Study On Complications of Ventriculoperitoneal Shunt Surgery in Bir Hospital, Kathmandu, NepalHaziq AnuarPas encore d'évaluation
- Jurnal VaskularDocument13 pagesJurnal VaskulardrelvPas encore d'évaluation
- Ying Li 2016Document8 pagesYing Li 2016Bogdan TrandafirPas encore d'évaluation
- Randomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseDocument9 pagesRandomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseTommy WidjayaPas encore d'évaluation
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaPas encore d'évaluation
- Stenting in Pediatric TransplantationDocument27 pagesStenting in Pediatric TransplantationChris FrenchPas encore d'évaluation
- Posterior Sagittal Anorectoplasty in Anorectal MalformationsDocument5 pagesPosterior Sagittal Anorectoplasty in Anorectal MalformationsmustikaarumPas encore d'évaluation
- Efficacy of Selective Arterial Embolisation For The Treatment of Life-Threatening Post-Partum Haemorrhage in A Large PopulationDocument6 pagesEfficacy of Selective Arterial Embolisation For The Treatment of Life-Threatening Post-Partum Haemorrhage in A Large PopulationAD MonikaPas encore d'évaluation
- Jurnal VaskularDocument5 pagesJurnal VaskulardrelvPas encore d'évaluation
- Surgical ComDocument13 pagesSurgical ComVanitha VeePas encore d'évaluation
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorPas encore d'évaluation
- Ginjal Jurnal ForensikDocument6 pagesGinjal Jurnal ForensikIlham Suryo Wibowo AntonoPas encore d'évaluation
- Arteriovenous Fistulae For Haemodialysis: A Systematic Review and Meta-Analysis of Ef Ficacy and Safety OutcomesDocument10 pagesArteriovenous Fistulae For Haemodialysis: A Systematic Review and Meta-Analysis of Ef Ficacy and Safety OutcomesMarco Antonio Galvan RuizPas encore d'évaluation
- Jurnal THTDocument3 pagesJurnal THTValentina AdindaPas encore d'évaluation
- Analysis of The Results of Sanitation Nephrectomies in Polycystic Kidney Disease in Recipients Before Kidney TransplantationDocument12 pagesAnalysis of The Results of Sanitation Nephrectomies in Polycystic Kidney Disease in Recipients Before Kidney TransplantationОлеся МураховськаPas encore d'évaluation
- Effect of Dialysis On Bleeding Time in Chronic Renal FailureDocument5 pagesEffect of Dialysis On Bleeding Time in Chronic Renal FailureAhsan Tanio DaulayPas encore d'évaluation
- Role of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Document3 pagesRole of Transabdominal Ultrasound in Evaluating Patients With Acute Urinary Retention (Aur) Due To Benign Prostatic Hyperplasia (BPH)Yuni AngrianiPas encore d'évaluation
- Acute Urinary PDFDocument5 pagesAcute Urinary PDFwawanarifkPas encore d'évaluation
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobPas encore d'évaluation
- Adler 2015Document7 pagesAdler 2015nathaliepichardoPas encore d'évaluation
- Risk Factors of THRDocument7 pagesRisk Factors of THRAya Rugaiyah AlkaffPas encore d'évaluation
- Goyal Et Al-2015-Annals of NeurologyDocument7 pagesGoyal Et Al-2015-Annals of NeurologyWinda Wahyu IkaputriPas encore d'évaluation
- Article 8Document4 pagesArticle 8Kamal SaleemPas encore d'évaluation
- Content ServerDocument9 pagesContent ServerenimaPas encore d'évaluation
- Pediatr Transplant 2016 Pundi - 1Document6 pagesPediatr Transplant 2016 Pundi - 1bm1Pas encore d'évaluation
- Downloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Document15 pagesDownloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Pra YudhaPas encore d'évaluation
- Comparison of Open and Laproscopic Live Donor NephrectomyDocument7 pagesComparison of Open and Laproscopic Live Donor NephrectomyEhab Omar El HalawanyPas encore d'évaluation
