Académique Documents
Professionnel Documents
Culture Documents
Crit Care Nurse 2006 Broscious 17 27
Transféré par
Galang Oktavianto Sujatmiko0 évaluation0% ont trouvé ce document utile (0 vote)
57 vues13 pagesfile pdf
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentfile pdf
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
57 vues13 pagesCrit Care Nurse 2006 Broscious 17 27
Transféré par
Galang Oktavianto Sujatmikofile pdf
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 13
Sharon K.
Broscious and Judith Castagnola
Chronic Kidney Disease: Acute Manifestations and Role of Critical Care Nurses
Published online http://www.cconline.org
2006 American Association of Critical-Care Nurses
2006, 26:17-27. Crit Care Nurse
http://ccn.aacnjournals.org/subscriptions
Subscription Information
http://ccn.aacnjournals.org/misc/ifora.xhtml
Information for authors
www.editorialmanager.com/ccn
Submit Manuscript
http://ccn.aacnjournals.org/subscriptions/etoc.xhtml
E-mail alerts
362-2049. Copyright 2011 by AACN. All rights reserved.
Telephone: (800) 899-1712, (949) 362-2050, ext. 532. Fax: (949)
The InnoVision Group 101 Columbia, Aliso Viejo, CA 92656.
by American Association ofCritical-Care Nurses, published bi-monthly
Critical Care Nurse is the official peer-reviewed clinical journal of the
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
http://ccn.aacnjournals.org CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 17
Sharon K. Broscious is an associate
professor in the School of Nursing at
Troy University, Atlantic Region, in
Norfolk, Va.
Judith Castagnola is a facility adminis-
trator at DaVita Peninsula Dialysis in
Newport News, Va.
Despite the improved diagno-
sis and treatment of kidney disease,
late diagnosis with resultant perma-
nent damage to the kidneys still
occurs. A work group established by
the National Kidney Foundation, the
Kidney Disease Outcome Quality
Initiative (KDOQI), was asked to
develop clinical practice guidelines
and a uniform classification system
for chronic kidney disease (CKD).
CKD is a public health issue because
of its increasing incidence and the
high cost of interventions.
1
An addi-
tional concern is the increasing inci-
dence of kidney disease in African
Americans and Native Americans.
2
According to the 2004 report
from the US Renal Data System,
3
the
number of patients with CKD receiv-
ing therapy in 2002 was 431284.
This number is a 4.6% increase over
the number for the year 2001. The
adjusted rate for CKD was 1435
cases per million population72%
of patients were undergoing dialysis;
the other 122374 had a functioning
transplant. The adjusted rate of
CKD for the white population was
1060 cases per million; for the African
American population, 4467 cases per
million; and for the Native American
population, 2569 cases per million.
In 2002, Medicare expenses for
CKD treatment increased 11% over
the level in 2001; Medicare expenses
were $17 billion and non-Medicare
expenses were $8.2 billion. From
the individual perspective, Medicare
costs per year are approximately
$53000, with deductibles and copay-
ments bringing the total to $63000
per year. Total cost for the entire CKD
program was approximately $25.2
billion at the end of 2002.
3
The KDOQI has identified 5 stages
of kidney failure (Table 1) on the basis
of glomerular filtration rate (GFR).
4
Normal GFR in men is 125 to 150
mL/min per 1.73 m
2
(1.73 m
2
is
considered the standard normal body
surface area). Chronic kidney failure
Chronic Kidney
Disease
Acute Manifestations
and Role of Critical
Care Nurses
CoverArticle
Authors
* This article has been designated for CE credit.
A closed-book, multiple-choice examination fol-
lows this article, which tests your knowledge of
the following objectives:
1. Identify the expected outcomes of patients
with chronic kidney disease (CKD)
2. Describe the pathophysiology of CKD
3. Discuss the impact of CKD in relation to
body systems
Sharon K. Broscious, RN, DSN, CCRN
Judith Castagnola, RN, MSN
Corresponding author: Sharon K. Broscious, Troy Uni-
versity, Atlantic Region, 5425 Robin Hood Rd, Ste B1,
Norfolk, VA 23513. (e-mail: sbroscious@troy.edu)
To purchase electronic or print reprints, contact The
InnoVision Group, 101 Columbia, Aliso Viejo, CA
92656. Phone, (800) 809-2273 or (949) 362-2050
(ext 532); fax, (949) 362-2049; e-mail,
reprints@aacn.org.
CEContinuing Education
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
is defined by the KDOQI as having
kidney damage lasting for 3 months
or more or having a GFR less than
60 mL/min per 1.73 m
2
for 3 months
or more, with or without kidney dam-
age.
4
End-stage renal disease (ESRD) is
described as the stage of CKD when
damage to the kidneys is permanent
and kidney function cannot maintain
life; consequently, patients at this time
require dialysis or transplantation.
5
ESRD is at the far end of the spectrum
of progressive renal dysfunction.
Healthy People 2010 identifies the 5
risk factors for ESRD as diabetes
mellitus, hypertension, proteinuria,
family history, and increasing age.
2
Unfortunately, patients are often
asymptomatic in the early stages of
kidney failure when renoprotective
strategies
6
that could slow or reverse
the process of kidney damage could
be implemented. Because of the lack
of early signs and symptoms and
interventions, patients may come to
an acute care facility with signs and
symptoms of newly diagnosed ESRD.
What do critical care nurses need to
know about CKD and its treatment
to improve patients outcomes? A
thorough assessment of this complex
situation by critical care nurses is
ventricular hypertrophy and ST-T
waves consistent with a strain pattern.
A funduscopic examination showed
bilateral chronic and new hemor-
rhages (cotton wool hemorrhages
and exudates), arteriolar narrowing,
and arteriovenous nicking. Labora-
tory results are reported in Table 2.
J.M. was admitted to the intensive
care unit with a diagnosis of ESRD
due to hypertension with hyperten-
sive crisis and metabolic acidosis.
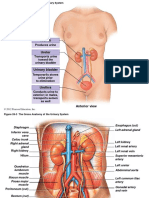
Pathophysiology
The kidneys act as regulators for
many of the bodys functions and
control complex processes that main-
tain homeostasis (Figure 1). The kid-
neys receive approximately 20% to
25% of the cardiac output per minute;
blood is filtered through the nephrons,
the functioning units of the kidneys.
Each kidney has approximately 1
million nephrons, providing a large
reserve of nephrons that enables
homeostasis to be maintained, even
when nephrons have been damaged.
7
However, when 90% of nephrons are
lost, renal function is significantly
impaired, resulting in ESRD.
