Académique Documents
Professionnel Documents
Culture Documents
Rna Vaccines
Transféré par
biotech_vidhya0 évaluation0% ont trouvé ce document utile (0 vote)
153 vues5 pagesscience
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentscience
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
153 vues5 pagesRna Vaccines
Transféré par
biotech_vidhyascience
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 5
Vaccine 30 (2012) 44144418
Contents lists available at SciVerse ScienceDirect
Vaccine
j our nal home page: www. el sevi er . com/ l ocat e/ vacci ne
Review
RNA-based vaccines
Jeffrey B. Ulmer
, Peter W. Mason, Andrew Geall, Christian W. Mandl
Novartis Vaccines, Cambridge, MA 02139, United States
a r t i c l e i n f o
Article history:
Received 3 February 2012
Received in revised form10 April 2012
Accepted 18 April 2012
Available online 28 April 2012
Keywords:
Nucleic acid vaccine
Viral vector
a b s t r a c t
Nucleic acid vaccines consisting of plasmid DNA, viral vectors or RNA may change the way the next
generation vaccines are produced, as they have the potential to combine the benets of live-attenuated
vaccines, without the complications often associated with live-attenuated vaccine safety and manufac-
turing. Over the past two decades, numerous clinical trials of plasmid DNA and viral vector-based vaccines
have shown them to be safe, well-tolerated and immunogenic. Yet, sufcient potency for general utility
in humans has remained elusive for DNA vaccines and the feasibility of repeated use of viral vectors
has been compromised by anti-vector immunity. RNA vaccines, including those based on mRNA and
self-amplifying RNA replicons, have the potential to overcome the limitations of plasmid DNA and viral
vectors. Possible drawbacks related to the cost and feasibility of manufacturing RNA vaccines are being
addressed, increasing the likelihood that RNA-based vaccines will be commercially viable. Proof of con-
cept for RNA vaccines has been demonstrated in humans and the prospects for further development into
commercial products are very encouraging.
2012 Elsevier Ltd. All rights reserved.
Contents
1. Background. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4414
2. Nucleic acid vaccines. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4414
2.1. DNA vaccines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4415
2.2. Viral vectors . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4415
2.3. RNA vaccines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4415
3. Prospects . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4417
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4417
1. Background
The discovery and development of newand improved vaccines
have been greatly facilitated by the application of new technolo-
gies to identify protective antigens, to optimally present antigens
to the immune system, and to manufacture vaccines using highly
characterized, synthetic methods of production. This progress has
been spurred by a need to move beyond empirical approaches to
vaccines research and development, and has ushered in several
new paradigms including reverse, structural and synthetic vacci-
nology approaches, respectively [1]. The use of nucleic acid-based
vaccines to combine the benets of in situ expression of antigens,
with the safety of inactivated and subunit vaccines, has been a key
advancement. Upontheir discovery more than20years ago, nucleic
acid vaccines promised to be a safe and effective means to mimic
Corresponding author at: Novartis Vaccines, 350 Massachusetts Ave., Cam-
bridge, MA 02139, United States.
E-mail address: jeffrey.ulmer@novartis.com(J.B. Ulmer).
immunization with a live organismvaccine, particularly for induc-
tion of T cell immunity [2]. In addition, the manufacture of nucleic
acid-based vaccines offered the potential to be relatively simple,
inexpensive and generic. Since then, clinical trials have amply
demonstrated the safety and tolerability of nucleic acid vaccines
[3], and robust manufacturing processes have been developed [4].
However, potency in humans has been disappointing, which has
ledto extensive activity to identify enabling technologies. The main
areas for improvement have been directed toward the nucleic acid
vector, targeting the innate immune system to enhance immuno-
genicity, and delivery systems to overcome the barriers to efcient
transfectionof host cells invivo. Signicant progress has beenmade
on all these fronts. This review paper will focus on the use of an
alternative nucleic acid vector, namely RNA, as the basis of a new
generation of vaccines.
2. Nucleic acid vaccines
By denition, nucleic acid vaccines are based on DNA or RNA
encoding the antigen(s) of interest. In their simplest form, they can
0264-410X/$ see front matter 2012 Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.vaccine.2012.04.060
J.B. Ulmer et al. / Vaccine 30 (2012) 44144418 4415
consist of highly puried nucleic acids formulated in a buffer. Most
often, however, specializeddeliverysystems areutilizedtoincrease
vaccine potency. Means to facilitate nucleic acid delivery involve
(1) viral particles to take advantage of the efciency of viral entry
mechanisms, (2) non-viral formulations of DNA or RNA involving
lipids, polymers, emulsions or other synthetic approaches to avoid
the use of viral vectors, and (3) physical delivery technologies, such
as electroporationinsitu. Themajorityof thepreclinical andclinical
experiences with nucleic acid vaccines so far have been with DNA
vaccines and DNA-based viral vectors.
2.1. DNA vaccines
DNAvaccines have been widely evaluated in many animal mod-
els of infectious and non-infectious diseases with generally good
success at eliciting potent immune responses against encodedanti-
gens, which have ranged fromdiscrete T or B cell epitopes to large
polyprotein complexes. The utility of DNA vaccines in animals has
been further documented by the development and commercializa-
tion of plasmid DNA-based animal health products. These include
a West Nile virus vaccine for horses [5], an infectious hematopoi-
etic necrosis virus vaccine for sh [6], a melanoma cancer vaccine
for dogs [7], and a growth hormone releasing hormone gene ther-
apy for pigs [8]. In humans, proof of concept for induction of both
antibody and T cell responses has been demonstrated for various
indications in multiple clinical trials. However, the magnitude of
these immune responses has been lower than those observed for
conventional vaccines consistingof liveor inactivatedwholeorgan-
isms, or subunit proteins formulated with adjuvants. The reasons
for this shortcoming of DNA vaccines are not clear, but are likely
due, at least in part, to inefcient delivery of DNA into human cells
andinadequate stimulationof the humanimmune system. To over-
come these limitations, various technologies have been evaluated
and the most promising current approaches involve facilitation of
DNAdelivery by electroporation[9] and stimulationof the immune
system via the use of genetic adjuvants (i.e., in situ expression of
immunologically active molecules encoded by the DNA vaccine)
[10]. Combinations of these approaches have resulted in potent
induction of immunity in non-human primates [11,12] and pre-
liminary results of human clinical trials are encouraging [3,9].
