Académique Documents
Professionnel Documents
Culture Documents
Feasibility Study of Stroke Surveillance: Data From Bangalore, India
Transféré par
Angad Singh0 évaluation0% ont trouvé ce document utile (0 vote)
9 vues8 pagesGlobally, stroke is a leading cause of death and disability. This study aimed to develop a feasible stroke surveillance program in Bangalore, India using the WHO STEPS methodology. The study collected data on 1,174 stroke patients admitted to 3 major hospitals over 6 months, following them until discharge and 28 days to measure outcomes like death and disability. Nearly half had at least one risk factor. One third were dependent at discharge and follow up. Analysis of death records identified 6% of total deaths in Bangalore as due to stroke, with over 50% occurring in major hospitals. The study demonstrated the feasibility of institutional-based stroke surveillance supplemented with periodic population-based data to provide comprehensive information for prevention and control programs.
Description originale:
hospital surveillance stroke
Titre original
1007
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentGlobally, stroke is a leading cause of death and disability. This study aimed to develop a feasible stroke surveillance program in Bangalore, India using the WHO STEPS methodology. The study collected data on 1,174 stroke patients admitted to 3 major hospitals over 6 months, following them until discharge and 28 days to measure outcomes like death and disability. Nearly half had at least one risk factor. One third were dependent at discharge and follow up. Analysis of death records identified 6% of total deaths in Bangalore as due to stroke, with over 50% occurring in major hospitals. The study demonstrated the feasibility of institutional-based stroke surveillance supplemented with periodic population-based data to provide comprehensive information for prevention and control programs.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
9 vues8 pagesFeasibility Study of Stroke Surveillance: Data From Bangalore, India
Transféré par
Angad SinghGlobally, stroke is a leading cause of death and disability. This study aimed to develop a feasible stroke surveillance program in Bangalore, India using the WHO STEPS methodology. The study collected data on 1,174 stroke patients admitted to 3 major hospitals over 6 months, following them until discharge and 28 days to measure outcomes like death and disability. Nearly half had at least one risk factor. One third were dependent at discharge and follow up. Analysis of death records identified 6% of total deaths in Bangalore as due to stroke, with over 50% occurring in major hospitals. The study demonstrated the feasibility of institutional-based stroke surveillance supplemented with periodic population-based data to provide comprehensive information for prevention and control programs.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 8
Globally, stroke is the third commonest cause of
mortality
1
and the fourth leading cause of disease burden
2
.
In 2005, stroke accounted for nearly 5.7 million deaths
Feasibility study of stroke surveillance: Data from Bangalore, India
D. Nagaraja
*
, G. Gururaj
**
, N. Girish
**
, Samhita Panda
*
, A.K. Roy, G.R.K. Sarma
& R. Srinivasa
*
Departments of
*
Neurology &
**
Epidemiology, National Institute of Mental Health & Neuro Sciences
Department of Neurology, St. Johns Medical College & Hospital &
*
Department of Neurology
M.S. Ramaiah Medical College & Hospital, Bangalore, India
Received June 10, 2008
Background & objectives: Stroke is a leading cause of deaths, and disabilities in India. Reliable and good
quality data on epidemiological characteristics of stroke are essential to plan, implement and evaluate
stroke prevention and control programmes. A feasibility study was undertaken in Bangalore to examine
the possibility of establishing stroke surveillance and to develop methodology for a larger programme.
Methods: The study adapted WHO STEPs-STROKE methodology to collect data on hospitalized stroke
events and fatal stroke events in the city of Bangalore. In STEP I, Information was collected from 1,174
stroke patients in three large hospitals and were followed till discharge and 28 days; outcome was measured
as death or disability. Stroke cases fulflling diagnostic criteria, evaluated by neurologists and CT/MRI
confrmed cases were included. Brief information on major risk factors was collected from all stroke
patients / family members and from medical records by trained research offcers. In STEP II, death records
of Bangalore Mahanagara Palike for 2004 (n=23,312) were analyzed to identify stroke related deaths.
Results: Using WHO-STEPs approach, a methodology was developed for stroke surveillance in a
geographically defned population. By STEP 1 method - 7 per cent of medical and 45 per cent of
neurological admissions were due to stroke with a fatality rate of 9 per cent at hospital discharge and 20
per cent at 28 days. With a mean age of 54.5 ( 17.0) yr and male preponderance, nearly half had one or
more risk factors. Weakness or paresis (92%) was the commonest presentation and ischaemic stroke was
most frequent (73.8%). One third of total stroke patients were dependent at both discharge and 28 day
follow up. By STEP II method the proportional mortality rate for Bangalore city was observed to be 6
per cent and more than 50 per cent of total stroke deaths had occurred in 10 major hospitals.
Interpretation & conclusions: The present study has shown that stroke surveillance is possible and feasible.
Institution based (hospitals and vital registry data) stroke surveillance supplemented with periodical
population based information can provide comprehensive information on vital aspects of stroke like
mortality, risk factors, disability and outcome. There is a need to develop stroke surveillance in a phased
manner along with mechanisms to apply data for prevention and control programmes.
Key words Chronic disease - developing countries - National Health Programme - stroke - stroke surveillance - WHO STEPS-Stroke
and 16 million cases of frst ever strokes worldwide
2
.
More than three fourths of these occur in low and middle
income countries (LMICs) of the world
3
. Countries
Indian J Med Res 130, October 2009, pp 396-403
396
with large populations (like India, China, Brazil and
Russia) contribute for greater numbers of deaths and
disability due to stroke
4-7
. In 2001, pooled estimates for
India showed that the prevalence of stroke was 203 per
100,000 population above 20 years (resulting in about
1 million cases) and contributing for 1.2 per cent of
the total deaths (approximately 102,000 deaths)
8
. The
Indian Council of Medical Research (ICMR) estimates
indicated that amongst the non communicable diseases
(NCDs), stroke contributes for 41 per cent of deaths and
72 per cent of disability adjusted life years (DALYS)
9
.
The ongoing socio-demographic and epidemiological
transition in India has a key infuence on the burden
of stroke and the problem is likely to increase in the
coming years. The socio-economic impact due to stroke
on individuals, families and health care institutions
is enormous. The economic loss due to heart disease,
stroke and diabetes between the years 2006 to 2015 is
estimated to be approximately 9 billion international
dollar loss of national income in India
5
.