4,8
The
best laboratory indicator of kidney
function is the estimated GFR. Several
equations are available to estimate
GFR. The National Kidney Disease
Education Program of the National
Institute of Diabetes and Digestive
and Kidney Diseases, the National
Kidney Foundation, and the American
Society of Nephrology have recently
recommended the Modification of
Diet in Renal Disease Study equation
as the formula to calculate GFR
9
:
GFR = 186 (serum creatinine
[mg/dL])
-1.154
(age [years])
-0.203
0.742 (if female) 1.210 (if
African-American)
8
essential, because multiple body sys-
tems are altered when kidney func-
tion is impaired. In this article, we use
a case study to review the pathophysi-
ological changes that occur when the
kidneys fail, resulting in admission to
the critical care unit. The immediate
interventions and the expected out-
comes are also presented.
Case Study
J.M., a 34-year-old African Amer-
ican man, came to the emergency
department with a 6-day history of
increasing swelling in both lower
extremities. A similar swelling had
occurred once before recently but
had cleared up spontaneously. J.M.
said he had no history of headaches,
hypertension, nausea, vomiting or
diarrhea, fever and chills, shortness
of breath, chest pain, urinary prob-
lems, weight loss, confusion or other
neurological changes, or exposure to
toxic substances. He also stated that
he was not taking any medication.
On physical examination, his blood
pressure was 222/142 mm Hg, his
heart rate was 110/min with S
3
and
S
4
gallops, and his respiratory rate
was 24/min with bibasilar crackles.
Electrocardiography showed left
18 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
Table 1 Chronic kidney disease defined by the National Kidney Foundation
*
Stage
1
2
3
4
5
Description
Kidney damage with normal
or increased GFR
Kidney damage with mild
decrease in GFR
Moderate decrease in GFR
Severe decrease in GFR
Kidney failure
Glomerular filtration rate (GFR), mL/min
per 1.73 m
2
>90
60-89
30-59
15-29
<15 (or dialysis)
*Chronic kidney disease is defined as either kidney damage or a glomerular filtration rate less than 60
mL/min per 1.73 m
2
for 3 months or longer. Kidney damage is defined as pathologic abnormalities or
markers of damage, including abnormalities in blood or urine tests or imaging studies.
Reprinted from the National Kidney Foundation,
4
with permission.
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
On the basis of this formula, J.M.
had a GFR of 3 mL/min per 1.73 m
2
,
meeting the definition of kidney fail-
ure. Whatever the underlying cause
of CKD, the effects of kidney failure
on the bodys homeostatic mecha-
nisms are the same. The next section
provides a comparison of the nor-
mal homeostatic regulations and the
alterations assessed in J.M.
Alterations in
Regulatory Functions
Body Water Regulation
Fluid volume is altered when the
kidney loses its ability to excrete
water because of damaged nephrons
and the resultant decreased GFR.
Other factors that contribute to the
development
of fluid vol-
ume overload
are protein-
uria and
increased
renin. Protein-
uria occurs in
response to
damage of the
glomeruli.
High blood
pressure can
cause sclerotic
changes in the
glomeruli
with a result-
ant loss of
protein, espe-
cially albumin
in the urine.
10
This damage
to the kidneys
from hyper-
tension is also
known as
hypertensive
http://ccn.aacnjournals.org CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 19
Figure 1 Homeostatic functions of the kidney.
Body water regulation
Urine output
Blood pressure
Normal
kidney
function in
homeostasis
Electrolyte balance
Sodium
Potassium
Phosphorus
Calcium
Magnesium
Acid-base balance
Metabolic
compensation
Metabolic (endocrine)
regulation
Erythropoietin
Renin-angiotensin-aldosterone
Vitamin D
Excretory regulation
Nitrogenous waste products
Drug metabolites and other
wastes
Uric acid
Table 2 J.M.s laboratory results
Laboratory test
Serum urea nitrogen,
mmol/L (mg/dL)
Creatinine,
mol/L (mg/dL)
Sodium, mmol/L
Potassium, mmol/L
Chloride, mmol/L
Carbon dioxide,
mmol/L
Uric acid,
mol/L (mg/dL)
Calcium,
mmol/L (mg/dL)
Phosphorus,
mmol/L (mg/dL)
Hemoglobin, g/L
Hematocrit
Arterial blood gases
on room air
Urinalysis
Alkaline
phosphatase, U/L
Admission results
67.47 (189)
1909.4 (21.6)
127
5.8
90
9.9
1142.0 (19.2)
2.05 (8.2)
3.91 (12.1)
83
0.252
pH 7.32
PCO
2
22.9 mm Hg
Bicarbonate 11.9 mmol/L
Base excess -12
PO
2
45.9 mm Hg
4+ protein
2+ hematuria
536
Results after dialysis
66.04 (185)
1865.2 (21.1)
129
3.9
89
12
Not determined
2.35 (9.4)
3.87 (12)
Not determined
Not determined
pH 7.44
PCO
2
18.1 mm Hg
Bicarbonate 12.5 mmol/L
Base excess -9
PO
2
81.7 mm Hg
Not determined
Not determined
378
Reference intervals
2.9-6.4 (8-18)
53-106 (0.6-1.2)
135-147
3.5-5.0
95-105
23-30
237.9-505.6 (4-8.5)
2.20-2.58 (8.8-10.3)
0.81-1.61 (2.5-5.0)
140-180
0.42-0.52
pH not determined
PCO
2
33-44 mm Hg
Bicarbonate 21-28 mmol/L
Base excess not determined
PO
2
75-100 mm Hg
30-120
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
20 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
nephrosclerosis and may cause dam-
age not only to the glomueruli but
also to the arteriolar walls.
8
The loss
of albumin in the urine contributes
to fluid shifting from the intravascu-
lar space to the interstitial space
because of decreased oncotic pres-
sure. As a response to decreased
GFR, aldosterone is released from the
adrenal cortex, causing the kidneys
to reabsorb sodium and water. Fluid
retention in turn results in the devel-
opment of respiratory and cardio-
vascular clinical manifestations. In
J.M., cardiovascular assessment find-
ings included 3+ edema of the lower
extremities, an albumin level of 32
g/L, blood pressure of 222/142 mm
Hg, the presence of S
3
and S
4
heart
sounds, sinus tachycardia (heart rate
108-112/min), crackles in the lungs,
and a decreased sodiumlevel (dilu-
tional hyponatremia).
Acid-Base Balance
Metabolic acidosis is associated
with CKD because the tubules cannot
excrete hydrogen ions (H
+
), resulting
in the use of bicarbonate (HCO
3
-
)
anions to maintain acid-base balance.
Two other buffering systems are in
place that assist in compensating for
the acidosis. Hydrogen ions combine
with ammonia produced in the renal
tubule cells to form ammonium,
which combines with chloride and is
excreted in the urine. This mechanism
helps to remove H
+
while generating
HCO
3
-
. However, because of impaired
nephron function, excretion of ammo-
niumis decreased. The third mecha-
nism involved with acid-base balance
results in H
+
combining with phos-
phate (one of the bodys buffering
systems). Metabolic acidosis also
contributes to a shift of calcium from
the bone, allowing H
+
to enter and
Serum phosphorus and calcium
levels are also altered in CKD. When
GFR is less than 30 to 50 mL/min
per 1.73 m
2
, phosphorus excretion
is impaired.
