Académique Documents
Professionnel Documents
Culture Documents
Volume Estimation From Multiplanar 2D Ultrasound Images
Transféré par
Harshoi KrishannaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Volume Estimation From Multiplanar 2D Ultrasound Images
Transféré par
Harshoi KrishannaDroits d'auteur :
Formats disponibles
ELSEVIER
Ultrasound in Med. & Biol., Vol. 22, No. 5. pp. 561-572, 1996
Copyright 0 1996 World Federation for Ultrasound in Medicine & Biology
Printed in the USA. All rights reserved
0301.S629/96 515.00 + .OO
PII: SO301-5629( 96)00022-l
*Original Contribution
VOLUME ESTIMATION FROM MULTIPLANAR 2D ULTRASOUND
IMAGES USING A REMOTE ELECTROMAGNETIC
POSITION AND ORIENTATION SENSOR
S. W. HUGHES, T. J. DARcY,* D. J. MAXWELL,* W. CHIU, A. MILNER, *
J. E. SAUNDERS? and R. J. SHEPPARD~
- Departments of Medical Physics, *Obstetrics & Gynaecology and Paediatrics, Guys and
St. Thomas Hospital Trust, London UK; and Department of Physics, Kings College.
University of London, Strand, London UK
(Received 6 June 1995; in $nal form 21 November 1995)
Abstract-A system is described for calculating volume from a sequence of multiplanar 2D ultrasound
images. Ultrasound images are captured using a video digitising card (Hauppauge Win/TV card) installed
in a personal computer, and regions of interest transformed into 3D space using position and orientation
data obtained from an electromagnetic device (Polbemus, Fastrak). The accuracy of the system was assessed
by scanning 10 water fllled balloons (13-141 mL), 10 kidneys (147-200 mL) and 16 fetal livers (S-37
mL) in water using an Acuson 128XP/lO (5 MHz curvilinear probe). Volume was calculated using the
ellipsoid, planimetry, tetrahedral and ray tracing methods and compared with the actual volume measured
by weighing (balloons) and water displacement (kidneys and livers). The mean percentage error for the
ray tracing method was 0.9 2 2.4%, 2.7 2 2.3%, 6.6 & 5.4% for balloons, kidneys and livers, respectively.
So far the system has been used clinically to scan fetal livers and lungs, neonate brain ventricles and adult
prostate glands.
Key Words: Three dimensional ultrasound, Multiplanar image registration, Volume measurement.
INTRODUCTION
The measurement of volume is becoming increasingly
important in medicine as abnormal volume is often
indicative of abnormal function or pathology. In the
past, attempts have been made to estimate the volume
of an organ or structure from plain X-rays by measur-
ing, for instance, the height, width and depth and as-
suming that the object approximates to a geometric
shape such as an ellipsoid (Dodge et al. 1960; McLach-
lan et al. 1968; Austin 1971 et al. 1977; Levine et al.
1979). This has obvious drawbacks as it is impossible
to accurately describe the shape of an organ from just
three dimensions.
With the advent of tomographic imaging modalities
such as computed tomography (CT), magnetic resonance
imaging (MRI) and positron emission tomography
(PET) it has become possible to obtain a number of
cross-sectional images through an object to enable more
Address correspondence to: Stephen W. Hughes, M.Sc., Medi-
cal Physics Department, St. Thomas Hospital, Lambeth Wing, Lon-
don SE1 7EH UK.
accurate determinations of volume. CT, MR and PET
scanners produce parallel images of known separation
making volume calculations fairly straightforward. Ultra-
sound images are also tomographic in nature, but are
usually acquired by hand and so tend to be multiplanar,
i.e., non-parallel, unevenly spaced and maybe sheared.
Images must be registered in some way to a common
coordinate system before accurate volume calculations
can be made. There are two essential requirements for
calculating volume: ( 1) delineation of a region interest
(ROI) on each image; and (2) knowledge of the position
and orientation of each image with respect to a common
coordinate system.
REGISTRATION OF IMAGES
Various techniques have been developed for regis-
tering ultrasound images. The ultrasound transducer
can be attached to a mechanism to ensure that parallel
images of known separation are acquired. e.g., for
scanning the fetus (Klein et al. 1993), blood vessels
(Blankenhorn et al. 1983; Picot et al. 1993; Pretorius
et al. 1992), heart (Matsumoto et al. 1981; Raichlen
561
ih Llltmsound in Medicme and Biology Volume 37. Numhrr 5. I996
et al. I986 ), prostate ( Hastak et al. 1982) and maxillo-
facial anatomy (Hell et al. 1993).
Motorised pull-back systems for use with intra-
cavity transducers have been reported for imaging the
prostate t Sehgal et al. 1993 ), female urethra
( Kirschener-Hermanns et al. 1994) and transesopha-
geal imaging of the heart (Wollschlager et al. 1989).
In motorised pull-back systems, the distance between
image planes is found by multiplying the pull-back
velocity by the time interval between image acquisi-
tions. In manual pull-back systems, image separation
is measured using a scale beside the catheter. Intravas-
cular catheters can also be used to acquire a 3D data
set, either using the manual pull-back method (Ennis
et al. 1993: Rosenheld et al. 1991, 1992). or rotation
about the central axis ( Kok-Hwee et al. 1994).
Ghosh et al. ( 1982) and Pini et al. ( 1989) describe
a system in which the transducer is held in a rig allowing
only central axis rotation of the transducer. Fine et al.
( 1991 ) describe a similar technique using a hand held
transducer. Knowledge of the angle between image
planes enables image registration to be carried out.
Any system in which the ultrasound probe is
attached to a mechanical device obviously restricts free-
dom of movement in some way. This problem can be
overcome to some extent by connecting the transducer
to an articulated arm that records the position and orienta-
tion as the transducer is scanned across the body (Sawada
et al. 1983: Teicholz et al. 1974). Such arms usually
have variable potentiometers placed at each joint to mea-
sure limb angle.
To allow more or less complete freedom of move-
ment. remote systems for measuring the position and
orientation of an ultrasound transducer are required.
Brinkley et al. ( 1978), King et al. ( 1990), Moritz et al.
( 1983) and Levine et al. ( 1989) describe an acoustic
ranging system. This utilises three spark gaps attached
to a small platform connected to the transducer, and four
microphones placed on a stationary L shaped bar.
The distance between the microphones and spark gaps
is calculated from the time-of-flight of the sound. To
avoid significant errors, the air temperature must be con-
tinually monitored as the velocity of sound in air changes
at a rate of about 2% per 10C and there must be a clear
path between the spark gaps and microphones.