Comprehensive information on stroke mortality,
morbidity, risk factors and disability are required for
planning and implementing programmes in prevention,
management and rehabilitation
3,10
. Previous studies on
stroke have documented the burden of stroke across the
country. Banerjee & Das reviewing the epidemiology of
stroke in India observe that the age adjusted prevalence
rates vary between 250 to 350 per 100,000 population
in different studies
11
. The incidence study from eastern
India has shown the adjusted annual incidence (per
100,000 persons) of stroke to be 124 in rural area
12
and 145 in urban area
13
. As stroke shares many risk
factors with other NCDs, studies on hypertension
14
also
point to the greater burden of stroke in India. Several
studies have elucidated the characteristics of stroke
(type, mortality rates, complication, risk factors, etc.)
and brought out the need for preventive measures in
India
15,16
. In addition, stroke registries in Hyderabad
17
,
Mumbai
7
, Chennai
18
, and Bangalore
19
have delineated
the treatment and rehabilitation components for better
management of stroke. However, these initiatives
have differed in methodology, been center specifc
and undertaken on different populations of varying
sizes, focused on individual components and have
not been continuous in nature (mostly one time
effort). Systematic, uniform and continuous data /
evidence can lead to stroke prevention, management
and rehabilitation programmes in India
20
. This type
of surveillance data will also help in monitoring and
evaluating the impact of ongoing and future initiatives
in this area.
Stroke surveillance provides inputs for planning
services, monitoring trends, assessing the burden of
problem, identifying changing profle and pattern of
risk factors, and to monitor and evaluate the impact
of intervention
21
. WHO has recommended STEPS
approach for stroke surveillance and has examined
feasibility of implementation in LMICs, including
India
7,16,22,23
to assess the magnitude and profle of
stroke, design appropriate interventions and monitor
their effectiveness
21
.
The present study examines the feasibility of
developing a stroke surveillance programme, develop
methodology and examine various issues of a larger
programme in the Indian context. The specifc
objectives were to develop a strategy for establishment
of a population based stroke surveillance system,
implement the same and delineate mechanisms for a
feasible system in a wider geographic area. The study
thus explored the possibility of collecting uniform data
on burden and other salient characteristics of stroke like
mortality, morbidity, socio-demographic correlates,
risk factors, patterns and disability.
Material & Methods
WHO STEPS stroke surveillance aims at
collecting information on stroke events by a uniform
and standardized method in hospital and community
settings. Information is collected on both fatal and non
fatal events and also hospitalized and non hospitalized
events in different phases or steps (referred to as
Step 1, Step 2 and Step 3). Step 1 aims at collecting
information on stroke patients admitted to hospitals,
Step 2 identifes fatal stroke events in the community
and step 3 estimates community based non fatal stroke
events
21
. Pooling of data from all 3 steps can provide
complete and total information on both public health
and clinical aspects of stroke, thus, helping to develop
integrated programmes. Experience of several centres
is vital to develop a larger uniform approach for the
country to develop uniformity in procedures and
practices
16, 23
. Due to resource constraints, the present
study attempted implementation of steps 1 and 2 only.
The Institutional Ethical Committee at National Institute
of Mental Health and Neurosciences (NIMHANS),
Bangalore, approved the study protocol.
Stroke events in hospitals (STEP 1): Three major
referral treatment centres for stroke were selected from
amongst the hospitals in Bangalore: NIMHANS, an
apex public sector institution for neurological services;
St. Johns Medical College Hospital (SJMCH) and M.S.
NAGARAJA et al: BANGALORE STROKE SURVEILLANCE 397
availability of services round the clock, presence of
medical and neurological services, good recording
systems and willingness to participate, the 3 hospitals
were chosen for the feasibility study.
Data collection was undertaken during the 6 month
period of March 1 to August 31, 2005. The defnitions
as recommended in the STEPS stroke manual were
followed (Appendix). All 3 hospitals followed uniform
methods in data capture procedures. The data capture
forms were translated, pre-tested and validated in the
local vernacular language (Kannada) for feld use prior
to beginning of the study. The focus of information
gathering was on socio-demographic characteristics,
past history, risk factors, details pertaining to the
acute stroke event, diagnosis and classifcation of
stroke, management, complications, status (death or
disability) at discharge and at 28 day follow up. The
risk factors were as reported by patients or attendants
and supplemented with data from medical records.
Information on diagnosis, complications, management
and outcome was extracted from medical records.
Trained research offcers visited various divisions
of the hospital (casualty and emergency, intensive
care unit, male and female wards (both medical
and neurological), stroke unit and medical records
department for identifying stroke patients on a
daily basis. The diagnosis of stroke was based on
neurological evaluation supported by CT / MRI. Every
identifed patient was followed up daily till discharge
or death. Among those discharged alive, 664 (61.9%)
subjects (residents of Bangalore city) were followed
up at 28 days post discharge to identify post hospital
deaths and to ascertain disability status. The modifed
Rankins scale which measures independence and
functional level of the individual was used for assessing
disability
21
.
Stroke mortality in the community (STEP 2) : Death
records for the period January 1, 2004 to December
31, 2004 maintained by Bangalore Mahanagara Palike
(BMP) - Central administrative offce of the city
were analysed. The Central Statistical Offce receives
mortality information from all 100 ward health offces,
including government hospitals and BMP referral
maternity hospitals. Each death is registered only after
obtaining information in Form 4 (institutional deaths)
or form 4A (non institutional deaths). A data recording
format was developed to extract available information
from death certifcates which included age, gender,
Appendix
The following defnitions were used in the study as recommended
in WHO STEPS stroke manual
21
Stroke: A focal (or at times global) neurological impairment
of sudden onset, and lasting more than 24 h (or leading to
death) and of presumed vascular origin, excludes transient
ischaemic attack (TIA) and haemorrhage and symptoms
caused by trauma.
Defnitive focal signs can be accepted as indicative of a stroke
but must have lasted for more than 24 h and the signs must
be of a presumed vascular origin and include: Unilateral or
bilateral motor impairment and or sensory impairment, non-
fuent speech, half sided impairment of visual felds, diplopia,
conjugate deviation, acute onset apraxia or ataxia or perception
of defcit,
Ischaemic stroke: Caused by sudden occlusion of arteries
supplying the brain, either, due to a thrombus at the site
of occlusion or formed in another part of the circulation.
The diagnosis is based on clinical examination along with
neuroimaging fndings.
Intra-cerebral haemorrhage: Bleeding from one of the brains
arteries into the brain tissue. Usually sudden in onset and the
diagnosis is based on clinical presentation and confrmed by
neuroimaging.
Sub-arachnoid haemorrhage: Characterized by arterial bleeding
in the space between the two meninges; sudden onset of severe
headache or unconsciousness or both. Diagnosis is established
by neuroimaging methods.
Unspecifed stroke: To be used if no diagnostic examination (like
brain imaging ) was performed and diagnosis based on clinical
examination alone.
Fatal stroke: Stroke resulting in death within 28 days after the
onset.
Non fatal stroke: Patients who survive 28 days after the onset
of stroke.
Current tobacco use: Patient currently using any form tobacco
including those who have stopped using less than 3 months
before the stroke event.
Current alcohol use: Patient currently using any type of alcohol
including those who have stopped using less than 1 year before
the stroke event (This defnition was used in the Bangalore study
but is not mentioned in the WHO guidelines).