10
Because of the recipro-
cal relationship between phosphorus
and calcium, this increased retention
of phosphorus results in a decrease
in the serum level of calcium. Three
additional mechanisms can affect
calcium level. Calcium is found in 3
forms in the blood: attached to pro-
tein, attached to other complexes,
and free or ionized. Because some
calcium is bound to protein, total
serum calcium level can decrease
when albumin level decreases. J.M.
had proteinuria. This loss of albumin
can contribute to a decreased serum
level of calcium. CKD also has an
effect on vitamin D synthesis. The
kidneys normally convert inactive
vitamin D to its active form: 1,25-
dihydroxycholecalciferol.
11
Impaired
vitamin D synthesis results in
decreased absorption of calcium in
the gastrointestinal tract. The third
mechanism that affects serum levels
of calcium is the endocrine system.
When the serum level of calcium
decreases, the parathyroid gland
increases its secretion of parathyroid
hormone, causing calcium to be
released from the bone and compen-
sating for the decreased serum level
of calcium.
12
Results of J.M.s labora-
tory tests showed a calcium level of
2.05 mmol/L (8.2 mg/dL) and a
phosphorus level of 3.91 mmol/L
(12.1 mg/dL), indicating impaired
phosphorus excretion and a recip-
rocal decrease in calcium level.
Alterations in
Excretory Function
In CKD, nitrogenous waste
products from protein metabolism
be buffered in the bone.
7
Results of
J.M.s laboratory tests revealed a pH
of 7.32, HCO
3
-
11.9 mmol/L, base
excess -12, and serum carbon dioxide
9.9 mmol/L, all indicating metabolic
acidosis. A decreased arterial PCO
2
of 22.9 mm Hg results from an
increased respiratory rate as the
body attempts to compensate for
the acidosis by exhaling the respira-
tory acid carbon dioxide. The anion
gap can be used to determine the
cause of the metabolic acidosis. Nor-
mally the kidney conserves HCO
3
-
and excretes H
+
. In CKD, when the
glomeruli are damaged, metabolic
acids such as sulfuric and phosphoric
acid are retained, causing a widening
of the anion gap.
8
The anion gap is
calculated mathematically:
Anion gap = Na
+
(Cl
-
+ HCO
3
-
)
The normal anion gap is approx-
imately 12 mmol/L. J.M.s anion gap
was 127 (90 + 11.9) = 25.1 mmol/L,
supporting the diagnosis of metabolic
acidosis due to kidney failure.
Electrolyte Balance
Multiple electrolyte levels are
altered in patients with CKD. Potas-
sium levels may be normal until late in
ESRD, and elevated potassium levels
are often associated with CKD because
of the inability of the kidney to excrete
potassium as a result of decreased
GFR. In addition, when metabolic aci-
dosis is present, potassium ions shift
from the intracellular compartment to
the extracellular space in exchange for
H
+
, in an effort to maintain extra-
cellular acid-base balance. The kid-
neys normally excrete 40 to 60 mmol
of potassium daily.
11
J.M.s potassium
level was 5.8 mmol/L, increasing his
risk for fatal dysrhythmias.
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
are retained in the body, resulting
in azotemia, as evidenced by the
increased serum levels of urea nitro-
gen and creatinine. The tubules,
which are permeable to urea, nor-
mally reabsorb little urea. However,
as GFR decreases, more urea is reab-
sorbed. Although elevated serum
levels of urea nitrogen alone can indi-
cate other abnormalities, such as
dehydration, elevation of serum levels
of both urea nitrogen and creatinine
indicates kidney failure. The serum
urea nitrogencreatinine ratio (normal
10:1 to 20:1) was once used to assess
kidney function, but the ratio is not
considered as an important indicator
today. J.M.s serum level of urea nitro-
gen was 66.05 mmol/L (185 mg/dL),
and his serum creatinine level was
1909.4 mol/L (21.6 mg/dL), result-
ing in a ratio of 9:1. This slightly
decreased ratio could reflect fluid
overload from the CKD or an undi-
agnosed liver disease, because J.M.s
alkaline phosphatase level was also
elevated.
Proteinuria and hematuria are
associated with glomerulonephritis
and result from damage of the
glomeruli with the resultant increased
permeability. Albumin is a sensitive
indicator of CKD related to diabetes,
glomerular disease, and hyperten-
sion.
13
Although J.M. had no history
of kidney disease, he did have hyper-
tension, which can damage the
glomeruli. Glomerular damage was
evidenced by the 4+ protein and 2+
hematuria.
Uric acid is an end product of
purine metabolism that is filtered in
the glomeruli and secreted into the
distal tubule.
10
Impaired glomerular
function results in decreased excre-
tion of uric acid by the kidney and
may result in the development of
gouty arthritis with deposits of uric
acid in joints or soft tissue.
8
J.M.s
uric acid level was 1142 mol/L
(19.2 mg/dL). This elevated level of
uric acid increased J.M.s risk of gout
developing with symptoms such as
joint pain, redness, and swelling,
particularly in the great toe.
Alterations in Metabolic/
Endocrine Functions
Anemia results from several fac-
tors in patients with CKD. The per-
itubular capillary endothelium in
the kidneys produces erythropoietin,
which is needed to stimulate bone
marrow to release red blood cells. In
addition, uremia inactivates erythro-
poietin. Failure of this mechanism
results in a normochromic, normo-
cytic anemia. Uremia can also con-
tribute to anemia by shortening the
life span of the red blood cells. Finally,
the low hemoglobin level contributes
to acidosis, because less hemoglobin
is available in the body to buffer acids.
Additionally, uremia causes impaired
platelet aggregation, increasing the
potential for bleeding.
10
J.M.s hemo-
globin level was 83 g/L, his hemat-
ocrit was 0.252, and his platelet
counts were adequate. The decreased
hemoglobin level and hematocrit
could have caused signs and symp-
toms of anemia, and although his
platelet count was adequate, the
platelets would not function effec-
tively, increasing the risk for bleeding.
Renin is released in response to
changes in intravascular pressure
or sympathetic stimulation.
8
The
resultant stimulation of the renin-
angiotensin-aldosterone system
contributes to the retention of water
and elevated blood pressure.
4,14
Renin
is an enzyme released from the jux-
taglomerular cells in response to
decreases in blood flow to the kidney,
changes in tubular fluid composition,
or stimulation by the sympathetic
nervous system. Renin then acts on
angiotensinogen, a plasma protein,
and converts it to angiotensin I.
