Académique Documents
Professionnel Documents
Culture Documents
Celecoxib & Ketoprofen For Pain Management
Transféré par
Ubaidillah AfiffDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Celecoxib & Ketoprofen For Pain Management
Transféré par
Ubaidillah AfiffDroits d'auteur :
Formats disponibles
Celecoxib and ketoprofen for pain management during
tonsillectomy: A placebo-controlled clinical trial
ELINA NIKANNE, MD, PHD, HANNU KOKKI, MD, PHD, JUHA SALO, MD, and TIMO-JUSSI LINNA, MD, Kuopio, Finland
OBJECTIVE: To evaluate the efcacy and safety of
celecoxib and ketoprofen in pain management
during tonsillectomy in 120 patients.
STUDY DESIGN AND SETTING: The study was random-
ized, double-blind, and placebo-controlled with
parallel groups. Sixty minutes before anesthesia in-
duction and 12 hours after, the patients received a
200-mg celecoxib, a 100-mg ketoprofen, or a pla-
cebo capsule. After discharge, patients were pre-
scribed either celecoxib or ketoprofen capsules to
be taken every 12 hours.
RESULTS: During the rst 24 hours, the need for res-
cue analgesic was less in the ketoprofen-group (5
[1-9]) doses (median [range]) than in the placebo-
group (6 [1-13]) (P 0.021), but similar to the cele-
coxib-group (5 [2-14]). After discharge, the cessa-
tion of pain during eating occurred earlier in the
celecoxib-treated patients, after 10 (1-17) days,
than in the ketoprofen-treated patients, after 12 (1-
21) days, (P 0.008). One celecoxib-treated pa-
tient and 6 ketoprofen-treated patients (P 0.013)
needed electrocautery to stop postoperative
bleeding.
CONCLUSION: Ketoprofen provided a better initial
analgesic efcacy but after discharge the recovery
with celecoxib was faster and the incidence of sec-
ondary hemorrhages was lower.
SIGNIFICANCE: Celecoxib seems to be more effec-
tive and safe than ketoprofen for pain manage-
ment after discharge in patients with tonsillectomy.
(Otolaryngol Head Neck Surg 2005;132:287-94.)
Most patients experience intensive pain after tonsil-
lectomy, which may delay return to normal daily ac-
tivities, such as eating, drinking, and sleeping, for sev-
eral days.
1-3
Opioid analgesics provide pain relief in a
dose-dependent manner, but several adverse effects,
such as emesis, constipation, excessive sedation, and
risk of respiratory depression, can inhibit their abun-
dant use.
Conventional nonsteroidal anti-inammatory drugs
(NSAIDs) are potent analgesics and can reduce signif-
icantly the need for postoperative opioids. During ton-
sillectomy ketoprofen, a conventional NSAID of the
phenylpropionic acid derivatives group, has a signi-
cant opioid sparing effect.
4,5
However, a concern re-
garding the use of ketoprofen is the risk from postop-
erative bleeding, because conventional NSAIDs
prolong the bleeding time by inhibiting the biosynthesis
of thromboxane A
2
that can consequently increase
blood loss during and after surgery.
6
Ketoprofen inhibits both cyclo-oxygenase-1 (COX-1)
and COX-2, but the most recent NSAIDs, eg, celecoxib,
act mainly on COX-2 with less inhibition on COX-1.
Theoretically, the COX-2 selective NSAIDs should have
no or less effect on platelet aggregation, and thus cause
low risk for intra- and postoperative bleeding.
6
In the
management of long-lasting pain by osteoarthritis and
rheumatoid arthritis, the new COX-2 selective NSAIDs
are as effective as conventional NSAIDs. However, only
a few trials have evaluated the effectiveness and safety of
celecoxib in the management of acute pain.
7,8
The aim of the recent study was to evaluate the
analgesic efcacy and safety of celecoxib in the man-
agement of pain after tonsillectomy, a pain model
known to cause signicant pain and increased risk for
postoperative bleeding. For the rst 24 hours, the study
was a 3-arm trial with the ketoprofen group performing
as an active control and a placebo group as an internal
evidence for assay sensitivity. The primary outcome
parameter was the consumption of rescue analgesic
during the rst 24 hours after surgery, and the second-
ary outcome parameter the amount of surgical blood
loss. After discharge, the trial was continued with 2
active arms. The efcacy of celecoxib and ketoprofen
was evaluated by the duration of signicant pain, the
recovery of normal daily activities, and for safety by
the incidence of postoperative hemorrhage and other
adverse effects.
METHODS
The study was approved by our Ethics Committee,
was conducted in accordance with the Declaration of
From the Department of Otorhinolaryngology (Drs Nikanne, Salo, and
Linna), Central Hospital of Central Finland, and the Departments of
Anesthesiology and Intensive Care, Kuopio University Hospital, and
Pharmacology and Toxicology, University of Kuopio, Finland (Dr
Kokki).
This study was not nancially supported from any external sources.
Reprint requests: Hannu Kokki, MD, PhD, Department of Anesthesiology and
Intensive Care, Kuopio University Hospital, PO Box 1777, FIN-70211
Kuopio, Finland; e-mail, hannu.kokki@kuh..
0194-5998/$30.00
Copyright 2005 by the American Academy of OtolaryngologyHead and
Neck Surgery Foundation, Inc.
doi:10.1016/j.otohns.2004.09.005
287
Helsinki,
9
and the National Agency for Medicines was
notied of the trial protocol. Informed written consent
was obtained from each patient during the preoperative
visit.