- Chapter 15 Step by Step Guide Trans Carotid Trans Caval and Direct Aortic March 2 2018Document9 pagesChapter 15 Step by Step Guide Trans Carotid Trans Caval and Direct Aortic March 2 2018Jacinto ThèauxPas encore d'évaluation
- Management of Acute Cholecystitis in UK Hospitals: Time For A ChangeDocument4 pagesManagement of Acute Cholecystitis in UK Hospitals: Time For A ChangeRana BishwoPas encore d'évaluation
- Use of Port-A-Cath in Cancer Patients: A Single-Center ExperienceDocument7 pagesUse of Port-A-Cath in Cancer Patients: A Single-Center ExperienceLydia AmaliaPas encore d'évaluation
- Surgical Repair of Traumatic Pseudoaneurysms Profile at The DR Sutomo 2013-2017 v1507 1905Document8 pagesSurgical Repair of Traumatic Pseudoaneurysms Profile at The DR Sutomo 2013-2017 v1507 1905Nabigh EssadioPas encore d'évaluation
- Annsurg00185 0122Document6 pagesAnnsurg00185 0122Fajr MuzammilPas encore d'évaluation
- Management of Acute Upper Gastrointestinal Bleeding: Urgent Versus Early EndosDocument5 pagesManagement of Acute Upper Gastrointestinal Bleeding: Urgent Versus Early EndosCarolina Ormaza GiraldoPas encore d'évaluation
- Management of Acute Upper Gastrointestinal Bleeding: Urgent Versus Early EndosDocument5 pagesManagement of Acute Upper Gastrointestinal Bleeding: Urgent Versus Early EndossamuelPas encore d'évaluation
- Kurum Boor 2016Document4 pagesKurum Boor 2016Chema ToledoPas encore d'évaluation
- Clinical Efficacy of Enhanced Recovery After Surgery in Percutaneous Nephrolithotripsy: A Randomized Controlled TrialDocument8 pagesClinical Efficacy of Enhanced Recovery After Surgery in Percutaneous Nephrolithotripsy: A Randomized Controlled TrialfaundraPas encore d'évaluation
- Operations Patients Hepatic: Clarification of Risk Factors in With CirrhosisDocument7 pagesOperations Patients Hepatic: Clarification of Risk Factors in With CirrhosisdaviddchandraPas encore d'évaluation
- Research ArticleDocument8 pagesResearch ArticleHuda Al-AnabrPas encore d'évaluation
- The Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalDocument7 pagesThe Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalZablon KodilaPas encore d'évaluation
- Risk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisDocument8 pagesRisk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisSanti ParambangPas encore d'évaluation
- Extending The Interval For Port-A-Cath Maintenance: Eugenia Girda, Rebecca Phaeton, Gary L. Goldberg, Dennis KuoDocument4 pagesExtending The Interval For Port-A-Cath Maintenance: Eugenia Girda, Rebecca Phaeton, Gary L. Goldberg, Dennis KuoJane PengPas encore d'évaluation
- Journal For MEdical WardDocument8 pagesJournal For MEdical WardValcrist BalderPas encore d'évaluation
- Researcharticle Open AccessDocument7 pagesResearcharticle Open AccessvanyPas encore d'évaluation
- A Retrospective Analysis of Complications of Pelvic Exenteration - A Single Institution Experience of 6 YearsDocument6 pagesA Retrospective Analysis of Complications of Pelvic Exenteration - A Single Institution Experience of 6 YearsPremier PublishersPas encore d'évaluation
- HDFVVC EfectoDocument11 pagesHDFVVC Efectogiseladelarosa2006Pas encore d'évaluation
- Cardiac Interventions in Neonates WiDocument11 pagesCardiac Interventions in Neonates WiimPas encore d'évaluation
- Angio Acces OsDocument16 pagesAngio Acces OsKarely TapiaPas encore d'évaluation
- Percutaneous Nephrolithotomy : Randomized Comparison of Large Bore, Small Bore and TubelessDocument6 pagesPercutaneous Nephrolithotomy : Randomized Comparison of Large Bore, Small Bore and TubelessAmir Akram MasihPas encore d'évaluation