Angiotensin I in turn is converted
to angiotensin II by angiotensin-
converting enzyme in the lungs.
Angiotensin II produces 2 outcomes.
The first is a short-acting vasocon-
striction. The second action is an
increase in blood pressure through
stimulation of the adrenal cortex,
which releases aldosterone, causing
sodium reabsorption and concomi-
tant water reabsorption by the kid-
neys. J.M.s blood pressure was
221/142 mm Hg. It was unknown
on admission whether J.M. had a
primary hypertension that had led
to kidney failure or if the kidney fail-
ure had contributed to the hyperten-
sion. The retention of water and
production of angiotensin certainly
contributed to the hypertension and
the cardiovascular and respiratory
findings from fluid overload.
Assessment Findings
Because the pathophysiological
changes associated with CKD affect
every body system (Figure 2), a thor-
ough nursing assessment of patients
with CKD is essential. A systems
approach to assessment is used here.
Cardiovascular
Hypertension is a result of
increased fluid retention and stim-
ulation of the renin-angiotensin-
aldosterone system. In addition,
hypertension can lead to the devel-
opment of CKD. For J.M., it was
unknown whether the hypertension
contributed to the renal failure or
the renal failure contributed to the
22 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
hypertension. J.M.s clinical assess-
ment revealed left ventricular hyper-
trophy and a strain pattern on the
electrocardiogram, indicating long-
standing left ventricular failure.
Auscultation of heart sounds revealed
an S
3
(fluid overload) and S
4
gallop
(decreased compliance and hyper-
tension). Funduscopic examination
showed arteriovenous nicking and
cotton wool hemorrhages with exu-
dates (hypertensive retinopathy), all
indicating significant hypertension.
The sinus tachycardia could have
been a compensatory mechanism
for the decreased PaO
2
, the anemia,
the metabolic acidosis, or the fluid
overload. Uremic pericarditis, another
manifestation of ESRD, often devel-
ops from the accumulation of toxins;
nate carbon
dioxide in an
attempt to
reestablish
normal pH.
Fluid overload
with pul-
monary con-
gestion was
manifested in
J.M. by crack-
les, decreased
PaO
2
, and
increased res-
piratory rate.
J.M.s acid-
base results
were
described pre-
viously. The
focus of the
nursing
assessment is
breath
sounds, respi-
ratory rate
and pattern,
and results of arterial blood gas
analysis.
Gastrointestinal
Anorexia, weight loss, nausea,
and vomiting are frequent findings
in patients with CKD, although J.M.
said that he did not have these signs
and symptoms. Halitosis, a metallic
taste in the mouth, and ulcers in the
mouth may occur because bacteria
in the mouth break down urea into
ammonia. Gastrointestinal bleeding
from altered platelet function and
increased gastric acid secretion from
increased release of parathyroid hor-
mone
10
may occur. The focus of the
nursing assessment includes inspect-
ing oral mucous membranes, moni-
toring weight, checking stool for
J.M. did not have this manifestation.
Electrolyte imbalances such as
hyperkalemia and hypocalcemia can
also lead to dysrhythmias. The focus
of the nursing assessment is periph-
eral edema, circulatory overload evi-
denced by congestive heart failure
and pulmonary edema, cardiac dys-
rhythmias, hypertension, and elec-
trolyte levels.
Respiratory
An increased respiratory rate may
result from fluid overload, as a com-
pensatory mechanism for metabolic
acidosis, or from decreased PaO
2
.
Although not identified as Kussmaul
respirations, deep breaths associated
with metabolic acidosis occur as a
compensatory mechanism to elimi-
http://ccn.aacnjournals.org CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 23
Figure 2 Clinical manifestations of chronic kidney disease.
Integumentary
Bruises, pruritus, dry skin,
skin color changes ashen
gray to yellowish,
dry brittle hair and nails
Clinical
manifestations of
chronic kidney
disease
Respiratory
Increased respiratory rate,
Kussmaul respirations,
crackles, decreased PO
2
Renal
Decreased urine output,
azotemia, proteinuria,
hematuria, hyperuricemia
Gastrointestinal
Anorexia, nausea,
vomiting, halitosis,
metallic taste in mouth,
bleeding in
gastrointestinal tract
Neurological
Peripheral neuropathy, restless legs,
change in level of consciousness,
lethargy, confusion, encephalopathy,
altered motor function
Hematological
Anemia, weakness,
fatigue, pallor,
lethargy, bleeding due
to impaired platelet
aggregation
Musculoskeletal
Renal osteodystrophy, decreased
calcium, vitamin D impairment,
hyperparathyroidism,
pathological fractures
Immune
Increased risk of infection
Cardiovascular
High blood pressure, increased heart rate,
dysrhythmias, electrocardiographic changes,
abnormal heart sounds, retinopathy, fluid
retention with peripheral edema and/or
pulmonary edema
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
occult blood, and noting breath
odor.
Neurological
Central nervous system findings
in patients with CKD can range
from confusion and difficulty con-
centrating to seizures and coma.
These findings are described as ure-
mic encephalopathy. Impaired
thinking processes are sometimes
described as BUN [blood urea
nitrogen] blunting. The effects of
CKD on the peripheral nervous sys-
tem result in peripheral neuropathy,
particularly affecting the lower
extremities. The cause of these neu-
rological effects is thought to be
atrophy and demeylination of the
nerves as a result of uremic toxins
and electrolyte imbalances.
8,10
Early
findings include restless leg syn-
drome progressing to pain, sensa-
tions of tightness in the legs, and
pain in a stocking-like pattern.
Finally motor function may be
impaired with resultant changes in
gait and fine motor movement.
8,10
J.M. had none of these neurological
signs or symptoms. The focus of the
nursing assessment is mental status
and motor and sensory function.
Integumentary
Pruritus often occurs in patients
with CKD because of the excretion
of waste products and phosphate
10
through the skin. The skin is often
dry because of decreased activity of
sweat glands and oil glands, and the
skin may undergo changes in color,
from pallor related to the anemia to
a yellow-brown or gray aspect from
urochrome, a urinary pigment.
8
The
nails and hair may become brittle.
Bruises may also occur because of
impaired platelet function and
increased capillary fragility. J.M. had
none of these manifestations. The
focus of the nursing assessment
includes inspection of the skin for
color changes or impaired integrity
as a result of scratching of the skin
by the patients.
Musculoskeletal
Renal osteodystrophy results from
the loss of calcium in the bones and
ineffective conversion of vitamin D
to allow absorption of calcium. Three
bone changes are associated with
this syndrome: (1) osteomalacia due
to inadequate absorption of calcium
from the gastrointestinal tract, (2)
osteitis fibrosa or bone demineral-
ization due to increased parathyroid
hormone, and (3) osteosclerosis,
which is manifested as bands of
increased and decreased bone density
in the vertebrae.
