Académique Documents
Professionnel Documents
Culture Documents
R Hipotermia
Transféré par
Manuel AzabacheDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
R Hipotermia
Transféré par
Manuel AzabacheDroits d'auteur :
Formats disponibles
Hypothermia and Early Neonatal Mortality in Preterm Infants
Maria Fernanda Branco de Almeida, MD, PhD
1
, Ruth Guinsburg, MD, PhD
1
, Guilherme Assis Sancho, MD
1
,
Izilda Rodrigues Machado Rosa, MD, PhD
2
, Zeni Carvalho Lamy, MD, PhD
3
, Francisco Eul
ogio Martinez, MD, PhD
4
,
Regina Paula Guimar
~
aes Vieira Cavalcante da Silva, MD, PhD
5
, L
gia Silvana Lopes Ferrari, MD, PhD
6
,
Ligia Maria Suppo de Souza Rugolo, MD, PhD
7
, V
^
ania Olivetti Steffen Abdallah, MD, PhD
8
, and
Rita de C
assia Silveira, MD, PhD
9
, on behalf of Brazilian Network on Neonatal Research*
Objective To evaluate intervention practices associated with hypothermia at both 5 minutes after birth and at
neonatal intensive care unit (NICU) admission and to determine whether hypothermia at NICU admission is asso-
ciated with early neonatal death in preterm infants.
Study design This prospective cohort included 1764 inborn neonates of 22-33 weeks without malformations
admitted to 9 university NICUs from August 2010 through April 2012. All centers followed neonatal International
Liaison Committee on Resuscitation recommendations for the stabilization and resuscitation in the delivery room
(DR). Variables associated with hypothermia (axillary temperature <36.0
C) 5 minutes after birth and at NICUadmis-
sion, as well as those associated with early death, were analyzed by logistic regression.
Results Hypothermia 5 minutes after birth and at NICU admission was noted in 44% and 51%, respectively, with
6% of early neonatal deaths. Adjusted for confounding variables, practices associated with hypothermia at 5 mi-
nutes after birth were DR temperature <25
C (OR 2.13, 95% CI 1.67-2.28), maternal temperature at delivery
<36.0
C(OR1.93, 95%CI 1.49-2.51), and use of plastic bag/wrap (OR0.53, 95%CI 0.40-0.70). The variables asso-
ciated with hypothermia at NICU admission were DR temperature <25
C (OR 1.44, 95% CI 1.10-1.88), respiratory
support with cold air in the DR (OR 1.40, 95% CI 1.03-1.88) and during transport to NICU (OR 1.51, 95% CI 1.08-
2.13), and cap use (OR 0.55, 95% CI 0.39-0.78). Hypothermia at NICU admission increased the chance of early
neonatal death by 1.64-fold (95% CI 1.03-2.61).
Conclusion Simple interventions, such as maintaining DR temperature >25
C, reducing maternal hypothermia
prior to delivery, providing plastic bags/wraps and caps for the newly born infants, and using warm resuscitation
gases, may decrease hypothermia at NICU admission and improve early neonatal survival. (J Pediatr
2014;164:271-5).
P
reterm infants are susceptible to hypothermia shortly after birth. Laptook et al
1
found that 47% of 5277 very low birth
weight (VLBW) infants had a body temperature <36
C on admission to the neonatal intensive care unit (NICU).
Adjusted analyses showed that admission temperature was inversely related to intrahospital mortality, with a 28% in-
crease in mortality per 1
C decrease in body temperature. Moderate and severe hypothermia were associated with the risk of
death before hospital discharge in a population-based cohort of 8782 VLBW infants in California NICUs in 2006 and 2007.
2
Neither study reported the practices applied to maintain normal body tempera-
ture from birth to NICU admission. According to McCall et al,
3
plastic wraps or
bags and plastic caps are effective in reducing heat losses in infants born at <28-
29 weeks gestation, but it is unclear whether they reduce the risk of death.
The Neonatal Task Force of the International Liaison Committee on Resusci-
tation recommended in 2010 Consensus on Science that newborn infants of <28
weeks gestation should be completely covered in a polythene wrap or bag up to
their necks without drying immediately after birth and then placed under a
radiant heater and resuscitated or stabilized in a standard fashion. Infants should
be kept wrapped until admission and temperature check. Hyperthermia should
be avoided. Delivery room (DR) temperatures should be at least 26
C for infants
of <28 weeks gestation.
4
However, all of these recommendations have lowlevels
of evidence regarding their efcacy and effectiveness in reducing neonatal mor-
tality.
From the
1
Division of Neonatal Medicine, Universidade
Federal de S~ ao Paulo/Escola Paulista de Medicina, S~ ao
Paulo;
2
Department of Pediatrics, Universidade Estadual
de Campinas/Hospital da Mulher Prof. Dr. Jos e
Aristodemo Pinotti, Campinas, SP, Brazil;
3
Department
of Public Health, Universidade Federal do Maranh~ ao/
Hospital Universit ario, S~ ao Lus, MA, Brazil;
4
Department
of Pediatrics, Universidade de S~ ao Paulo/Hospital das
Clnicas de Ribeir~ ao Preto, Ribeir~ ao Preto, SP, Brazil;
5
Department of Pediatrics, Universidade Federal do
Paran a/Hospital de Clnicas, Curitiba;
6
Department of
Pediatrics and Pediatric Surgery, Universidade Estadual
de Londrina/Hospital Universit ario, Londrina, PR, Brazil;
7
Department of Pediatrics, Faculdade de Medicina de
Botucatu da Universidade Estadual Paulista, Botucatu,
SP, Brazil;
8
Department of Pediatrics, Universidade
Federal de Uberl^ andia/Hospital de Clnicas, Uberl^ andia,
MG, Brazil; and
9
Department of Pediatrics, Universidade
Federal do Rio Grande do Sul/Hospital de Clnicas de
Porto Alegre, Porto Alegre, RS, Brazil
*List of members of the Brazilian Network on Neonatal
Research is available at www.jpeds.com (Appendix).
