Académique Documents
Professionnel Documents
Culture Documents
Oxidative Stress
Transféré par
valentinamorantes0 évaluation0% ont trouvé ce document utile (0 vote)
23 vues6 pagesarticulo sobre la Modulación de la expresión y función de las enzimas oxidantes y antioxidantes de las células vasculares
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentarticulo sobre la Modulación de la expresión y función de las enzimas oxidantes y antioxidantes de las células vasculares
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
23 vues6 pagesOxidative Stress
Transféré par
valentinamorantesarticulo sobre la Modulación de la expresión y función de las enzimas oxidantes y antioxidantes de las células vasculares
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 6
Modulation of Oxidant and Antioxidant Enzyme Expression
and Function in Vascular Cells
Sven Wassmann, Kerstin Wassmann, Georg Nickenig
AbstractPathological conditions that predispose to cardiovascular events, such as hypertension, hypercholesterolemia,
and diabetes, are associated with oxidative stress. These observations and further data derived from a plethora of
investigations provided accumulating evidence that oxidative stress is decisively involved in the pathogenesis of
endothelial dysfunction and atherosclerosis. Several enzymes expressed in vascular tissue contribute to production and
efficient degradation of reactive oxygen species, and enhanced activity of oxidant enzymes and/or reduced activity of
antioxidant enzymes may cause oxidative stress. Various agonists, pathological conditions, and therapeutic interventions
lead to modulated expression and function of oxidant and antioxidant enzymes, including NAD(P)H oxidase, endothelial
nitric oxide synthase, xanthine oxidase, myeloperoxidase, superoxide dismutases, catalase, thioredoxin reductase, and
glutathione peroxidase. Data from numerous studies underline the importance of dysregulated oxidant and antioxidant
enzymes for the development and progression of atherosclerotic disease in animal models and humans. Specific
pharmacological modulation of key enzymes involved in the propagation of oxidative stress rather than using direct
antioxidants may be an approach to reduce oxygen radical load in the vasculature and subsequent disease progression
in humans. This review focuses on the modulation of expression and activity of major antioxidant and oxidant enzymes
expressed in vascular cells. (Hypertension. 2004;44:381-386.)
Key Words: free radicals
oxidative stress
enzymes
gene regulation
atherosclerosis
T
he family of reactive oxygen species (ROS) includes
highly bioactive, short-living molecules that are derived
from reduction of molecular oxygen. Multiple enzyme sys-
tems use different substrates as sources of electrons to
produce a variety of ROS, including superoxide, hydroxyl
radical, hydrogen peroxide, peroxynitrite, hypochlorous acid,
and lipid radicals. Several enzymes are expressed in vascular
tissue that contribute to production as well as to degradation
of ROS (Figure 1). Under physiological conditions, ROS
formation and elimination are delicately balanced in the
vascular wall. However, enhanced activity of oxidant en-
zymes and/or reduced activity of antioxidant enzymes lead to
oxidative stress.
Oxidant Enzyme Systems
NAD(P)H Oxidase
A major source of ROS in vascular cells is the NAD(P)H
oxidase, which consists of the membrane subunits gp91phox
and p22phox and the cytosolic subunits p67phox, p47phox,
and the small GTPase rac1. The subunits assemble on
activation and form the functional enzyme, which after
electron transfer to molecular oxygen produces superoxide
radicals. In contrast to endothelial cells (EC) and adventitial
cells, gp91phox is expressed only at low levels in vascular
smooth muscle cells (VSMC) and is (functionally) replaced
by the homologue nox1. VSMC from resistance arteries,
however, express a functionally active gp91phox subunit.
Regulation of the expression levels and translocation of the
different NAD(P)H oxidase subunits leads to changes in
activity of the entire enzyme system.
Xanthine Oxidase
Xanthine oxidase catalyzes the oxidation of xanthine and
hypoxanthine during purine metabolism. This enzyme re-
duces molecular oxygen, leading to the formation of both
superoxide and hydrogen peroxide. Xanthine oxidase is
capable of producing large amounts of ROS under patholog-
ical conditions. The enzyme is not only expressed in vascular
cells but also circulates in the plasma and binds to endothelial
cell extracellular matrix.
Myeloperoxidase
Myeloperoxidase is a hemoprotein expressed in neutrophils
and monocytes, which is secreted during activation of these
cells and localizes in and around endothelial cells after
leukocyte degranulation. Myeloperoxidase uses hydrogen
peroxide to produce hypochlorous acid in a 2-step reaction
involving the redox reaction intermediate compound I. The
enzyme also exerts classic peroxidase activity and oxidizes a
variety of organic substrates to reactive oxygen intermediates
Received December 2, 2003; first decision December 26, 2003; revision accepted August 4, 2004.
From Klinik fur Innere Medizin III, Universitatsklinikum des Saarlandes, Homburg/Saar, Germany.
Correspondence to Prof. Georg Nickenig, Klinik fur Innere Medizin III, Universitatsklinikum des Saarlandes, D-66421 Homburg/Saar, Germany.
E-mail nickenig@med-in.uni-sb.de
2004 American Heart Association, Inc.
Hypertension is available at http://www.hypertensionaha.org DOI: 10.1161/01.HYP.0000142232.29764.a7
381
involving compound I and compound II formation. Important
substrates are tyrosine and nitrite, resulting in the formation
of tyrosyl radicals and nitrogen dioxide radicals, respectively.
The latter and other reactions involving hypochlorous acid
lead to formation of reactive nitrogen species and to protein
nitration, for example, nitrotyrosine formation.