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystDocument4 pagesEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterPas encore d'évaluation
- Eco en DPNDocument6 pagesEco en DPNpbchantaPas encore d'évaluation
- Critical Care for Potential Liver Transplant CandidatesD'EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverPas encore d'évaluation
- 1 s2.0 S0140673606691113 MainDocument7 pages1 s2.0 S0140673606691113 MainLuis Angel Ruiz ZamoraPas encore d'évaluation
- SudaniwawiDocument7 pagesSudaniwawiMouhammed SleiayPas encore d'évaluation
- Vur KoreanDocument7 pagesVur KoreanIoannis ValioulisPas encore d'évaluation
- Fifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDocument6 pagesFifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDavid RamirezPas encore d'évaluation
- Ni Hms 777674Document13 pagesNi Hms 777674cliffwinskyPas encore d'évaluation
- Anaesthesia For Laparoscopic SurgeryDocument4 pagesAnaesthesia For Laparoscopic SurgeryRubén Darío HerediaPas encore d'évaluation
- NFT 1Document2 pagesNFT 1cliffwinskyPas encore d'évaluation
- FSFSFSDFDocument7 pagesFSFSFSDFcliffwinskyPas encore d'évaluation
- Tropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakaDocument2 pagesTropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakacliffwinskyPas encore d'évaluation
- Perbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaDocument5 pagesPerbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaTeguh_Yudha_Adi_WijaPas encore d'évaluation
- 6Document2 pages6cliffwinskyPas encore d'évaluation
- Kikel JurnalDocument4 pagesKikel JurnalcliffwinskyPas encore d'évaluation
- Reconstruction of Defects of The Posterior Pinna.15Document4 pagesReconstruction of Defects of The Posterior Pinna.15cliffwinskyPas encore d'évaluation
- Tropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakaDocument2 pagesTropical Gastroenterology. 2011 32 (3) :167-174: Tinjauan PustakacliffwinskyPas encore d'évaluation
- Perbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaDocument5 pagesPerbedaan Efektifitas Pemberian Vitamin E 100 Iu Dengan Aspirin 81 MG Untuk Pencegahan Preeklamsia Pada PrimigravidaTeguh_Yudha_Adi_WijaPas encore d'évaluation
- Lisence Agreement Fine CollegeDocument2 pagesLisence Agreement Fine Collegedidididididididi1234Pas encore d'évaluation
- Follow UpDocument5 pagesFollow UpcliffwinskyPas encore d'évaluation
- Malignancy in OrthopaedicDocument14 pagesMalignancy in OrthopaediccliffwinskyPas encore d'évaluation
- Morning Report InternaDocument14 pagesMorning Report InternacliffwinskyPas encore d'évaluation
- S0733861911X00026 S073386191000157X MainDocument19 pagesS0733861911X00026 S073386191000157X MaincliffwinskyPas encore d'évaluation
- Effect of Rosuvastatin On Cytokines After TraumaticDocument7 pagesEffect of Rosuvastatin On Cytokines After TraumaticcliffwinskyPas encore d'évaluation
- 3.05 Potential Cancer Risk IRSN PaperDocument8 pages3.05 Potential Cancer Risk IRSN PapercliffwinskyPas encore d'évaluation
- Chest X Ray in CAPDocument7 pagesChest X Ray in CAPsahatmanurungPas encore d'évaluation
- Biology of Belief ReviewDocument12 pagesBiology of Belief ReviewcliffwinskyPas encore d'évaluation
- 56 CBT For OCD 2007Document9 pages56 CBT For OCD 2007cliffwinskyPas encore d'évaluation
- Reconstruction of Defects of The Posterior PinnaDocument11 pagesReconstruction of Defects of The Posterior PinnacliffwinskyPas encore d'évaluation
- Cognitive Behavioral Therapy For Pediatric Obsessive CompulsivedisorderDocument9 pagesCognitive Behavioral Therapy For Pediatric Obsessive CompulsivedisordercliffwinskyPas encore d'évaluation
- Varicella Fact Sheet PDFDocument6 pagesVaricella Fact Sheet PDFgodeapPas encore d'évaluation