Electromagnetic systems for image registration
have been reported by Gardener et al. ( 1991), Lees et
al. ( 1991 a.b, 1993 ). Kelly et al. ( 1992) and Hodges et
al. ( 1994 ) In all of these systems, an electromagnetic
signal is emitted from a stationary transmitter and de-
tected by a mobile receiver. Both the transmitter and
receiver are constructed from three mutually orthogo-
nal coils of copper wire. The distance and orientation
of the receiver are calculated from the relative strength
of the signals received in each sensing coil. The advan
tage of electromagnetic systems is that the receiver i\
small and light and so can easily be attached to an
ultrasound transducer. A major disadvantage is that
nearby metal and stray electromagnetic signals can
produce errors in the measurements.
MATERIALS AND METHODS
Hardware
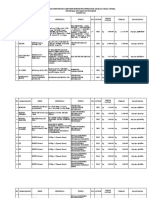
The system that we have developed tits onto a
trolley (Fig. 1) , and comprises an IBM compatible PC
(486 DX2-66, 8 MB memory, 200 MB hard disc)
(ProData 486, Data Products and Services, Inc. Love-
land, CO, USA ) . Ultrasound images are captured using
a video digitising card (Win/TV, Hauppauge Com-
puter Works. Inc., Hauppauge, NY, USA, distributed
in the UK by ODT, London). The image data is stored
in a 1 MB frame buffer in YUV 4: 1: 1 format and then
transferred to the hard disc in various standard image
formats (in this case BMP, Microsoft Windows device
independent bitmap). The video signal is digitised with
a resolution of 7 bits, resulting in 128 grey levels. The
acquisition rate depends on image size. For 328 X 228
pixel images, the acquisition rate is two frames per
second directly to the hard disc.
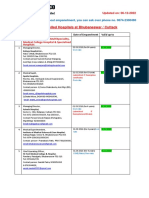
The position and orientation of the ultrasound
transducer is measured using a Polhemus 3Space Fas-
trak system (Polhemus, Inc., Colchester, VT, USA.
distributed in the UK by Virtual Presence, London).
The Fastrak system comprises a transmitter and re-
ceiver, both of which connect to a system electronics
unit (SEU ). The SEU is connected to the PC via a
RS-232 serial link (Fig. 2 ) . The transmitter emits a
8013 Hz electromagnetic signal that is detected by
the receiver. In a metal-free environment, the static
accuracy of the system is specified as 0.8-mm RMS
and 0.15 (2.6 18 X 10 - radians) RMS, and the resolu-
tion, 0.005 mm per cm of range and 0.025 (2.181 x
lo- radians). These values apply when the receiver
is within 76 cm of the centre of the transmitter.
We found that direct placement of the receiver
onto the Acuson l28XP transducer used in this experi-
ment caused skewing of the outlines. To overcome this
problem the receiver was attached to a perspex bar,
which was attached to a moulded plastic shell clipped
onto the transducer case (Fig. 3). The receiver is small
(2.8 X 2.3 X 1.5 cm) and light ( 17 g) and so does
not interfere with normal scanning.
Software
The SEU is controlled by sequences of ASCII
characters transmitted from the PC via the serial link.
Each value is transmitted in binary (4 bytes/number),
Volume estimation from multiplanar 2D ultrasound images 0 S. W. HUGHES et a/. 563
Fig. 1. The main components of the system fit onto a trolley that can easily be transported between hospital
departments and ultrasound machines. The Acuson 128XP scanner is seen in the centre with the PC and Fastrak
on the trolley to the left and the wooden transmitter stand to the right of the examination couch.
at a baud rate of 9600 bits/s; therefore 41 ms are
required to transmit each set of position and orientation
data (seven numbers in total). Position and orientation
data (POD) are acquired immediately after each image
acquisition.
The Win/TV card was programmed using a soft-
ware development kit produced by Hauppauge. The pro-
gram described here was written in C using the Microsoft
Visual C+ + programming environment. Programs were
developed to outline regions of interest (ROIs), trans-
form the outline points to real space, connect the trans-
formed outline points into a series of triangles. and apply
receiver
GlL
transmitter
/
ultrasound transducer
C
video signal from
US machine
Fig. 2. The Fastrak transmitter and receiver are attached to
a systems electronic unit (SEU) , which in turn is connected
to a personal computer (PC) via an RS-232 serial link. The
video signal from any ultrasound machine is connected to a
video capture board within the PC, which enables images to
be displayed in Microsoft Windows and subsequently stored
on disc.
Fig. 3. The Fast& receiver is attached to the ultrasound
transducer by means of a moulded plastic shell and perspex
bar. The receiver is held away from the transducer to reduce
electromagnetic interference from components within the
transducer.
564 Ultrasound in Medicine and Biology Volume 22, Number 5, 1996
the volume calculations. In order to transform the outline
points to real space, the position and orientation of the
Fastrak receiver with respect to the centre of the front
face of the ultrasound transducer must be recorded along
with information such as image calibration factors, etc.
These data are stored as a separate position information
file. Analysis of the results was carried out using a Unix
graphics supercomputer (Titan Kubota Pacific Inc.,
Santa Clara, CA, USA).
Algorithms
extending above the origin and the +z axis extending
out of the page toward the viewer. The 3D coordinate
of any point within an image is calculated by summing
the vectors between the centre of the receiver and a
point on the image, as shown in Fig. 4 where:
p = position vector of image point;
f = position vector of Fastrak receiver;
v1 = vector projecting from Fastrak receiver to a point
above the transducer centre;
v2 = vector projecting from the end of v, to the trans-
ducer centre;
Conversion of image coordinates to Fastrak coor-
dinates. Orientation quarternions are used to calculate
the direction cosines (Cooke et al. 1992) of three vec-
tors that project from the centre of the receiver (Fig.
4). Quarternions were used as only four numbers are
required to encode the same orientation information as
six direction cosines, therefore, the data can be trans-
ferred more quickly. Also quarternions are a more ro-
bust way of encoding directional information, espe-
cially compared to Euler angles where there is an ambi-
guity between yaw and roll at high pitch angles.
v,, vY = vectors pointing in the same direction as the
image x and y axes;
t,, t, = image coordinates of the centre of the trans-
ducer face;
c,, c, = calibration factors in the x and y direction;
Ax, Ay = x,y coordinates of image point relative to
the centre of the transducer face;
Ax = t, - x, Ay = t, - y. where x and y represent
the image coordinates of
a point.