Endothelial Nitric Oxide Synthase
Under physiological conditions, endothelial nitric oxide (NO)
synthase (eNOS, NOS III) produces NO, which interacts with
ROS. eNOS requires tetrahydrobiopterin as cofactor, which
has to be bound near the heme group in the oxygenase domain
for the electron transport to L-arginine to form L-citrulline and
NO. In the absence of L-arginine or tetrahydrobiopterin,
because of oxidative destruction of this cofactor or down-
regulation of GTP cyclohydrolase-1, which is the rate-
limiting enzyme in tetrahydrobiopterin production, the elec-
trons reduce molecular oxygen to superoxide instead of
producing NO. Dysfunctional or uncoupled eNOS can
produce large amounts of superoxide under certain patho-
physiological conditions.
Other Sources of ROS
Besides the described enzyme systems, there are other
sources of ROS production in vascular cells, including the
mitochondrial electron transport chain, cytochrome P450
isoenzymes, lipoxygenase, cyclooxygenase, heme oxygenase,
and glucose oxidase, which contribute to a variable extent to
the oxygen radical load of the vasculature.
Antioxidant Enzyme Systems
Superoxide Dismutases
The superoxide dismutases (SOD) are a major cellular de-
fense system against superoxide in all vascular cells. These
enzymes contain redox metals in the catalytic center and
dismutase superoxide radicals to hydrogen peroxide and
oxygen. Three different isoforms of SOD have been identi-
fied: the mitochondrial manganese-containing SOD (Mn-
SOD, SOD-2), the cytosolic copper/zinc-containing SOD
(CuZnSOD, SOD-1), and the extracellular SOD (ecSOD,
SOD-3), which is also a copper/zinc-containing enzyme that
is mainly produced and secreted by VSMC and binds to
glycosaminoglycans in the vascular extracellular matrix on
the endothelial cell surface. EcSOD plays an important role in
the regulation of the oxidant status in the vascular
interstitium.
Glutathione Peroxidase
Reduced glutathione plays a major role in the regulation of
the intracellular redox state of vascular cells by providing
reducing equivalents for many biochemical pathways. Gluta-
thione peroxidase (GPX) is a selenium-containing antioxidant
enzyme that effectively reduces hydrogen peroxide and lipid
peroxides to water and lipid alcohols, respectively, and in
turn oxidizes glutathione to glutathione disulfide. In the
absence of adequate GPX activity or glutathione levels,
hydrogen peroxide and lipid peroxides are not detoxified and
may be converted to hydroxyl radicals and lipid peroxyl
radicals, respectively, by transition metals (eg, Fe
2
). The
GPX/glutathione system is thought to be a major defense in
low-level oxidative stress.
Catalase
Catalase is an intracellular antioxidant enzyme that is mainly
located in cellular peroxisomes and to some extent in the
cytosol, which catalyzes the reaction of hydrogen peroxide to
water and molecular oxygen in a 2-step reaction involving
compound I. By removing hydrogen peroxide, it indirectly
detoxifies superoxide radicals, which are turned into hydro-
gen peroxide by SOD. The enzyme also has peroxidase
activity and reacts with organic peroxides and hydrogen
donors to water and organic alcohols. Catalase is very
effective in high-level oxidative stress and protects cells from
hydrogen peroxide produced within the cell. The enzyme is
especially important in the case of limited glutathione content
or reduced GPX activity and plays a significant role in the
development of tolerance to oxidative stress in the adaptive
response of cells.
Thioredoxin Reductase
Thioredoxin reductase is an antioxidant enzyme that partici-
pates in thiol-dependent cellular reductive processes. The
enzyme regenerates reduced thioredoxin, which serves as
reducing equivalent, and may also directly reduce lipid
hydroperoxides. In addition, thioredoxin and glutaredoxin,
which catalyzes glutathione-dependent disulfide reduction,
are reductants for plasma GPX, allowing the latter enzyme to
reduce hydroperoxides in surroundings with low levels of
glutathione. Moreover, thioredoxin was shown to enhance
MnSOD expression. The thioredoxin system may effectively
regenerate proteins that were inactivated by oxidative stress.
Regulation of Oxidant and Antioxidant
Enzyme Expression and Activity
There is a tight regulation of production and elimination of
ROS in the vasculature. However, several agonists and
pathological conditions may lead to dysregulated expression
and activity levels of the oxidant and antioxidant enzyme
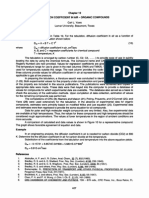
Figure 1. Oxidant and antioxidant enzymes in vascular cells.
Several enzymes expressed in vascular tissue contribute to pro-
duction and elimination of reactive oxygen species. O
2
indi-
cates superoxide; H
2
O
2
, hydrogen peroxide; ONOO
, peroxyni-
trite; OH
, hydroxyl radical; NO, nitric oxide; H
4
B,
tetrahydrobiopterin; GPX, glutathione peroxidase; SOD, super-
oxide dismutase; ecSOD, extracellular SOD; MnSOD, manga-
nese SOD; Cu/ZnSOD, copper/zinc SOD.
382 Hypertension October 2004
systems; in contrast, certain interventions and drugs may
decrease oxidative stress.
Angiotensin II
Angiotensin II (Ang II) is a potent stimulus for the production
of ROS in vascular cells. One of the main actions in this
context is the activation of the NAD(P)H oxidase. Ang II
enhances NAD(P)H oxidase activity within minutes of stim-
ulation because of changes in the assembly of the enzyme
subunits, but longer incubation periods for hours markedly
increase enzyme activity, mainly as a result of upregulated
subunit expression, including nox1 and rac1 in VSMC,
p22phox, gp91phox, p67phox, and p47phox in EC and
VSMC of resistance vessels, and p67phox in fibroblasts.