2.2. Viral vectors
In situ expression of antigens in a vaccinated host can be effec-
tively achieved through the use of recombinant vectors, often DNA
viruses, engineered to be safe and to encode the gene(s) of interest.
Vectors based on adenoviruses and poxviruses have been studied
extensively, although several other viral vectors are being evalu-
atedat earlier stages of development. Bothadenovirus andpoxvirus
vectors have demonstrated safety and immunogenicity in human
clinical trials [13]. Notably, a poxvirus vector encoding HIV enve-
lope protein used in a prime-boost regimen with recombinant
envelope protein plus adjuvant elicited modest protection in a
phase III efcacy trial [14]. One clear advantage of viral vectors
over DNA vaccines is the efciency with which the DNA payload
is introduced into host cells, due to the natural invasiveness of
the viral particle. Hence, the amount of plasmid DNA required
for induction of immune responses is typically many orders of
magnitude greater than the amount of DNA contained in a viral
vector vaccine. Two potential limitations of viral vectors, though,
are related to safety and the inherent immunogenicity of the vec-
tor itself. First, because viral vectors are usually originally derived
from wild-type pathogenic viruses, there is at least a theoretical
potential for reversion to a virulent state, just as there is for atten-
uated live virus-based vaccines. However, extensive safety testing
of these vectors has demonstrated that this is likely not a major
issue. Second, because viral vectors contain, and in some cases
express, viral antigens in addition to the target antigen of inter-
est, such vectors are usually quite immunogenic (i.e., elicit immune
responses against the vectors themselves). Pre-existing anti-vector
immunity (either due to prior infection with wild-type virus, vac-
cines or immunization with the vector) has been shown to blunt
the ability of the vector to launch production of the target anti-
gen and, hence, limits induction of immune responses against the
antigen of interest. Strategies to circumvent this limitation have
included use of certain adenovirus strains not commonly circulat-
ing in humans, to allow initial take of the viral vector vaccine, and
heterologous prime-boost approaches involving different vectors,
to alloweffective boosting of immune responses against the target
antigen. While these approaches canbe effective, at least temporar-
ily, they complicate the vaccination regimen and do not provide an
optimal solution.
2.3. RNA vaccines
Proof of concept for RNA vaccines was provided two decades
ago, when intramuscular injection of mRNA in mice resulted in
local production of an encoded reporter protein [15] and induc-
tion of immune responses against an encoded antigen [16]. In
a direct comparison with a corresponding plasmid DNA vaccine,
injection of similar doses of mRNA (on a mass basis) formulated
in sucrose resulted in similar levels of reporter gene expression,
suggesting equivalent efciencies of cellular transfection in vivo
by the two types of nucleic acid vaccines [15]. These initial pub-
lications were followed by many more demonstrating the general
utility of eliciting immune responses by RNA vaccines (for review,
see [17]). The variety of gene targets included reporter genes
[15,1820] viral antigens [16,21], tumor antigens [2226], and
allergens [27,28]. In these animal models, both antibody and T
cell responses, including CD4
+
and CD8
+
, were elicited. Further-
more, functional immunity, as measured by protective efcacy
against challenge with live pathogens or tumors, was achieved. In
preclinical models of allergy, low doses of an RNA vaccine encod-
ing allergens induce a Th1-biased immune response that provided
resistance against subsequent allergic sensitization. Induction of
antigen-specic immune responses can be achieved by adminis-
tration of RNA vaccines via various routes, including intramuscular
[15,19], intradermal [22], subcutaneous [16], intravenous [16],
intrasplenic [21], and intranodal [24], as well as delivery into the
skin by the gene gun [29,30]. In addition, a considerable amount
of work has been done using mRNA vaccines to pulse dendritic
cells in vitro, which are then administered as the immunizing
agent (for review, see [31]). Hence, like DNAvaccines, RNAvaccines
have demonstrated versatility in many animal models of infectious
and non-infectious diseases. However, RNA vaccines have several
attributes that provide potential advantages over DNA vaccines.
First, there is a nite chance that plasmid DNA vaccines can inte-
grate into the genome of the immunized host. Although there has
beenlittleevidencesofar that integrationoccurs after DNAvaccina-
tion, use of RNA would eliminate this as an issue. Second, plasmid
DNA vaccines must be delivered into and transcribed within the
nucleus in order to transfect a cell, i.e. they must traverse two
membrane barriers (plasma and nuclear membranes). This could
be particularly problematic in non-dividing cells, such as mature
myocytes, where the nuclear membrane remains intact. Several
publications have demonstrated that microinjection of pDNA into
the cytoplasm of non-dividing cells resulted in very low levels
of gene expression, but direct intra-nuclear injection of the same
number of pDNAcopies ledtoefcient transfection[3234]. Incon-
trast, since RNA vaccines are translated directly in the cytoplasm,
the need for delivery into the nucleus is obviated. Finally, the kinet-
ics of antigen expression after RNA administration appears to peak
4416 J.B. Ulmer et al. / Vaccine 30 (2012) 44144418
5' nonstructural proteins Antigen A
n
m7G
Replicon vector
Capsid, E2/E1 glycoproteins A
n
m7G
Virus genome
5' nonstructural proteins
Sub-genomic promoter
Sub-genomic promoter
Fig. 1. Schematic illustration of an RNA replicon vaccine. Example of an RNA replicon vector derived froma positive-strand alphavirus genome. All replicons encode genes
(indicated here as nonstructural proteins) that drive their amplication within the cytoplasmof host cells. For use as vaccine vectors, replicons also encode antigen genes.