The line-of-sight (LOS) vector projects from the
front face of the receiver, the line-of-hear (LOH) vec-
tor is directed out of the right hand side at right angles
to the LOS, and the line-of-plumb (LOP) vector is
directed downwards at right angles to both the LOS
and LOH vectors (Fig. 4). The coordinate system is
the same as that generally used for graphs with the +x
axis extending to the right of the origin, the +y axis
If v, is in the LOS direction, v2 in the LOP direc-
tion, v, in the LOH direction and v, in the LOS direc-
tion, the coordinates of an image point in Fastrak space
are given by:
PX = fX + 10% Iv,1 + lopxlv*l
+ los,Ayc, + loh,Axc,
py=fy+losy Iv11 +lop, Iv21
+ los,Ayc, + loh,Axc,
Pz = fz + 10% Iv1 I + lop, lvzl
+ los,Ayc, + loh,Axc,
LOH
traasducer case
Fastrak sensor
Perspex rod
. centre of transducer face
ROI points
Fig. 4. The Fast& receiver is attached to the ultrasound
transducer by means of a perspex bar. The receiver contains
three orthogonal copper coils that define the x, y and z axes
(LOS, LOH and LOP, respectively). In this arrangement,
four vectors (v, , v2, v, and v,) are summed to enable region
of interest (ROI) points to be transformed from image to
Fast& coordinates. Any other configuration of the vectors
could be used, but the error is likely to increase with the
number of vectors used.
The above equations are converted into matrix
form as,follows.
Let:
m, = loh,c,
ml0 = los,c,
mzo = f, + 10~ Iv11 + lop, Iv21
mm = lohyc,
ml, = los,c,
ml = fy + los, 1~11 + lop, IhI
mo2 = loh,c,
ml2 = los,c,
m22 = L + los, Iv11 + lop, lb1
Volume estimation from multiplanar 2D ultrasound images 0 S. W. HUGHES et al. 565
and
Pi = (AX, AY, 1).
Then
fi = pims
where:
f, = Fastrak coordinate of ith image point;
pi = coordinate of ith point relative to the centre of
the transducer face;
m, = transformation matrix for slice s.
A ruler was used to measure the distances of the
centre of the receiver above the image plane ( 1 v1 I) and
between the point in the image plane directly below the
receiver and the centre of the ultrasound transducer
face ( 1 vZ I) . The position and orientation of the receiver
does not matter so long as the lengths and directions
of the vectors are known. The position of the receiver
relative to the ultrasound transducer face can be de-
scribed by more than two vectors if necessary, but this
may increase the error in the volume estimate. This is
because each vector has a certain error in the position
of the start point and projection angle. The uncertainty
will increase with the number of vectors placed end
to end. For the receiver attachment shown in Fig. 3,
I v, 1 = 17.9 cm and I v2 1 = 2.8 cm. The centre of the
receiver was assumed to be where the manufacturer
claims it is.
The centre of the transducer face is marked on
one of the images and this point assumed to be at the
end of the LOS vector projecting to the centre of the
transducer face. (If the LOS vector is offset to one
side of the centre of the transducer face, then the equiv-
alent point must be marked on the image.) This point
becomes a new origin on the image and is essential
for calculating the 3D coordinate of an image point.
The x and y axis calibration factors are calculated using
scale markers on the ultrasound image. The x,y,z Fas-
trak coordinate of a point in the image is calculated
by multiplying the x,y image coordinates (relative to
the transducer origin) by the unit receiver vectors that
happen to be aligned with the x and y axes of the
image (in the example shown in Fig. 4, the LOH vector
for the x axis and the LOS vector for the y axis).
If the x axis of the image is antiparallel to the
positive direction of the corresponding receiver axis,
the object will be reflected about a line parallel to the
y axis that passes through the centre of the transducer
face. However, as all points retain their relative posi-
tion, the calculated volume will not be affected. If, for
some reason, the absolute positions of the ROI points
are required, the image x axis may have to be reversed
(most machines have a facility for doing this).
Volume calculations. Volume was estimated using
the ellipsoid, planimetry and tetrahedral methods, and
a new ray tracing method. These methods were chosen
to cover the types of algorithm that might be used to
calculate volume. The latter two methods require the
surface of the object to be represented as a triangular
mesh and the former two require just the basic ROI
points. The ellipsoid method is the most commonly
used method to estimate volume, especially for hearts
and prostate glands in which the volume of the organ
is assumed to be equal to that of a prolate ellipsoid of
the same length, height and width as the organ. The
main advantage of the ellipsoid technique is its sim-
plicity. The main disadvantage is that significant errors
that can result if an organ is not roughly ellipsoidal in
shape. The algorithm implemented on our system is a
simulation of the usual ellipsoid technique. The long
axis is taken as the distance between the centroids of
the first and last outlines and the product of the two
minor axes is calculated by dividing the largest outline
area by 2~.
Planimetry involves multiplying the area of each
ROI by the local slice thickness (Watanabe 1982).
The accuracy of this technique depends on image
planes being close together with only a slight differ-
ence in orientation between adjacent planes. If the sur-
face of the ROI is modelled by a triangular mesh,
the volume can be calculated be generating tetrahedra
using the triangle vertices and outline centroids (Cook
et al. 1980). We have developed a fourth ray tracing
technique that enables the volume of a triangulated
object of any shape to be calculated. A grid is con-
structed in the x,y plane equal in extent to the maxi-
mum x and y sizes of the triangulated object. Rays are
cast through the object from each grid node, and the
volume calculated by multiplying the distance between
intercepts on each side of the object by the area of
each grid element.
Balloons. Ten balloons (ranging in size from
13.6- 141.6 mL) were filled with water and the necks
tied off with surgical suture. Water filled balloons were
chosen for this experiment because, unlike organ phan-
toms, their volume can be accurately measured by
weighing (assuming a density of 1 g/mL for water).