Supported by Conselho Nacional de Desenvolvimento
Cientco e Tecnol ogico (472827-2009-0). The authors
declare no conicts of interest.
0022-3476/$ - see front matter. Copyright 2014 Mosby Inc.
All rights reserved. http://dx.doi.org/10.1016/j.jpeds.2013.09.049
DR Delivery room
NICU Neonatal intensive care unit
VLBW Very low birth weight
271
Our goal is to evaluate intervention practices associated
with hypothermia at 5 minutes after birth and at NICU
admission and to determine whether hypothermia at NICU
admission is associated with early neonatal death in preterm
infants.
Methods
We conducted a multicenter prospective cohort study of in-
fants born at gestational ages of 23
0/7
to 33
6/7
weeks without
congenital anomalies and admitted at 9 centers of the Brazil-
ian Network on Neonatal Research between August 2010 and
April 2012. All of the centers are level III public university
hospitals and serve as referral centers for high-risk pregnan-
cies. All of the hospitals have NICU beds and the staff, equip-
ment, and infrastructure required to treat critically ill
neonates. The study was approved by the institutional review
boards of each institution, and informed consent was signed
by the mother of each enrolled neonate.
At each NICU, 1 neonatologist prospectively collected
maternal and neonatal data in a Web-based data system
specially designed for the study. Gestational age was dened
by the hierarchy of obstetric measures (last menstrual period,
followed by rst trimester ultrasonography) and a neonatal
exam.
5
The centers followed the Neonatal Resuscitation
Program of the Brazilian Pediatric Society guidelines for stabi-
lization and resuscitation at birth according to the Interna-
tional Liaison Committee on Resuscitation Consensus on
Science and Treatment Recommendations.
4,6
All of the centers
used the same types of digital environmental (Term^ ometro
Digital 7665; Incoterm, Porto Alegre, Brazil) and individual
thermometers (Medex; Incoterm, Porto Alegre, Brazil). DR
temperature was registered at birth. Axillary maternal temper-
ature was assessed up to 20 minutes before delivery; axillary
neonatal temperature was measured 5 minutes after birth
and at NICU admission. Both maternal and neonatal hypo-
thermia were dened as a body temperature <36.0
C. The
neonatal thermal care practices analyzed were the following:
use of a plastic bag or wrap; use of a linen or woolen cap;
use of heated gases for ventilation; and use of a transport incu-
bator. Care of all newly born infants was given under radiant
heaters in the DR, and exothermic mattresses were not used.
The main outcomes were hypothermia 5 minutes after
birth, hypothermia at NICU admission, and death by 6
days after birth. Stepwise logistic regression was applied to
evaluate the variables associated with these outcomes. For hy-
pothermia 5 minutes after birth, maternal and neonatal char-
acteristics at birth and variables related to neonatal thermal
care in the DR were considered to be independent variables.
For hypothermia at NICU admission, variables related to
thermal care during transport from the DR to the NICU
were also included. For early neonatal death, maternal and
neonatal characteristics at birth, hypothermia at NICU
admission, and neonatal morbidity were evaluated as inde-
pendent variables. Variables with a value of P <.20 in the uni-
variate analysis were included in the initial model. The tness
of the model was assessed by use of the Hosmer-Lemeshow
test. We calculated that a study population of 1660 patients
would be required to detect a difference of 3% in early
neonatal mortality (exposed, 8%; nonexposed, 5%) consid-
ering a b error of 20%, an a error of 5%, and a ratio of
exposed/nonexposed to hypothermia at NICU admission
of 1:1.
Results
During the study period, 1955 inborn preterm infants with
gestational ages of 23-33 weeks and without congenital
anomalies satised our inclusion criteria, and 1764 (90%)
were enrolled in the study. Enrollment varied from 115 to
262 neonates per center. Axillary temperature at 5 minutes
after birth was measured in 1374 neonates, and hypothermia
was noted in 44% (median 36.0
C; 25th-75th percentiles
35.5
C-36.4
C). Axillary temperature at NICU admission
was measured in 1764 neonates at an average of 32 minutes
after birth, and hypothermia was noted in 51% (median
35.9
C; 25th-75th percentiles 35.3
C-36.4
C).
Hypothermia 5 minutes after birth and at NICU admission
varied among centers from 13% to 62% (P < .001) and from
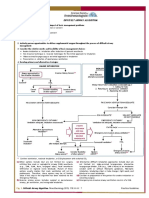
25% to 75% (P < .001), respectively (Figure). Hypothermia
at 5 minutes after birth and at NICU admission was inversely
related to gestational age (P < .001), but 35% of neonates
with gestational ages of 32 and 33 weeks were hypothermic at
5 minutes, and z40% were hypothermic at NICU admission.
Early neonatal death occurred in 6% of the 1764 neonates,
varying among centers between 4% and 9% (P = .478).
Maternal and neonatal characteristics, including thermal
neonatal care practices, in infants with and without
hypothermia at 5 minutes after birth and at NICU
admission are shown in Table I. Median DR temperature
was 24.8
C (25th-75th percentiles 23.7
C-25.8
C); median
maternal axillary temperature was 36.2
C (25th-75th
percentiles 35.8
C-36.6
C; 9 mothers had temperature
$38
C) at an average of 18 minutes prior birth; and
median transport incubator temperature was 36.1
C (25th-
75th percentiles 35.0
C-37.0
C). Among the 1764 neonates,
9 (0.5%) had hyperthermia ($38.0
C) at NICU admission.