Diabetes mellitus: Either diagnosis of diabetes pre-stroke or
patient self report, or use of anti-diabetic medication. Includes
diagnosis of diabetes during current hospital stay.
Hypercholesterlaemia: Reported pathological elevated plasma
total or LDL cholesterol levels or use of lipid lowering
medication.
Ramaiah Hospitals (MSRMH), two major tertiary care
institutions attached to medical colleges. A preliminary
exploration was carried out in identifed hospitals
and based on larger registration of stroke patients,
398 INDIAN J MED RES, OCTOBER 2009
NAGARAJA et al: BANGALORE STROKE SURVEILLANCE 399
immediate cause of death, antecedent cause of death,
and other signifcant conditions associated with
death. Stroke specifc search words like weakness of
limbs, paralysis, stroke, cerebrovascular accident, and
hemiplegia was listed out after a pilot validation study
of death records in one of the wards. Research offcers
trained in manual record search by visual sighting
using key search words identifed and recorded all
probable deaths due to stroke
21
. At the second level,
a trained physician again reviewed these records for
cause of death and those due to stroke were included.
In addition to a retrospective mortality record analysis
of one full calendar year, a prospective analysis for
the study reference period was also undertaken using
similar method.
Step 3 focusing on nonfatal events in the community
was not included in the present programme due to
resource constraints. Data analysis was done using Epi-
Info
24
and SPSS
25
. Only major descriptive fndings are
provided in this communication to highlight the type
and nature of information that will be available from a
surveillance approach.
Proportions and rates were used to describe and
compare the results.
Results
Stroke events in the hospitals: A total of 1,174 cases
were registered from the three hospitals during the 6
month period. Stroke constituted 4 per cent (1.5 to
7.5%) of casualty registration, 5 per cent (1 to 18%) of
inpatient registrations, 7 per cent of medical admissions
and 45 per cent (22 to 60%) of neurology registrations
with rates varying across institutions.
The mean age of stroke patients was 54.5 ( 17.0)
yr, with two thirds (65.6%) being 50+ and 18 per cent
below 40 yr (Fig.). A greater preponderance was seen
among men (67%) with a male to female ratio of 2:1.
Higher proportion of women below 30 yr was due
to cortical venous thrombosis (CVT). The observed
difference between age and sex and occurrence of
stroke was statistically signifcant (P<0.01). Nearly
half of stroke subjects were without any education
(N=535, 46%) and employed in non government or
unorganized sectors (N=525, 44.8%), while more than
three fourths were married (N=931, 79.3%)), with a
near equal number of patients residing within (N=664,
56.6%) and outside (N=510, 43.4%) Bangalore.
One third (N=393, 33.5%) of subjects reported
directly and remaining were referred either from
government hospitals (28.6%) or private health care
institutions (36%). Of the latter, approximately 69 per
cent referrals came from private nursing homes, 11 per
cent from general practitioners or a family practitioner.
Amongst those residing in the city, 44 per cent reached
a defnitive hospital later than 48 h, while similar fgure
for those residing outside the city was 56 per cent from
rural areas. The commonest presentation of stroke was
weakness or paresis (92%) with the left and the right side
of the body being involved in almost equal proportions
(46.2 and 47.4%, respectively). Speech and/or language
disturbances and disturbed consciousness was reported
by 73.9 and 14.7 per cent of the patients, respectively
(Table I). A CT scan was done for 1085 (92%) of the
registered patients; amongst them 610 (52%) was
within 24 h but was delayed (24 h to 7 days) in 468
Fig. Age-sex distribution of stroke patients (% hospitalised
patients).
Table I. Neurological presentation of the stroke subjects and
diagnosis (n=1174)
n %
Source of referral:
Direct or self referral 393 33.5
Government hospital 336 28.6
Nursing home 289 24.6
Private teaching hospital 72 6.1
General practitioner 47 4.0
Others 37 3.2
Time interval since stroke onset and defnitive care:
Less than 24 h 320 27.3
24 to 48 h 343 29.2
> 48 h 511 43.5
Presenting symptoms:
Weakness or paresis 1081 92.1
Left 499 46.2
Right 513 47.4
Both 69 6.4
Problems with speech 868 73.9
Disturbed consciousness 173 14.7
Diagnostic investigations:
CT scan 1085 92.4
MRI scan 163 13.9
Carotid ultrasound 162 13.8
(40%) of the cases. The certainty of diagnosis of stroke
was very high in 92 per cent of the cases. Ischaemic
stroke was the most frequent (73.8%), followed by
Intra-cerebral hemorrhage (13.7%), cortical venous
thrombosis (8.7%) and subarachnoid haemorrhage
(1.4%). Depending on the type of institution, majority
of the cases were frst admitted into the emergency
rooms (63.5%) and subsequently managed by either
neurology and / or medical unit.
With regard to risk factors, 13 per cent reported
a previous history of stroke, 48 per cent were
hypertensive, 23 per cent reported to be diabetic, 33 per
cent used tobacco and 25 per cent consumed alcohol
(Table II). Nearly 1 in 5 patients had both hypertension
and diabetes (18.5%). A family history of stroke was
reported by 7.3 per cent of patients. While 23 per cent
did not have any risk factor, 29 per cent had one risk
factor and 30.0 and 11.6 per cent, had 3 or more than 3
risk factors, respectively.
Among the hospital registered patients, 102 out
of 1174 died during their hospital stay resulting in
case fatality rate of 8.7 per cent. Of those patients
discharged alive (1072), 664 patients could be followed
up to 28 days and 81 (12.2%) patients had died during
the reference period. Assuming the same fatality rate
amongst those who could not be followed up (50 out
of 408), the total number of deaths in the series was
233, with an overall case fatality rate of 19.8 per cent.
Among the survivors (1072 patients), one-third (32.5%)
were discharged home and remaining were referred to
other hospitals (67.5%). At the time of discharge, one
third of the patients (31.3%) were dependent on others
[either being not able to walk - 25.7% or having other
severe disabilities - 5.6%]. This overall proportion
changed marginally (from 31.3 to 29.7%) during the 28
day follow up. Further, it was observed that nearly one
out of two patients continued to have some disability
even at 28 days after discharge (Slight disability-25.3%
and moderate disability but able to walk-26.8%)
(Table III).
Stroke mortality in the community: From a total
of 23,312 available death records at Bangalore
Mahanagara Palike, 1,690 (7.5%) deaths could be
categorized as probably due to stroke. The physician
review of the given cause(s) of death excluded non
stroke deaths and resulted in 83 per cent of deaths
classifed as defnitively due to stroke. The proportional
mortality rate of stroke in the city of Bangalore for the
year 2004 was thus calculated to be 6.0 per cent. The
overall crude stroke mortality rate was 326 per million,
with rates being higher in men (388 vs. 257 per million
population). Nearly 97 per cent of stroke deaths
occurred in health care institutions; it was observed
that nearly 50 per cent of stroke deaths occurred in 10
major hospitals alone. Nearly 62 per cent of the stroke
deaths were amongst men with a male: female ratio of
2:1. The age specifc mortality rate revealed that stroke
deaths increased from 30 yr and reached a peak around
65 yr (45%) with 20 per cent in less than 45 yr.