The balloons were attached to a hollow perspex cylin-
der by means of a rubber band and placed in a tank
of tap water at 26C. The tank was placed on an exami-
nation couch (Fig. 1) in approximately the same posi-
tion as a patient undergoing an ultrasound scan. The
balloons were scanned using an Acuson 128XP/lO
with a ~-MHZ curvilinear probe. The transducer was
566 Ultrasound in Medicine and Biology Volume 22, Number 5. 1996
moved continuously across the balloons. The operator
was an experienced ultrasonographer who is currently
using the system in a clinical trial designed to assess
the benefits of ultrasonic volume measurements in fetal
medicine. The Fastrak transmitter was attached to a
purpose-built wooden stand (Fig. 1) and suspended
above and to the side of the tank. During scanning,
the transducer was oriented so that there was a clear
line of sight between the transmitter and receiver. The
receiver and transmitter were between 0.5 and 1 m
apart during scanning. Twenty images with a 324 x
224 matrix were acquired over a period of 10 s (two
images per second). The x,y dimensions of each pixel
was 0.353 and 0.376 mm, respectively. After scanning,
the balloons were emptied and weighed (Sartorius
MC 1, Sartorius AG, Gottingen, Germany ) to an accu-
racy of kO.01 g. The volume of the water in the bal-
loons was assumed to be the total weight of the balloon
minus the weight of the rubber and suture, divided by
the density of water.
of the difference in the speed of sound in tissue at
37C ( 1540 m/s) and in water at 26C ( 1495 m/s;
Bamber and Hill 1979). This discrepancy results in
overestimation of distance in the direction of sound
propagation by 2.92%; therefore, the calculated vol-
umes need to be reduced by a factor of 0.9708.
The mean percentage error was calculated by di-
viding the measured volume by the ( signed) difference
between the measured and calculated volumes. The F-
test was used to assess the significance of the differ-
ences between the variances and in cases where the
variances were not significantly different, one-way
analysis of variance was used to assess the significance
of differences between the means.
The image and data files were transferred to the
Titan computer via a local network and the edges of
the balloons (Fig. 5 ) outlined using a mouse and trans-
formed to Fastrak coordinates (Fig. 6). After transfor-
mation, a triangulation algorithm (Hughes and Brueton
1994) was used to tessellate the surface of each balloon
(Fig. 7 ) . Prior to tessellation and transformation, the
outline points are interpolated into a number of evenly
spaced points to improve triangulation. The surface is
displayed as a sequence of alternating light and dark
triangular facets and can be rotated about the x,y,z axes
in the display to check that triangulation has proceeded
correctly. The volume of each balloon was estimated
using the four algorithms described above.
The volumes were corrected to take into account
Kidneys. Ten cadaveric pigs kidneys (obtained
from a local supermarket), ranging in volume from
147-200 mL, were placed in turn on a perspex plinth
in a 26-L perspex tank filled with normal saline (0.9%
NaCl solution), and scanned using an Acuson 128XP/
3. The transducer was placed in a derrick placed at
right angles to the long axis of the tank, which enabled
the transducer to be set at various angles. The kidneys
were scanned with radial, parallel and slanted scans to
simulate how an organ might be scanned in the clinic.
The transducer was positioned by hand, but was sta-
tionary during each image acquisition. Between 15 and
20 images were captured of each kidney, and the im-
ages were analysed in the same way as the balloons.
Immediately after scanning, each kidney was placed
in a 2000-mL graduated cylinder to measure the vol-
ume of water displaced. The accuracy of the water
displacement technique was assessed by measuring the
volume of five accurately machine perspex cylinders
ranging in volume from 30-260 mL. (The experiment
Fig. 5. Ultrasound image through one of the water filled balloons scanned in a plastic bowl full of tap water. The
middle of the balloon wall was outlined on successive images.
Fig. 6.
Volume estimation from multiplanar 2D ultrasound images 0 S. W. HUGHES et nl. 567
A balloon outline transformed using the position and orientation data obtained from the Fast&.
was carried out without the observers knowing the
volume of the cylinders.) The velocity of sound was
assumed to be 1540 m/s within the kidneys. Errors in
the path lengths of the A scan lines caused by differ-
ences between the velocities of sound in water and
tissue were ignored.
Fetal livers. Sixteen cadaveric fetal livers (8-
37.5 mL), fixed in formaldehyde, were scanned in
a tank of distilled water. The same scanner, scan
techniques and volume calculation methods were
used as for the kidneys. The actual volume of the
kidneys was assessed by placing the livers in a 500-
mL graduated cylinder and noting the rise in water
level. The accuracy of this method was assessed by
measuring the volume of seven perspex blocks ( 3-
71 mL).
Scanner test
The Acuson scanner was tested using the Cardiff
resolution test object (Gammex-RMI Ltd, Nottingham,
UK), which contains parallel wires of known separa-
tion embedded in tissue equivalent gel. The tests in-
volve measuring distances between wires and assessing
the minimum wire separation that can be resolved. The
range was set to 140 mm, with a medium depth focus.
The mean vertical large scale linear calliper accuracy
was 0.16 & 0.1 mm and the mean horizontal large
scale linear calliper accuracy 0.6 2 1.64 mm. The axial
Fig. 7. Transformed ROI points are connected to form a series of triangles. Alternate dark/light shading makes
it easier for an observer to check that the triangulation algorithm has been performed correctly.
568 Ultrasound in Medicine and Biology
LOS
Volume 22, Number 5, 1996
d = 2r sin(W2) = 2.61 cm
If 1 ,m and n designate x,y and z
direction cosines, the angle
between vl and v2 may be calculated
from cos 8 = l,l, + m,m, + n,n2
centre of wheel
Fig. 8. A perspex wheel was constructed to test the accuracy of the Fastrak system. The receiver was attached to
the wheel as shown. The wheel was moved in 15 increments and the angle and distance moved were calculated.
resolution was <l mm, and the horizontal resolution
was between 1.25 and 2.5 mm.
Fastrak accuracy
The accuracy of the Fastrak system was assessed
by attaching the Fastrak receiver to a perspex wheel
23 cm in diameter and 1 cm thick. It is very tedious
to fully assess the accuracy of a device that has six
degrees of freedom, however, a wheel is a convenient
way to combine the measurement of position and
angle. The receiver was fixed onto the wheel by
means of polythene screws so that the electrical centre
of the receiver (as specified in the manual) was 10
cm (20.01 cm) from the centre of the wheel. The
receiver was oriented so that the LOS vector pointed
to the centre of the wheel. The wheel was fixed to a
base and could be rotated 360 about the vertical and
horizontal axes. The whole assembly was fixed to a
board (using reusable plastic adhesive), which was
then placed on the treatment couch. The centre of the
wheel was about 30 cm above the top surface of the
couch. (With receiver attached to the ultrasound
transducer as shown in Fig. 3, the receiver is unlikely
to go lower than 30 cm above the surface of the couch
when a patient is being scanned.) The centre of the
wheel was positioned at a distance of about 50 cm
from the centre of the transmitter, with the plane of
the wheel oriented at approximately 45 to the x and
y axes of the Fastrak transmitter. The transmitter was
positioned next to the couch as shown in Fig. 1, and
was above the top of the wheel. (The transmitter is
always placed slightly above the scan region to ensure
a clear path to the receiver.) The wheel was moved
in 15 increments and the position and orientation
quartemions were recorded by a notebook PC
attached to the Fastrak SEU via the serial link. One
hundred data samples were acquired over 10 s to as-
sess the overall noise level with the ultrasound ma-
chine switched on and off.