DR temperature <25
C, administration of cold air during
positive pressure ventilation, and endotracheal intubation
soon after birth were associated with hypothermia at 5
minutes of life and at NICU admission (Table I). The
following practices were also associated with hypothermia
at NICU admission: absence of cap, transport from DR to
NICU with cold air, and temperature of the transport
incubator <35
C.
Demographic and clinical characteristics of the patients,
according to early neonatal mortality, are shown in
Table II. Male sex, gestational age <28 weeks, birth weight
<1000 g, 1-minute Apgar score <4, 5-minute Apgar score
<7, hypothermia at NICU admission, Neonatal Acute
Physiology, Perinatal Extension, Version II score >40,
respiratory distress syndrome, air leaks, and grades III/IV
THE JOURNAL OF PEDIATRICS www.jpeds.com Vol. 164, No. 2
272 de Almeida et al
intraventricular hemorrhage were more frequent in newborn
infants who died in the rst week after birth.
The independent variables associated with the main out-
comes are shown in Table III. The nal logistic models
were adjusted for birth center. The HosmerLemeshow
goodness-of-t test values for hypothermia at 5 minutes
after birth, hypothermia at NICU admission, and early
neonatal death were 0.959, 0.939, and 0.495, respectively.
Adjusted for confounders, the DR temperature <25
C,
maternal hypothermia, and absence of plastic bag/wrap
were independent risk factors for hypothermia 5 minutes
after birth. In turn, hypothermia 5 minutes after birth was
strongly associated with hypothermia at NICU admission.
Absence of cap use and administration of cold air during
resuscitation and transport were also independent risk
factors for hypothermia at NICU admission. Hypothermia
at NICU admission increased the chance of early neonatal
death by 64%.
Discussion
In this cohort of inborn preterm infants born at 23-33 weeks
of gestational age, the incidence of hypothermia 5 minutes af-
ter birth was extremely high and was independently associ-
ated with low DR temperature, maternal hypertension,
maternal hypothermia, lower gestational age, and lack of
plastic bag/wrap. The presence of hypothermia soon after
birth was the main contributor to hypothermia at NICU
admission, which increased the chance of early neonatal
death by 64%. These results add to the current evidence in
the literature arguing for the urgency of initiating practices
to maintain normothermia as soon as the preterm neonate
is born. These practices include the following: maintenance
of DR temperature >25
C, careful assessment of maternal
temperature, use of a radiant heater in the DR, use of plastic
bag/wrap and cap, respiratory support with humidied and
Figure. Frequency of hypothermia at 5 minutes after birth, hypothermia at NICU admission, and early neonatal death per study
center and per gestational age (number of patients given in parentheses).
Table I. Maternal and neonatal characteristics in infants with and without hypothermia 5 minutes after birth and at
NICU admission
Hypothermia at 5 min Hypothermia at admission
Present
(n = 606)
Absent
(n = 768) P value
Present
(n = 894)
Absent
(n = 870) P value
Maternal age <20 y 21% 19% .253 20% 19% .579
Prenatal care $6 visits 42% 50% .003 40% 49% <.001
Maternal hypertension 42% 30% <.001 40% 27% <.001
Antenatal steroids 74% 68% <.001 71% 66% .004
Multiple gestation 21% 23% .170 20% 25% .006
Spinal anesthesia 71% 70% .447 67% 70% .190
Maternal hypothermia 39% 24% <.001 33% 28% .054
Cesarean delivery 72% 69% .110 70% 68% .627
DR <25
C 63% 47% .001 60% 47% <.001
Male sex 50% 54% .120 52% 53% .719
Gestational age <32 wk 68% 53% <.001 68% 53% <.001
Birth weight <1500 g 71% 50% <.001 70% 50% <.001
Use of plastic bag/wrap 61% 59% .228 54% 55% .564
Use of cap 77% 79% .190 65% 77% <.001
PPV with cold air at DR 58% 48% <.001 57% 46% <.001
Endotracheal intubation 36% 20% <.001 34% 20% <.001
Hypothermia at 5 min - - - 70% 22% <.001
Transport incubator <35
C - - - 25% 20% .025
Transport on O
2
/CPAP/MV - - - 81% 68% <.001
NICU admission >30 min - - - 43% 44% .687
O
2
/CPAP/MV, free-ow oxygen or continuous positive airway pressure or mechanical ventilation; PPV, positive pressure ventilation.
February 2014 ORIGINAL ARTICLES
Hypothermia and Early Neonatal Mortality in Preterm Infants 273
heated gases from birth until NICU admission, and use of
transport incubator with adequate temperature control. It
should be noted that these practices must be considered for
preterm infants with gestational age of 29-33 weeks, because
this study shows a high frequency of hypothermia 5 minutes
after birth and at NICU admission in this group of patients.
Environmental cold temperature has been associated with
higher odds of hypothermia at NICU admission in preterm
infants; however, the ideal DRtemperature is unknown. Kno-
bel et al
7
performed a post-hoc analysis of preterm infants
withgestational age <29 weeks under radiant heaters random-
ized to receive or not receive polyurethane bags and showed
that room temperatures $26
C were associated with higher
admission temperatures in both the intervention and control
groups. According to Jia et al,
8
an increase in the room tem-
perature to an average of 25.1
Cfroma control roomtemper-
ature of 22.5
C was associated with a 0.5
C higher mean
NICU admission rectal temperature and a decrease in the
incidence of hypothermia in preterm infants with gestational
age #32 weeks who were warmed under radiant heaters. The
present study provides further evidence to support the main-
tenance of DRtemperatures at $25
Cbecause the odds of hy-
pothermia at 5 minutes after birth and at NICU admission
were 2.13 and 1.44 times greater, respectively, when the
room temperature was below this threshold.
A newly born infants body temperature is associated with
maternal temperature
9
; in fact, maternal fever and/or hyper-
thermia has been associated with high neonatal body temper-
atures.