1,2
Activation and membrane translocation of rac1 seem to be
particularly important for the activation of the enzyme com-
plex. Ang II stimulation causes enhanced expression, GTPase
activity, and membrane translocation of rac1 in VSMC.
35
In animals made hypertensive by Ang II infusion, vascular
superoxide production, NAD(P)H oxidase activity, and ex-
pression levels of the p22phox, gp91phox, p67phox, and
nox1 subunits were enhanced. Further experiments with SOD
injection or genetic disruption of p47phox demonstrated the
importance of NAD(P)H oxidase-mediated superoxide pro-
duction for Ang IIinduced hypertension.
1,6
In other models
of hypertension, an increased NAD(P)H oxidase activity was
found, which was either associated with increased Ang II
levels (2-kidney1-clip rats) or could be normalized by
treatment with an AT
1
receptor antagonist (spontaneously
hypertensive rats).
7,8
Ang II infusion has also been shown to upregulate vascular
eNOS expression, which was accompanied with uncoupling
of the enzyme, reduced NO production, and enhanced super-
oxide release.
1
In a genetic model of endogenous Ang II
overproduction, enhanced activity of vascular and renal
xanthine oxidase was found.
9
These studies indicate that
besides NAD(P)H oxidase, other enzymes contribute to Ang
IIinduced oxidative stress in the vasculature, as well. Prob-
ably as an adaptive negative feedback mechanism, Ang II
increases vascular expression of ecSOD in vitro and in vivo.
10
Finally, modulation of AT
1
receptor expression levels by
various agonists influences Ang IIinduced ROS production
in vascular cells.
5
Growth Factors and Cytokines
Many growth factors are known to influence oxidant and
antioxidant enzyme function. Platelet-derived growth factor,
epidermal growth factor, transforming growth factor-, and
thrombin lead to increased subunit expression and activity of
the NAD(P)H oxidase and to decreased ecSOD expression in
VSMC.
11
The proinflammatory cytokines interferon-,
interleukin-1, and especially tumor necrosis factor- seem to
promote oxidant effects in vascular cells by activating
NAD(P)H oxidase and xanthine oxidase, although there are
differential regulations of antioxidant enzymes, for example,
ecSOD, MnSOD, and GPX, presumably because of compen-
satory mechanisms.
12
During endotoxemia, lipopolysaccha-
rides induce oxidative stress by enhancing xanthine oxidase
and NAD(P)H oxidase expression and activity, and superox-
ide, hydrogen peroxide, and peroxynitrite formation.
13
Reactive Oxygen Species
ROS not only are products of oxidant enzymes but also are
involved in the regulation of oxidant and antioxidant en-
zymes. Superoxide enhances the activity of myeloperoxidase
and may activate xanthine oxidase in EC.
14
The reaction
product of superoxide and NO, peroxynitrite, leads to oxida-
tive destruction of tetrahydrobiopterin, which causes uncou-
pling of eNOS, as demonstrated in various animal models,
including Ang IIinduced hypertension, DOCA-salt hyper-
tension, and SHR.
1,15
However, peroxynitrite may induce
thioredoxin reductase expression in EC, possibly as a protec-
tive mechanism during oxidative stress.
16
Hydrogen peroxide
is capable of activating NAD(P)H oxidase and reducing the
activity of CuZnSOD and ecSOD, but may also increase the
expression of catalase and eNOS.
1719
Nitric Oxide
NO rapidly reacts with ROS, and the scavenging of ROS as
well as the formation of new radicals by these reactions
influence cellular function of vascular cells. NO leads to
upregulation of ecSOD and MnSOD in VSMC and inhibits
xanthine oxidase activity in hypoxia.
20
Lipids
Hypercholesterolemia is associated with increased oxidative
stress, eNOS uncoupling occurs, and NAD(P)H oxidase
activity is increased. Low-density lipoprotein (LDL) choles-
terol and oxidized LDL upregulate nox1 and gp91phox
expression and NAD(P)H oxidase activity. As an adaptive
process, increased MnSOD and catalase expression were
found.
19
Hormones
Estrogens act antioxidative in vascular cells. 17-Estradiol
decreases NAD(P)H oxidase activity by downregulation of
rac1 expression and activity (VSMC) and gp91phox expres-
sion (EC), and enhances eNOS expression and activity in
EC.
4,21
Similar effects were seen with the selective estrogen
receptor modulator raloxifene.
22
Furthermore, 17-estradiol
was shown to enhance expression and activity of MnSOD and
ecSOD in VSMC, and to induce the thioredoxin system in EC
by increasing thioredoxin, glutaredoxin, and thioredoxin re-
ductase expression.
23,24
In contrast to estrogen, progesterone
increases ROS production, decreases the expression of Mn-
SOD and ecSOD, and abolishes the effects of estrogen on
SOD expression and ROS production in VSMC (unpublished
observations). In humans, progesterone was reported to coun-
teract the beneficial effects of estrogen on endothelial
function.
25
Glucose and Insulin
Data from animal and human studies show that diabetes
mellitus is associated with increased oxidative stress. In
cultured EC and VSMC, NAD(P)H oxidase activity and
superoxide production are enhanced by high glucose levels
involving protein kinase C activation, and an upregulation of
Wassmann et al Regulation of Oxidant and Antioxidant Enzymes 383
p22phox expression was found in isolated arteries stimulated
with high glucose.