For alphavirus vectors, antigen genes are most commonly inserted in place of the capsid and glycoprotein genes, which are not needed for genome replication. In this way,
the vector amplies its full-length genome when it is introduced into the cytoplasm, and then following genome amplication it initiates production of a sub-genomic mRNA
encoding the target antigen.
anddecay rapidly, incontrast toDNAadministrationwhere antigen
expressioncanpersist for manyweeks [35]. Hence, RNAvaccination
better mimics antigen expression during an acute infection, which
may be more conducive to induction of antigen-specic immune
responses.
The mechanisms of action for RNA vaccines have not been
fully elucidated, but likely involve some of the same processes
utilized by DNA vaccines for the expression and presentation of
encoded antigens leading to induction of immune responses. After
injection, the RNA is exposed to RNases in the tissue [36], which
can degrade the vaccine and limit uptake of functional RNA by
cells. In addition, the 2
-hydroyxl on the ribose sugar prevents the
mRNA adopting a stable double -helix, due to steric hindrance,
and makes the macromolecule more prone to hydrolysis. Never-
theless, various cell types are capable of internalizing RNA by an
active, saturable and specic process leading to local expression
of antigen [35]. Uptake is mediated by membrane domains rich
in caveolae and lipid rafts, and involves scavenger receptors [37].
Upon internalization, a portion of the RNAaccumulates in the cyto-
plasm where it is translated into protein. This in situ production
of antigen provides a means to mimic pathogen infections and
expression of tumor antigens leading to efcient presentation of
antigens by major histocompatibility complex (MHC) class I and II
proteins, and induction of T cell responses in a manner analogous
to that provided by DNA vaccines and viral vectors. Alternatively,
RNA vaccines can be constructed for the efcient production and
secretion (or cell-surface expression) of extracellular antigens to
stimulate B cell responses and antigen-specic antibody produc-
tion. The effectiveness of RNA vaccines may also be related to the
fact that RNA is known to be a potent stimulator of innate immu-
nity. In vitro, mRNA has been shown to activate dendritic cells and
monocytes in a MyD88-dependent fashion involving signaling via
Toll-like receptors (TLR) [38,39]. In vivo, it was recently demon-
strated that an mRNA vaccine caused the upregulation of various
genes involved in chemotaxis and cell activation [40] as well as
induction of TLR7-dependent CD4
+
and CD8
+
T cell responses, and
anti-tumor immunity[41]. Hence, thefunctionalityof RNAvaccines
involves at least two components: (1) local expression of antigen
to facilitate presentation by MHC molecules and (2) engagement of
patternrecognitionreceptors tostimulate innate immunityleading
to potentiation of antigen-specic immune responses.
Many of the above-referenced studies have used naked mRNA
as the vaccine (i.e., simply formulated in a buffer). While this
approach has been shown to elicit immune responses, the pres-
ence of degradative enzymes in tissues likely limits the amount
of RNA that is available for internalization by cells in vivo. As a
means to overcome this inherent drawback of using naked RNA,
work has focused on delivery systems, adjuvants, and engineering
of the RNA molecule. First, to protect RNA from degradation and
enhance cellular uptake, encapsulationinliposomes [16,18,26] and
complexationwithcationic polymers [38,41] haveproveneffective.
As an alternative delivery system, the gene gun has been used to
directly introduce mRNA into the cytoplasm of cells [29]. Second,
although RNA vaccines have a built-in adjuvant effect in the form
of TLR engagement, mRNA vaccine potency has been enhanced by
coadministration of recombinant GM-CSF [19] or Flt-3 ligand [42],
or RNA encoding GM-CSF [43]. Finally, several approaches have
been taken to improve the RNA molecule itself. Various modi-
cations have been made to the 5
cap structure, the untranslated
regions, and codon usage in the translated region (for review,
see [44]), which have resulted in increased mRNA stability and
expression.
The feasibility of using RNAas the basis for a nucleic acidvaccine
was initially regarded as questionable, due the inherent instabil-
ity of mRNA in the presence of tissue uids, the uncertainty of
developing reasonable manufacturing processes yielding a stable
formulation, and the anticipated high cost of the product. Each of
these potential limitations is being addressed. Even naked mRNA
is immunogenic in animals [1921,25,45] and humans [46], indi-
cating that RNA degradation in tissues after administration does
not completely abrogate vaccine effectiveness. However, the ef-
ciency of RNA delivery should be increased markedly through the
use of enabling synthetic and viral delivery systems. For research
purposes, in vitro transcribed mRNA can be obtained from plas-
mid DNA containing a bacteriophage promoter (T7, SP6 or T3) and
over the past 10 years many technical renements to the com-
mercial kits have resulted in dramatic improvements in quality
and yield [31,47]. More recently, RNA manufacturing by enzymatic
transcription of appropriate DNA templates now seems attainable
at reasonable cost and large scale. Long-termstorage of lyophilized
RNA vaccines have previously been studied and RNAse-free RNA
vaccines were demonstrated to be no less stable than other con-
ventional vaccines that require a cold chain to retain efcacy [48].
These advancements have enabled the development of process for
the GMP production of mRNA vaccines in quantities sufcient for
human clinical trials (for review, see [17]).