One hundred twenty healthy patients, aged 16-47
years and scheduled to undergo tonsillectomy with 24
hours follow-up in hospital, were enrolled. All patients
gave their consent, but 2 patients withdrew their con-
sent before surgery (reason not specied). All patients
were included unless there was any contraindication for
anti-inammatory drugs, paracetamol, codeine, or oxy-
codone in their detailed medical and surgical history or
in a complete physical examination of vital signs. Pa-
tients with a known allergy to ketoprofen, celecoxib, or
other nonsteroidal anti-inammatory drugs, asthma,
any kidney or liver dysfunction, or a hemorrhagic dia-
thesis and sulphonamide allergy were excluded. During
the preoperative visit and on the morning before sur-
gery, the patients were instructed in the use of an
11-point numeric pain rating scale (NRS).
10
A prospective, randomized (by a computer-gener-
ated randomization sequence with sealed enveloped
method), double-blind, placebo- and active-controlled,
parallel group study design was used in the hospital.
Sixty minutes before anesthesia and 12 hours after, the
patients in the celecoxib group (n 40) received cele-
coxib 200 mg capsule (Celebra, Pharmacia Oy, Vantaa,
Finland) and in the ketoprofen group (n 37) keto-
profen 100 mg capsule (Orudis, Aventis Pharma, Hel-
sinki, Finland) by mouth with 50 mL of water. The
dosage of celecoxib and ketoprofen was based on an
approved summary of product characteristics. Patients
in the placebo group (n 40) received placebo capsule
respectively (Fig 1).
The same endotracheal anesthesia was used for each
patient. Premedication comprised of 10 mg diazepam
tablet 60 minutes before induction. Fentanyl 1 g kg
1
IV was given and anesthesia was induced with thiopen-
tal 5 mg kg
1
IV, and tracheal intubation was facili-
tated with mivacurium 0.2 mg kg
1
. At incision a
second dose of fentanyl 1 g kg
1
was given, and no
more opioids were allowed during the surgery. Anes-
thesia was maintained with sevourane in 35% oxygen
in nitrous-oxide with intermittent positive pressure ven-
tilation. On completion of the procedure, the tracheal
Fig 1. Trial prole.
Otolaryngology
Head and Neck Surgery
288 NIKANNE et al February 2005
tube was removed when respiration was regular and
adequate in rate and depth.
The tonsils were removed using electrodissection
technique using electrocautery set at 20-30 W (Valley-
lab PTY Ltd., Australia) by an experienced surgeon.
Hemostasis was achieved during the dissection with
cautery current and, if needed, with compression of the
surgical area and ligation. The intraoperative blood loss
in milliliters was assessed by making a visual estima-
tion of blood lost on sponges and collected in a suction
bottle.
After surgery, the patients were transferred to the
postanesthesia care unit (PACU) for continuous moni-
toring of vital signs and the assessment of pain and
adverse events. After 4 hours of observation in the
PACU, the patients were transferred to the ward.
The patients expressed pain on an 11-point NRS (0
no pain, 10 worst pain)
10
at rest and during
swallowing continuously, and scores were recorded at
1, 2, 3, 4, and 24 hours after surgery. If the patient was
in pain (pain score 3 at rest or 5 during swallowing)
oxycodone, 0.05 mg kg
1
IV in the PACU or 0.1 mg
kg
1
IM on the ward, was given for rescue analgesia.
The IV dose was repeated at 10 minute intervals until
the patient was comfortable. A maximum of 3 doses of
oxycodone was allowed in 1 hour. No additional anal-
gesic medication was permitted during the study. The
worst and the average level of pain during the PACU
stay and at the ward during the rst 24 hours were also
recorded. The number of oxycodone doses needed and
all adverse events were recorded and summarized for
each patient.
The patients were discharged the day after surgery.
After discharge, the patients in the celecoxib-group and
29 patients from the placebo-group were instructed to
use celecoxib 200 mg capsules, and the patients in the
ketoprofen-group and 10 patients from the placebo
group were told to take ketoprofen 100 mg capsules at
every 12 hours for the rst 5 days and thereafter if
needed. For rescue analgesia at home, all patients were
prescribed paracetamol-codeine effervescent tablets
(Panacod, paracetamol 500 mgcodeine 30 mg/tablet,
Sano Synthelabo, Solna, Sweden), a maximum of 8
tablets in 24 hours (a single dose in patients under 50 kg
one-half tablet and in patients over 50 kg 1 tablet).
At discharge, patients received a follow-up chart
where they were instructed to record the intensity of
postoperative pain and the pain relief achieved with
medication on an 11-point NRS. The interference of
pain with normal activities of daily living (drinking,
eating, speech, sleep, general activity, mood, relation
with other people) was assessed on an 11-point numeric
rating scale (0 does not interfere, 10 completely
interferes). The use of study medication and the number
of paracetamol-codeine-tablets for rescue analgesia
were reported. Awakenings during the nights and all
adverse events were also recorded. All the information
was recorded on a follow-up chart rst thing in the
morning on the second, third, fourth, and seventh post-
operative day.
At 3 weeks, the patients were phoned and the fol-
lowing information was recorded: the cumulative cele-
coxib/ketoprofen and paracetamol-codeine doses, the
number of days with postoperative pain, the rst day
with no pain during drinking and eating, and the num-
ber of nights with awakenings due to postoperative
pain. Patients were also asked whether the pain relief
had been achieved and whether there were any prob-
lems in taking the capsules or tablets. All adverse
effects were recorded. After discharge, patients esti-
mated the degree of postoperative bleeding using a
3-point scale (1 no bleeding, 2 some bleeding, 3
profuse bleeding requiring contact with health care
professionals) and any need for further medical contact
was registered.
Postoperative bleeding was classied as insigni-
cant if no medical attention was required, minor if
medical attention was required and intravenous uid or
suction of the clot was initiated, and major, if electro-
cautery, re-operation, or blood transfusion was re-
quired. Postoperative bleeding was classied as a pri-
mary hemorrhage if it occurred during the rst 24 hours
after surgery and as a secondary when it occurred later.
Power analysis based on our pilot study suggested
that 40 patients per group would need to be enrolled to
have an 80% chance at the 0.05 level of signicance for
detecting a 35% reduction in the need for rescue anal-
gesic (3 vs 2 doses, SD 1.5 doses) between the 2 active
groups.