Continuing to explore the feasibility of a stroke
surveillance programme, a total of 2049 deaths records
were analyzed for the period March 1, 2005 to August
31, 2005 in the three health ranges attached to 3 study
hospitals. Nearly 85 per cent (76 to 95%) of the stroke
deaths reported from the three ranges were from the
three study hospitals and 7.9 per cent (6 to 11%) of the
deaths in these 3 ranges were due to stroke.
Discussion
Previous studies on stroke
11,12
, earlier
neuroepidemiological surveys
11,26
and stroke
registries
7,17-19
have identifed the burden and select
characteristics of stroke but there have been several
gaps in continuous and comprehensive information
needed for planning and implementing integrated
programmes. Most studies have been one time efforts
and not continuous, single hospital based, while the
methodology and focus of information gathering
has varied. Hospital registries have estimated risk
Table II. Major risk factors for stroke
*
Risk factors n=1174 %
Previous history of stroke 154 13.1
Hypertension 563 48.0
Tobacco use 383 32.6
Alcohol use 295 25.1
Diabetes mellitus 271 23.1
Atrial fbrillation 114 9.7
Family history of stroke 86 7.3
*As reported by patients and/or ascertained from medical records
Table III. Disability status of the hospitalized stroke subjects
(Modifed Rankin Scale, %)
At discharge
(n=1072)
At 28 day
follow up
(n=583)
No symptoms (0) 1.4
Symptoms present but not related to
stroke and no disability (1)
24.4 16.8
Slight disability (2) 6.5 25.3
Moderate disability able to walk (3) 37.8 26.8
Moderate disability not able to walk (4) 25.7 26.8
Severe disability (5) 5.6 2.9
400 INDIAN J MED RES, OCTOBER 2009
factors and selective fatality rates but failed to provide
information on mortality for the larger population. The
present study has shown that it was possible to collect
minimal, good quality, vital data in different hospital
settings and also from the city vital registry division.
Information on characteristics of stroke, risk factors,
disability and outcome and mortality rates were
gathered by a uniform methodology. Supplementing
this information with periodical data from non fatal
events in community can help in comprehensive
and total understanding of stroke events in defned
populations.
The present study registered a larger number of
CT confrmed stroke cases in the limited period of 6
months. The observation that nearly 6 - 8 per cent of
total deaths in the city and 20 per cent of stroke deaths
occurring during or soon after discharge (case fatality
rate of 20%) indicate that stroke is a major public
health problem. Nearly 5 to 10 per cent of the hospital
patients and half of neurology patients were due to
stroke. Majority of stroke deaths and hospitalizations
occurred amongst the 50 to 65 yr old population and
were predominantly among men. The 28 day follow
up showed that 55 per cent of the stroke survivors had
moderate to severe disabilities. The methodology and
mechanism evolved by the current study (integrating
with existing systems - vital registration system and
hospitals), collecting data by use of existing and
available records, ensuring completeness of data
and simplicity of the study instrument can serve as
guidelines for initiating stroke surveillance in India.
The need for strengthening mortality information
needs no overemphasis and is critical to identify fatal
stroke events in the community.
At the city level, 97 per cent of the stroke deaths
occurred in institutions, with 50 per cent of these
from 10 major hospitals alone. Thus, identifcation
and inclusion of select large health care institutions
will ensure wider coverage along with inclusion
of large number of patients in a given and defned
geographic area. It is desirable to begin with lesser
number of institutions, establish quality control
mechanisms and expand in phases. These centres can
serve as sentinel centres for stroke surveillance. In
India, private sector provides care for nearly 70 per
cent of health care needs
27
, and in the present study
nearly 50 per cent of deaths occurred in smaller
hospitals or nursing homes and all these were in the
private sector. Thus, it is important to involve these
in the overall programme for stroke management
and prevention.
Nearly three fourths (77%) of the study group had
one or more known risk factors for stroke with one
in fve patients being both hypertensive and diabetic.
Mendis et al
28
have reported that in middle and low
income countries one in two patients has at least two or
more risk factors for either ischaemic heart disease or
stroke and a signifcant number of patients do not receive
appropriate medication. Evidence from high income
countries reveal that modifying risk factors remains
a major strategy for decreasing the stroke burden
2,5,,29
.
As many risk factors are common between stroke and
other NCDs, risk factor prevention programmes would
contribute to a greater extent in reducing the burden
of stroke and other NCDs
1,2,30,31
. The observations from
the current study critically refects on need for building
integrated programmes and surveillance will be helpful
in strengthening these activities. NCD risk factor
surveillance is already under progress and it would be
helpful to include stroke surveillance in these centers.
However, certain challenges need to be overcome
for establishing stroke surveillance and from the
early stages itself. Methods to include cases based on
physician / neurologist evaluation (neurologists and
CT facilities may not be available everywhere) and
inclusion of private hospitals and diagnostic centers
need to be evolved in a systematic way. With availability
of CT facilities in urban areas and in districts, case
identifcation and diagnostic ascertainment would
become easier. Identifying units in hospitals where
stroke patients are likely to be included (emergency
room, outpatients, inpatients, ICU) and utilizing
different types of hospital records ensured that all cases
were included in the present study, and this needs to
be developed in all centers included for surveillance in
future.
Step 3 which aims at inclusion of non fatal
community stroke events was not included in present
feasibility study. However, some of the centres have
initiated this and their experience has shown that it is
possible
23
.
Stroke surveillance needs to be planned and
implemented in a phased manner, beginning with
medical college hospitals, select urban hospitals and
district hospitals in rural areas. Stroke surveillance
can be initiated in centers already identifed for
NCD risk factor surveillance along with appropriate
use of information technology through web based
approaches. This integrated approach is feasible
and better suited to the Indian context to develop
programmes in India and other LMICs in the coming
NAGARAJA et al: BANGALORE STROKE SURVEILLANCE 401
years
3
. The success and sustainability of stroke
surveillance programme depends on simplicity of
data collection process, utilization and feedback to
all partners for action
33,32
.
In conclusion, despite limitations of shorter
duration along with resource constraints, the present
study has shown that establishing population based
stroke surveillance for fatal and non fatal events
is both possible and feasible and needs to develop
specifc mechanisms to overcome challenges in India.
With the recognition of stroke as a major public health
problem, there is a need for long term, continuous,
and good quality information to monitor trends,
identify risk factors, develop - implement and evaluate
interventions.
Acknowledgment
Authors acknowledge the fnancial grant received from World
Health Organization, South East Asia Regional Offce, New Delhi
(ICP GPE 002) and Indian Council of Medial Research, New Delhi.