While most of the published work has utilized mRNA as the
vaccine, several publications have shown that RNA vaccines can
also be derived from sub-genomic replicons that lack viral struc-
tural proteins. Replicon RNA-based vaccines have been generated
for a variety of RNA viruses including, Semliki Forest virus [21,25],
Sindbis virus [20], poliovirus [49,50], tick-borne encephalitis virus
[51,52], Kunjinvirus [53], andbovineviral diarrhea[54]. RNA-based
vaccines have also been described in which the RNAvaccine is used
to launcha live-attenuatedvirus infection. Inthis case, the inherent
potency of the encoded live viral vaccine has permitted this type
of RNA vaccine to elicit protective immunity at very low (ng) RNA
doses [51]. More commonly, experimental RNA-based vaccines are
viral-particle delivered products engineered to express a heterol-
ogous antigen in place of the viral structural genes. These vaccines
are produced under special conditions (e.g., packaging cell lines)
that permit productionof single-roundinfectious particles carrying
J.B. Ulmer et al. / Vaccine 30 (2012) 44144418 4417
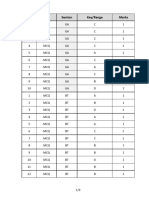
Table 1
Superior attributes of RNA vaccines.
Parameter Vaccine type
Live Subunit Viral vector DNA mRNA Replicon RNA
Synthetic +/ + +
Generic manufacturing + + +
Safety +/ + +/ + + +
Antibody induction + + + +/ + +
CTL induction + + + + +
In vivo expression + + + + +
Control of expression + + + +
Absence of eukaryotic contaminants +/ + + +
In vivo self amplication + + +
Potency in humans + + +/ +/ +/ TBD
RNAs encoding the vaccine antigens [5559]. In this way, transient,
highlevels of antigenproductioncanbeachievedwithout theuseof
a live, spreading viral infection. Replicons derived fromdifferent
RNA viruses differ with regard to levels and duration of heterolo-
gous gene expression allowing the generation of a versatile toolbox
for vaccine or gene therapy applications [60]. An illustration of an
RNA vaccine based on an alphavirus replicon is depicted in Fig. 1.
The RNA amplication process in the cytoplasmproduces multiple
copies of antigen-encoding mRNA and creates dsRNA intermedi-
ates, which are known to be potent stimulators of innate immunity
[61]. Thus, onamass basis, repliconRNAvaccines havethepotential
to be more effective than corresponding mRNA vaccines. Indeed, a
direct comparison of the two types of RNA vaccines demonstrated
signicantly higher and more persistent expression levels in vivo
after replicon RNA administration [20].
These replicon vaccines have been administered as naked RNA
packaged in viral particles, or delivered by electroporation in situ
[52,62,63] Viral particle delivery of replicons has the advantage of
efciency, as previously describedfor viral vectors, but complicates
manufacturing, introduces theoretical safety considerations, and
has the potential limitation of anti-vector immunity. Hence, facil-
itated delivery of RNA replicons using synthetic systems, such as
those evaluated for mRNA or DNA vaccines may increase potency
without the added complications commonly seen with viral vec-
tors.
3. Prospects
RNA vaccines, particularly self-amplifying replicons, have the
potential to capture the advantages of both DNA vaccines and
viral delivery while overcoming the drawbacks of each technology
(see Table 1). The prospect of RNA vaccines being a more effec-
tive approach than other types of nucleic acid vaccines has led to
their advancement into human clinical trials. So far, mRNA vac-
cines have been administered to cancer patients in several trials as
active immunotherapeutic immunization protocols, supported by
preclinical proof of concept inanimal tumor models (for review, see
[31]). Intherst trial, mRNAencodinggenes clonedfrommetastatic
melanoma tumors were usedas anautologous immunizationstrat-
egy [46]. Subsequent trials used combinations of known tumor
antigens, such as MUC1, CEA, telomerase, MAGE-1, tyrosinase, in
metastatic melanoma [64] and renal cell carcinoma [65] patients.
In these exploratory clinical trials, the mRNA vaccines elicited
antigen-specic immune responses (both antibodies and T cells),
demonstrating proof of concept that mRNA vaccines are active in
humans. Clinical trials have also beenperformedwithRNAreplicon
vaccines packaged in viral particles. A bivalent vaccine consisting
of replicons encoding cytomegalovirus (CMV) gBandpp65/IE1 pro-
teins was shown to be well tolerated and immunogenic in healthy
CMV seronegative volunteers [66]. All 40 individuals generated
polyfunctional CD4
+
and CD8
+
T cell responses, as well as virus
neutralizing antibodies. However, the magnitude of the responses
in these recent trials was similar to those previously observed
for other types of nucleic acid vaccines. Therefore, the RNA vac-
cine approach holds promise as an effective means of eliciting
functional, protective immune responses in humans, but success
will likely require enabling delivery technologies. Next generation
replicon RNA vaccines will be formulated with synthetic delivery
technologies and will aspire to combine the effectiveness of live
attenuated vaccines, an equal or better safety prole than plasmid
DNA vaccines, and completely synthetic methods of manufacture.
Such a vaccine would possess the desired attributes of an ideal
vaccine.
References
[1] Rappuoli R, Mandl CW, Black S, De Gregorio E. Vaccines for the twenty-rst
century society. Nature Reviews Immunology 2011;11(12):86572.
[2] Ulmer JB, Donnelly JJ, Parker SE, Rhodes GH, Felgner PL, Dwarki VJ, et al. Het-
erologous protection against inuenza by injection of DNA encoding a viral
protein. Science 1993;259(5102):17459.
[3] Ferraro B, Morrow MP, Hutnick NA, Shin TH, Lucke CE, Weiner DB. Clinical
applications of DNA vaccines: current progress. Clinical Infectious Diseases
2011;53(3):296302.
[4] Lara AR, Ramirez OT. Plasmid DNA production for therapeutic applications.
Methods in Molecular Biology 2012;824:271303.
[5] Davis BS, Chang GJ, Cropp B, Roehrig JT, Martin DA, Mitchell CJ, et al. West
Nile virus recombinant DNA vaccine protects mouse and horse from virus
challenge and expresses in vitro a noninfectious recombinant antigen that
can be used in enzyme-linked immunosorbent assays. Journal of Virology
2001;75(9):40407.