The
2
test or Fishers exact test was used to analyze
the differences between the groups for the frequency
data, eg, gender, need for rescue analgesia, and the
number of patients with vomiting. The differences be-
tween the 3 groups concerning continuous variables,
such as the height, weight, and age, and the pain scores
were analyzed by the Kruskal-Wallis test, and the
MannWhitney test with Bonferonni correction was
used for post hoc analysis. Two-tailed signicance was
obtained and P 0.05 was considered statistically
signicant. The results are presented as the number of
cases or median and range. All the data were analyzed
using a statistical program (SPSS for Windows 11.5,
SPSS Inc, Chicago, IL).
RESULTS
The patients and surgical characteristics were com-
parable in the 3 groups (Table 1). One hundred eighteen
patients entered the study, but 2 patients were with-
Otolaryngology
Head and Neck Surgery
Volume 132 Number 2 NIKANNE et al 289
drawn due to protocol violations and 1 due to a medical
condition, leaving 115 evaluable patients. After dis-
charge 4 patients were withdrawn; 2 celecoxib-treated
patients developed allergic reaction and 1 was readmit-
ted due to intensive pain, and 1 ketoprofen-treated
patient developed protracted vomiting. Four celecoxib-
treated and 5 ketoprofen-treated patients were lost to
follow-up. After 1 week, 108 follow-up diaries (94%)
were returned and at 3 weeks telephone interviews were
completed for 102 patients (89%) (Fig 1).
There was no difference between the celecoxib-
group and ketoprofen-group in the operation duration
or surgical blood loss, but in the placebo-group both the
duration (P 0.03) and the blood loss was higher than
in the celecoxib-group (P 0.039) (Table 1).
All patients in the celecoxib-group, 32 of 37 patients
in the ketoprofen-group (86%) (P 0.024, celecoxib
vs ketoprofen) and 37 of 39 patients in the placebo-
group (95%) were provided oxycodone for rescue an-
algesia during the rst 4 hours after surgery. In the
celecoxib-group, the time to the rst dose of rescue
analgesic was signicantly shorter than in the ketopro-
fen-group (P 0.039) (Figs 2 and 3).
All patients were provided rescue analgesia during
the rst 24 hours after surgery. The total number of
oxycodone doses was 215 in the celecoxib group, 179
doses in the ketoprofen group, and 230 doses in the
placebo group (P 0.021, placebo vs ketoprofen) (Fig
2).
The pain scores during the rst 24 hours were
closely similar in the celecoxib group and in the keto-
profen group, but at 2 hours the pain scores on swal-
lowing were signicantly lower in the ketoprofen group
than in the placebo group (P 0.05) (Fig 4).
At the end of the rst postoperative week, all except
1 patient had pain during swallowing. Among the cele-
coxib-treated patients, 19 of 65 (29%) reported signif-
icant pain at rest (NRS 3) and 24 (37%) on swallow-
ing (NRS 5) compared to the ketoprofen-treated
patients with 20 of 41 (49%) patient reporting signi-
cant pain at rest and on swallowing. At the end of the
rst week 44 of 65 (67%) patient used celecoxib at a
regular basis compared to 37 of 41 (91%) patient using
ketoprofen regularly (P 0.002).
All the activities of normal daily living were signif-
icantly affected in both the celecoxib- and ketoprofen-
treated patients. Eating was the activity most severely
disturbed as a consequence of pain, and at the end of
rst week only 9 (14%) celecoxib-treated patients and
4 (10%) ketoprofen-treated patients were able to eat
Table 1. Patient characteristics and surgical data of the two study groups. Data are median (minimum-
maximum) or number of cases
Celecoxib group
(n 39)
Ketoprofen group
(n 37)
Placebo group
(n 39)
Gender (male/female) 16/23 19/18 16/23
Age (y) 21 (16-47) 22 (16-45) 22 (16-42)
Weight (kg) 68 (46-110) 68 (47-96) 68 (48-107)
Height (cm) 175 (155-191) 172 (153-189) 172 (159-196)
Diagnosis: Tonsillitis recidivans/ Status post abscessus
peritonsillaris/Hypertrophia tonsillae
34/4/1 33/2/2 32/4/3
Operation duration (min) 17 (6-52) 20 (8-47) 22 (8-59)*
Surgical-blood loss (mL) 5 (1-280) 8 (1-100) 20 (1-250)
*P 0.03.
P 0.039, Mann-Whitney test with Bonferroni correction placebo compared to celecoxib.
Fig 2. Box plots (showing 10th, 25th, 50th, 75th, and 90th
centiles and outliers) of supplementary analgesic doses
during the rst 24 hours according study group. (*P
0.021, placebo compared to ketoprofen, Mann-Whitney
test with Bonferroni correction.)
Otolaryngology
Head and Neck Surgery
290 NIKANNE et al February 2005
without pain. However, the cessation of signicant pain
during eating occurred a median of 2 days earlier in the
celecoxib-treated patients than in the ketoprofen-
treated patients (P 0.008) (Tables 2 and 3).
At 3 weeks, none of the patients reported signicant
pain, and only 3 reported mild pain at rest and 12
during swallowing. At 3 weeks, 14 patients (9 cele-
coxib-treated and 5 ketoprofen-treated) reported that
pain had still interference on daily activities.
The satisfaction with the analgesic treatment was
closely similar in both groups, the median (range) score
on a scale 0completely satised to 10completely
unsatised was 1 (0-9) among the celecoxib-treated
patients and 2 (0-9) among the ketoprofen-treated pa-
tients. The analgesic efcacy of celecoxib and ketopro-
fen combined with paracetamol-codeine was also as-
sessed as being closely similar, where median score
was 2 (0-9) in both groups.