The authors thank Drs Ruth Bonita and Thomas Truelson from
WHO, Geneva, for technical guidance, encouragement and support
in undertaking this study and the entire feld staff involved in data
collection (Dr Kavita R, Junior Scientifc Offcer in Epidemiology,
Dr Pandian D, Assistant Professsor of Psychiatric Social Work,
Lakshminarayan KL, Narayanaswamy and Dr Thandavamurthy
PS from Bangalore Mahanagara Palike and the feld team of Dr
Lavanya G; Shriyut Basavaraju KS, Manjunath DP, Shanmukha
CG, Srinivasamurthy KG , Suresh C, Gangaraju, Saniwaram Reddy
and Ananda G).
References
1. Warlow C, Sudlow C, Dennis M, Warlow C, Sudlow C, Dennis
M, et al. Stroke. Lancet 2003; 362 : 1211-24.
2. Strong K, Mathers C, Bonita R. Preventing stroke: saves lives
around the world. Lancet Neurol 2007; 6 : 182-7.
3. Feigin VL. Stroke in developing countries: can the epidemic
be stopped and outcomes improved. Lancet Neurol 2007; 6 :
94-7.
4. Feigin VL. Stroke epidemiology in the developing world.
Lancet 2005; 365 : 2160-1.
5. World Health Organization. The economic impact of chronic
diseases in preventing chronic diseases: a vital investment.
World Health Organization, Geneva; 2005.
6. Liu M, Wu B, Wang W, Lee L, Zhang S, Kong L. Stroke in
China: Epidemiology, prevention and management strategies.
Lancet Neurol 2007; 8 : 456-64.
7. Dalal P, Bhattacharjee M, Vairale J, Bhat P. UN Millennium
development goals: Can we halt the stroke epidemic in India.
Ann Indian Acad Neurol 2007; 10 : 130-6.
8. Anand K, Chowdury D, Singh KB, Pandav CS, Kapoor SK.
Estimation of mortality and morbidity due to strokes in India.
Neuroepidemiology 2001; 20 : 208-11.
9. Indian Council for Medical Research. Stroke. In: Assessment
of the burden of non communicable diseases: Final project
report. New Delhi: Indian Council of Medical Research;
2004. p. 18-22.
10. Indrayan A. Forecasting vascular disease cases and associated
mortality in India. In; Burden of disease in India, Vol
2, NMCH background papers, National Commission on
Macroeconomics nd Health, Ministry of Health and Family
Welfare, Government of India; 2005. p. 197-215.
11. Baneerjee TK, Das SK. Epidemiology of strokes in India.
Neurol Asia 2006; 11 : 1-4.
12. Bhattacharya S, Saha SP, Basu A, Das SK. A 5 years prospective
study of incidence, morbidity and mortality profle of stroke in
a rural community of eastern India. J Indian Med Assoc 2005;
103 : 655-9.
13. Das SK, Banerjee TK, Biswas A, Roy T, Raut DK, Mukherjee
CS, et al. A prospective community-based study of stroke in
Kolkata, India. Stroke 2007; 38 : 906-10.
14. Gupta R. Trends in hypertension epidemiology in India.
J Hum Hypertens 2004; 18 : 73-8.
15. Banerjee TK, Roy MK, Bhoi KK. Is stroke increasing in
India preventive measures that need to be implemented?
J Indian Med Assoc 2005; 103 : 162-4.
16. Dalal PM. Burden of stroke: Indian perspective. Int J Stroke
2006; 1 : 164-6.
17. Kaul S, Venkataswmy P, Meena AK, Sahay R, Murthy
JMK. Frequency, clinical features and risk factors of lacunar
infarction (Data from a Stroke registry from South India).
Neurol India 2000; 48 : 116-9.
18. Arjundas D, Pandiyan U, Arjundas G, Baux H. Surveillance
of stroke: WHO STEP-wise approach: A Chennai stroke Unit
report. Ann Indian Acad Neurol 2007; 10 : 154-9.
19. Nagaraja D, Gururaj G, Jayakumar R, Subbakrishna DK.
Summary report of the project Stroke Registry in NIMHANS,
NIMHANS/NEU/Reports/Stroke/2000 (unpublished report).
20. Dalal PM, Bhattacharjee M. Stroke epidemic in India:
Hypertension stroke control programme is urgently needed
J Assoc Physicians India 2007; 55 : 689-91.
21. World Health Organization: The WHO STEPs Stroke Manual.
The WHO STEPwise approach to stroke surveillance Geneva:
World Health Organization; 2006.
22. Truelsen T, Heuschmann PU, Bonita R, Arjundas G, Dalal
P, Damasceno A, et al. Standard method for developing
stroke registers in low-income and middle-income countries:
experiences rom a feasibility study of a stepwise approach to
stroke surveillance (STEPS Stroke). Lancet Neurol 2007; 6 :
134-9.
23. Dalal PM, Bhattacharjee M, Vairale J, Bhat P. Mumbai stroke
registry (2005-2006) Surveillance using WHO steps stroke
Instrument challenges and opportunities. J Assoc Physicians
India 2008; 56 : 675-80.
24. Epi Info: Database and statistics software for public health
professionals. Version 3.3.2 February 9 2005, Centre for
Disease Control. Available from: http://www.cdc.gov/epiinfo/,
accessed on March 4, 2005.
25. SPSS (Statistical Package for Social Sciences) for Windows,
Release 11.0.0; 2001.
26. Gourie-Devi M, Gururaj G, Satishchandra P, Subbakrishna
DK. Prevalence of neurological disorders in Bangalore, India:
402 INDIAN J MED RES, OCTOBER 2009
Reprint requests: Dr D. Nagaraja, Professor of Neurology & Director & Vice Chancellor, National Institute of Mental Health &
Neuro Sciences, Bangalore 560 029, India
e-mail: dnn@nimhans.kar.nic.in
A community based study with an urban-rural comparison.
Neuroepidemiology 2004; 23 : 261-8.
27. Government of India. National Health Accounts India 2001
2002, National Health Accounts Cell, Ministry of Health
and Family Welfare, Government of India, New Delhi; 2005.
28. Mendis S, Abegunde D, Yusuf S, Ebrahim S, Shaper G,
Ghannem H, et al. WHO study on prevention of recurrences
of myocardial infarction and stroke (WHO-PREMISE). Bull
World Health Organ 2005; 83 : 820-8.
29. Rothwell PM, Coull AJ, Giles MF, Howard S, Silver L,
Bull L, et al. Change in stroke incidence, mortality, case-
fatality, severity, and risk factors in Oxfordshire, UK from
1981 to 2004 (Oxford Vascular Study). Lancet 2004; 363 :
1925-33.
30. Goyal A, Yusuf S. The burden of cardiovascular disease in the
Indian subcontinent. Indian J Med Res 2006; 124 : 235-44.