The position and orientation data were stored in
ASCII and transferred to a spreadsheet program (Mi-
crosoft Excel). The quartemions were used to calcu-
lated the direction cosines of the LOS, LOH and LOP
vectors as described above. Sector angles were calcu-
lated by taking the arcosine of the sum of the product
of the x,y and z direction cosines (Stroud 1984). As
the wheel is rotated in 15 increments the LOS and
LOH vectors should change by 15 and the LOP vector
by 0 and the position of centre of the receiver should
change by 2.61 cm (Fig. 8). This represents the length
of the chord across the ends of a 15 sector of a circle
of 10 cm in radius. The angle could be set to within half
of the 0.25~mm thick 15 marks around the perimeter
corresponding to an error of 0.11.
Volume estimation from multiplanar 2D ultrasound images l S. W. HUGHES et al.
569
RESULTS
Balloons
Figure 9(a) shows a plot of the measured volume
vs. that calculated by the four methods described
above. It is apparent that the ellipsoid method has more
scatter than the other three methods. Figure 9(b)
shows that the 95% range for the ellipsoid method is
much greater than for the other three methods. There
is little difference in the 95% limits of agreement for
the other three methods. The error bars indicate
the mean +2 standard deviations of the differences
between the measured and calculated volumes for the
four methods (Bland and Altman 1986). Analysis of
variance showed no significant difference (p = 0.49)
between the planimetry, tetrahedral and ray tracing
methods. However, there was a significant difference
between the ellipsoid technique and the other three
techniques (p = 0.018).
Kidneys
For the ray tracing method, there was no signifi-
cant differences (p > 0.4) between the variances of the
three scan techniques. However, there was a significant
difference (p = 0.02) between the mean volumes pro-
duced by the radial, parallel and slanted scan tech-
niques. For radial scanning, there was no significant
difference between the mean volumes produced by the
four volume estimation methods (p = 0.56)) however,
there was a highly significant difference between the
variances of the ellipsoid and the other three methods
(p < 0.001). The mean percentage error for the ray
tracing method using the radial scan technique was
2.7 k 2.3%. The accuracy and precision of the water
displacement technique was -0.93 2 1.82%.
Fetal livers
As for the kidneys, for ray tracing there was no
significant difference in the variance between the three
different scanning techniques (p > 0.36) although
there was a significant difference between the means
(p < 0.001). For the radial scanning technique there
was no significant difference between the mean and
variance of the planimetry, tetrahedral and ray tracing
volume estimation methods; however, there was a sig-
nificant difference (p < 0.04) between variance of
these three methods and the ellipsoid method. The
mean percentage error for the radial scanning tech-
nique and ray tracing volume calculation method was
6.6 2 5.4%. The accuracy and precision of the water
displacement technique was 7.8 2 9.8%.
Balloons, kidneys and livers grouped together
Figure 9(a) shows a plot of measured volume
versus calculated volume for the balloons, kidneys and
fetal livers. Figure 10(b) shows a Bland-Altman plot
showing the variance of the absolute error about the
mean error. An interesting point to note is that although
the percentage error decreases with volume, or at least
in the order liver, balloons and kidneys, the absolute
error in terms of milliliters increases. Table 1 summa-
0 20 40 60 60 100 120 140 160
Measured volume (ml)
a
10
o
i
00
0
8 . , .bQ * _ , . . . . . . 1. . . O. . . . Q g;
t
-10 -20 ; 1,
0 20 40 60 80 100 120 140 160 180
Average of measured and calculated volume (ml)
b
Fig. 9. (a) Plot of measured balloon volume verses the volume calculated by the ellipsoid (el), planimetry ( pla),
tetrahedral (tet) and ray (ray) tracing methods. The line of identity is shown. (b) Bland-Altman plot of the
difference between the calculated volumes and tire actual volume against the average of the two. The 95% range
bars are designated by the first letter of the method that they refer to. The middle of each bar represents the mean
difference and the two outer bars plus or minus two standard deviations.
Ultrasound in Medicine and Biology Volume 22, Number 5, 1996
25C
s
E
200
E
_3
P 150
8
l-l
P
100
t
F!
0 50 100 150 200 250
Measured volume (ml)
a
-10 i +
0 50 100 150 200 250
Average of the measured and calculated volumes (ml)
b
Fig. 10. (a) Plot of calculated versus measured volume for the balloons, kidneys and fetal livers. The ray tracing
technique was used to calculate all volumes. The balloons were scanned free-hand and the kidneys and livers
scanned with radial technique with the transducer held in a rig. The line of identity is shown. (b) Bland-Altman
plot as described for Fig. 9. The 95% range bars error bars are designated by the first letter of the scanned object.
rises the results for each group and for all groups taken
as a whole. There appears to be a correlation (Y =
0.99, p = 0.008) between the mean balloon, kidney
and liver volumes and the standard deviations of the
absolute errors. Table 2 shows the results for ray trac-
ing volumes for kidneys and livers for the three scan-
ning techniques. Note that the for some reason the
slanted scans underestimate volume.
Fastrak accuracy
Over a complete rotation of 360, the means and
standard deviations of the LOS, LOH and LOP vectors
were 15.03 + 0.7, 15.04 t 0.7 and 1.09 + 0.7,
respectively, and the mean chord length was 2.715 ?
0.22 cm. In reality the transducer would probably not
be moved more than ?30 from the vertical. For a 60
excursion over 10.4 cm, the angle was measured as
15.18 5 0.06 ( 1.2 + 0.4% ) and the chord length 2.609
+ 0.019 cm (0.05 + 0.73%). Over a distance of 10
cm, a 0.18 error in measuring angle would result in
Table 1. The mean and standard deviation of the
percentage error, for the ellipsoid, planimetry,
tetrahedral and ray tracing methods for the balloons,
kidneys and livers.
Ellipsoid Planimetry Tetrahedral Ray trace
Balloons 13.4 t 20.9 2.1 * 2.1 0.9 2 1.9 0.9 2 2.4
Kidneys 5.3 10.6 5.9 t 2.1 4.3 f 2.2 2.7 ir 2.3
Livers 2.9 ?I 8.7 6.5 k 5.2 1.3 + 5.2 5.2 2 4.7
The kidneys and livers were scanned radially (therefore all the
scans used to produce data for this table were multiplanar).
a position error of 0.3 mm. To assess the noise level,
the standard deviation of the x,y and z coordinates and
LOS, LOH and LOP vectors were calculated. The
mean standard deviation of the x,y and z coordinates
was 0.012 mm, and the mean angular standard devia-
tion 0.028, which over a distance of 10 cm will result
in a position error of 0.05 mm.