[6] Garver KA, LaPatraSE, KurathG. Efcacyof aninfectious hematopoietic necrosis
(IHN) virus DNA vaccine in Chinook Oncorhynchus tshawytscha and sockeye O.
nerka salmon. Diseases of Aquatic Organisms 2005;64(1):1322.
[7] Grosenbaugh DA, Leard AT, Bergman PJ, Klein MK, Meleo K, Susaneck S, et al.
Safety andefcacy of a xenogeneic DNAvaccine encoding for humantyrosinase
as adjunctive treatment for oral malignant melanoma in dogs following sur-
gical excision of the primary tumor. American Journal of Veterinary Research
2011;72(12):16318.
[8] Draghia-Akli R, Li X, Schwartz RJ. Enhanced growth by ectopic expression
of growth hormone releasing hormone using an injectable myogenic vector.
Nature Biotechnology 1997;15(12):12859.
[9] Sardesai NY, Weiner DB. Electroporation delivery of DNA vaccines: prospects
for success. Current Opinion in Immunology 2011;23(3):4219.
[10] Lori F, Weiner DB, Calarota SA, Kelly LM, Lisziewicz J. Cytokine-adjuvanted
HIV-DNA vaccination strategies. Springer Seminars in Immunopathology
2006;28(3):2318.
[11] Belisle SE, Yin J, Shedlock DJ, Dai A, Yan J, Hirao L, et al. Long-term program-
ming of antigen-specic immunity from gene expression signatures in the
PBMC of rhesus macaques immunized with an SIV DNA vaccine. PLoS One
2011;6(6):e19681.
[12] Hirao LA, Hokey DA, MorrowMP, Jure-Kunkel MN, Weiner DB. Immune modu-
lation through 4-1BB enhances SIV vaccine protection in non-human primates
against SIVmac251 challenge. PLoS One 2011;6(9):e24250.
[13] Rollier CS, Reyes-Sandoval A, Cottingham MG, Ewer K, Hill AV. Viral vectors
as vaccine platforms: deployment in sight. Current Opinion in Immunology
2011;23(3):37782.
[14] Vaccari M, Poonam P, Franchini G. Phase III HIV vaccine trial in Thailand:
a step toward a protective vaccine for HIV. Expert Review of Vaccines
2010;9(9):9971005.
[15] Wolff JA, Malone RW, Williams P, Chong W, Acsadi G, Jani A, et al. Direct
gene transfer into mouse muscle in vivo. Science 1990;247(4949 Pt 1):
14658.
4418 J.B. Ulmer et al. / Vaccine 30 (2012) 44144418
[16] MartinonF, KrishnanS, LenzenG, Magne R, GomardE, Guillet JG, et al. Induction
of virus-specic cytotoxic Tlymphocytes invivobyliposome-entrappedmRNA.
European Journal of Immunology 1993;23(7):171922.
[17] Pascolo S. Messenger RNA-based vaccines. Expert Opinion on Biological Ther-
apy 2004;4(8):128594.
[18] Hoerr I, Obst R, Rammensee HG, Jung G. In vivo application of RNA leads to
induction of specic cytotoxic T lymphocytes and antibodies. European Journal
of Immunology 2000;30(1):17.
[19] Carralot JP, Probst J, Hoerr I, Scheel B, Teufel R, Jung G, et al. Polarization of
immunity induced by direct injection of naked sequence-stabilized mRNAvac-
cines. Cellular and Molecular Life Sciences 2004;61(18):241824.
[20] Johanning FW, Conry RM, LoBuglio AF, Wright M, Sumerel LA, Pike MJ,
et al. A Sindbis virus mRNA polynucleotide vector achieves prolonged and
high level heterologous gene expression in vivo. Nucleic Acids Research
1995;23(9):1495501.
[21] Zhou X, Berglund P, Rhodes G, Parker SE, Jondal M, LiljestromP. Self-replicating
Semliki Forest virus RNAas recombinant vaccine. Vaccine1994;12(16):15104.
[22] Granstein RD, Ding W, Ozawa H. Induction of anti-tumor immunity with epi-
dermal cells pulsed with tumor-derived RNA or intradermal administration of
RNA. Journal of Investigative Dermatology 2000;114(4):6326.
[23] Conry RM, LoBuglio AF, Wright M, Sumerel L, Pike MJ, Johanning F, et al. Charac-
terization of a messenger RNA polynucleotide vaccine vector. Cancer Research
1995;55(7):1397400.
[24] Kreiter S, Selmi A, Diken M, Koslowski M, Britten CM, Huber C, et al. Intranodal
vaccination with naked antigen-encoding RNA elicits potent prophylactic and
therapeutic antitumoral immunity. Cancer Research 2010;70(22):903140.
[25] Ying H, Zaks TZ, Wang RF, Irvine KR, Kammula US, Marincola FM, et al.
Cancer therapy using a self-replicating RNA vaccine. Nature Medicine
1999;5(7):8237.
[26] Zhou WZ, Hoon DS, Huang SK, Fujii S, Hashimoto K, Morishita R, et al. RNA
melanoma vaccine: induction of antitumor immunity by human glycoprotein
100 mRNA immunization. Human Gene Therapy 1999;10(16):271924.
[27] Roesler E, Weiss R, Weinberger EE, Fruehwirth A, Stoecklinger A, Mostbock
S, et al. Immunize and disappear-safety-optimized mRNA vaccination with
a panel of 29 allergens. The Journal of Allergy and Clinical Immunology
2009;124(5), 1070-7 e111.
[28] Weiss R, Scheiblhofer S, Roesler E, Weinberger E, Thalhamer J. mRNA vaccina-
tionas a safe approachfor specic protectionfromtype I allergy. Expert Review
of Vaccines 2012;11(1):5567.