8
J.M. had no indica-
tions of skeletal deficiencies, although
his calcium level was 2.05 mmol/L
(8.2 mg/dL). The focus of the nursing
assessment is monitoring calcium
and phosphorus levels. Signs and
symptoms of hypocalcemia include
neuromuscular irritability manifested
by paresthesia and tetany, which is
assessed by testing for the Chvostek
sign and the Trousseau phenomenon,
muscle cramps, hypotension, and
prolonged QT interval.
Hematological
Decreased erythropoietin levels
result in anemia. J.M.s laboratory
results showed decreases in hemoglo-
bin level and hematocrit. The focus
of the nursing assessment is detection
of signs and symptoms of anemia,
including pallor, fatigue, shortness
of breath, and tachycardia, and on
laboratory evaluation of hematocrit
and hemoglobin and iron levels.
Immunological
Increased levels of uremic tox-
ins can lead to impaired immune
and inflammatory responses with
resultant defects in granulocytes,
impaired B- and T-cell functioning,
and impaired phagocytosis.
10
The
focus of the nursing assessment is
examination for signs or symptoms
of an impaired inflammatory and
infectious response. Infection is a
common occurrence in patients with
CKD that often results in hospital-
ization and death.
10
Renal
In patients with CKD, urinary
signs and symptoms are related to
fluid balance; as GFR decreases, urine
output decreases. Retention of waste
products such as urea nitrogen and
creatinine leads to azotemia, whereas
uric acid retention may lead to gout.
Proteinuria and hematuria were dis-
cussed previously. The focus of the
nursing assessment is fluid balance
(intake and output, daily weight,
edema) and monitoring of labora-
tory results.
Current Standards of Care
The clinical manifestations due
to the pathophysiological changes
of CKD create a need for immediate
interventions and constant monitor-
ing. Because J.M.s serum level of
urea nitrogen was 67.47 mmol/L
(189 mg/dL) and his creatinine level
was 1909.4 mol/L (21.6 mg/dL),
the immediate clinical action required
for J.M., according to the KDOQI
clinical action plan for CKD, was
renal replacement therapy
1
started
as soon as possible. After the initial
assessment was completed in the
emergency department, a nephrolo-
gist was consulted and a double-
24 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
lumen percutaneous catheter was
inserted. Hemodialysis was selected
as the intervention rather than peri-
toneal dialysis because of J.M.s acute
condition.
The mechanics of hemodialysis,
with all access types, involves blood
being removed from the body by the
blood pump of the dialysis machine;
the blood then passes through the
dialyzer
14
(artificial kidney), where it
is cleansed by osmosis and diffusion
(hemodialysis works by diffusion of
low-molecular-weight solutes across
a semipermeable membrane). Finally,
the blood completes the circuit and
returns to the patients vascular com-
partment, the cycle repeats constantly
while the patient is on dialysis. The
total amount of blood outside the
body at any time is approximately
200 to 300 mL.
A vascular access for arterial flow
and venous return is needed for the
dialysis procedure. Of 3 access types,
1 is temporary and 2 are permanent
(Table 3). The central venous catheter
is the least desirable because compli-
cations are common, particularly
infection; however, because of the
emergent nature of J.M.s situation,
a temporary access was required.
The right internal jugular vein is the
preferred site,
15
although the femoral
venous or subclavian venous sites
are also used. Using the subclavian
site can cause venous stenosis and
thrombosis,
16
interfering with any
future access for fistulas or grafts;
therefore, it should be used only when
the femoral or jugular sites are not
accessible.
A temporary access is placed in a
large central vein and can be used
for as long as 3 months. The proce-
dure is done by using sterile technique
in an angiography suite, procedure,
tional support, and/or obtaining
blood samples. It is important to
knowwhich site will be used, as well
as the size and body type of the
patient, to determine what size and
length catheter is needed. If the jugu-
lar or the subclavian site is used,
catheters must be longer than if the
femoral site is chosen, because of the
positioning of the catheter. The dial-
ysis catheter has a large lumen, 11.5F
or 12F, which allows a smooth flow
of blood throughout the hemodialy-
sis procedure.
Additional immediate interven-
tions initiated because of J.M.s criti-
cal condition included oxygen via
nasal cannula at 4L/min, cardiac
monitoring to assess for dysrhyth-
mias, insertion of a peripheral intra-
venous catheter and an indwelling
Foley catheter. After his initial dialy-
sis, J.M. was placed on a 1000-mL
fluid restriction and a renal diet of
or operating suite; however, because
of J.M.s critical condition, the pro-
cedure was done at the bedside. The
right jugular vein was used, and a
20-cmlong catheter was inserted
into the vein and then sutured in
place by using suture wings. Once
the catheter was in place, while
maintaining aseptic technique, a
nurse instilled heparin into each
lumen, per facility protocol, to equal
the total volume of each lumen (the
lumen volume is printed on each
lumen of the catheter). A catheter
cap was then placed on each lumen,
and a dressing was placed over the
site. J.M. was now ready for dialysis
after placement of the catheter had
been verified with a chest radiograph.
Several brands and types of dial-
ysis catheters are available
17
; those
commonly used are double or triple
lumen. The triple lumen gives an
added lumen for drug therapy, nutri-
http://ccn.aacnjournals.org CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 25
Access type
Arteriovenous fistula: A
permanent access that
is created surgically by
connecting an artery to
a vein
The forearm is the most
common site
Arteriovenous graft: A per-
manent access created
surgically by using a syn-
thetic material tunneled
under the skin
One end of graft is con-
nected to an artery; the
other, to a vein
Catheter: A temporary
access in which a
catheter is placed into a
large central vein such as
the internal jugular vein
Advantages
Preferred route for dialysis;
once matured, has good
blood flow, few problems
It is long lasting and is
associated with fewer
complications than are
other accesses
Shorter maturation time
than fistula; site can be
used in 3-6 weeks
No maturation time
Catheter can be used
immediately after place-
ment and is often used
in emergent situations
Disadvantages
Long maturation time (3-4
months until it can be used
for dialysis)
May not enlarge enough to
provide a good blood flow
for dialysis
Higher incidence of thrombo-
sis and clotting than with
arteriovenous fistula
Higher incidence of stenosis
than with fistula
Involves use of synthetic
material, creating the
potential for an allergic
response
Increased risk of infection in
catheter, at exit site, and in
bloodstream
Decreased flow rates with
catheter lead to low urea
reduction rate
Potential for discomfort at
catheter exit site and devel-
opment of poor body image
Table 3 Access sites for hemodialysis
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
60 g of protein, 2 g potassium, and
2 g sodium. Fluid volume intake is
based on 500 mL/day (insensible
fluid loss) plus fluid equal to the urine
output of the preceding 24 hours.