DISCUSSION
The results show that the system has the potential
to provide accurate estimates of organ volume using a
variety of volume calculation algorithms. Our results
are comparable to those obtained by other workers on
balloon phantoms (Brinkley et al. 1978; Eaton et al.
1979; Geirsson et al. 1982; Hastak et al. 1982; Hodges
et al. 1994).
In general, there was not much to choose between
the planimetry, tetrahedral and ray tracing methods of
estimating volume, which were much superior to the
ellipsoid method. The radial, parallel and slanted scan
methods produced results with similar variance, but
with significantly different means. More work needs
Table 2. The mean and standard deviations of the
percentage error for the kidney and liver ray trace volumes
for the three scan techniques.
Kidneys
Livers
Radial
2.7 2 2.3
6.6 F 5.4
Parallel
2.1 z 2.7
4.6 2 5.5
Slanted
-0.9 2 2.8
-2.8 lr 6.8
Volume estimation from multiplanar 2D ultrasound images 0 S. W. HUGHES et al. 571
to be done to assess the importance of these differences
and to see whether they can be reduced.
A number of factors influence the overall error in
the result, for instance the size and quality of the im-
ages, the scanning technique (e.g., orientation and
number of slices), errors in the Fastrak data, and errors
in the volume algorithms. Interference from metal is
a problem with electromagnetic systems; however, our
results show that for small excursions of the receiver
the accuracy is adequate even in the presence metal
(for instance in the examination couch). The accuracy
of the Fastrak is similar to that quoted by the manufac-
turer over the kind of excursions used for scanning an
organ. Errors in measuring relative position and angle
affect the error in measuring volume, but not errors
in absolute position. The percentage error seems to
decrease with volume while the limits of agreement
appear to increase. Clinically, in some cases the per-
centage error is likely to be of most interest, but in
other cases, e.g., cardiology, the actual difference will
be important (as this will have a direct bearing on the
precision of estimating stroke volume and, therefore,
cardiac output). As in other imaging modalities, the
critical factor influencing the error is likely to be the
accuracy of delineating in uivo ROIs. This will depend
on the quality of the machine used and the ability of
the ultrasonographer.
Further work needs to be done on assessing: inter-
and intraobserver ROI tracing errors; the accuracy re-
quired in positioning the Fastrak receiver relative to the
ultrasound transducer ; and environmental influences on
the Fastrak. Tissue inhomogeneities in the path of the
ultrasound beam are likely to cause geometric distortions
due to refraction and time-of-fight errors.
In recent years, dedicated 3D ultrasound scanners
have been developed. These systems have various ad-
vantages over add on systems, such as the one de-
scribed in this article. For instance, dedicated 3D sys-
tems are less cumbersome to use. They are excellent
for small objects, but cannot be used over extended
distances as is required for vascular imaging. There-
fore, 2D systems with an added 3D capability are likely
to complement dedicated 3D systems.
Currently, the vast majority of scanners are 2D,
and this is likely to remain the case for several years
to come. The system that we describe also has the
advantage of being relatively cheap (the Polhemus de-
vice costs just under &5000 and the video card &300),
can be connected to any scanner, and is easily trans-
portable enabling sharing between scanners. Another
advantage of external localisation systems is the ability
to scan an organ from different directions and to com-
bine the images.
The software to outline and transform ROIs and
to calculate volume has now been implemented on a
PC. So far the system has been used to scan fetal livers
and lungs, adult prostate glands and neonate brain ven-
tricles. We believe that these results are encouraging
and demonstrate that volume estimates within 10% are
obtainable in the clinic.
Acknowledgements-The authors would like to thank Terry Clark
for scanning the balloons. Roy Reed of the Medical Physics Work-
shop for crafting the transducer attachment, Chris Bunton of the
Medical Physics Workshop for making the wheel, Agnes Aning-
amoah for handling the organs, George Gore of the Carpentry De-
partment for making the transmitter stand, Sue Chin and Julie Simp-
son of the Public Health Department for advice on the statistical
analysis, Acuson for the lone of the 128XP/3 and Tommys Cam-
paign and BT for funding this work.
REFERENCES
Austin JHM, Gooding CA. Roentgenographic measurement of skull
size in children. Radiology 197 1;99:641-646.
Bamber JC, Hill CR. Ultrasonic attenuation and propagation speed
in mammalian tissues as a function of temperature. Ultrasound
Med Biol 1979;5:149-157.
Bland JM, Altman DG. Statistical methods for assessing agreement
between two methods of clinical measurement. Lancet
1986;1:307-310.
Blankenhorn DH, Chin HP, Strikwerda S, Bamberger J, Hestenes
JD. Common carotid artery contours reconstructed in three di-
mensions from parallel ultrasonic images. Radiology 1983:
148533-537.
Brinkley JF, Moritz WE, Baker DW. Ultrasonic three-dimensional
imaging and volume from a series of arbitrary sector scans.
Ultrasound Med Biol 1978;4:317-327.
Cook LT, Cook PN, Lee KR. Batnitzky S, Wong BYS. An algorithm
for volume estimation based on polyhedral approximation. IEEE
Trans Biomed Eng BME 1980;27:493-500.
Cooke JM, Zyda MJ, Pratt DR. McGhee RB. NPSNET: Flight simu-
lation dynamic modelling using quartemions. Presence 1992;
1:404-420.
Dodge HT, Sandler H, Ballew DW, Lord JD. The use of biplane
angiocardiography for the measurement of left ventricular vol-
ume in man. Am Heart J 1960;60:762-776.
Eaton LW, Maughan WL, Shoukas AA, Weiss JL. Accurate volume
determination in the isolated ejecting canine left ventricle by
two-dimensional echocardiography. Circulation 1979; 60:320-
326.
Ennis BM, Zientek DM, Ruggie NT, Billhardt RA, Klein LW. Char-
acterization of a saphenous vein graft aneurysm by intravascular
ultrasound and computerized three-dimensional reconstruction.
Cathet Cardiovasc Diagn 1993;28:328-33 I.
Fine D. Perring S, Herbetko J, Hacking CN, Fleming JS. Three-
dimensional imaging of the gallbladder and dilated biliary tree:
Reconstruction from real-time B-scans. Br J Radio1 1991:
64: 1056- 1057.