[29] Qiu P, Ziegelhoffer P, Sun J, Yang NS. Gene gun delivery of mRNA in situ results
in efcient transgene expression and genetic immunization. Gene Therapy
1996;3(3):2628.
[30] Aberle JH, Aberle SW, Koer RM, Mandl CW. Humoral and cellular immune
response to RNA immunization with avivirus replicons derived from tick-
borne encephalitis virus. Journal of Virology 2005;79(24):1510713.
[31] Kreiter S, Diken M, Selmi A, Tureci O, Sahin U. Tumor vaccination using mes-
senger RNA: prospects of a future therapy. Current Opinion in Immunology
2011;23(3):399406.
[32] Mirzayans R, Aubin RA, Paterson MC. Differential expression and stability of
foreign genes introduced into human broblasts by nuclear versus cytoplasmic
microinjection. Mutation Research 1992;281(2):11522.
[33] Thorburn AM, Alberts AS. Efcient expression of miniprep plasmid DNA after
needle micro-injection into somatic cells. Biotechniques 1993;14(3):3568.
[34] Zabner J, Fasbender AJ, Moninger T, Poellinger KA, Welsh MJ. Cellular and
molecular barriers to gene transfer by a cationic lipid. Journal of Biological
Chemistry 1995;270(32):189979007.
[35] Probst J, Weide B, Scheel B, Pichler BJ, Hoerr I, Rammensee HG, et al. Spon-
taneous cellular uptake of exogenous messenger RNA in vivo is nucleic acid-
specic, saturable and ion dependent. Gene Therapy 2007;14(15):117580.
[36] Probst J, Brechtel S, Scheel B, Hoerr I, Jung G, Rammensee HG, et al. Charac-
terization of the ribonuclease activity on the skin surface. Genetics Vaccines
Therapy 2006;4:4.
[37] Lorenz C, Fotin-Mleczek M, Roth G, Becker C, Dam TC, Verdurmen WP,
et al. Protein expression from exogenous mRNA: uptake by receptor-
mediated endocytosis and trafcking via the lysosomal pathway. RNA Biology
2011;8(4):62736.
[38] Scheel B, Teufel R, Probst J, Carralot JP, Geginat J, Radsak M, et al. Toll-like
receptor-dependent activationof several humanbloodcell types byprotamine-
condensed mRNA. European Journal of Immunology 2005;35(5):155766.
[39] Kariko K, Ni H, Capodici J, Lamphier M, Weissman D. mRNA is an
endogenous ligand for Toll-like receptor 3. Journal of Biological Chemistry
2004;279(13):1254250.
[40] Fotin Mleczek M, Zanzinger K, Heidenreich R, Lorenz C, Thess A, Duchardt KM,
et al. Highly potent mRNA based cancer vaccines represent an attractive plat-
formfor combinationtherapies supporting animprovedtherapeutic effect. The
Journal of Gene Medicine; in press.
[41] Fotin-Mleczek M, Duchardt KM, Lorenz C, Pfeiffer R, Ojkic-Zrna S, Probst J,
et al. Messenger RNA-based vaccines with dual activity induce balanced TLR-7
dependent adaptive immune responses andprovide antitumor activity. Journal
of Immunotherapy 2011;34(1):115.
[42] Kreiter S, Diken M, Selmi A, Diekmann J, Attig S, Husemann Y, et al. FLT3 lig-
and enhances the cancer therapeutic potency of naked RNA vaccines. Cancer
Research 2011;71(19):613242.
[43] Hess PR, Boczkowski D, Nair SK, Snyder D, Gilboa E. Vaccination with mRNAs
encoding tumor-associated antigens and granulocyte-macrophage colony-
stimulating factor efciently primes CTL responses, but is insufcient to
overcome tolerance to a model tumor/self antigen. Cancer Immunology and
Immunotherapy 2006;55(6):67283.
[44] Pascolo S. Vaccination with messenger RNA (mRNA). Handbook of Experimen-
tal Pharmacology 2008;183:22135.
[45] Conry RM, LoBuglio AF, Loechel F, Moore SE, Sumerel LA, BarlowDL, et al. Acar-
cinoembryonic antigen polynucleotide vaccine for human clinical use. Cancer
Gene Therapy 1995;2(1):338.
[46] Weide B, Carralot JP, Reese A, Scheel B, Eigentler TK, Hoerr I, et al. Results of the
rst phase I/II clinical vaccination trial with direct injection of mRNA. Journal
of Immunotherapy 2008;31(2):1808.
[47] Yamamoto A, Kormann M, Rosenecker J, Rudolph C. Current prospects for
mRNAgenedelivery. EuropeanJournal of Pharmaceutics andBiopharmaceutics
2009;71(3):4849.
[48] Jones KL, Drane D, Gowans EJ. Long-term storage of DNA-free RNA for use in
vaccine studies. Biotechniques 2007;43(5):67581.
[49] Jackson CA, Messinger J, Palmer MT, Peduzzi JD, Morrow CD. Gene expression
in the muscle and central nervous system following intramuscular inocu-
lation of encapsidated or naked poliovirus replicons. Virology 2003;314(1):
4561.
[50] Vignuzzi M, Gerbaud S, van der Werf S, Escriou N. Naked RNA immu-
nization with replicons derived from poliovirus and Semliki Forest virus
genomes for the generation of a cytotoxic T cell response against the
inuenza A virus nucleoprotein. Journal of General Virology 2001;82(Pt 7):
173747.
[51] Mandl CW, Aberle JH, Aberle SW, Holzmann H, Allison SL, Heinz FX. In vitro-
synthesized infectious RNA as an attenuated live vaccine in a avivirus model.
Nature Medicine 1998;4(12):143840.