- 3.05 Potential Cancer Risk IRSN PaperDocument8 pages3.05 Potential Cancer Risk IRSN PapercliffwinskyPas encore d'évaluation
- Chest X Ray in CAPDocument7 pagesChest X Ray in CAPsahatmanurungPas encore d'évaluation
- Classification of Speech ActDocument1 pageClassification of Speech ActDarwin SawalPas encore d'évaluation
- Biochem Nucleic Acid ReviewerDocument5 pagesBiochem Nucleic Acid ReviewerGabrielle FranciscoPas encore d'évaluation
- Recruitement Process - Siemens - Sneha Waman Kadam S200030047 PDFDocument7 pagesRecruitement Process - Siemens - Sneha Waman Kadam S200030047 PDFSneha KadamPas encore d'évaluation
- Starkville Dispatch Eedition 9-10-20Document12 pagesStarkville Dispatch Eedition 9-10-20The DispatchPas encore d'évaluation
- DyslexiaDocument19 pagesDyslexiaKeren HapkhPas encore d'évaluation
- Riber 6-s1 SP s17-097 336-344Document9 pagesRiber 6-s1 SP s17-097 336-344ᎷᏒ'ᏴᎬᎪᏚᎢ ᎷᏒ'ᏴᎬᎪᏚᎢPas encore d'évaluation
- 204-04B - Tire Pressure Monitoring System (TPMS)Document23 pages204-04B - Tire Pressure Monitoring System (TPMS)Sofia AltuzarraPas encore d'évaluation
- Itc LimitedDocument64 pagesItc Limitedjulee G0% (1)
- Chapter 2 and 3 ImmunologyDocument16 pagesChapter 2 and 3 ImmunologyRevathyPas encore d'évaluation
- Management of Preterm LaborDocument2 pagesManagement of Preterm LaborpolygonePas encore d'évaluation
- Food Processing NC II - SAGDocument4 pagesFood Processing NC II - SAGNylmazdahr Sañeud DammahomPas encore d'évaluation
- Pigeon Disease - The Eight Most Common Health Problems in PigeonsDocument2 pagesPigeon Disease - The Eight Most Common Health Problems in Pigeonscc_lawrence100% (1)
- Carboset CA-600 - CST600 - CO - enDocument3 pagesCarboset CA-600 - CST600 - CO - enNilsPas encore d'évaluation
- Multi-Wing Engineering GuideDocument7 pagesMulti-Wing Engineering Guidea_salehiPas encore d'évaluation
- Lichens - Naturally Scottish (Gilbert 2004) PDFDocument46 pagesLichens - Naturally Scottish (Gilbert 2004) PDF18Delta100% (1)
- RRC Group D Notification 70812Document11 pagesRRC Group D Notification 70812admin2772Pas encore d'évaluation
- Not Really A StoryDocument209 pagesNot Really A StorySwapnaPas encore d'évaluation
- TC 10 emDocument7 pagesTC 10 emDina LydaPas encore d'évaluation
- Heart Sounds: Presented by Group 2A & 3ADocument13 pagesHeart Sounds: Presented by Group 2A & 3AMeow Catto100% (1)
- Congenital Flexural Deformity in CalfDocument6 pagesCongenital Flexural Deformity in CalfBibek SutradharPas encore d'évaluation
- Comprehensive Safe Hospital FrameworkDocument12 pagesComprehensive Safe Hospital FrameworkEbby OktaviaPas encore d'évaluation
- Chemical Quick Guide PDFDocument1 pageChemical Quick Guide PDFAndrejs ZundaPas encore d'évaluation
- PolydactylyDocument43 pagesPolydactylyWara Samsarga GedePas encore d'évaluation
- Gendec - Inbound HS-HTNDocument1 pageGendec - Inbound HS-HTNKhalidPas encore d'évaluation
- Pip-Elsmt01 P66 Midstream Projects 0 1/02/18: Document Number S & B Job Number Rev Date SheetDocument11 pagesPip-Elsmt01 P66 Midstream Projects 0 1/02/18: Document Number S & B Job Number Rev Date SheetAjay BaggaPas encore d'évaluation
- Arsenal Strength Catalog 6.2-1Document41 pagesArsenal Strength Catalog 6.2-1Mohammed NavedPas encore d'évaluation
- 'Bubble Kid' Success Puts Gene Therapy Back On TrackDocument5 pages'Bubble Kid' Success Puts Gene Therapy Back On TrackAbby Grey Lopez100% (1)
- Cargador de BateríaDocument34 pagesCargador de BateríaBenPas encore d'évaluation
- Science 9 Q4 SML17 V2Document15 pagesScience 9 Q4 SML17 V2HotdogPas encore d'évaluation
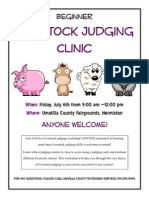
- Jun Judging ClinicDocument1 pageJun Judging Cliniccsponseller27Pas encore d'évaluation