One primary hemorrhage occurred in the ketoprofen
group and the patient required electrocautery under
local anesthesia to stop bleeding. A major secondary
hemorrhage occurred in 1 celecoxib-treated patient and
in 5 ketoprofen-treated patients (P 0.026). All 6
patients required electrocautery under local anesthesia
to stop the bleeding but no blood transfusions were
needed (Table 4).
A total of 271 adverse events were reported by 104
patients. Thirty-four (30%) vomited, 28 (24%) devel-
oped nausea, and 31 (27%) constipation. Two of the 68
celecoxib-treated patients developed allergic reaction, 4
developed rashes and 1 patient developed a face edema
compared to none of the ketoprofen-treated patients
(Table 4).
DISCUSSION
The primary outcome parameter was the consump-
tion of rescue analgesic during the rst 24 hours after
surgery. Ketoprofen 100 mg by mouth 1 hour before
and 12 hours after surgery seemed to performed better
than 2 doses of celecoxib 200 mg, because only the
ketoprofen-treated patients needed less rescue analgesia
during the rst 24 hours after tonsillectomy compared
to the patients in the placebo group. However, in a post
hoc analysis, it was revealed that the celecoxib-treated
patients needed several doses of rescue analgesic only
during the rst 4 postoperative hours. During the next
20 hours, analgesic consumption was similar in the 2
active treatment groups, and, in both groups, it was less
than in the placebo group. Moreover, after discharge,
celecoxib 200 mg bid seemed to provide a better anal-
gesia than ketoprofen 100 mg administered correspond-
ingly because the celecoxib-treated patients were able
to return to their normal daily activities earlier than the
ketoprofen-treated patients.
The slow onset of an analgesic effect of celecoxib
compared to ketoprofen may be explained by pharma-
cokinetic and pharmacodynamic differences between
these 2 compounds. First, ketoprofen is absorbed
readily after oral administration with the time to peak
plasma concentration occurring after 1 hour,
11
whereas
the absorption of celecoxib is moderate, the peak con-
centration occurs after 2 to 4 hours.
12
Second, the 11
hours half life of celecoxib
13
is signicantly longer than
that of ketoprofen, which is 2 hours.
11
This is a signif-
icant difference because it takes 5 half-lives before the
steady state plasma concentration of a drug is reached.
Fig 3. Box plots (showing 10th, 25th, 50th, 75th, and 90th)
of time to supplementary analgesia in minutes accord-
ing study group. (*P 0.039 celecoxib compared to
ketoprofen, Mann-Whitney test with Bonferroni correc-
tion.)
Fig 4. Pain on swallowing. (*P 0.05, placebo compared
to ketoprofen, Mann-Whitney test with Bonferroni correc-
tion.)
Otolaryngology
Head and Neck Surgery
Volume 132 Number 2 NIKANNE et al 291
With ketoprofen, the steady state concentration should
have been reached within the rst 24 hours; with cele-
coxib, it may have occurred only on day 2 or day 3.
Third, the volume of distribution of celecoxib is signif-
icantly larger, 455 L, compared to ketoprofen, 8 to 14
L. These differences may explain why celecoxib per-
formed less efciently during the rst hours after sur-
gery although it was superior compared to ketoprofen
later. Whether a higher initial dose of celecoxib (400
mg) or earlier administration of the rst dose would
have performed better is open for discussion. However,
the fact that the patients who had received celecoxib
recovered earlier than the patients who had received
ketoprofen is considered important. Recovery of nor-
mal daily activities, such as eating, drinking, and sleep-
ing, is important not only for the patient, but also for the
community because it is just after these activities have
been normalized that the patient is able to return back
to work.
Other studies with tonsillectomy have also found a
better immediate analgesic efcacy with conventional
NSAIDs, but, in the continuation of pain management,
new generation COX-2 selective inhibitors have per-
formed better.
14
The perception of acute pain is more
likely to be modulated by cyclo-oxygenase-1 as time
for induction must elapse for COX-2.
15
It seems that
the COX-1 inhibition is needed to provide appropriate
analgesic efcacy in cases where severe acute pain is
caused by for example surgical trauma. Later, when
COX-2 expression may play a more important role in
the continuation of hyperalgesia, COX-2 inhibitors
seem to perform efciently.
The efcacy of celecoxib during tonsillectomy has
been evaluated in 2 clinical trials. In the rst trial of
celecoxib 200 mg by mouth 30 minutes before otolar-
yngologic surgery alone was no more effective than
placebo or paracetamol 2000 mg in reducing postoper-
ative pain.
16
In a dose-nding study, celecoxib 400 mg
was more effective than celecoxib 200 mg in reducing
postoperative pain, but the lower dose did not perform
better than placebo in the early postoperative period.
17
Unfortunately, in these 2 studies, the patients were
provided with a single dose of celecoxib only and the
follow-up consisted only the rst 24 hours after the
surgery so the efcacy of celecoxib on cessation of
postoperative pain and on full recovery after surgery is
not known. Because signicant pain after tonsillectomy
may last for 1 to 2 weeks
3
further follow-up studies
with COX-2 selective inhibitors are needed.
Operative site bleeding is a concern during tonsil-
lectomy. In the present trial, no clinically signicant
differences in the intraoperative bleeding was seen be-
tween the patients who had received celecoxib, keto-
profen, or placebo. Patients were operated on with an
Table 2. The secondary outcome endpoints after discharge in the two study groups. Data are median
(minimum - maximum).
Celecoxib-treated
patients (n 66)
Ketoprofen-treated
patients (n 42) P
Number of study drug doses 28 (6-32) 28 (12-30) 0.47
Number of rescue analgesic doses 35 (0-120) 36 (6-112) 0.92
Duration of analgesic treatment (d) 14 (3-21) 14 (8-18) 0.64
Cessation of signicant pain during drinking (d) 7 (0-14) 8 (0-21) 0.055
Cessation of signicant pain during eating (d) 10 (1-17) 12 (1-21) 0.008
Normal night sleep (d) 7 (0-14) 8 (0-14) 0.097
Normal daily activities (d) 14 (3-20) 14 (4-21) 0.92
Table 3. Interfere of pain on daily activities. Data are worst scores expressed during the rst week after
surgery on an 11-point scale, 0 does not interfere, 10 completely interfere. Data are median
(minimum-maximum).