26
In experimental models of diabetes, such
as the streptozotocin-treated rat (model of type 1 diabetes),
high glucose levels are associated with enhanced vascular
NAD(P)H oxidase activity and superoxide production, in-
creased expression of gp91phox and p22phox, protein kinase
C activation, reduced glutathione levels, enhanced xanthine
oxidase activity, dysfunctional eNOS, and impaired endothe-
lial function.
27,28
In blood vessels from patients with type 2
diabetes, an upregulation of p22phox, p47phox, and p67phox,
and an enhanced NAD(P)H oxidase activity were found.
29
In
genetically diabetic rats (model of type 2 diabetes), a similar
activation of the NAD(P)H oxidase was demonstrated.
30
Taken together, metabolic changes associated with diabetes
mellitus lead to a strong activation of several oxidant enzyme
systems in the vasculature.
Drugs
Antioxidants such as vitamin C, vitamin E, probucol, tiron, or
N-acetylcysteine directly scavenge and inactivate ROS rather
than interfering with expression and function of oxidant and
antioxidant enzymes.
Allopurinol and its active metabolite oxypurinol are direct
inhibitors of xanthine oxidase and suppress xanthine oxidase-
mediated ROS production in vascular cells. Oxypurinol
decreased ROS production and lowered blood pressure levels
in diabetic animals and SHR. In addition, allopurinol and
oxypurinol were shown to reduce oxidative stress and to
improve endothelial function in diabetic, hyperuricemic, and
hypercholesterolemic patients.
28,31,32
HMG-CoA reductase inhibitors (statins) block not only
cholesterol synthesis but also isoprenoid metabolism, which
is needed for posttranslational modifications of numerous
regulatory proteins, such as small GTP-binding proteins.
Statins lead to upregulation of eNOS expression and activity
in EC, and to increased expression and activity of catalase in
VSMC.
33
Otherwise, statins inhibit ROS production by re-
duction of NAD(P)H oxidase activity, decreased expression
of nox1 in VSMC and gp91phox, p22phox, and p47phox in
EC, and inhibition of activity and geranylgeranylation-
dependent membrane translocation of rac1 GTPase.
5,33
Taken
together, the described effects of statins result in decreased
vascular ROS production, increased NO bioactivity, and
improvement of endothelial function.
Peroxisome proliferator-activated receptors (PPAR) are
ligand-activated transcription factors, which have been shown to
mediate anti-inflammatory actions in vascular cells. Activators
of PPAR (lipid-lowering fibrate derivatives) and PPAR (an-
tidiabetic thiazolidinediones) reduce the expression of p22phox
and p47phox, decrease NAD(P)H oxidase activity and ROS
production, and increase CuZnSOD and catalase expression and
NO release in EC.
34,35
Moreover, PPAR agonists diminish
ROS production in Ang II-infused rats and decrease p22phox
expression and improve endothelial function in diabetic rats.
36
These data show that PPAR agonists may exert favorable effects
on the oxidant status of vascular cells.
Angiotensin-converting enzyme inhibitors and AT
1
receptor
antagonists are inhibitors of the renin-angiotensin system that do
not act as direct antioxidants. However, these drugs inhibit the
actions of Ang II and thus block the activation of oxidant
enzymes and redox-sensitive genes by Ang II (see Angiotensin
II section of this article). In many cell culture and animal studies,
their antioxidant potential was demonstrated, associated with
improvement of endothelial function and inhibition of athero-
sclerotic lesion formation in the absence of blood pressure
reduction.
8,37
Antioxidant effects and improvement of vascular
function were confirmed in human studies.
38
Other antihypertensive drugs, namely -blockers and cal-
cium channel antagonists, have been shown to exert antioxi-
dative properties as well. Third-generation -blockers like
carvedilol and nebivolol may enhance NO release in EC,
increase vascular glutathione content, inhibit ROS formation,
and reduce lipid peroxidation.
39
Several calcium channel
blockers were shown to inhibit oxidation of LDL and other
lipids in animals and humans. For example, nifedipine in-
creases NO bioavailability by decreased ROS formation in
EC and enhances MnSOD expression in VSMC.
40
Oxidative Stress and Atherosclerosis
Oxidative stress may lead to many cellular events, such as
inactivation of NO, oxidative modifications of DNA and
proteins, lipid oxidation, enhanced mitogenicity and apopto-
sis of vascular cells, and increased expression and activation
of redox-sensitive genes, such as the receptor for oxidized
LDL, adhesion molecules, chemotaxis factors, proinflamma-
tory cytokines, regulators of cell cycle progression, and
matrix metalloproteinases (Figure 2). Several cardiovascular
risk factors are associated with oxidative stress and dysregu-
lated expression and activity of oxidant and antioxidant
enzymes, including arterial hypertension, hypercholesterol-
emia, diabetes mellitus, and cigarette smoking, and the
described effects of ROS and impaired NO bioactivity in
vascular cells contribute to the development and progression
of atherosclerosis at all stages of the disease (Figure 2).
Increased levels of ROS were demonstrated in all layers of
the diseased arterial wall and within the atherosclerotic
plaque. Many studies demonstrated an upregulation of several
vascular NAD(P)H oxidase subunits and increased enzyme
activity in atherosclerotic animals and humans and after
vascular injury,
4143
and genetic disruption of p47phox strik-
ingly inhibited atherosclerotic lesion formation in mice.
44
Besides dysregulated NAD(P)H oxidase, increased xanthine
oxidase activity and reduced ecSOD activity were found in
coronary arteries and the plasma of patients with coronary
artery disease.
42,45
Taken together, data from numerous stud-
ies underscore the notion that modulation of oxidant and
antioxidant enzymes, leading to oxidative stress, plays an
important role in the pathogenesis of atherosclerotic disease.