[52] Koer RM, Aberle JH, Aberle SW, Allison SL, Heinz FX, Mandl CW. Mimicking
live avivirus immunization with a noninfectious RNA vaccine. Proceed-
ings of the National Academy of Sciences of the United States of America
2004;101(7):19516.
[53] Harvey TJ, Anraku I, Linedale R, Harrich D, Mackenzie J, Suhrbier A, et al. Kunjin
virus replicon vectors for human immunodeciency virus vaccine develop-
ment. Journal of Virology 2003;77(14):7796803.
[54] Edlich B, Hogdal LJ, Rehermann B, Behrens SE. Dendritic cells transfected with
Her2 antigen-encoding RNAreplicons cross-prime CD8 T cells andprotect mice
against tumor challenge. Vaccine 2010;28(49):776473.
[55] Li HO, Zhu YF, Asakawa M, Kuma H, Hirata T, Ueda Y, et al. A cytoplasmic RNA
vector derived fromnontransmissible Sendai virus with efcient gene transfer
and expression. Journal of Virology 2000;74(14):65649.
[56] Kalhoro NH, Veits J, Rautenschlein S, Zimmer G. A recombinant vesicular stom-
atitis virus replicon vaccine protects chickens from highly pathogenic avian
inuenza virus (H7N1). Vaccine 2009;27(8):117483.
[57] Widman DG, Frolov I, Mason PW. Third-generation avivirus vaccines based
on single-cycle, encapsidation-defective viruses. Advances in Virus Research
2008;72:77126.
[58] Perri S, Greer CE, Thudium K, Doe B, Legg H, Liu H, et al. An alphavirus repli-
con particle chimera derived fromvenezuelan equine encephalitis and sindbis
viruses is a potent gene-based vaccine delivery vector. Journal of Virology
2003;77(19):10394403.
[59] Caley IJ, Betts MR, Irlbeck DM, Davis NL, Swanstrom R, Frelinger JA,
et al. Humoral, mucosal, and cellular immunity in response to a human
immunodeciency virus type 1 immunogen expressed by a Venezuelan
equine encephalitis virus vaccine vector. Journal of Virology 1997;71(4):
30318.
[60] Gehrke R, Heinz FX, Davis NL, Mandl CW. Heterologous gene expression by
infectious and replicon vectors derived fromtick-borne encephalitis virus and
direct comparison of this avivirus systemwith an alphavirus replicon. Journal
of General Virology 2005;86(Pt 4):104553.
[61] Wang Y, Swiecki M, McCartney SA, Colonna M. dsRNA sensors and plasmacy-
toid dendritic cells in host defense and autoimmunity. Immunological Review
2011;243(1):7490.
[62] Piggott JM, Sheahan BJ, Soden DM, OSullivan GC, Atkins GJ. Electroporation
of RNA stimulates immunity to an encoded reporter gene in mice. Molecular
Medicine Report 2009;2(5):7536.
[63] Johansson DX, Ljungberg K, Kakoulidou M, Liljestrom P. Intradermal electro-
poration of naked replicon RNA elicits strong immune responses. PLoS One
2012;7(1):e29732.
[64] Weide B, Pascolo S, Scheel B, Derhovanessian E, Pugfelder A, Eigentler TK,
et al. Direct injection of protamine-protected mRNA: results of a phase 1/2
vaccination trial in metastatic melanoma patients. Journal of Immunotherapy
2009;32(5):498507.
[65] Rittig SM, Haentschel M, Weimer KJ, Heine A, Muller MR, Brugger W, et al.
Intradermal vaccinations with RNA coding for TAA generate CD8
+
and CD4
+
immuneresponses andinduceclinical benet invaccinatedpatients. Molecular
Therapy 2011;19(5):9909.
[66] Bernstein DI, Reap EA, Katen K, Watson A, Smith K, Norberg P, et al.
Randomized, double-blind, phase 1 trial of an alphavirus replicon vac-
cine for cytomegalovirus in CMV seronegative adult volunteers. Vaccine
2009;28(2):48493.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Facs ProtocolDocument7 pagesFacs ProtocolmisterxPas encore d'évaluation
- BT 2019Document13 pagesBT 2019biotech_vidhyaPas encore d'évaluation
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatorePas encore d'évaluation
- Q.No. Type Section Key/Range MarksDocument3 pagesQ.No. Type Section Key/Range Marksbiotech_vidhyaPas encore d'évaluation
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatorePas encore d'évaluation
- Polymerase Chain Reaction (PCR)Document3 pagesPolymerase Chain Reaction (PCR)biotech_vidhyaPas encore d'évaluation
- Brad FordDocument12 pagesBrad FordQi ChaoPas encore d'évaluation
- SDS PageDocument2 pagesSDS Pagebiotech_vidhyaPas encore d'évaluation
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaPas encore d'évaluation
- Troubleshooting SDS-PAGE 1Document3 pagesTroubleshooting SDS-PAGE 1biotech_vidhyaPas encore d'évaluation
- Polymerasen GuideDocument16 pagesPolymerasen Guidebiotech_vidhyaPas encore d'évaluation
- Components Reaction MixtureDocument3 pagesComponents Reaction Mixturebiotech_vidhyaPas encore d'évaluation
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaPas encore d'évaluation
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaPas encore d'évaluation
- Whole Cell ExtractDocument1 pageWhole Cell Extractbiotech_vidhyaPas encore d'évaluation
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaPas encore d'évaluation
- Befcv List PDFDocument22 pagesBefcv List PDFbiotech_vidhyaPas encore d'évaluation
- Nuclear ExtractsDocument2 pagesNuclear Extractsbiotech_vidhyaPas encore d'évaluation
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaPas encore d'évaluation
- Ies 17 Set A Me Q ADocument67 pagesIes 17 Set A Me Q Abiotech_vidhyaPas encore d'évaluation