10
It is intuitive to assume that maternal hypothermia
would conversely be associated with neonatal hypothermia
soon after birth, but this association has not been demon-
strated consistently. We show that maternal hypothermia
prior to delivery nearly doubles the chance that a newly born
infant will present a body temperature <36
C at 5 minutes af-
ter birth, indicating that maternal thermal care is animportant
measure for the prevention of neonatal hypothermia.
In the present study, the use of a plastic bag/wrap indepen-
dently decreased the chance of hypothermia at 5 minutes after
birth by 47%, and the use of cotton cap decreased the chance
of hypothermia at NICU admission by 45%. A Cochrane Re-
view article
3
indicates that the use of plastic bag or wrap soon
after birth in preterm infants with gestational age <28 weeks
decreases the likelihood of body temperature <36.0
C at
NICU admission by 34% (OR 0.66, 95% CI 0.51%-0.84%).
In the literature, the efcacy of cap use to decrease hypother-
mia in newly born preterm infants is controversial.
3
A ran-
domized clinical trial of 96 preterm infants born at a
gestational age <29 weeks showed similar axillary tempera-
ture at NICU admission when patients under a radiant heater
received only a polyethylene cap (36.1
C 1.4
C) or only a
polyethylene occlusive skin wrapping (35.8
C 1.6
C).
11
A study by the Eunice Kennedy Shriver National Institute of
Child Health and Human Development Neonatal Network
that included 9565 preterm infants born between 22 and 28
weeks gestation showed that 67% required ventilation by
endotracheal tube at birth.
12
Among preterm neonates who
do not need resuscitation, respiratory stabilization with
noninvasive continuous positive airway pressure is increas-
ingly applied in the DR.
13
However, the warming and humid-
ication of inspired gases for invasive and noninvasive
ventilation in neonates are not routine for neonatal resusci-
tation.
14
In the present study, all of the patients who received
any respiratory support in the DRand during transport to the
NICU received cold humidied air. The use of positive pres-
sure ventilation with cold air in the DR and at transport
increased the chance of hypothermia at NICU admission
by 1.40-fold (95% CI 1.03-fold to 1.88-fold) and 1.51-fold
(95% CI 1.08-fold to 2.13-fold), respectively. Te Pas et al
15
Table II. Maternal and neonatal characteristics of
preterm infants according to early neonatal mortality
Early neonatal death
Present
(n = 109)
Absent
(n = 1655) P value
Maternal age <20 y 19% 20% .900
Prenatal care $6 visits 30% 46% .002
Maternal hypertension 38% 34% .398
Peripartum infection 23% 19% .301
Multiple gestation 15% 23% .046
Antenatal steroids 59% 69% .026
Cesarean delivery 62% 69% .127
Male sex 64% 52% .010
Gestational age <28 wk 69% 15% <.001
Birth weight <1000 g 78% 20% <.001
Small for gestational age 35% 28% .141
1-min Apgar score 0-3 53% 19% <.001
5-min Apgar score 0-6 36% 11% <.001
Hypothermia at NICU admission 72% 49% <.001
SNAPPE II >40 64% 10% <.001
Respiratory distress syndrome 88% 57% <.001
Air leaks 18% 4% <.001
Persistent ductus arteriosus 28% 26% .649
Intraventricular hemorrhage III/IV 21% 4% <.001
Culture-proved sepsis 10% 9% .735
Necrotizing enterocolitis 2% 2% .699
SNAPPE II, Score for Neonatal Acute Physiology, Perinatal Extension, Version II.
Table III. Logistic regression analysis for independent
variables associated with the main study outcomes
Outcome OR (95% CI)
Hypothermia 5 min after birth
DR temperature <25
C 2.13 (1.67-2.28)
Gestational age <32 wk 2.01 (1.51-2.68)
Maternal hypertension 2.00 (1.55-2.59)
Maternal temperature at delivery <36
C 1.93 (1.49-2.51)
Use of plastic bag/wrap 0.53 (0.40-0.70)
Hypothermia at NICU admission
Hypothermia 5 min after birth 7.45 (5.70-9.73)
Maternal hypertension 1.77 (1.34-2.33)
Transport on O
2
/CPAP/MV 1.51 (1.08-2.13)
DR temperature <25
C 1.44 (1.10-1.88)
PPV with cold air in the DR 1.40 (1.03-1.88)
Use of cap 0.55 (0.39-0.78)
Early neonatal death
Gestational age <28 wk 7.77 (4.87-12.41)
Respiratory distress syndrome 2.40 (1.28-4.51)
5-min Apgar score 0-6 1.87 (1.17-3.00)
Male sex 1.84 (1.19-2.85)
Hypothermia at NICU admission 1.64 (1.03-2.61)
Antenatal steroids 0.59 (0.38-0.91)
THE JOURNAL OF PEDIATRICS www.jpeds.com Vol. 164, No. 2
274 de Almeida et al
analyzed 2 cohorts of preterm infants born at #32 weeks of
gestational age. In the rst period, respiratory support from
birth to NICU admission was performed with cold air, and
the mean rectal temperature at admission was 35.9
C
0.6
C. In the second period, heated and humidied gas was
introduced for respiratory support, and admission tempera-
ture increased to 36.4
C 0.6
C. These ndings suggest that
the delivery of heated humidied gases in the DR and during
neonatal transport may play an important role in decreasing
the frequency of hypothermia after birth.
The studies that provide evidence of the association be-
tween hypothermia at NICU admission and neonatal mortal-
ity are either retrospective or secondary analyses of data
collected to evaluate other primary outcomes. In a Malaysian
VLBW study group with 868 patients, the chance of hospital
mortality was 1.26 times (95% CI 1.06-1.50 times) greater for
infants with body temperature <36.5
Cat NICUadmission.