Celecoxib-treated
patients (n 66)
Ketoprofen-treated
patients (n 42) P
General daily activities 6 (1-10) 6 (1-10) 0.47
Drinking 5 (1-9) 4 (2-9) 0.57
Eating 7 (2-10) 7 (2-10) 0.93
Speech 6 (0-9) 6 (1-10) 0.36
Sleep 5 (0-9) 4 (0-9) 0.39
Mood 4 (0-10) 5 (0-10) 0.69
Relations to other people 5 (1-9) 6 (0-9) 0.79
Otolaryngology
Head and Neck Surgery
292 NIKANNE et al February 2005
electrocautery technique and based on our clinical ex-
perience, the amount of bleeding is relatively small
with this technique. However, the celecoxib-treated
patients experienced less secondary hemorrhage than
the patients who had received ketoprofen. All together
6 patients experienced major secondary bleeding; 5 of
them had received ketoprofen and 1 celecoxib. All the
patients were treated with electrocautery with local
anesthesia and recovered without any further compli-
cations. The lower number of bleeding episodes in the
celecoxib group is in agreement with the expectations
because COX-2 selective NSAIDs do not affect platelet
aggregation and should cause less risk for perioperative
bleeding than the conventional NSAIDs.
6
In our study, a high number (90%) of the patients
reported adverse effects. The logical explanation is that
every event the patient reported was noted, but this
approach does not allow causality assessment. The
most frequently reported adverse effects, somnolence,
vomiting, constipation, and nausea are, however, more
likely connected with anesthetic drugs, codeine, or sur-
gery than the NSAIDs. On the contrary, some adverse
effects are likely to be caused by the study drugs.
Conventional NSAIDs can cause a direct local injury to
the gastric mucosa whereas COX-2 selective agents
should exert a decreased risk for gastrointestinal ad-
verse effects.
18
In the present trial, however, the inci-
dence of gastrointestinal adverse effects was similar in
the 2 groups. Nine patients reported symptoms of hy-
persensitivity reactions with celecoxib. As celecoxib
contain sulphonamide, there is a risk for hypersensitiv-
ity reactions, caution should be exercised in prescribing
celecoxib for patients with a history of allergic-type
reactions to NSAIDs or sulphonamides.
In conclusion, in patients with tonsillectomy, keto-
profen provided a better analgesic efcacy during the
rst 24 hours after surgery, but, after discharge, cele-
coxib allowed the patients to return to their normal
daily activities earlier. Secondary hemorrhage occurred
more commonly with ketoprofen, but the incidence of
other adverse effects was closely similar between the 2
drugs.
REFERENCES
1. Toma AG, Blanshard J, Eynon-Lewis N, et al. Post-tonsillec-
tomy pain: the rst ten days. J Laryngol Otol 1995;109:963-4.
(Grade C)
2. Virtaniemi J, Kokki H, Nikanne E, et al. Ketoprofen and fentanyl
for pain after uvulopalatopharyngoplasty and tonsillectomy. La-
ryngoscope 1999;109:1950-4. (Grade B)
3. Salonen A, Kokki H, Nuutinen J. Recovery after tonsillectomy in
adults: a three-week follow-up study. Laryngoscope 2002;112:
94-8. (Grade C)
4. Tarkkila P, Saarnivaara L. Ketoprofen, diclofenac or ketorolac
for pain after tonsillectomy in adults. Br J Anaesth 1999;82:56-
60. (Grade A)
5. Salonen A, Kokki H, Tuovinen K. IV ketoprofen for analgesia
after tonsillectomy: comparison of pre- and postoperative admin-
istration. Br J Anaesth 2001;86:377-81. (Grade A)
6. Leese P, Hubbard R, Karim A, et al. Effects of celecoxib, a novel
cyclooxygenase-2 inhibitor, on platelet function in healthy
adults: a randomized, controlled trial. J Clin Pharmacol 2000;40:
124-32. (Grade A)
7. Gimbel JS, Brugger A, Zhao W, et al. Efcacy and tolerability of
celecoxib versus hydrocodone/acetaminophen in the treatment of
pain after ambulatory orthopaedic surgery in adults. Clinical
Therapeutics 2001;23:228-41. (Grade A)
8. Malmstrm K, Daniels S, Kotey P, et al. Comparison of rofe-
coxib and celecoxib, two cyclooxygenase-2 inhibitors, in post-
operative dental pain: a randomized, placebo- and active-com-
parator-controlled clinical trial. Clin Ther 1999;21:1653-63.
(Grade A)
9. World Medical Association Declaration of Helsinki. Ethical
Principles for Medical Research Involving Human Subjects.
52nd World Medical Association, General Assembly, Edin-
burgh, Scotland, October 2000. (Grade A)
10. American Pain Society Quality of Care Committee. Quality
improvement guidelines for the treatment of acute pain and
cancer pain. JAMA 1995;274:1874-80. (Grade A)
11. Upton RA, Williams RL, Guentert TW, et al. Ketoprofen phar-
macokinetics and bioavailability based on an improved sensitive
Table 4. Adverse events after discharge. *Data
are number of cases.
Celecoxib-
treated
patients
(n 68)
Ketoprofen-
treated patients
(n 47) P
Patients with one or more
adverse events
61 43
Total number of adverse
events
152 119
Adverse event
Vomiting 17 17
Nausea 21 7
Abdominal pain 4 2
Constipation 18 13
Somnolence 26 21
Dizziness 4 6
Confusion 5 6
Allergic reaction 2
Rash 4
Face/mouth edema 3
Tongue edema 4
Glossitis 2 2
Larynx pain 2 3
Taste perversion 1 2
Respiratory insufciency 2
Headache 2 2
Sweating increased 3
Fever 1 2
Major bleeding 1 5 0.026
Minor bleeding 6 1
Insignicant bleeding 20 15
*Adverse events with a single mention.Celecoxib-treated patients: atulence,
emotional lability, paroniria, nervousness, larynx edema, rhinitis, pruritus,
sputum increased, coughing, hypotension.