Recently, low levels of GPX activity and elevated levels of
myeloperoxidase were shown to be an independent risk factor
for cardiovascular events in patients with coronary artery
disease and in patients presenting with chest pain.
46,47
Perspectives
From the available data, it may be assumed that reduction of
oxidative stress and restoration of NO bioactivity are impor-
tant mechanisms for the improvement of endothelial dysfunc-
tion, the treatment of more advanced stages of atherosclero-
384 Hypertension October 2004
sis, and for the treatment of restenosis after vascular injury.
Small clinical trials with antioxidants like vitamins E and C
demonstrated improvements of endothelial function and sur-
rogate parameters of atherosclerosis.
48
However, recent large
clinical trials with antioxidant vitamins (mostly vitamin E)
did not show therapeutic benefits concerning cardiovascular
events and mortality.
49
The lack of effect of these substances
on hard end points may be explained by pharmacokinetic and
pharmacodynamic properties. In contrast to local treatment
(eg, intraarterial infusion), antioxidant vitamins may be
(partly) inactivated after oral treatment before they reach the
vasculature, thus producing only modest increases of their
plasma and tissue concentrations. Vitamin E concentrates
predominantly in cellular lipid bilayers and lipoproteins, and
may therefore not interfere appropriately with ROS accumu-
lating in the cytoplasm or the interstitial space. This vitamin
does not react as rapidly with superoxide as does NO, thus
leading to incomplete prevention of NO inactivation. Impor-
tantly, the antioxidant vitamins E and C may act pro-oxidant
themselves by being converted into tocopheroxyl and ascor-
byl radicals, respectively, which may enhance lipid peroxi-
dation. In addition, antioxidants may be more beneficial in
primary prevention rather than in patients with advanced
atherosclerotic disease. However, there is evidence that some
drugs that do not act as direct antioxidants, for example,
statins and AT
1
receptor antagonists, exert their therapeutic
benefits at least in part through antioxidant actions. This may
have several implications. First, testing diseased individuals
for markers of oxidative stress could be used for risk
stratification. Treatment with potent antioxidants may poten-
tially be beneficial in this group of patients. Second, given the
fact that dysregulated oxidant and antioxidant enzyme ex-
pression and function is found in patients with cardiovascular
risk factors and manifested atherosclerotic disease (Figure 2),
specific pharmacological modulation of key enzymes, such as
inhibition of the vascular NAD(P)H oxidase, may be an
effective approach to reduce vascular oxidative stress and
subsequent disease progression in humans that is potentially
more powerful than the use of systemic antioxidants. These
important issues should be clarified in future studies.
References
1. Mollnau H, Wendt M, Szocs K, Lasse`gue B, Schulz E, Oelze M, Li H,
Bodenschatz M, August M, Kleschyov AL, Tsilimingas N, Walter U,
Forstermann U, Meinertz T, Griendling K, Munzel T. Effects of angio-
tensin II infusion on the expression and function of NAD(P)H oxidase
and components of nitric oxide/cGMP signaling. Circ Res. 2002;90:
E58E65.
2. Touyz RM, Chen X, Tabet F, Yao G, He G, Quinn MT, Pagano PJ,
Schiffrin EL. Expression of a functionally active gp91phox-containing
neutrophil-type NAD(P)H oxidase in smooth muscle cells from human
resistance arteries: regulation by angiotensin II. Circ Res. 2002;90:
12051213.
3. Seshiah PN, Weber DS, Rocic P, Valppu L, Taniyama Y, Griendling KK.
Angiotensin II stimulation of NAD(P)H oxidase activity: upstream
mediators. Circ Res. 2002;91:406413.
4. Laufs U, Adam O, Strehlow K, Wassmann S, Konkol C, Laufs K,
Schmidt W, Bohm M, Nickenig G. Down-regulation of Rac-1 GTPase by
Estrogen. J Biol Chem. 2003;278:59565962.
5. Wassmann S, Laufs U, Baumer AT, Muller K, Konkol C, Sauer H, Bohm
M, Nickenig G. Inhibition of geranylgeranylation reduces angiotensin
II-mediated free radical production in vascular smooth muscle cells:
involvement of angiotensin AT1 receptor expression and Rac1 GTPase.
Mol Pharmacol. 2001;59:646654.
6. Landmesser U, Cai H, Dikalov S, McCann L, Hwang J, Jo H, Holland
SM, Harrison DG. Role of p47(phox) in vascular oxidative stress and
hypertension caused by angiotensin II. Hypertension. 2002;40:511515.
7. Heitzer T, Wenzel U, Hink U, Krollner D, Skatchkov M, Stahl RA,
MacHarzina R, Brasen JH, Meinertz T, Munzel T. Increased NAD(P)H
oxidase-mediated superoxide production in renovascular hypertension:
evidence for an involvement of protein kinase C. Kidney Int. 1999;55:
252260.
8. Zalba G, Beaumont FJ, San Jose G, Fortuno A, Fortuno MA, Etayo JC,
Diez J. Vascular NADH/NADPH oxidase is involved in enhanced
superoxide production in spontaneously hypertensive rats. Hypertension.
2000;35:10551061.
9. Mervaala EM, Cheng ZJ, Tikkanen I, Lapatto R, Nurminen K, Vapaatalo
H, Muller DN, Fiebeler A, Ganten U, Ganten D, Luft FC. Endothelial
dysfunction and xanthine oxidoreductase activity in rats with human renin
and angiotensinogen genes. Hypertension. 2001;37:414418.
10. Fukai T, Siegfried MR, Ushio-Fukai M, Griendling KK, Harrison DG.
Modulation of extracellular superoxide dismutase expression by angio-
tensin II and hypertension. Circ Res. 1999;85:2328.