16
The Epicure study, which included 811 neonates born at <25
weeks, showed that body temperature <35
Cat NICUadmis-
sion increased the chance of hospital death by 1.72-fold (95%
CI 1.17-fold to 2.56-fold).
17
The chance of death rose 1.28-
fold (95% CI 1.16-fold to 1.41-fold) for each 1
C decrease
in temperature at NICU admission in 5277 VLBW infants
admitted to Eunice Kennedy Shriver National Institute of
Child Health and Human Development Neonatal Network
Centers.
1
Miller et al studied 8782 VLBW infants and found
a 1.5-fold (95% CI 1.3-fold to 1.9-fold) increase in the chance
of hospital death for neonates admitted to the NICU with
body temperature <36
C.
2
Our study, which was prospec-
tively designed to verify an association between early neonatal
mortality and hypothermia at NICU admission, showed that
the chance of early neonatal death is 1.64-fold (1.03-2.61)
higher in infants with admission temperatures <36
C,
adjusted for birth center and for other maternal and neonatal
variables that contribute to early mortality, such as gestational
age, sex, perinatal asphyxia, respiratory distress syndrome,
and the absence of antenatal steroid treatment. However, as
noted by Laptook and Watkinson,
18
it remains unclear
whether hypothermia at NICU admission is a cause of
neonatal mortality or a marker of high patient acuity.
As this was an observational cohort study, the results
shown here reect only associations. However, as a careful
prospective observation of practices applied to thermal care
in the daily routine of the studied DRs, it provides a picture
of the magnitude of the problem and the independent pro-
tective practices that may decrease hypothermia at 5 minutes
after birth and at NICU admission. Simple interventions,
such as maintaining a DR temperature >25
C, reducing
maternal hypothermia prior to delivery, using plastic bags/
wraps and caps for the newly born infants, and using warm
resuscitation gases, may decrease hypothermia at NICU
admission and improve early neonatal survival. n
We thank Olga LC Bomm, MD (Executive Manager of the Brazilian
Network on Neonatal Research; supported by the Ministry of Health of
Brazil [MS/VIGISUS 1755/2000, MS/FNS 274, FIOCRUZ/PDTSP]),
and Cynthia Magluta, MD (Brazilian Network on Neonatal Research
coordinator; Instituto Fernandes Figueira of Fundacao Osvaldo Cruz,
Rio de Janeiro, Brazil), for helping with the logistic management of the
Brazilian Network on Neonatal Research.
Submitted for publication Jun 17, 2013; last revision received Aug 22, 2013;
accepted Sep 20, 2013.
Reprint requests: Ruth Guinsburg, MD, PhD, Rua Vicente Felix 77, apt 09, CEP
01410-020, S~ ao Paulo, SP, Brazil. E-mail: ruthgbr@netpoint.com.br
References
1. Laptook AR, Salhab W, Bhaskar B. Neonatal Research Network. Admis-
sion temperature of low birth weight infants: predictors and associated
morbidities. Pediatrics 2007;119:e643-9.
2. Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight in-
fants: distribution, risk factors and outcomes. J Perinatol 2011;31(Suppl
1):S49-56.
3. McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S. Interven-
tions to prevent hypothermia at birth in preterm and/or low birthweight
infants. Cochrane Database Syst Rev 2010;CD004210.
4. Perlman JM, Wyllie J, Kattwinkel J, Atkins DL, Chameides L,
Goldsmith JP, et al. Part 11: neonatal resuscitation: 2010 International
consensus on cardiopulmonary resuscitation and emergency cardiovas-
cular care science with treatment recommendations. Circulation 2010;
122(16 Suppl 2):S516-38.
5. Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R.
New Ballard Score, expanded to include extremely premature infants.
J Pediatr 1991;119:417-23.
6. The International Liaison Committee on Resuscitation. The Interna-
tional Liaison Committee on Resuscitation (ILCOR)consensus on sci-
ence with treatment recommendations for pediatric and neonatal
patients: neonatal resuscitation. Pediatrics 2006;117:e978-88.
7. Knobel RB, Wimmer JE Jr, Holbert D. Heat loss prevention for preterm
infants in the delivery room. J Perinatol 2005;25:304-8.
8. Jia YS, Lin ZL, Lv H, Li YM, Green R, Lin J. Effect of delivery room tem-
perature on the admission temperature of premature infants: a random-
ized controlled trial. J Perinatol 2013;33:264-7.
9. Lunze K, Bloom DE, Jamison DT, Hamer DH. The global burden of
neonatal hypothermia: systematic review of a major challenge for
newborn survival. BMC Med 2013;11:24.
10. Perlman JM. Hyperthermia in the delivery: potential impact on neonatal
mortality and morbidity. Clin Perinatol 2006;33:55-63.
11. Trevisanuto D, Doglioni N, Cavallin F, Parotto M, Micaglio M,
Zanardo V. Heat loss prevention in very preterm infants in delivery
rooms: a prospective, randomized, controlled trial of polyethylene
caps. J Pediatr 2010;156:914-7.
12. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al.
Neonatal outcomes of extremely preterm infants from the NICHD
Neonatal Research Network. Pediatrics 2010;126:443-56.
13. Pster RH, Soll RF. Initial respiratory support of preterm infants: the
role of CPAP, the INSURE method, and noninvasive ventilation. Clin
Perinatol 2012;39:459-81.
14. Farley RC, Gibbons K, Jardine LA, Shearman AD. Effect of ow rate, hu-
midier dome and water volume on maximising heated, humidied gas
use for neonatal resuscitation. Resuscitation 2013;84:1428-32.
15. te Pas AB, Lopriore E, Dito I, Morley CJ, Walther FJ. Humidied and
heated air during stabilization at birth improves temperature in preterm
infants. Pediatrics 2010;125:e1427-32.
16. MalaysianVery LowBirthWeight Study Group. Anational study of risk fac-
tors associated with mortality in very lowbirth weight infants in the Malay-
sian neonatal intensive care units. J Paediatr Child Health 1997;33:18-25.
17. Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR. The
EPICure study: outcomes to discharge from hospital for infants born
at the threshold of viability. Pediatrics 2000;106:659-71.
18. Laptook AR, Watkinson M. Temperature management in the delivery
room. Semin Fetal Neonatal Med 2008;13:383-91.
February 2014 ORIGINAL ARTICLES
Hypothermia and Early Neonatal Mortality in Preterm Infants 275
Appendix
Additional members of the Brazilian Network on Neonatal
Research include:
Universidade Estadual de Campinas/Hospital da Mulher
Prof. Dr. Jose Aristodemo Pinotti: Sergio Tadeu Martins
Marba, MD, PhD, Ana Cristina Pinto, MD, Andrea Eliana
Lovato Cassone, MD, Jamil Pedro de Siqueira Caldas, MD,
PhD; Universidade Federal do Maranh~ao/Hospital Univer-
sitario: Marynea do Vale Nunes, MD, Ana Claudia Garcia
Marques, MD; Universidade de S~ao Paulo/Hospital das
Clnicas de Ribeir~ao Preto: Ana Beatriz Goncalves, MD, Wa-
lusa Assad Goncalves Ferri, MD, PhD; Universidade Federal
do Parana/Hospital de Clnicas: Paulyne Stadler Venzon,
MD; Universidade Estadual de Londrina/Hospital Univer-
sitario: Angela Sara Jamusse de Brito, MD, Ana Berenice Ri-
beiro Carvalho, MD, Maria Rafaela Conde Gonzalez, MD;
Faculdade de Medicina de Botucatu da Universidade Estad-
ual Paulista: Maria Regina Bentlin, MD, PhD, Glauce Regina
Fernandes Giacoia, MD; Universidade Federal de Uberl^an-
dia/Hospital de Clnicas: Daniela Marques de Lima Mota
Ferreira, MD, Helosio dos Reis, MD; Universidade Federal
do Rio Grande do Sul/Hospital de Clnicas de Porto Alegre:
Renato S Procianoy, MD, PhD.
THE JOURNAL OF PEDIATRICS www.jpeds.com Vol. 164, No. 2
275.e1 de Almeida et al
Vous aimerez peut-être aussi
- Hypothermia and Early Neonatal Mortality in Preterm InfantsDocument6 pagesHypothermia and Early Neonatal Mortality in Preterm InfantskemalmiaPas encore d'évaluation
- Hypothermie NigeriaDocument5 pagesHypothermie NigeriaMadina NacroPas encore d'évaluation
- Hypothermia in Very Low Birth Weight InfantsDocument9 pagesHypothermia in Very Low Birth Weight InfantsGiovanni MictilPas encore d'évaluation
- Jurding HieDocument8 pagesJurding HieSiska SulistiyowatiPas encore d'évaluation
- JournalDocument7 pagesJournalFaris LahmadiPas encore d'évaluation
- The The TheDocument47 pagesThe The TheTarus El AzizzPas encore d'évaluation
- The Effect of Coverings, Including Plastic Bags and Wraps, On Mortality and Morbidity in Preterm and Full-Term NeonatesDocument7 pagesThe Effect of Coverings, Including Plastic Bags and Wraps, On Mortality and Morbidity in Preterm and Full-Term NeonatesSherli Prima SHedPas encore d'évaluation
- Trasitional Hypothermia PDFDocument3 pagesTrasitional Hypothermia PDFDella Putri Ariyani NasutionPas encore d'évaluation
- Expectant Versus Aggressive Management in Severe Preeclampsia Remote From TermDocument6 pagesExpectant Versus Aggressive Management in Severe Preeclampsia Remote From Termmiss.JEJEPas encore d'évaluation
- Impact On Delayed Newborn Bathing On Exclusive Breastfeed - 2019 - Journal of NeDocument6 pagesImpact On Delayed Newborn Bathing On Exclusive Breastfeed - 2019 - Journal of NeCarol HPas encore d'évaluation
- Trevisan U To 2018Document7 pagesTrevisan U To 2018linamaria.pedPas encore d'évaluation
- Randomized Trial of Plastic Bags To Prevent TermDocument8 pagesRandomized Trial of Plastic Bags To Prevent TermkemalmiaPas encore d'évaluation
- Journal Pone 0248838Document11 pagesJournal Pone 0248838helentika AvianaPas encore d'évaluation
- Intervenção Sobre Hipotermia NeonatalDocument13 pagesIntervenção Sobre Hipotermia NeonatalAna PaulaPas encore d'évaluation
- Preterm Premature Rupture of Membranes in The Presence of Cerclage: Is The Risk For Intra-Uterine Infection and Adverse Neonatal Outcome Increased?Document6 pagesPreterm Premature Rupture of Membranes in The Presence of Cerclage: Is The Risk For Intra-Uterine Infection and Adverse Neonatal Outcome Increased?stephaniedianPas encore d'évaluation
- Lead Ford 2013Document9 pagesLead Ford 2013AnnidaulfhPas encore d'évaluation
- Fetal Inflamatory Response SyndromeDocument9 pagesFetal Inflamatory Response SyndromeAnonymous mvNUtwidPas encore d'évaluation
- Chorioamnionitis and Prognosis For Term Infants-13Document5 pagesChorioamnionitis and Prognosis For Term Infants-13ronny29Pas encore d'évaluation
- Mi2018 2845352 PDFDocument5 pagesMi2018 2845352 PDFDewi LarasatiPas encore d'évaluation
- Tercer Articulo IsaDocument4 pagesTercer Articulo IsaIsabel Cristina Castro SernaPas encore d'évaluation
- Insidence of Fever in Labor and Risk of Neonatal SepsisDocument5 pagesInsidence of Fever in Labor and Risk of Neonatal SepsisSNFauziaPas encore d'évaluation