8
Once a patients condition stabi-
lizes, after the diagnosis of CKD is
made and initial treatment has begun,
the patient is referred to a surgeon
for establishment of a permanent
vascular access. The National Kidney
Foundation
18
recommends the arte-
riovenous fistula as the preferred type
of access; this access is associated with
fewer complications and provides
longer trouble-free use than does an
arteriovenous graft or a catheter. The
catheter is the access least recom-
mended because of the frequent
complications associated with its use.
J.M. had an arteriovenous fistula
placed 8 days after admission. Nurs-
ing assessment after a fistula is placed
focuses on patency of the fistula,
determined by palpating a thrill and
auscultating a bruit.
Expected Outcomes
On the basis of the KDOQI guide-
lines, the focus of treatment in CKD
is specific therapy, dialysis in J.M.s
case, and treatment of comorbid
conditions.
19
Particularly for J.M.,
the clinical findings such as hyperten-
sion, anemia, calcium and phospho-
rus balance, and nutritional status
required treatment.
The expected outcomes and nurs-
ing considerations for J.M. would
include the following:
Adequate hemodialysis
20
is
determined by measurement of levels
of nitrogenous waste products (serum
levels of urea nitrogen and creatinine)
and the urea reduction ratio, in which
the measurements from before and
after dialysis are entered into a math-
ematical formula. Adequate dialysis
will also result in correction of acid-
base imbalance, fluid volume over-
load, and electrolyte imbalances
(particularly sodium and potas-
sium). Results of J.M.s laboratory
tests after dialysis are found in Table
2. J.M. initially received daily dialy-
sis for 3 days. Correction of the fluid
imbalance in turn will correct
impaired gas exchange. Nursing
implications include fluid restric-
tion, monitoring, and daily weight.
The focus of educating patients is
teaching about foods that are high
in potassium and the importance of
potassium restriction in preventing
cardiac dysrhythmias. Disregarding
potassium restriction can be fatal
for a patient with CKD. Immediate
referral to a dietician is also appro-
priate because not only potassium
but also sodium and phosphorus are
restricted on a renal diet.
Blood pressure within normal
limits
21
is related to several interven-
tions, including adequate hemodial-
ysis and fluid restriction. The most
important nondrug management for
hypertension is fluid removal and
restriction of sodium and fluid in the
diet. Education of patients focuses on
teaching about foods high in sodium
that must be avoided and manage-
ment of fluid intake. Pharmacological
intervention includes the use of
angiotensin-converting enzyme
inhibitors, which decrease not only
systemic blood pressure but also
intraglomerular pressure by dilating
the efferent arteriole.
8
Angiotensin-
converting enzyme inhibitors must
be used with caution because a con-
comitant increase in serum potassium
levels may occur. Calcium channel
blockers are also effective in decreas-
ing blood pressure through systemic
vasodilatation. J.M. was treated with
captopril (Capoten) and nifedipine
(Procardia). For patients on dialysis,
antihypertensive medications should
be given after hemodialysis to prevent
hypotension.
Prevention of other cardiovas-
cular diseases
22
is accomplished
through control of hypertension and
fluid volume, physical exercise, and
prevention of end-organ damage.
Cardiovascular disease is the leading
cause of death in patients with ESRD.
22
A physician-approved exercise pro-
gram for patients with CKD provides
the positive benefits of exercise such
as decreasing blood pressure, choles-
terol and triglyceride levels, and
insomnia and the obvious benefit of
maintaining weight control. Nursing
interventions focus on monitoring
weight loss/gain, blood pressure, and
peripheral edema and on educating
patients about diet and exercise.
Target hemoglobin and hemat-
ocrit levels can be reached
23
through
the use of iron supplements, multivi-
tamins, and epoetin alfa (Epogen),
which stimulates production of red
blood cells. Nursing interventions
include monitoring hemoglobin levels
and hematocrit and assessing patients
for clinical findings of anemia.
Prevention of bony changes
24
is
accomplished through the manage-
ment of calcium and phosphorus
levels. In addition to dietary man-
agement, phosphate binders (alu-
minum hydroxide) or calcium salts
(PhosLo) may be used to reach this
outcome. Because medications are
the primary method of removing
phosphorus from the body (dialysis
removes very little), the necessity of
taking the phosphate binder with
food to be effective is a significant
aspect of patients education. Moni-
26 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
toring calcium and phosphorus levels
would also be part of the nursing role.
Adequate nutrition (based on
albumin level)
25
is managed through
dietary regulation. Proteins of high
biological value are essential because
total protein intake is restricted.
Adequate protein levels result in
maintenance of fluid balance, heal-
ing and maintenance of skin integrity,
and finally maintenance of immune
function. Providing dietary education
on appropriate protein foods and
serving size is an important activity
of nurses and/or dieticians, along
with monitoring albumin levels.
Conclusion
The significant role of critical
care nurses in providing care to
patients with CKD is clear. A thor-
ough assessment of all body systems
is essential in evaluating each patient.
This assessment will enable the early
detection of systemic alterations
related to CKD and the implementa-
tion of appropriate interventions.
Education of patients about the
management of CKD and continued
evaluation of patients outcomes are
also essential so that critical care
nurses can determine the effective-
ness of interventions.
Acknowledgments
The data reported here have been supplied by the US
Renal Data System. The interpretation and reporting of
these data are the responsibility of the author(s) and in
no way should be seen as an official policy or interpreta-
tion of the US government.
References
1. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for chronic kidney
disease: executive summary. Available at:
http://www.kidney.org/professionals/kdoqi
/guidelines_ckd/p1_exec.htm. Accessed
May 15, 2006.
2. National Institute of Diabetes and Digestive
and Kidney Disease. Healthy People 2010
objectives: chronic kidney disease. Available
at: http://www.niddk.nih.gov/fund
/divisions/KUH/KidneyHP2010.htm.
Accessed May 15, 2006.
3. US Renal Data System. USRDS 2004
21. National Kidney Foundation. K/DOQI clini-
cal practice guidelines on hypertension and
antihypertensive agents in chronic kidney
disease. Available at: http://www.kidney
.org/professionals/kdoqi/guidelines_bp
/guide_1.htm. Accessed May 15, 2006.
22. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for cardiovascular
disease in dialysis patients. Available at:
http://www.kidney.org/professionals/kdoqi
/guidelines_cvd/overview.htm. Accessed
May 15, 2006.
23. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for anemia of chronic
kidney disease: update 2000. Available at:
http://www.kidney.org/professionals/kdoqi
/guidelines_updates/doqiupan_iv.html#11.
Accessed May 15, 2006.
24. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for bone metabolism
and disease in chronic kidney disease. Avail-
able at: http://www.kidney.org
/professionals/kdoqi/guidelines_bone
/index.htm. Accessed May 15, 2006.
25. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for nutrition in
chronic renal failure. Available at: http://
www.kidney.org/professionals/kdoqi
/guidelines_updates/doqi_nut.html.
Accessed May 15, 2006.
Annual Data Report: Atlas of End-Stage
Renal Disease in the United States, National
Institutes of Health, National Institute of
Diabetes and Digestive and Kidney Dis-
eases, Bethesda, Md. Available at: http://
www.usrds.org/atlas.htm. Accessed May
15, 2006.
4. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for chronic kidney
disease: evaluation, classification, and strat-
ification. Guideline 1: Definition and stages
of chronic kidney disease. Am J Kidney Dis.
2002;39(suppl 1):S1-S266. Also available at:
http://www.kidney.org/professionals/kdoqi
/guidelines_ckd/ex2.htm#ckdex1.
Accessed May 15, 2006.
5. Copstead LC, Banasik JL. Pathophysiology:
Biological and Behavioral Perspectives. 2nd ed.
Philadelphia, Pa: WB Saunders Co; 2000.
6. Ruggenenti P, Schieppati A, Remuzzi G.
Progression, remission, regression of chronic
renal disease. Lancet. 2001;357:1601-1608.
7. Heuther SE, McCance KL. Understanding
Pathophysiology. 3rd ed. St Louis, Mo:
Mosby; 2004.
8. Price S, Wilson L. Pathophysiology: Clinical
Concepts of Disease Processes. 6th ed. St
Louis, Mo: Mosby; 2003.
9. Kidney Learning System. Frequently asked
questions about GFR estimates. Available
at: http://www.kidney.org/professionals
/KLS/gfr.cfm. Accessed May 15, 2006.
10. Porth CM. Pathophysiology Concepts of
Altered Health States. 6th ed. Philadelphia,
Pa: Lippincott; 2002.
11. Metheny N. Fluid and Electrolyte Balance.
4th ed. Philadelphia, Pa: Lippincott
Williams & Wilkins; 2000.
12. Wallace M. Anatomy and physiology of the
kidney. AORN J. 1998;68:799-780, 803-804,
806, 808, 810-811, 813-816, 819-824, 827-828.
13. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for chronic kidney
disease: guideline, assessment of protein-
uria. Available at: http://www.kidney.org
/professionals/kdoqi/guidelines_ckd
/p5_lab_g5.htm. Accessed May 15, 2006.
14. Cannon JD. Recognizing chronic renal fail-
ure. Nursing. January 2004;34:50-53.
15. Kapoian T, Kaufman J, Nosher J, Sherman
RA. Dialysis access and recirculation. In:
Henrich WL, Bennet WM, eds. Atlas of Kid-
ney Disease. 1999:5.1-5.14. Available at:
www.kidneyatlas.org/book5/adk5-05.ccc
.QXD.pdf. Accessed May 15, 2006.
16. Trerotola SO. Hemodialysis catheter place-
ment and management. Radiology. 2000;
215:651-658.
17. Ash SR. The evolution and function of cen-
tral venous catheters for dialysis. Semin
Dial. 2001;14:416-424.
18. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for vascular access,
2000. Am J Kidney Dis. 2001;37(suppl 1):
S137-S181.
19. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for chronic kidney
disease: guideline 2. Evaluation and treat-
ment. Available at: http://www.kidney.org
/professionals/kdoqi/guidelines_ckd/ex2
.htm#ckdex2. Accessed May 15, 2006.
20. National Kidney Foundation. K/DOQI clini-
cal practice guidelines for hemodialysis ade-
quacy: update 2000. Available at: http://
www.kidney.org/professionals/kdoqi
/guidelines_updates/doqi_uptoc.html#hd.
Accessed May 15, 2006.
http://ccn.aacnjournals.org CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 27
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
28 CRITICALCARENURSE Vol 26, No. 4, AUGUST 2006 http://ccn.aacnjournals.org
CE Test Test ID C064: Chronic Kidney Disease: Acute Manifestations and Role of Critical Care Nurses
Learning objectives: 1. Identify the expected outcomes of patients with chronic kidney disease (CKD) 2. Describe the pathophysiology of CKD
3. Discuss the impact of CKD in relation to body systems
Program evaluation
Yes No
Objective 1 was met K K
Objective 2 was met K K
Objective 3 was met K K
Content was relevant to my
nursing practice K K
My expectations were met K K
This method of CE is effective
for this content K K
The level of difficulty of this test was:
Keasy Kmedium Kdifficult
To complete this program,
it took me hours/minutes.
Test answers: Mark only one box for your answer to each question. You may photocopy this form.
1. Why is chronic kidney disease (CKD) a public health issue? ?
a. Because of increasing incidence and the high cost of interventions
b. Because of increasing cost of insurance premiums and loss of insurance
c. Because of limited access to dialysis centers and limited public education of the
disease
d. Because of limited access to dialysis centers and the high cost of interventions
2. Which of the following are 3 risk factors for end-stage renal disease
according to Healthy People 2010?
a. Hypertension, proteinuria, and family history
b. Diabetes mellitus, coronary artery disease, and smoking
c. Obesity, smoking, and proteinuria
d. Increasing age, hypertension, and hypercholesterolemia
3. In relationship to cardiac output, what percentage of blood is
f iltered through the nephrons per minute in normal homeostasis?
a. 20% to 25%
b. 35% to 45%
c. 45% to 50%
d. 75% to 80%
4. Which of the following best describes the response to decreased
glomerular f iltration rate?
a. Cortisol is released from the adrenal medulla, resulting in reabsorption of
sodium and water.
b. Aldosterone is released from the adrenal cortex, resulting in excretion of
water, sodium, and potassium.
c. Antidiuretic hormone is released resulting in reabsorption of water, sodium,
and potassium.
d. Aldosterone is released from the adrenal cortex, resulting in reabsorption of
water and sodium.
5. Which of the following best illustrates the correct anion gap equation?
a. Anion gap = Na
+
+ (Cl
-
+ HCO
3
-
)
b. Anion gap = Na
+
- (Cl
-
+ HCO
3
-
)
c. Anion gap = 6.1 + log (HCO
3
-
/ [0.03 PCO
2
])
d. Anion gap = Cl
-
+ (Na
+
/ HCO
3
-
)
6. Which of the following best describes the normal excretion of
potassium by the kidneys?
a. 20 to 40 mmol daily
b. 40 to 60 mmol daily
c. 30 to 50 mmol daily
d. 80 to 100 mmol daily
7. Which of the following best describes the function of the
endocrine system in CKD in relationship to hypocalcemia?
a. The thyroid gland increases it secretion of thyroid hormone, stimulating
the release of cortisol into the blood.
b. The thyroid gland decreases secretion of thyroid hormone, decreasing
the amount of calcium excreted.
c. The parathyroid glands secrete parathyroid hormone, decreasing the
amount of calcium released from the bone into the vascular system.
d. The parathyroid glands secrete parathyroid hormone, increasing the
amount of calcium released from the bone in the vascular system.