Ketoprofen-treated patients; eructation, diarrhea, abdominal rumbling, halluci-
nation, pruritus, muscle weakness, thirst, shivering.
Otolaryngology
Head and Neck Surgery
Volume 132 Number 2 NIKANNE et al 293
and specic assay. Eur J Clin Pharmacol 1981;20:127-33. (Grade
B)
12. Paulson SK, Vaughn MB, Jessen SM, et al. Pharmacokinetics of
celecoxib after oral administration in dogs and humans: effect of
food and site of absorption. J Pharmacol Exp Ther 2001;297:
638-45. (Grade B)
13. Wynn RL. The new COX-2 inhibitors: rofecoxib (Vioxx) and
celecoxib (Celebrex). Gen Dent 2000;48:16-20. (Grade B)
14. Aho M, Kokki H, Nikanne E. Nimesulide versus ibuprofen for
postoperative tonsillectomy pain: a double blind, randomised,
and active comparator controlled clinical trial. Clin Drug Invest
2003;23:651-60. (Grade A)
15. Mitchell JA, Warner TD. Cyclo-oxygenase-2: pharmacology,
physiology, biochemistry and relevance to NSAID therapy. Br J
Pharmacol 1999;128:1121-32. (Grade B)
16. Issioui T, Klein KW, White PF, et al. The efcacy of premedi-
cation with celecoxib and acetaminophen in preventing pain after
otolaryngologic surgery. Anesth Analg 2002;94:1188-93. (Grade
A)
17. Recart A, Issioui T, White PF, et al. The efcacy of celecoxib
premedication on postoperative pain and recovery times after
ambulatory surgery: a dose-raging study. Anesth Analg 2003;96:
1631-5. (Grade A)
18. Rowbotham DJ. COX-2 selective inhibitors: clinical relevance in
surgical and acute pain. Eur J Anaesthesiol 2002;25(Suppl):11-
20. (Grade B)
Otolaryngology
Head and Neck Surgery
294 NIKANNE et al February 2005
Vous aimerez peut-être aussi
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYD'EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYPas encore d'évaluation
- Dolor Postop, Ligamentos Cruzados, AmbulatorioDocument7 pagesDolor Postop, Ligamentos Cruzados, AmbulatorioChurrunchaPas encore d'évaluation
- JCM 08 02014 v2Document9 pagesJCM 08 02014 v2burhanPas encore d'évaluation
- 0 Aet484Document7 pages0 Aet484UsbahPas encore d'évaluation
- Effect of Pharyngeal Packing During Nasal SurgeryDocument12 pagesEffect of Pharyngeal Packing During Nasal SurgeryRahma R SPas encore d'évaluation
- 1828 1833Document6 pages1828 1833abdulPas encore d'évaluation
- 与扑热息痛联用增效Document5 pages与扑热息痛联用增效zhuangemrysPas encore d'évaluation
- Effects of Propofol Anesthesia Versus SevofluraneDocument33 pagesEffects of Propofol Anesthesia Versus SevofluraneJuwita PratiwiPas encore d'évaluation
- 404 2019 Article 5260Document7 pages404 2019 Article 5260Farida SiggiPas encore d'évaluation
- Analgesic Efficacy of The Cyclooxygenase-2Specific Inhibitor Rofecoxib in Post-Dental Surgery Pain: A Randomized, Controlled TrialDocument11 pagesAnalgesic Efficacy of The Cyclooxygenase-2Specific Inhibitor Rofecoxib in Post-Dental Surgery Pain: A Randomized, Controlled TrialLeo AlbertoPas encore d'évaluation
- EpinephrineDocument5 pagesEpinephrinesheynnaPas encore d'évaluation
- Eledjam1991 Article BrachialPlexusBlockWithBupivac PDFDocument6 pagesEledjam1991 Article BrachialPlexusBlockWithBupivac PDFKalpanaPas encore d'évaluation
- RCT Parecoxib Acetaminophen...Document7 pagesRCT Parecoxib Acetaminophen...Paulina MuñozPas encore d'évaluation
- The Effects of Anesthetic Technique On Postoperative Opioid Consumption in Ankle Fracture SurgeryDocument16 pagesThe Effects of Anesthetic Technique On Postoperative Opioid Consumption in Ankle Fracture SurgeryGio VandaPas encore d'évaluation
- International Journal of Anesthetics and Anesthesiology Ijaa 7 118Document7 pagesInternational Journal of Anesthetics and Anesthesiology Ijaa 7 118Ferdy RahadiyanPas encore d'évaluation
- Efficacy of Dexamethasone For Reducing Postoperative Nausea and Vomiting and Analgesic Requirements After ThyroidectomyDocument4 pagesEfficacy of Dexamethasone For Reducing Postoperative Nausea and Vomiting and Analgesic Requirements After ThyroidectomyDr shehwarPas encore d'évaluation
- The Impact of Preemptive Perianal Anaesthetic Block in Open Haemorrhoidectomy - A Randomised Controlled TrialDocument3 pagesThe Impact of Preemptive Perianal Anaesthetic Block in Open Haemorrhoidectomy - A Randomised Controlled TrialhrtfdnbzvwPas encore d'évaluation
- Small-Dose Ketamine Infusion Improves Postoperative Analgesia and Rehabilitation After Total Knee ArthroplastyDocument6 pagesSmall-Dose Ketamine Infusion Improves Postoperative Analgesia and Rehabilitation After Total Knee ArthroplastyArturo AlcantaraPas encore d'évaluation
- Effect of Ketofol On Pain and Complication After Caesarean Delivery Under Spinal Anaesthesia: A Randomized Double-Blind Clinical TrialDocument4 pagesEffect of Ketofol On Pain and Complication After Caesarean Delivery Under Spinal Anaesthesia: A Randomized Double-Blind Clinical TrialHaryoko AnandaputraPas encore d'évaluation