Gardener JE, Lees WR, Gillams A. Volume imaging with US. Radi-
ology 1991;18l(P):l33.
Geirsson RT, Christie AD, Pate1 N. Ultrasound volume measure-
ments comparing a prolate ellipsoid method with a parallel plani-
metric area method against a known volume. J Clin Ultrasound
1982; 10:329-332.
Ghosh A, Nanda NC. Maurer G. Three-dimensional reconstruction
of echocardiographic images using the rotation method. Ultra-
sound Med Biol 1982;8:655-661.
Gohari P. Berkowitz RL, Hobbins JC. Predication of intrauterine
growth retardation by determination of total intrauterine volume.
Am J Obstet Gynecol 1977; 127:255-260.
Hastak SM, Gammelgaard J, Holm HH. Transrectal ultrasonic vol-
ume determination of the prostate-a preoperative and postoper-
ative study. J Urol 1982; 127:l 115-I 118.
571 Ultrasound in Medicine and Biology Volume 22, Number 5, 1996
Hell B, Walter FA, Schreiber S, Blase H, Bielke G. Three-dimen-
sional ultrasonography in maxillofacial surgery. A new diagnos-
tic tool. Int J Oral Maxillofac Surg 1993;22:173-177.
Hodges TC, Detmer PR, Bums DH, Beach KW, Strandness DE Jr.
Ultrasonic three-dimensional reconstruction: In vitro and in viva
volume and area measurement. Ultrasound Med Biol 1994:
20:7 199729.
Hughes SW, Brueton RN. A technique for measuring the surface
area of articular cartilage in acetabular fractures. Br J Radio1
1994;67:584-588.
Kelly IMG, Gardener JE, Lees WR. S-dimensional fetal ultrasound.
Lancet 1992;339:1062-1064.
King DL, King DL Jr, YiCi Shao M. Three-dimensional spatial
registration and interactive display of position and orientation of
real-time ultrasound images. J Ultrasound Med 1990;9:525-532.
Kirschener-Hermanns R, Klein HM, Muller U, Schafer W, Jakse G.
Intraurethral ultrasound in women with stress incontinence. Br
J Ural 1994;74:315-318.
Klein H, Marqaurt M, Polz H, Schuller G. 3D reconstruction of fetal
images based on ultrasound. In: computer assisted radiology.
Lemke HU, Inamura K, Jaffe CC, Felix R, ed. Berlin: Proceed-
ings of the International Symposium, 1993534-538.
Kok-Hwee Ng. Evans JL, Vonesh MJ, Meyers SN. Mills TA. Arte-
rial imaging with a new forward-viewing intravascular ultrasound
catheter, II. Three-dimensional reconstruction and display of
data. Circulation 1994; 89:718-723.
Lees WR, Chong WK, Lawrence R, Gardener J. Intravascular ultra-
sound with 3D reconstruction: A new way to image vascular
disease. Br J Radio1 1991a;64:655.
Lees WR, Gardener JE, Brett AD, Davey MK. Assessment of 3D
US image acquisition. Radiology 1993; 189( P):341.
Lees WR, Gardener JE, Gillams A. Three-dimensional US of the
fetus. Radiology 1991b; 181 (P):132.
Levine RA, Handschumacher MD, Sanfilippo AJ, Hagege AA, Har-
rigan P. Three-dimensional echocardiographic reconstruction of
the mitral valve, with implications for the diagnosis of mitral
valve prolapse. Circulation 1989; 80:589-598.
Levine SC, Filly RA, Creasy RK. Identification of fetal growth
retardation by ultrasonic estimation of total intrauterine volume.
.I Clin Ultrasound 1979;7:21-26.
Matsumoto M, Inoue M, Tamura S, Tanaka K, Abe H. Three-dimen-
sional echocardiography for spatial visualisation and volume cal-
culation of cardiac structures. J Clin Ultrasound 1981;9: 157-
165.
McLachlan MSF, Williams ED, Fortt RW, Doyle FH. Estimation
of pituitary gland dimensions from radiographs of the sella tur--
cica. Br J Radio1 1968;41:323-330.
Moritz WE, Pearlman AS, MC Cabe DH. et al. An ultrasonic tech-
nique for imaging the ventricle in three dimensions and calculat-
ing its volume. IEEE Trans Biomed Eng BME 1983:30:48X
492.
Picot PA. Rickey DW, Mitchell R. Rankin RN. Fenster A. Three-
dimensional Doppler imaging. Ultrasound Med Biol 1993:
19:95-104.
Pini R, Monnini E, Masotti L, Greppi B, Gerofolini M. Echocardio-
graphic computed tomography-of the heart: Preliminary results.
J Am Co11 Cardiol 1989:49:896.
Pretorius DH, Nelson TR, Jaffe JS. 3-dimensional sonographic anal-
ysis based on color flow Doppler and gray scale image data: a
preliminary report. J Ultrasound Med 1992; 11:225-232.
Raichlen JS, Trivedi SS, Herman GT, St. John Sutton MG, Reichek
N. Dynamic three-dimensional reconstruction of the left ventricle
from two-dimensional echocardiograms. J Am Co11 Cardiol
1986;8:364-370.
Rosenfield K, Kauffman J, Pieczek AM, Langevin RE, Palefski PE.
Human coronary and peripheral arteries: On-line three-dimen-
sional reconstruction from two-dimensional intravascular US
scans. Radiology 1992; 184:823-832.
Rosenfield K, Los&do DW, Ramaswamy K, Pastore JO, Langevin
RE. Three-dimensional reconstruction of human coronary and
peripheral arteries from images recorded during two-dimensional
intravascular ultrasound examination. Circulation 1991: 84:
1938-1956.
Sawada H, Fujii J, Kato K, Onoe M, Kuno Y. Three dimensional
reconstruction of the left ventricle from multiple cross sectional
echocardiograms. Value for measuring left ventricular volume.
Br Heart J 1983; 50:438-442.
Sehgal CM, Broderick GA, Gomiak RJ, Arger PH. Three-dimen-
sional imaging of prostates with transrectal sonography. Radiol-
ogy 1993; 189(P):342.
Stroud KA. Engineering mathematics. London: Macmillan, 1984.
Teicholz LE, Cohen MV, Sonnenblick EH, Gorlin R. Study of left
ventricular geometry and function by B-scan ultrasonography in
patients with and without asynergy. N Engl J Med 1974;
291:1220-1226.
Watanabe Y. A method for volume estimation by using vector areas
and centroids of serial cross-sections. IEEE Trans Biomed Eng
BME 1982;29:202-205.