31. Gaziano TA. Reducing the growing burden of cardiovascular
disease in the developing world. Health Aff (Millwood) 2007;
26 : 13-24.
32. Truelson T, Bonita R, Jamrozik K. Surveillance of stroke: a
global perspective Int J Epidemiol 2001; 30 : s11-6.
33. World Bank, 2002: Public Health Surveillance tool kit.
Available from: http://siteresources.worldbank.org/INTPH/
Resources/376086-1133371165476/PHSurveillanceToolkit.pdf,
accessed on December 9, 2007.
NAGARAJA et al: BANGALORE STROKE SURVEILLANCE 403
Vous aimerez peut-être aussi
- Telemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.D'EverandTelemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.Pas encore d'évaluation
- 2020-Indian Journal of Public Health Research and Development (Scopus Q-4)Document5 pages2020-Indian Journal of Public Health Research and Development (Scopus Q-4)NoniAndayaniPas encore d'évaluation
- Hypertension Prediction Using Machine Learning Algorithm Among Indonesian AdultsDocument9 pagesHypertension Prediction Using Machine Learning Algorithm Among Indonesian AdultsIAES IJAIPas encore d'évaluation
- Assessment of Knowledge of Osteoarthritis Among Elderly PatientsDocument7 pagesAssessment of Knowledge of Osteoarthritis Among Elderly PatientsMostafa ShabanPas encore d'évaluation
- A Data-Driven Approach To Predicting Diabetes and Cardiovascular Disease With Machine LearningDocument15 pagesA Data-Driven Approach To Predicting Diabetes and Cardiovascular Disease With Machine LearningKnowledgepoint KpPas encore d'évaluation
- Sample 2Document11 pagesSample 2Muhamad Fikri AzizPas encore d'évaluation
- AP Comparación PaisesDocument10 pagesAP Comparación PaisesMiguel Ángel Estévez PAzPas encore d'évaluation
- Diagnostics: A Machine-Learning-Based Prediction Method For Hypertension Outcomes Based On Medical DataDocument21 pagesDiagnostics: A Machine-Learning-Based Prediction Method For Hypertension Outcomes Based On Medical DatafarzanaPas encore d'évaluation
- Chronic Diseases and InjuriesDocument16 pagesChronic Diseases and InjuriesShama ChalkePas encore d'évaluation
- CVD Risk EstimationDocument8 pagesCVD Risk EstimationparthibanePas encore d'évaluation
- Prevalence of Stroke in The Elderly A Systematic Review and Meta-AnalysisDocument10 pagesPrevalence of Stroke in The Elderly A Systematic Review and Meta-AnalysisMarian J. NietoPas encore d'évaluation
- Post-Stroke Patients With Moderate Function Have The Greatest Risk of Falls: A National Cohort StudyDocument9 pagesPost-Stroke Patients With Moderate Function Have The Greatest Risk of Falls: A National Cohort Studyhari vijayPas encore d'évaluation
- ContentServer Psico1Document14 pagesContentServer Psico1Luis.fernando. GarciaPas encore d'évaluation
- Elsevier Article PaperDocument24 pagesElsevier Article Paperjaveriazia97Pas encore d'évaluation
- Proceedings ICHLSR Singapore, JuneDocument29 pagesProceedings ICHLSR Singapore, JuneGlobal Research and Development ServicesPas encore d'évaluation
- WHO CVD Risk FactorsDocument18 pagesWHO CVD Risk FactorsparthibanePas encore d'évaluation
- 2019 - Kang - Does A Mobile App Improve Patients'Document9 pages2019 - Kang - Does A Mobile App Improve Patients'Warsi MaryatiPas encore d'évaluation
- The Bioterrorism Preparedness and Response Early Aberration Reporting System (EARS)Document8 pagesThe Bioterrorism Preparedness and Response Early Aberration Reporting System (EARS)Jojo MarinayPas encore d'évaluation
- Medical Tribune January 2012 HKDocument72 pagesMedical Tribune January 2012 HKKarena SabadoPas encore d'évaluation
- Aids 33 s283Document12 pagesAids 33 s283ilhamfajriPas encore d'évaluation
- Life Expectancy Using Data AnalyticsDocument9 pagesLife Expectancy Using Data AnalyticsIJRASETPublications100% (1)
- TH 16024Document10 pagesTH 16024dnoksPas encore d'évaluation
- 2008 - Feigin - Long Term Neuropsychological Functional Outcomes StrokeDocument8 pages2008 - Feigin - Long Term Neuropsychological Functional Outcomes StrokeLourdes CFPas encore d'évaluation
- Effect of Lifestyle Modification Intervention On Health Status of Coronary Artery Disease Patients Randomized Control TrialDocument14 pagesEffect of Lifestyle Modification Intervention On Health Status of Coronary Artery Disease Patients Randomized Control TrialRobet Agung wicaksonoPas encore d'évaluation
- 14 - Towards Best Practice in Acute Stroke Care in Ghana A Survey of Hospital ServicesDocument11 pages14 - Towards Best Practice in Acute Stroke Care in Ghana A Survey of Hospital ServicesChristel CibalonzaPas encore d'évaluation
- A Hybrid Model For Forecasting Communicable Diseases in MaldivesDocument13 pagesA Hybrid Model For Forecasting Communicable Diseases in MaldivesMervat BamiahPas encore d'évaluation
- The Satisfactionof Patients On Maintenance Hemodialysis Concerning The Provided Nursing Care in Hemodialysis UnitsDocument11 pagesThe Satisfactionof Patients On Maintenance Hemodialysis Concerning The Provided Nursing Care in Hemodialysis Unitsbe a doctor for you Medical studentPas encore d'évaluation
- Stroke Risk Screening Scales (SRSS) : Identi Fication of Domain and Item GenerationDocument8 pagesStroke Risk Screening Scales (SRSS) : Identi Fication of Domain and Item Generationandi kurniawanPas encore d'évaluation
- J of Clinical Hypertension - 2019 - Kanegae - Highly Precise Risk Prediction Model For New Onset Hypertension UsingDocument6 pagesJ of Clinical Hypertension - 2019 - Kanegae - Highly Precise Risk Prediction Model For New Onset Hypertension UsingMarie VarangotPas encore d'évaluation
- Risk Factors, Clinical Presentations and Predictors of Stroke Among Adult Patients Admitted To Stroke Unit of Jimma University Medical Center, South West Ethiopia: Prospective Observational StudyDocument11 pagesRisk Factors, Clinical Presentations and Predictors of Stroke Among Adult Patients Admitted To Stroke Unit of Jimma University Medical Center, South West Ethiopia: Prospective Observational StudyReyhan AristoPas encore d'évaluation
- Prediction of Intracranial Aneurysm Risk Using Machine LearningDocument10 pagesPrediction of Intracranial Aneurysm Risk Using Machine LearningKiran KumarPas encore d'évaluation
- Assessment of Knowledge, Attitude and Practice of Health Information Management Professionals Towards Integrated Disease Surveillance & Response (IDSR) in Abuja, Nigeria.Document48 pagesAssessment of Knowledge, Attitude and Practice of Health Information Management Professionals Towards Integrated Disease Surveillance & Response (IDSR) in Abuja, Nigeria.Victor Chibueze IjeomaPas encore d'évaluation