8. Which of the following cardiovascular changes do critical care
nurses need to monitor during their assessment of the patient with
CKD?
a. Peripheral edema, cardiac dysrhythmia, and electrolyte levels
b. Gastroesophageal reflux disease, pulmonary edema, and hypotension
c. Dehydration, gastrointestinal bleeding, and hypotension
d. Endocarditis, hyperglycemia, and congestive heart failure
9. Which of the following are associated with renal osteodystrophy?
a. Osteomalacia, osteitis fibrosa, and osteosclerosis
b. Peripheral neuropathy, osteoperiostitis, and osteophlebitis
c. Osteomatosis, osteomyelitis, and dysostosis
d. Dermatitis, desmosis, and myelolysis
10. As blood completes the circuit during dialysis, approximately
how much blood is outside the body at any time?
a. 75 to 150 mL
b. 100 to 300 mL
c. 200 to 300 mL
d. 250 to 400 mL
11. The National Kidney Foundation recommends which type of
access for permanent vascular access?
a. Infusaport
b. Ash catheter
c. Arteriovenous graft
d. Arteriovenous fistula
Mail this entire page to:
AACN
101 Columbia
Aliso Viejo, CA 92656
(800) 899-2226
Test ID: C064 Form expires: August 1, 2008. Contact hours: 2.0 Fee: $12 Passing score: 8 correct (73%) Category: A Test writer: Todd M. Grivetti, RN, BSN, CCRN
9. Ka
Kb
Kc
Kd
8. Ka
Kb
Kc
Kd
7. Ka
Kb
Kc
Kd
6. Ka
Kb
Kc
Kd
5. Ka
Kb
Kc
Kd
4. Ka
Kb
Kc
Kd
3. Ka
Kb
Kc
Kd
2. Ka
Kb
Kc
Kd
1. Ka
Kb
Kc
Kd
11. Ka
Kb
Kc
Kd
10. Ka
Kb
Kc
Kd
Name Member #
Address
City State ZIP
Country Phone
RN Lic. 1/St RN Lic. 2/St
Payment by: KVisa KM/C KAMEX KDiscover KCheck
Card # Expiration Date
Signature
The American Association of Critical-Care Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Centers Commission on Accreditation.
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
by guest on August 11, 2014 http://ccn.aacnjournals.org/ Downloaded from
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Pathophysiology of LeptospirosisDocument26 pagesPathophysiology of LeptospirosisHY Hong Yi0% (1)
- Process of urine formation and blood pressure regulationDocument3 pagesProcess of urine formation and blood pressure regulationSamia TazinPas encore d'évaluation
- Lecture Notes On The Renal System-1Document51 pagesLecture Notes On The Renal System-1GiftedPas encore d'évaluation
- Renal Physiology Practice QuestionsDocument4 pagesRenal Physiology Practice QuestionsAndiWilkinsPas encore d'évaluation
- 33 Cisplatin A ReviewDocument18 pages33 Cisplatin A Reviewtrifamonika23Pas encore d'évaluation
- Homeostatis F & EDocument11 pagesHomeostatis F & EYa Mei LiPas encore d'évaluation
- Renal Physiology: Structure and Function of KidneysDocument16 pagesRenal Physiology: Structure and Function of KidneysSufyan MirzaPas encore d'évaluation
- Definitions: - PharmacokineticsDocument31 pagesDefinitions: - PharmacokineticsmebibegPas encore d'évaluation
- Intact Nephron HypothesisDocument1 pageIntact Nephron HypothesisSudeep PradhanPas encore d'évaluation
- Peritoneal Dialysis SeminarDocument25 pagesPeritoneal Dialysis SeminardrresmiajithPas encore d'évaluation
- Renal Function Testing and Non-Protein Nitrogen SubstancesDocument77 pagesRenal Function Testing and Non-Protein Nitrogen SubstancesSolomon MesenaPas encore d'évaluation
- Renal Physiology For The Clinician Full Series CJASN PDFDocument230 pagesRenal Physiology For The Clinician Full Series CJASN PDFmms100% (3)
- EMQ and SAQ Revision QuestionsDocument12 pagesEMQ and SAQ Revision QuestionsSanathRaoPas encore d'évaluation
- Class 11th Human Physio TestDocument8 pagesClass 11th Human Physio TestSaurabh KrishnaPas encore d'évaluation
- Urinary System Slides Lab 8Document17 pagesUrinary System Slides Lab 8Asad Javed Mehmood100% (1)
- Regulation of Body FluidsDocument7 pagesRegulation of Body FluidsRuth FamillaranPas encore d'évaluation
- Drugs and Kidney Dec 28 2012Document43 pagesDrugs and Kidney Dec 28 2012Vin BitzPas encore d'évaluation
- NephronDocument5 pagesNephronrdeguzma100% (1)
- Unlock SGCh16Document7 pagesUnlock SGCh16SilaxPas encore d'évaluation
- Chlinical Pharmacokinetics On Renal Failure PatientsDocument29 pagesChlinical Pharmacokinetics On Renal Failure PatientsDenadaPutriPas encore d'évaluation
- Anatomi Dan Fisiologi GinjalDocument32 pagesAnatomi Dan Fisiologi GinjalScholastika PalayukanPas encore d'évaluation
- MC I Modular Reviewer Urinary SystemDocument12 pagesMC I Modular Reviewer Urinary SystemSteiner LimPas encore d'évaluation
- Nephrons Lab Lesson PlanDocument2 pagesNephrons Lab Lesson PlanKian VeracionPas encore d'évaluation
- Kidney Structure and FunctionDocument68 pagesKidney Structure and FunctionAsmara Syed100% (1)
- AUBF Chapter 3-ReviewerDocument4 pagesAUBF Chapter 3-ReviewerSalvani, Shane JudePas encore d'évaluation
- Renal Excretion of Drugs 3Document36 pagesRenal Excretion of Drugs 3Noorulhuda AbbasiPas encore d'évaluation
- 30th January 2021 Combined Test (PSM, Pharmacology, Forensic Medicine, Microbiology, Pathology)Document14 pages30th January 2021 Combined Test (PSM, Pharmacology, Forensic Medicine, Microbiology, Pathology)siddhantaPas encore d'évaluation
- Act 1 Urinary SystemDocument20 pagesAct 1 Urinary Systemisabellamarie.castillo.crsPas encore d'évaluation
- BIOLOGY Form 5 Chapter 3Document52 pagesBIOLOGY Form 5 Chapter 3Shephard Png100% (17)
- Case 8 GUS - AKIDocument210 pagesCase 8 GUS - AKIGroup 12 Sofia HanaPas encore d'évaluation