Wollschlager H, Zeiher AM, Klein H, Kasper W, Wollschlager S.
Transesophageal echo computer tomography: A new method for
dynamic 3-D imaging of the heart. J Am Co11 Cardiol 1989;
13:68A.
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Standfor Refrence 3Document6 pagesStandfor Refrence 3Harshoi KrishannaPas encore d'évaluation
- Benefits, Harms, and Cost-Effectiveness of Supplemental Ultrasonography Screening For Women With Dense BreastsDocument15 pagesBenefits, Harms, and Cost-Effectiveness of Supplemental Ultrasonography Screening For Women With Dense BreastsHarshoi KrishannaPas encore d'évaluation
- Nonrandomized Intervention Study of Naloxone Coprescription For Primary Care Patients Receiving Long-Term Opioid Therapy For PainDocument24 pagesNonrandomized Intervention Study of Naloxone Coprescription For Primary Care Patients Receiving Long-Term Opioid Therapy For PainHarshoi KrishannaPas encore d'évaluation
- Effectiveness of An Internet-Delivered Exercise and Pain-Coping Skills Training Intervention For Persons With Chronic Knee PainDocument19 pagesEffectiveness of An Internet-Delivered Exercise and Pain-Coping Skills Training Intervention For Persons With Chronic Knee PainHarshoi KrishannaPas encore d'évaluation
- Original Research: Epidural Steroids, Etanercept, or Saline in Subacute SciaticaDocument10 pagesOriginal Research: Epidural Steroids, Etanercept, or Saline in Subacute SciaticaHarshoi KrishannaPas encore d'évaluation
- Walking Through The Resume: Personal DetailsDocument3 pagesWalking Through The Resume: Personal DetailsHarshoi KrishannaPas encore d'évaluation
- Original Research: A Comparison of The Effects of 2 Types of Massage and Usual Care On Chronic Low Back PainDocument12 pagesOriginal Research: A Comparison of The Effects of 2 Types of Massage and Usual Care On Chronic Low Back PainHarshoi KrishannaPas encore d'évaluation
- A Review of The Evidence For TDocument9 pagesA Review of The Evidence For THarshoi KrishannaPas encore d'évaluation
- Differences in Pain Perception in Children Reporting Joint andDocument8 pagesDifferences in Pain Perception in Children Reporting Joint andHarshoi KrishannaPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 16 Personalities ResultsDocument9 pages16 Personalities Resultsapi-605848036Pas encore d'évaluation
- Case No. Class Action Complaint Jury Trial DemandedDocument43 pagesCase No. Class Action Complaint Jury Trial DemandedPolygondotcom50% (2)
- Mobile Services: Your Account Summary This Month'S ChargesDocument3 pagesMobile Services: Your Account Summary This Month'S Chargeskumarvaibhav301745Pas encore d'évaluation
- Bulletin PDFDocument2 pagesBulletin PDFEric LitkePas encore d'évaluation
- BSDDocument26 pagesBSDEunnicePanaliganPas encore d'évaluation
- GA Power Capsule For SBI Clerk Mains 2024 (Part-2)Document82 pagesGA Power Capsule For SBI Clerk Mains 2024 (Part-2)aa1904bbPas encore d'évaluation
- Controlled DemolitionDocument3 pagesControlled DemolitionJim FrancoPas encore d'évaluation
- Weg CFW500 Enc PDFDocument32 pagesWeg CFW500 Enc PDFFabio Pedroso de Morais100% (1)
- BA 4722 Marketing Strategy SyllabusDocument6 pagesBA 4722 Marketing Strategy SyllabusSri GunawanPas encore d'évaluation
- Sanskrit Lessons: �丘��恆� � by Bhikshuni Heng HsienDocument4 pagesSanskrit Lessons: �丘��恆� � by Bhikshuni Heng HsiendysphunctionalPas encore d'évaluation
- Introduction To AmplifierDocument8 pagesIntroduction To AmplifierElaine BicolPas encore d'évaluation
- Slides - SARSDocument191 pagesSlides - SARSCedric PoolPas encore d'évaluation
- Wins Salvacion Es 2021Document16 pagesWins Salvacion Es 2021MURILLO, FRANK JOMARI C.Pas encore d'évaluation
- Percentage and Profit & Loss: Aptitude AdvancedDocument8 pagesPercentage and Profit & Loss: Aptitude AdvancedshreyaPas encore d'évaluation
- Personal Narrative RevisedDocument3 pagesPersonal Narrative Revisedapi-549224109Pas encore d'évaluation
- Rab Sikda Optima 2016Document20 pagesRab Sikda Optima 2016Julius Chatry UniwalyPas encore d'évaluation
- JBF Winter2010-CPFR IssueDocument52 pagesJBF Winter2010-CPFR IssueakashkrsnaPas encore d'évaluation
- Assessing The Marks and Spencers Retail ChainDocument10 pagesAssessing The Marks and Spencers Retail ChainHND Assignment Help100% (1)
- Junos ErrorsDocument2 pagesJunos ErrorsrashidsharafatPas encore d'évaluation
- Heart Rate Variability Threshold As An Alternative.25Document6 pagesHeart Rate Variability Threshold As An Alternative.25Wasly SilvaPas encore d'évaluation
- DLI Watchman®: Vibration Screening Tool BenefitsDocument2 pagesDLI Watchman®: Vibration Screening Tool Benefitssinner86Pas encore d'évaluation
- Anviz T5 RFID ManualDocument52 pagesAnviz T5 RFID ManualLuis Felipe Olaya SandovalPas encore d'évaluation
- ProbDocument10 pagesProbKashif JawaidPas encore d'évaluation
- Key Performance Indicators - KPIsDocument6 pagesKey Performance Indicators - KPIsRamesh Kumar ManickamPas encore d'évaluation
- Mindray PM 9000 User ID10240 PDFDocument378 pagesMindray PM 9000 User ID10240 PDFJuan FernandoPas encore d'évaluation
- List of Olympic MascotsDocument10 pagesList of Olympic MascotsmukmukkumPas encore d'évaluation
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Document19 pagesEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uPas encore d'évaluation
- 2432 - Test Solutions - Tsol - 2432 - 21702Document5 pages2432 - Test Solutions - Tsol - 2432 - 21702Anmol PanchalPas encore d'évaluation
- Durability of Prestressed Concrete StructuresDocument12 pagesDurability of Prestressed Concrete StructuresMadura JobsPas encore d'évaluation
- MPT EnglishDocument5 pagesMPT Englishkhadijaamir435Pas encore d'évaluation