- Asfr 2 QrqwasfcagsevDocument6 pagesAsfr 2 QrqwasfcagsevkennydimitraPas encore d'évaluation
- Efficacy Lidocaine Endoscopic Submucosal DissectionDocument7 pagesEfficacy Lidocaine Endoscopic Submucosal DissectionAnonymous lSWQIQPas encore d'évaluation
- Is Ginger Effective in Reducing Post-Tonsillectomy Morbidity? A Prospective Randomised Clinical TrialDocument6 pagesIs Ginger Effective in Reducing Post-Tonsillectomy Morbidity? A Prospective Randomised Clinical TrialRenaldyTandraPas encore d'évaluation
- Postoperative Nausea and Vomiting in OpioidFree Anesthesia Versus Opioid Based Anesthesia in Laparoscopic CholecystectomyDocument8 pagesPostoperative Nausea and Vomiting in OpioidFree Anesthesia Versus Opioid Based Anesthesia in Laparoscopic Cholecystectomypepe4dwinPas encore d'évaluation
- 10.1007@s00405 020 05801 6Document6 pages10.1007@s00405 020 05801 6Leonardo GuimelPas encore d'évaluation
- 2264-Article Text-5024-4-10-20151024Document6 pages2264-Article Text-5024-4-10-20151024shivamPas encore d'évaluation
- Acta Anaesthesiologica Taiwanica: Research PaperDocument6 pagesActa Anaesthesiologica Taiwanica: Research PaperStela MpPas encore d'évaluation
- Epiduroscopy Transforaminal Egyptian Society of Pain Ahmed El MollaDocument12 pagesEpiduroscopy Transforaminal Egyptian Society of Pain Ahmed El MollaProf. Dr. Ahmed El MollaPas encore d'évaluation
- Effect of Dexamethasone On The Duration of Interscalene Nerve Blocks With Ropivacaine or BupivacaineDocument8 pagesEffect of Dexamethasone On The Duration of Interscalene Nerve Blocks With Ropivacaine or BupivacaineIda KatarinaPas encore d'évaluation
- SMW 10163 PDFDocument9 pagesSMW 10163 PDFAngela PagliusoPas encore d'évaluation
- Haloperidol Combined With DexamethasoneDocument6 pagesHaloperidol Combined With Dexamethasoneapi-741687858Pas encore d'évaluation
- Efficay TAP Block PDFDocument5 pagesEfficay TAP Block PDFMarius PapuricaPas encore d'évaluation
- Anasthesia 1Document7 pagesAnasthesia 1Rionald SitompulPas encore d'évaluation
- Results and Complications of Spinal Anesthesia in Percutaneous NephrolithotomyDocument4 pagesResults and Complications of Spinal Anesthesia in Percutaneous NephrolithotomyDella Puspita SariPas encore d'évaluation
- 617 08 16 ArticleDocument8 pages617 08 16 Articlewilliam lozaPas encore d'évaluation
- Early Postoperative ComplicationsDocument6 pagesEarly Postoperative Complications49hr84j7spPas encore d'évaluation
- Oral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementDocument9 pagesOral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementSasmira JamalPas encore d'évaluation
- Research ArticleDocument7 pagesResearch Articlenaljnaby9Pas encore d'évaluation
- p6 High Risk PatientDocument6 pagesp6 High Risk Patientika lindaPas encore d'évaluation
- Initial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryDocument6 pagesInitial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryilhamPas encore d'évaluation
- JAnaesthClinPharmacol312191-1284204 033402Document5 pagesJAnaesthClinPharmacol312191-1284204 033402Rusman Hadi RachmanPas encore d'évaluation
- The Addition of Clonidine To Bupivacaine in Combined Femoral-Sciatic Nerve Block For Anterior Cruciate Ligament ReconstructionDocument0 pageThe Addition of Clonidine To Bupivacaine in Combined Femoral-Sciatic Nerve Block For Anterior Cruciate Ligament Reconstructionpshz92Pas encore d'évaluation
- Amalia 163216 - Journal ReadingDocument26 pagesAmalia 163216 - Journal ReadingGhifari FarandiPas encore d'évaluation
- TNF TreatmentDocument9 pagesTNF Treatmentachal12Pas encore d'évaluation
- Dr. - Nataraj - EJCM 132 1888 1893 2023Document7 pagesDr. - Nataraj - EJCM 132 1888 1893 2023vithz kPas encore d'évaluation
- Jurnal 2Document9 pagesJurnal 2Muhammad AgussalimPas encore d'évaluation
- Medi 96 E8514Document4 pagesMedi 96 E8514Syd BarretPas encore d'évaluation
- Effectiveness of Epidural Blood Patch in The Management of Post-Dural Puncture HeadacheDocument6 pagesEffectiveness of Epidural Blood Patch in The Management of Post-Dural Puncture HeadacheFabiola Valdez MaldonadoPas encore d'évaluation
- Piis0007091217365649Document6 pagesPiis0007091217365649I Made AryanaPas encore d'évaluation
- Aep 338Document9 pagesAep 338Luifer AgudeloPas encore d'évaluation
- Batoz 2009 Acute-PainDocument2 pagesBatoz 2009 Acute-PainOmar BazalduaPas encore d'évaluation
- Research ArticleDocument10 pagesResearch ArticlethiaPas encore d'évaluation
- Comparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphineDocument7 pagesComparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphinenatamkpPas encore d'évaluation