Figure 2. Pathophysiology of oxidative
stress and relevance for vascular dis-
ease. Cardiovascular risk factors that
predispose to atherogenesis are associ-
ated with oxidative stress. Several ago-
nists and pathological conditions lead to
dysregulated expression and function of
oxidant and antioxidant enzymes, result-
ing in enhanced free radical load in the
vasculature. Oxidative stress promotes
pathological cellular events, which are
involved in the development and pro-
gression of atherosclerosis at all stages
of the disease. oxLDL indicates oxidized
low-density lipoprotein; MMP, matrix
metalloproteinase.
Wassmann et al Regulation of Oxidant and Antioxidant Enzymes 385
11. Stralin P, Marklund SL. Vasoactive factors and growth factors alter
vascular smooth muscle cell EC-SOD expression. Am J Physiol Heart
Circ Physiol. 2001;281:H1621H1629.
12. Stralin P, Marklund SL. Multiple cytokines regulate the expression of
extracellular superoxide dismutase in human vascular smooth muscle
cells. Atherosclerosis. 2000;151:433441.
13. Brandes RP, Koddenberg G, Gwinner W, Kim D, Kruse HJ, Busse R,
Mugge A. Role of increased production of superoxide anions by
NAD(P)H oxidase and xanthine oxidase in prolonged endotoxemia.
Hypertension. 1999;33:12431249.
14. McNally JS, Davis ME, Giddens DP, Saha A, Hwang J, Dikalov S, Jo H,
Harrison DG. Role of xanthine oxidoreductase and NAD(P)H oxidase in
endothelial superoxide production in response to oscillatory shear stress.
Am J Physiol Heart Circ Physiol. 2003;285:H2290H2297.
15. Landmesser U, Dikalov S, Price SR, McCann L, Fukai T, Holland SM,
Mitch WE, Harrison DG. Oxidation of tetrahydrobiopterin leads to
uncoupling of endothelial cell nitric oxide synthase in hypertension.
J Clin Invest. 2003;111:12011209.
16. Park YS, Fujiwara N, Koh YH, Miyamoto Y, Suzuki K, Honke K,
Taniguchi N. Induction of thioredoxin reductase gene expression by
peroxynitrite in human umbilical vein endothelial cells. Biol Chem. 2002;
383:683691.
17. Drummond GR, Cai H, Davis ME, Ramasamy S, Harrison DG. Tran-
scriptional and posttranscriptional regulation of endothelial nitric oxide
synthase expression by hydrogen peroxide. Circ Res. 2000;86:347354.
18. Li WG, Miller FJ, Jr., Zhang HJ, Spitz DR, Oberley LW, Weintraub NL.
H(2)O(2)-induced O(2) production by a non-phagocytic NAD(P)H
oxidase causes oxidant injury. J Biol Chem. 2001;276:2925129256.
19. Meilhac O, Zhou M, Santanam N, Parthasarathy S. Lipid peroxides
induce expression of catalase in cultured vascular cells. J Lipid Res.
2000;41:12051213.
20. Fukai T, Siegfried MR, Ushio-Fukai M, Cheng Y, Kojda G, Harrison DG.
Regulation of the vascular extracellular superoxide dismutase by nitric
oxide and exercise training. J Clin Invest. 2000;105:16311639.
21. Wagner AH, Schroeter MR, Hecker M. 17beta-estradiol inhibition of
NADPH oxidase expression in human endothelial cells. FASEB J. 2001;
15:21212130.
22. Wassmann S, Laufs U, Stamenkovic D, Linz W, Stasch JP, Ahlbory K,
Rosen R, Bohm M, Nickenig G. Raloxifene improves endothelial dys-
function in hypertension by reduced oxidative stress and enhanced nitric
oxide production. Circulation. 2002;105:20832091.
23. Ejima K, Nanri H, Araki M, Uchida K, Kashimura M, Ikeda M. 17beta-
estradiol induces protein thiol/disulfide oxidoreductases and protects
cultured bovine aortic endothelial cells from oxidative stress. Eur J
Endocrinol. 1999;140:608613.
24. Strehlow K, Rotter S, Wassmann S, Adam O, Grohe C, Laufs K, Bohm
M, Nickenig G. Modulation of antioxidant enzyme expression and
function by estrogen. Circ Res. 2003;93:170177.
25. Wakatsuki A, Okatani Y, Ikenoue N, Fukaya T. Effect of medroxypro-
gesterone acetate on endothelium-dependent vasodilation in postmeno-
pausal women receiving estrogen. Circulation. 2001;104:17731778.
26. Inoguchi T, Li P, Umeda F, Yu HY, Kakimoto M, Imamura M, Aoki T,
Etoh T, Hashimoto T, Naruse M, Sano H, Utsumi H, Nawata H. High
glucose level and free fatty acid stimulate reactive oxygen species pro-
duction through protein kinase C-dependent activation of NAD(P)H
oxidase in cultured vascular cells. Diabetes. 2000;49:19391945.
27. Hink U, Li H, Mollnau H, Oelze M, Matheis E, Hartmann M, Skatchkov
M, Thaiss F, Stahl RA, Warnholtz A, Meinertz T, Griendling K, Harrison
DG, Forstermann U, Munzel T. Mechanisms underlying endothelial dys-
function in diabetes mellitus. Circ Res. 2001;88:E14E22.
28. Matsumoto S, Koshiishi I, Inoguchi T, Nawata H, Utsumi H. Confir-
mation of superoxide generation via xanthine oxidase in streptozotocin-
induced diabetic mice. Free Radic Res. 2003;37:767772.