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaPas encore d'évaluation
- A.E. (Mechanical Engineering I) 2007Document24 pagesA.E. (Mechanical Engineering I) 2007Mukesh KumarPas encore d'évaluation
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaPas encore d'évaluation
- ESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionDocument52 pagesESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionpataPas encore d'évaluation
- Img Word-To PDFDocument3 pagesImg Word-To PDFbiotech_vidhyaPas encore d'évaluation
- Mechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010Document20 pagesMechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010biotech_vidhyaPas encore d'évaluation
- TDC 41597 A (Mechanical Engg.) - 2012Document20 pagesTDC 41597 A (Mechanical Engg.) - 2012biotech_vidhyaPas encore d'évaluation
- Recruitment RulesDocument5 pagesRecruitment Rulesbiotech_vidhyaPas encore d'évaluation
- Part and Mold Design GuideDocument170 pagesPart and Mold Design GuideminhtintinPas encore d'évaluation
- 1 TolerancesDocument1 page1 Tolerancesbiotech_vidhyaPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Phagocytosis Assay Kit (Igg Fitc) : Item No. 500290Document9 pagesPhagocytosis Assay Kit (Igg Fitc) : Item No. 500290drfiatPas encore d'évaluation
- Ecg Quick Guide PDFDocument7 pagesEcg Quick Guide PDFansarijavedPas encore d'évaluation
- Master Tong-Style Acupuncturist Interview Part 1Document4 pagesMaster Tong-Style Acupuncturist Interview Part 1Anonymous uMnup2r100% (1)
- Final Benzodiazepine Guidelines Version 23 1495194854Document18 pagesFinal Benzodiazepine Guidelines Version 23 1495194854Kru PrimePas encore d'évaluation
- Congenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/PrhDocument66 pagesCongenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/Prhawaisjinnah100% (1)
- Petridou, Thumiger-Homo Patiens - Approaches To The Patient in The Ancient World (SAM 45)Document555 pagesPetridou, Thumiger-Homo Patiens - Approaches To The Patient in The Ancient World (SAM 45)jeremy_luckas100% (1)
- Tugas B.inggrisDocument14 pagesTugas B.inggrisLove.u. TooPas encore d'évaluation
- Aman Foundation Internship Application FormDocument4 pagesAman Foundation Internship Application Formabdullahnisar92Pas encore d'évaluation
- CH 25 Respiration Study GuideDocument2 pagesCH 25 Respiration Study Guide99646qbkdwPas encore d'évaluation
- Hospital Job DescriptionsDocument48 pagesHospital Job DescriptionsLoresita Amoranto Rebong RNPas encore d'évaluation
- Thyroid Gland AnatomyDocument11 pagesThyroid Gland AnatomyRem AlfelorPas encore d'évaluation
- Reading Sub-Test: Answer Key - Part ADocument23 pagesReading Sub-Test: Answer Key - Part AAlwin BrightPas encore d'évaluation
- 01 1 PDFDocument8 pages01 1 PDFpravikumar1989Pas encore d'évaluation
- Maximum Marks: 100Document35 pagesMaximum Marks: 100Yu HoyanPas encore d'évaluation
- Orthovoltage Vs MegavoltageDocument7 pagesOrthovoltage Vs MegavoltageEmmanuel Cuevas MisPas encore d'évaluation
- DiaDENS-Cardio Operations ManualDocument37 pagesDiaDENS-Cardio Operations Manualgetdenas100% (4)
- Pahs Mbbs Information BookletDocument18 pagesPahs Mbbs Information BookletKishor BajgainPas encore d'évaluation
- Mini Question Bank - Vety Sci - For Students PDFDocument106 pagesMini Question Bank - Vety Sci - For Students PDFRakesh Prajapati100% (3)
- Synthesis of Novel Amino Acid Derivative of 7-AVCADocument4 pagesSynthesis of Novel Amino Acid Derivative of 7-AVCAIOSRjournal0% (1)
- Treatment Head LiceDocument26 pagesTreatment Head LiceCherry Amor Betita MadronaPas encore d'évaluation
- Treponema Pallidum: Human PathogensDocument27 pagesTreponema Pallidum: Human PathogensGeorgeNecoarăPas encore d'évaluation
- Human Papillomavirus (HPV) Test and PAP Smear As Predictors of Outcome in Conservatively Treated Adenocarcinoma in Situ (AIS) of The Uterine CervixDocument7 pagesHuman Papillomavirus (HPV) Test and PAP Smear As Predictors of Outcome in Conservatively Treated Adenocarcinoma in Situ (AIS) of The Uterine CervixodivarPas encore d'évaluation
- Herb II-5-Herbs That Tonify Qi & BloodDocument51 pagesHerb II-5-Herbs That Tonify Qi & BloodEdison halimPas encore d'évaluation
- Assessment Diagnosis Planning Interventions Rationale Evaluation Subjective: "Maglisod Man Kog Short Term: Independent: - Establish RapportDocument3 pagesAssessment Diagnosis Planning Interventions Rationale Evaluation Subjective: "Maglisod Man Kog Short Term: Independent: - Establish RapportSergi Lee OratePas encore d'évaluation
- Procedimento Implante AmbicorDocument12 pagesProcedimento Implante Ambicorapi-3762376Pas encore d'évaluation
- Acute Care TestingDocument222 pagesAcute Care TestingAdel ChaabanePas encore d'évaluation
- 53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Document9 pages53 Vol. 6 Issue 7 IJPSR 2015 RA 4953Dina AyupnPas encore d'évaluation
- Pott's DiseaseDocument8 pagesPott's DiseaseBij HilarioPas encore d'évaluation
- Q4 Health 6 Week3Document4 pagesQ4 Health 6 Week3Ethelyn Joy FarquerabaoPas encore d'évaluation
- Clonus: Definition, Mechanism, Treatment: ReviewDocument8 pagesClonus: Definition, Mechanism, Treatment: ReviewLuqmanul HakimPas encore d'évaluation