- Ameeta Joshi:, Eleni Parara, Tatiana V. MacfarlaneDocument8 pagesAmeeta Joshi:, Eleni Parara, Tatiana V. MacfarlaneGustavo RodríguezPas encore d'évaluation
- Jimbo 2017Document15 pagesJimbo 2017Sahily MoralesPas encore d'évaluation
- Br. J. Anaesth.-2009-Foss-111-6Document6 pagesBr. J. Anaesth.-2009-Foss-111-6alejandropst1664Pas encore d'évaluation
- Ağrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Document4 pagesAğrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Ali ÖzdemirPas encore d'évaluation
- Abuelyazed 2016Document7 pagesAbuelyazed 2016AYŞE GÜLŞAH ATASEVERPas encore d'évaluation
- Intravenous Ketorolac Vs Diclofenac For AnalgesiaDocument6 pagesIntravenous Ketorolac Vs Diclofenac For AnalgesiaMuhammad AgussalimPas encore d'évaluation
- JAnaesthClinPharmacol294459-335648 091924 PDFDocument6 pagesJAnaesthClinPharmacol294459-335648 091924 PDFaltaikhsannurPas encore d'évaluation
- Comparative Study of Epidural Fentanyl and Buprenorphine For Post Operative Analgesia in Lower Abdominal and Lower Limb SurgeriesDocument8 pagesComparative Study of Epidural Fentanyl and Buprenorphine For Post Operative Analgesia in Lower Abdominal and Lower Limb SurgeriesIOSRjournalPas encore d'évaluation
- Practice Advisory On The Appropriate Use of Nsaids in Primary CareDocument15 pagesPractice Advisory On The Appropriate Use of Nsaids in Primary CareAsti IndriyaniPas encore d'évaluation
- Nonsteroidal Anti-Inflammatory Drugs, Disease-Modifying Antirheumatic Drugs, Nonopiod Analgesics, & Drugs Used in GoutDocument1 pageNonsteroidal Anti-Inflammatory Drugs, Disease-Modifying Antirheumatic Drugs, Nonopiod Analgesics, & Drugs Used in GoutLuna Abigail TorresPas encore d'évaluation
- Nama ObatDocument12 pagesNama Obatrolin novitaPas encore d'évaluation
- Unitatea de Măsură Cantitate A Preț Unitar, LeiDocument14 pagesUnitatea de Măsură Cantitate A Preț Unitar, LeivictorPas encore d'évaluation
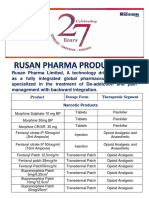
- Rusan Pharma Product ListDocument4 pagesRusan Pharma Product ListSanjay SharmaPas encore d'évaluation
- Lasa ListDocument11 pagesLasa ListerpPas encore d'évaluation
- Laporan Rak NarkotikaDocument18 pagesLaporan Rak NarkotikaaliyahPas encore d'évaluation
- Laporan Fornas Non FornasDocument6 pagesLaporan Fornas Non FornasrestyPas encore d'évaluation
- Opioids: Zainab Sabrie Pharmd MpharmDocument32 pagesOpioids: Zainab Sabrie Pharmd MpharmCabdiladif Ahmed McrfPas encore d'évaluation
- 13-Opioids Lecture 1Document41 pages13-Opioids Lecture 1api-343631539100% (1)
- AnalgesicDocument62 pagesAnalgesicAnjum IslamPas encore d'évaluation
- Opioid Analgesics and AntagonistsDocument8 pagesOpioid Analgesics and AntagonistsNishant KatiyarPas encore d'évaluation
- Miller's Drug Delivery SystemsDocument1 pageMiller's Drug Delivery SystemsNandor KissPas encore d'évaluation
- Ketamin Dan Blok Peritonsiler Untuk Penatalaksanaan Nyeri Post OperasiDocument6 pagesKetamin Dan Blok Peritonsiler Untuk Penatalaksanaan Nyeri Post OperasiranirahmaniPas encore d'évaluation
- Jeffrey L. Leal, MDDocument36 pagesJeffrey L. Leal, MDmemelandPas encore d'évaluation
- Anesthesia Hold List-MedicineDocument2 pagesAnesthesia Hold List-MedicineYogeswary RamachandranPas encore d'évaluation
- Codigos de Productos para SabanaDocument12 pagesCodigos de Productos para Sabanamarlenypilar30Pas encore d'évaluation
- Controlled Substances in Alphabetical OrderDocument17 pagesControlled Substances in Alphabetical Orderthor888888Pas encore d'évaluation
- DUROGESICDocument17 pagesDUROGESICshandybtPas encore d'évaluation
- Daftar Obat PrekusorDocument4 pagesDaftar Obat PrekusornovamunikaPas encore d'évaluation
- WHO Step Ladder For PainDocument5 pagesWHO Step Ladder For PainRizKyImanSariPas encore d'évaluation
- INCB Yellow ListDocument23 pagesINCB Yellow Listsunil_vaman_joshiPas encore d'évaluation
- Ace InhibitorsDocument15 pagesAce InhibitorsCarolyn Conn EdwardsPas encore d'évaluation
- I II III IV V: Description Examples ScheduleDocument1 pageI II III IV V: Description Examples ScheduleAndre PrayogoPas encore d'évaluation
- 9.4.48. 2004 Farre Paracetamol DOLORDocument12 pages9.4.48. 2004 Farre Paracetamol DOLORMonserrat Bello VargasPas encore d'évaluation
- OpioidsDocument29 pagesOpioidsHassan Jahangir100% (1)
- Anti Inflammatory DrugsDocument90 pagesAnti Inflammatory Drugsdrnasim2008817160% (5)
- SO Jan SepDocument28 pagesSO Jan SepApotek FazaPas encore d'évaluation
- Step Ladder in Pain Management (Dr. YNS)Document39 pagesStep Ladder in Pain Management (Dr. YNS)Erick Rangga JuniorPas encore d'évaluation
- Medicine ListDocument14 pagesMedicine Listapi-319888855Pas encore d'évaluation