29. Guzik TJ, Mussa S, Gastaldi D, Sadowski J, Ratnatunga C, Pillai R,
Channon KM. Mechanisms of increased vascular superoxide production
in human diabetes mellitus: role of NAD(P)H oxidase and endothelial
nitric oxide synthase. Circulation. 2002;105:16561662.
30. Kim YK, Lee MS, Son SM, Kim IJ, Lee WS, Rhim BY, Hong KW, Kim
CD. Vascular NADH oxidase is involved in impaired endothelium-
dependent vasodilation in OLETF rats, a model of type 2 diabetes.
Diabetes. 2002;51:522527.
31. Desco MC, Asensi M, Marquez R, Martinez-Valls J, Vento M, Pallardo
FV, Sastre J, Vina J. Xanthine oxidase is involved in free radical pro-
duction in type 1 diabetes: protection by allopurinol. Diabetes. 2002;51:
11181124.
32. Doehner W, Schoene N, Rauchhaus M, Leyva-Leon F, Pavitt DV,
Reaveley DA, Schuler G, Coats AJ, Anker SD, Hambrecht R. Effects of
xanthine oxidase inhibition with allopurinol on endothelial function and
peripheral blood flow in hyperuricemic patients with chronic heart
failure: results from 2 placebo-controlled studies. Circulation. 2002;105:
26192624.
33. Wassmann S, Laufs U, Muller K, Konkol C, Ahlbory K, Baumer AT,
Linz W, Bohm M, Nickenig G. Cellular antioxidant effects of atorvastatin
in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2002;22:300305.
34. Calnek DS, Mazzella L, Roser S, Roman J, Hart CM. Peroxisome
proliferator-activated receptor gamma ligands increase release of nitric
oxide from endothelial cells. Arterioscler Thromb Vasc Biol. 2003;23:
5257.
35. Inoue I, Goto S, Matsunaga T, Nakajima T, Awata T, Hokari S, Komoda
T, Katayama S. The ligands/activators for peroxisome proliferator-acti-
vated receptor alpha (PPARalpha) and PPARgamma increase
Cu2,Zn2-superoxide dismutase and decrease p22phox message
expressions in primary endothelial cells. Metabolism. 2001;50:311.
36. Diep QN, Amiri F, Touyz RM, Cohn JS, Endemann D, Neves MF,
Schiffrin EL. PPARalpha activator effects on Ang IIinduced vascular
oxidative stress and inflammation. Hypertension. 2002;40:866871.
37. Warnholtz A, Nickenig G, Schulz E, MacHarzina R, Brasen JH,
Skatchkov M, Heitzer T, Stasch JP, Griendling KK, Harrison DG, Bohm
M, Meinertz T, Mu nzel T. Increased NADH-oxidase-mediated
superoxide production in the early stages of atherosclerosis: evidence for
involvement of the renin-angiotensin system. Circulation. 1999;99:
20272033.
38. Wassmann S, Hilgers S, Laufs U, Bohm M, Nickenig G. Angiotensin II
type 1 receptor antagonism improves hypercholesterolemia-associated
endothelial dysfunction. Arterioscler Thromb Vasc Biol. 2002;22:
12081212.
39. Kalinowski L, Dobrucki LW, Szczepanska-Konkel M, Jankowski M,
Martyniec L, Angielski S, Malinski T. Third-generation beta-blockers
stimulate nitric oxide release from endothelial cells through ATP efflux:
a novel mechanism for antihypertensive action. Circulation. 2003;107:
27472752.
40. Berkels R, Egink G, Marsen TA, Bartels H, Roesen R, Klaus W. Nifed-
ipine increases endothelial nitric oxide bioavailability by antioxidative
mechanisms. Hypertension. 2001;37:240245.
41. Sorescu D, Weiss D, Lasse`gue B, Clempus RE, Szocs K, Sorescu GP,
Valppu L, Quinn MT, Lambeth JD, Vega JD, Taylor WR, Griendling KK.
Superoxide production and expression of nox family proteins in human
atherosclerosis. Circulation. 2002;105:14291435.
42. Spiekermann S, Landmesser U, Dikalov S, Bredt M, Gamez G, Tatge H,
Reepschlager N, Hornig B, Drexler H, Harrison DG. Electron spin res-
onance characterization of vascular xanthine and NAD(P)H oxidase
activity in patients with coronary artery disease: relation to endothelium-
dependent vasodilation. Circulation. 2003;107:13831389.
43. Szocs K, Lasse`gue B, Sorescu D, Hilenski LL, Valppu L, Couse TL,
Wilcox JN, Quinn MT, Lambeth JD, Griendling KK. Upregulation of
Nox-based NAD(P)H oxidases in restenosis after carotid injury. Arte-
rioscler Thromb Vasc Biol. 2002;22:2127.
44. Barry-Lane PA, Patterson C, van der MM, Hu Z, Holland SM, Yeh ET,
Runge MS. p47phox is required for atherosclerotic lesion progression in
ApoE(/) mice. J Clin Invest. 2001;108:15131522.
45. Landmesser U, Merten R, Spiekermann S, Buttner K, Drexler H, Hornig
B. Vascular extracellular superoxide dismutase activity in patients with
coronary artery disease: relation to endothelium-dependent vasodilation.
Circulation. 2000;101:22642270.
46. Blankenberg S, Rupprecht HJ, Bickel C, Torzewski M, Hafner G, Tiret L,
Smieja M, Cambien F, Meyer J, Lackner KJ. Glutathione peroxidase 1
activity and cardiovascular events in patients with coronary artery
disease. N Engl J Med. 2003;349:16051613.