- Clinical Profile and Predictors of Severe Illness in Young South African Infants ( 60 Days)Document6 pagesClinical Profile and Predictors of Severe Illness in Young South African Infants ( 60 Days)Sunu RachmatPas encore d'évaluation
- Hypoglycemia and Associated Comorbidities Among Newborns of Mothers With Diabetes in An Academic Tertiary Care CenterDocument15 pagesHypoglycemia and Associated Comorbidities Among Newborns of Mothers With Diabetes in An Academic Tertiary Care CenterrimzeenafeeshaPas encore d'évaluation
- The NeoUpdates - DecDocument7 pagesThe NeoUpdates - DecDr Satish MishraPas encore d'évaluation
- Pediatrics 2011Document9 pagesPediatrics 2011Rizky Amalia PutriPas encore d'évaluation
- Mat FeverDocument11 pagesMat FeverewiPas encore d'évaluation
- Bowling Nur3206 dl2 Root CauseDocument7 pagesBowling Nur3206 dl2 Root Causeapi-349455792Pas encore d'évaluation
- AsdasfasfvDocument7 pagesAsdasfasfvPulseWangminPas encore d'évaluation
- Comparison of Effectiveness of Two Polyethylene Covers On Body Temperature and Oxygen Saturation of Neonates Transferring To NicusDocument8 pagesComparison of Effectiveness of Two Polyethylene Covers On Body Temperature and Oxygen Saturation of Neonates Transferring To NicusOzy FerdPas encore d'évaluation
- Jean-Charles Pasquier, Olivier Claris, Muriel Rabilloud, René Ecochard, Jean-Charles Picaud, Stéphanie Moret, Danielle Buch, Georges MellierDocument8 pagesJean-Charles Pasquier, Olivier Claris, Muriel Rabilloud, René Ecochard, Jean-Charles Picaud, Stéphanie Moret, Danielle Buch, Georges Mellierclara giovaniPas encore d'évaluation
- Clinical Risk Index For Babies (Crib) Ii Score As A Predictor of Neonatal Mortality Among Low Birth Weight Babies at Kenyatta National HospitalDocument6 pagesClinical Risk Index For Babies (Crib) Ii Score As A Predictor of Neonatal Mortality Among Low Birth Weight Babies at Kenyatta National HospitalVladBadeaPas encore d'évaluation
- Sensitivity of Histological Chorioaminionitis and Premature Rupture of Membranes For Neonatal Sepsis and Its Risk FactorsDocument6 pagesSensitivity of Histological Chorioaminionitis and Premature Rupture of Membranes For Neonatal Sepsis and Its Risk Factorsizza istqmhPas encore d'évaluation
- Zapata 2003Document8 pagesZapata 2003Luis RodriguezPas encore d'évaluation
- Clinical Pathway Effectiveness: Riginal RticleDocument5 pagesClinical Pathway Effectiveness: Riginal RticleWynda NolaPas encore d'évaluation
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- 'Kangaroo Mother Care' To Prevent Neonatal Deaths Due To Preterm Birth ComplicationsDocument11 pages'Kangaroo Mother Care' To Prevent Neonatal Deaths Due To Preterm Birth ComplicationsLuzdelpilar RcPas encore d'évaluation
- Short-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalıDocument6 pagesShort-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalızulfikarPas encore d'évaluation
- 942pm - 25.EPRA JOURNALS-4957Document5 pages942pm - 25.EPRA JOURNALS-4957Anu SharmaPas encore d'évaluation
- Pengaruh Metode Kanguru Terhadap Stabilitis Suhu Tubuh Bayi Di Ruang Perinatologi Rumah Sakit Umum Daerah BengkalisDocument8 pagesPengaruh Metode Kanguru Terhadap Stabilitis Suhu Tubuh Bayi Di Ruang Perinatologi Rumah Sakit Umum Daerah BengkalisLaila AzizahPas encore d'évaluation
- Jurnal NH 1Document4 pagesJurnal NH 1Shintya DewiPas encore d'évaluation
- Jurnal B.inggris AnakDocument14 pagesJurnal B.inggris AnakLuciana LorenzaPas encore d'évaluation
- Fowke Projectpaper Summative 071913Document8 pagesFowke Projectpaper Summative 071913api-242279035Pas encore d'évaluation
- The Timing of Physiologic Maturation of PrematureDocument11 pagesThe Timing of Physiologic Maturation of Prematureminerva_stanciuPas encore d'évaluation
- Medication Errors in A Neonatal Intensive Care Unit: Riginal RticleDocument5 pagesMedication Errors in A Neonatal Intensive Care Unit: Riginal Rticlesuresh151971Pas encore d'évaluation
- Effect of SSCDocument7 pagesEffect of SSCgarethPas encore d'évaluation
- ILIE RO PHD Thesis AbstractDocument13 pagesILIE RO PHD Thesis AbstractAnonymous eson90Pas encore d'évaluation
- 1642 Full PDFDocument5 pages1642 Full PDFAriana FlemingPas encore d'évaluation
- (Temperature) Hypothermia Detection in LBWN Using Novel BraceletDocument9 pages(Temperature) Hypothermia Detection in LBWN Using Novel BraceletAnonymous KiraPas encore d'évaluation
- 37004-Article Text-130842-2-10-20180629Document5 pages37004-Article Text-130842-2-10-20180629nishita biswasPas encore d'évaluation
- A Cohort Study of The Impact of Epidural Analgesia On Maternal and Neonatal OutcomesDocument7 pagesA Cohort Study of The Impact of Epidural Analgesia On Maternal and Neonatal OutcomesHadad Setiawan FachrulPas encore d'évaluation