- Knowledge, Practice, and Attitude Towards Deep Vein Thrombosis Prophylaxis Among Residents and Interns in King Saud Medical CityDocument8 pagesKnowledge, Practice, and Attitude Towards Deep Vein Thrombosis Prophylaxis Among Residents and Interns in King Saud Medical CityIJAR JOURNALPas encore d'évaluation
- Main 25Document6 pagesMain 25pokharelriwaj82Pas encore d'évaluation
- Assessment of Awareness of Diabetic Retinopathy Among Type 2 Diabetes Mellitus Cross Sectional Study From Central IndiaDocument7 pagesAssessment of Awareness of Diabetic Retinopathy Among Type 2 Diabetes Mellitus Cross Sectional Study From Central IndiaAthenaeum Scientific PublishersPas encore d'évaluation
- Out 9Document11 pagesOut 9restu anindityaPas encore d'évaluation
- Who 2016 PDFDocument2 pagesWho 2016 PDFRefialy WahyyPas encore d'évaluation
- 75-Article Text-329-1-10-20220929Document16 pages75-Article Text-329-1-10-20220929BrianPas encore d'évaluation
- The Burden of Antimicrobial Resistance (AMR) in IndonesiaDocument4 pagesThe Burden of Antimicrobial Resistance (AMR) in IndonesiaJeanny APas encore d'évaluation
- Healthcare 11 01803Document25 pagesHealthcare 11 01803Trang PhạmPas encore d'évaluation
- Press Release-COVID-19 Survey (1) 5-12-20Document5 pagesPress Release-COVID-19 Survey (1) 5-12-20Ravikiran SuryanarayanamurthyPas encore d'évaluation
- Evaluation of Stroke Rehabilitation Services in The In-Hospital Phase: Findings From A Tertiary Care Centre in IndiaDocument15 pagesEvaluation of Stroke Rehabilitation Services in The In-Hospital Phase: Findings From A Tertiary Care Centre in IndiaIJAR JOURNALPas encore d'évaluation
- Jurnal MuskuloDocument8 pagesJurnal MuskuloarvinelaPas encore d'évaluation
- 25FirouzAmani EtalDocument6 pages25FirouzAmani EtaleditorijmrhsPas encore d'évaluation
- BMC Public Health: Evaluation of Reporting Timeliness of Public Health Surveillance Systems For Infectious DiseasesDocument9 pagesBMC Public Health: Evaluation of Reporting Timeliness of Public Health Surveillance Systems For Infectious DiseasesAnis RanisPas encore d'évaluation
- Prevalence and Awareness of Hypertension in NigeriaDocument13 pagesPrevalence and Awareness of Hypertension in NigeriaTaoreed AdegokePas encore d'évaluation
- Impact of Big Data Analytics On People's Health: Overview of Systematic Reviews and Recommendations For Future StudiesDocument14 pagesImpact of Big Data Analytics On People's Health: Overview of Systematic Reviews and Recommendations For Future Studiesalemayehu badargaPas encore d'évaluation
- The Relationships Between Step Count and All-Cause Mortality and Cardiovascular Events A Dose-Response Meta-Analysis - 1-S2.0-S2095254621001010-MainDocument9 pagesThe Relationships Between Step Count and All-Cause Mortality and Cardiovascular Events A Dose-Response Meta-Analysis - 1-S2.0-S2095254621001010-Mainandrina.michelPas encore d'évaluation
- 논문원문Document7 pages논문원문Donghee LeePas encore d'évaluation
- Diagnostics: Mobile Health in Remote Patient Monitoring For Chronic Diseases: Principles, Trends, and ChallengesDocument32 pagesDiagnostics: Mobile Health in Remote Patient Monitoring For Chronic Diseases: Principles, Trends, and ChallengesEngahmed IsmailPas encore d'évaluation
- Prevalence and Risk Factors For ChronicDocument10 pagesPrevalence and Risk Factors For ChronicKhoirul AnamPas encore d'évaluation
- Mhealth Interventions To Improve Cancer Screening and Early Detection: Scoping Review of ReviewsDocument19 pagesMhealth Interventions To Improve Cancer Screening and Early Detection: Scoping Review of ReviewsSiti MunawwarahPas encore d'évaluation
- Association Rules To Analyze Hospital Resources With Mortality RatesDocument7 pagesAssociation Rules To Analyze Hospital Resources With Mortality RatesIJRASETPublicationsPas encore d'évaluation
- Direct Costs of Parkinson's Disease in Brazil: A Case StudyDocument8 pagesDirect Costs of Parkinson's Disease in Brazil: A Case StudyIJAERS JOURNALPas encore d'évaluation
- Prevalence of Risk Factors of Non-Communicable Diseases in The Sultanate of Oman: STEPS Survey 2017Document23 pagesPrevalence of Risk Factors of Non-Communicable Diseases in The Sultanate of Oman: STEPS Survey 2017Muhrijal NurPas encore d'évaluation
- A Prospective Descriptive Study of Trauma Registry in Netaji Subhash Chandra Bose Medical College, JabalpurDocument9 pagesA Prospective Descriptive Study of Trauma Registry in Netaji Subhash Chandra Bose Medical College, JabalpurIJAR JOURNALPas encore d'évaluation
- Issm Prisma ChecklistDocument9 pagesIssm Prisma ChecklistInnani Wildania HusnaPas encore d'évaluation
- Prevalence of Diabetes in ArmyDocument12 pagesPrevalence of Diabetes in Armydhanusat20001828Pas encore d'évaluation
- Identification and Prediction of Chronic Diseases Using MachineDocument9 pagesIdentification and Prediction of Chronic Diseases Using MachineMuhammad Sadiq Khan NasarPas encore d'évaluation
- Paper 1Document13 pagesPaper 1Michael JamesPas encore d'évaluation
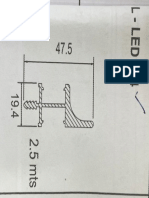
- Utturkar Wall L-Led 214 ProfileDocument1 pageUtturkar Wall L-Led 214 ProfileAngad SinghPas encore d'évaluation
- Shed DetailsDocument6 pagesShed DetailsAngad SinghPas encore d'évaluation
- 100 Beded Cancer HospitalDocument23 pages100 Beded Cancer Hospitalsureshvgk100% (1)
- Nursing Home 200 Beded PDFDocument40 pagesNursing Home 200 Beded PDFarun_tushar67% (3)
- 1business EnvironmentDocument13 pages1business EnvironmentAngad SinghPas encore d'évaluation
- Schedules of Shared Day Companies - MITCOEDocument1 pageSchedules of Shared Day Companies - MITCOEKalpak ShahanePas encore d'évaluation
- Family Code Cases Full TextDocument69 pagesFamily Code Cases Full TextNikki AndradePas encore d'évaluation
- PERDEV2Document7 pagesPERDEV2Riza Mae GardosePas encore d'évaluation
- 78 Complaint Annulment of Documents PDFDocument3 pages78 Complaint Annulment of Documents PDFjd fang-asanPas encore d'évaluation
- Modernity and Politics in IndiaDocument27 pagesModernity and Politics in Indiaarun_shivananda2754Pas encore d'évaluation
- StarbucksDocument19 pagesStarbucksPraveen KumarPas encore d'évaluation
- RPA Solutions - Step Into The FutureDocument13 pagesRPA Solutions - Step Into The FutureThe Poet Inside youPas encore d'évaluation