47. Brennan ML, Penn MS, Van Lente F, Nambi V, Shishehbor MH, Aviles
RJ, Goormastic M, Pepoy ML, McErlean ES, Topol EJ, Nissen SE,
Hazen SL. Prognostic value of myeloperoxidase in patients with chest
pain. N Engl J Med. 2003;349:15951604.
48. Fang JC, Kinlay S, Beltrame J, Hikiti H, Wainstein M, Behrendt D, Suh
J, Frei B, Mudge GH, Selwyn AP, Ganz P. Effect of vitamins C and E on
progression of transplant-associated arteriosclerosis: a randomised trial.
Lancet. 2002;359:11081113.
49. Yusuf S, Dagenais G, Pogue J, Bosch J, Sleight P. Vitamin E supple-
mentation and cardiovascular events in high-risk patients. The Heart
Outcomes Prevention Evaluation Study Investigators. N Engl J Med.
2000;342:154160.
386 Hypertension October 2004
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Formulas 1 AccordDocument86 pagesFormulas 1 AccordRakesh Karun100% (14)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Thiazolopyrimidines: A Retrospective Study of Synthesis, Structure-Activity Relationship and Diverse Pharmacological ActionsDocument12 pagesThiazolopyrimidines: A Retrospective Study of Synthesis, Structure-Activity Relationship and Diverse Pharmacological ActionsRajat GoyalPas encore d'évaluation
- Difusividad Aire OrganicosDocument90 pagesDifusividad Aire OrganicosPath VallejoPas encore d'évaluation
- Bases Nitrogenadas InglésDocument29 pagesBases Nitrogenadas InglésAndrea CardenasPas encore d'évaluation
- Physical Science Q2 Module 7Document23 pagesPhysical Science Q2 Module 7Earl InacayPas encore d'évaluation
- PROTEIN METABOLISM Dea Farha Fira Darson FineDocument44 pagesPROTEIN METABOLISM Dea Farha Fira Darson FineFarhati MardhiyahPas encore d'évaluation
- Stock 09.05.23Document10 pagesStock 09.05.23Kasi HumasPas encore d'évaluation
- CBSE Class 10 Chemistry Worksheet - Carbon and Its CompoundDocument4 pagesCBSE Class 10 Chemistry Worksheet - Carbon and Its CompoundRaghav GuptaPas encore d'évaluation
- Oman - Drug - Prices - 06 - 04 - 2013Document488 pagesOman - Drug - Prices - 06 - 04 - 2013Anuj Mairh73% (11)
- Antiinflammatory Drugs: Toya AriawanDocument27 pagesAntiinflammatory Drugs: Toya Ariawanlast100% (1)
- H - NMR Spectroscopy WorksheetDocument11 pagesH - NMR Spectroscopy WorksheetAldyan FaturahmanPas encore d'évaluation
- B 28050253Document546 pagesB 28050253Madalina HerPas encore d'évaluation
- Study Guide Unit 2.1 - Dna, Rna, & ProteinsDocument31 pagesStudy Guide Unit 2.1 - Dna, Rna, & ProteinsGracePas encore d'évaluation
- Synthesis of Schiff Bases by Organic Free Solvent MethodDocument4 pagesSynthesis of Schiff Bases by Organic Free Solvent Methodlox agencyPas encore d'évaluation
- Catálogo DescripciónDocument7 pagesCatálogo DescripciónAlexis RuanoPas encore d'évaluation
- Oligosaccharides. Polysaccharides. Terpenes.Document182 pagesOligosaccharides. Polysaccharides. Terpenes.Umar M abubakarPas encore d'évaluation
- Organic (Introduction 1&2)Document10 pagesOrganic (Introduction 1&2)Shahd WaelPas encore d'évaluation
- Pharmacology Step 1 For USMLEDocument3 pagesPharmacology Step 1 For USMLEraj_1041100% (1)
- Write An Essay On The Importance of Functions of Enzymes in OrganismsDocument3 pagesWrite An Essay On The Importance of Functions of Enzymes in OrganismsXx Jasmine XxPas encore d'évaluation
- USANA CRB CoQ10BioavailabilityDocument3 pagesUSANA CRB CoQ10BioavailabilityMhay AntenorPas encore d'évaluation
- Cuaderno Trabajo1 Qu334 2019-6Document42 pagesCuaderno Trabajo1 Qu334 2019-6Anthony Carhuaz AncheliaPas encore d'évaluation
- Chapter 14 Test BankDocument20 pagesChapter 14 Test BankquynhphamftPas encore d'évaluation
- AtorvastatinDocument27 pagesAtorvastatinBolgam PradeepPas encore d'évaluation
- Colour Reaction of Amino AcidsDocument27 pagesColour Reaction of Amino AcidsJacqueline Ann71% (7)
- Fat and Protein MetabolismDocument2 pagesFat and Protein MetabolismMark Zedrix MediarioPas encore d'évaluation
- Aliphatic HydrocarbonsDocument17 pagesAliphatic HydrocarbonsZunaira NoreenPas encore d'évaluation
- Chapter 19. Aldehydes and Ketones: Nucleophilic Addition ReactionsDocument45 pagesChapter 19. Aldehydes and Ketones: Nucleophilic Addition ReactionsPra YogaPas encore d'évaluation
- GENIRICDocument2 pagesGENIRICŃtǿxPas encore d'évaluation
- Akotop P70 - PDSDocument2 pagesAkotop P70 - PDSMohamed Zaki GhonemPas encore d'évaluation
- Sikemia Coupling Agents CatalogueDocument30 pagesSikemia Coupling Agents CataloguearunabhagnihotriPas encore d'évaluation