- Basic Fortigate Firewall Configuration: Content at A GlanceDocument17 pagesBasic Fortigate Firewall Configuration: Content at A GlanceDenisa PriftiPas encore d'évaluation
- Chapter 1 Basic-Concepts-Of-EconomicsDocument30 pagesChapter 1 Basic-Concepts-Of-EconomicsNAZMULPas encore d'évaluation
- Lec 15. National Income Accounting V3 REVISEDDocument33 pagesLec 15. National Income Accounting V3 REVISEDAbhijeet SinghPas encore d'évaluation
- Department of Planning and Community Development: Organizational ChartDocument5 pagesDepartment of Planning and Community Development: Organizational ChartkeithmontpvtPas encore d'évaluation
- Online Advertising BLUE BOOK: The Guide To Ad Networks & ExchangesDocument28 pagesOnline Advertising BLUE BOOK: The Guide To Ad Networks & ExchangesmThink100% (1)
- Swot MerckDocument3 pagesSwot Mercktomassetya0% (1)
- Three VignettesDocument3 pagesThree VignettesIsham IbrahimPas encore d'évaluation
- British Airways Vs CADocument17 pagesBritish Airways Vs CAGia DimayugaPas encore d'évaluation
- JAR66Document100 pagesJAR66Nae GabrielPas encore d'évaluation
- 2018-Gray-Life, Death, or Zombie - The Vitality of International OrganizationsDocument13 pages2018-Gray-Life, Death, or Zombie - The Vitality of International OrganizationsNightWalkerPas encore d'évaluation
- Tok SB Ibdip Ch1Document16 pagesTok SB Ibdip Ch1Luis Andrés Arce SalazarPas encore d'évaluation
- A Collection of Poems by AKDocument16 pagesA Collection of Poems by AKAnanda KrishnanPas encore d'évaluation
- List of Ielts Speking Part 3Document20 pagesList of Ielts Speking Part 3Kumiko LinoPas encore d'évaluation
- Special Power of Attorney: Know All Men by These PresentsDocument1 pageSpecial Power of Attorney: Know All Men by These PresentsTonie NietoPas encore d'évaluation
- Ppg-Gdch-Nur-45 Crash Cart Maintenance and ChecksDocument5 pagesPpg-Gdch-Nur-45 Crash Cart Maintenance and ChecksKenny JosefPas encore d'évaluation
- AKL - Pert 2-2Document2 pagesAKL - Pert 2-2Astri Ririn ErnawatiPas encore d'évaluation
- Project On Hospitality Industry: Customer Relationship ManagementDocument36 pagesProject On Hospitality Industry: Customer Relationship ManagementShraddha TiwariPas encore d'évaluation
- Greek Gods & Goddesses (Gods & Goddesses of Mythology) PDFDocument132 pagesGreek Gods & Goddesses (Gods & Goddesses of Mythology) PDFgie cadusalePas encore d'évaluation
- Ethiopia Pulp & Paper SC: Notice NoticeDocument1 pageEthiopia Pulp & Paper SC: Notice NoticeWedi FitwiPas encore d'évaluation
- Philippine CuisineDocument1 pagePhilippine CuisineEvanFerrerPas encore d'évaluation
- Digi Bill 13513651340.010360825015067633Document7 pagesDigi Bill 13513651340.010360825015067633DAVENDRAN A/L KALIAPPAN MoePas encore d'évaluation
- Monopolistic CompetitionDocument4 pagesMonopolistic CompetitionAzharPas encore d'évaluation
- WAS 101 EditedDocument132 pagesWAS 101 EditedJateni jotePas encore d'évaluation
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryD'EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryÉvaluation : 4.5 sur 5 étoiles4.5/5 (157)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisD'EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (9)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreD'EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreÉvaluation : 5 sur 5 étoiles5/5 (17)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesD'EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesÉvaluation : 5 sur 5 étoiles5/5 (70)
- An Autobiography of Trauma: A Healing JourneyD'EverandAn Autobiography of Trauma: A Healing JourneyÉvaluation : 5 sur 5 étoiles5/5 (2)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeD'EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeÉvaluation : 4.5 sur 5 étoiles4.5/5 (140)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDD'EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDÉvaluation : 4.5 sur 5 étoiles4.5/5 (167)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerD'EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerÉvaluation : 4.5 sur 5 étoiles4.5/5 (16)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionD'EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionPas encore d'évaluation
- Triggers: How We Can Stop Reacting and Start HealingD'EverandTriggers: How We Can Stop Reacting and Start HealingÉvaluation : 5 sur 5 étoiles5/5 (58)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsD'EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsÉvaluation : 4.5 sur 5 étoiles4.5/5 (39)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeD'EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeÉvaluation : 4.5 sur 5 étoiles4.5/5 (49)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeD'EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeÉvaluation : 5 sur 5 étoiles5/5 (558)
- Brain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensD'EverandBrain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensÉvaluation : 5 sur 5 étoiles5/5 (2)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaD'EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (56)
- I Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionD'EverandI Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionÉvaluation : 4 sur 5 étoiles4/5 (74)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveD'EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveÉvaluation : 4 sur 5 étoiles4/5 (250)
- Don't Panic: Taking Control of Anxiety AttacksD'EverandDon't Panic: Taking Control of Anxiety AttacksÉvaluation : 4 sur 5 étoiles4/5 (12)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisD'EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisÉvaluation : 5 sur 5 étoiles5/5 (5)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIOND'EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONÉvaluation : 4.5 sur 5 étoiles4.5/5 (24)
- Embrace Your Weird: Face Your Fears and Unleash CreativityD'EverandEmbrace Your Weird: Face Your Fears and Unleash CreativityÉvaluation : 4.5 sur 5 étoiles4.5/5 (124)
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsD'EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsÉvaluation : 4.5 sur 5 étoiles4.5/5 (48)
- When Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionD'EverandWhen Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionÉvaluation : 4 sur 5 étoiles4/5 (11)