- Khair-Un-Nisa FormattedDocument4 pagesKhair-Un-Nisa FormattedMominah MayamPas encore d'évaluation
- Thermal BlanketDocument7 pagesThermal BlanketMega PuspitaPas encore d'évaluation
- Correspondence: Therapeutic Hypothermia For Birth Asphyxia in Low-Resource Settings: A Pilot Randomised Controlled TrialDocument3 pagesCorrespondence: Therapeutic Hypothermia For Birth Asphyxia in Low-Resource Settings: A Pilot Randomised Controlled TrialAlia SalviraPas encore d'évaluation
- Ni Hms 448407Document14 pagesNi Hms 448407Patrick RamosPas encore d'évaluation
- Scopus (29) Many2017Document7 pagesScopus (29) Many2017ika puspitaPas encore d'évaluation
- Jurnal Kangoroo Method CareDocument7 pagesJurnal Kangoroo Method CareShinta Andi SarasatiPas encore d'évaluation
- Admission of Term Infants To The NicuDocument6 pagesAdmission of Term Infants To The NicucarlsonrenovatioPas encore d'évaluation
- Omj D 09 00101Document6 pagesOmj D 09 00101DewinsPas encore d'évaluation
- Medical Microbiology for the New Curriculum: A Case-Based ApproachD'EverandMedical Microbiology for the New Curriculum: A Case-Based ApproachPas encore d'évaluation
- Pulmonary ThromboembolismDocument61 pagesPulmonary ThromboembolismsanjivdasPas encore d'évaluation
- NCLEX OB Peds 2 of 3 - 947 TermsDocument243 pagesNCLEX OB Peds 2 of 3 - 947 TermsCharaPas encore d'évaluation
- Dwnload Full The Ophthalmic Assistant e Book A Text For Allied and Associated Ophthalmic Personnel PDFDocument51 pagesDwnload Full The Ophthalmic Assistant e Book A Text For Allied and Associated Ophthalmic Personnel PDFebony.blanchard21195% (22)
- 3D Prints Are Not A Panacea, But Definitely SupportDocument4 pages3D Prints Are Not A Panacea, But Definitely SupportYAKESH KARTHIKEYAN BPas encore d'évaluation
- Diagnostic LaparosDocument58 pagesDiagnostic LaparosJaka SembungPas encore d'évaluation
- Special Articles: Awake Intubation Intubation After Induction of General AnesthesiaDocument1 pageSpecial Articles: Awake Intubation Intubation After Induction of General AnesthesiaOKE channelPas encore d'évaluation
- ENT EEE by Dr. Manisha Budhiraja 5th Edition - UnlockedDocument448 pagesENT EEE by Dr. Manisha Budhiraja 5th Edition - UnlockedArbin PanjaPas encore d'évaluation
- Chapter 1Document2 pagesChapter 1longaitiPas encore d'évaluation
- Jonelta Foundation School of Medicine: University of Perpetual Help System DaltaDocument5 pagesJonelta Foundation School of Medicine: University of Perpetual Help System DaltaMark Joshua CervantesPas encore d'évaluation
- Nonsurgical Rhinoplasty: A Realself Social Media AnalysisDocument4 pagesNonsurgical Rhinoplasty: A Realself Social Media AnalysisFemale calmPas encore d'évaluation
- Osteoarthritis Malaysian CPG 2013Document25 pagesOsteoarthritis Malaysian CPG 2013aideeh3110100% (1)
- A Randomized Trial Comparing 2 Doses of Polidocanol Sclerotherapy For Hydrocele or SpermatoceleDocument5 pagesA Randomized Trial Comparing 2 Doses of Polidocanol Sclerotherapy For Hydrocele or SpermatoceleproluvieslacusPas encore d'évaluation
- Wound Healing: Dr. Shaimaa Alaraby Specialist of General SurgeryDocument21 pagesWound Healing: Dr. Shaimaa Alaraby Specialist of General SurgeryOsama Fadel ahmedPas encore d'évaluation
- Hernias: Daniel IgoDocument46 pagesHernias: Daniel Igobigboss80s100% (1)
- Precedex Delirium Spine - AA2023Document9 pagesPrecedex Delirium Spine - AA2023Ahida VelazquezPas encore d'évaluation
- Treatment of Anal Stenosis A 5year Revie PDFDocument3 pagesTreatment of Anal Stenosis A 5year Revie PDFJimi Kalvin SarareniPas encore d'évaluation
- BSC Nursing: Medical Surgical Nursing Unit V - Disorders of The Cardio Vascular SystemDocument34 pagesBSC Nursing: Medical Surgical Nursing Unit V - Disorders of The Cardio Vascular SystemPoova Ragavan100% (1)
- RizkyMayoHutama 22010110130195 Bab8KTI PDFDocument32 pagesRizkyMayoHutama 22010110130195 Bab8KTI PDFAldi VizehPas encore d'évaluation
- MCN Lec M1L3A ReviewerDocument10 pagesMCN Lec M1L3A ReviewerEmily BernatPas encore d'évaluation
- MedCosmos Surgery - History TakingDocument18 pagesMedCosmos Surgery - History TakingEmmanuel DanielsPas encore d'évaluation
- 2010 December TUS Exam - Clinical Sciences - TUS QuestionsDocument25 pages2010 December TUS Exam - Clinical Sciences - TUS QuestionsAzzim El KanzyPas encore d'évaluation
- Elastomeric Impression TechniquesDocument60 pagesElastomeric Impression TechniquesAnupriya SinghPas encore d'évaluation
- 09 Catastrophe Cover 2011 5.1Document2 pages09 Catastrophe Cover 2011 5.1Tufha NiwaPas encore d'évaluation
- PeritonitisDocument36 pagesPeritonitisbrnardPas encore d'évaluation
- Daftar Obat High Alert Dan High Risk: Instalasi Farmasi Rumah Sakit Baptis BatuDocument2 pagesDaftar Obat High Alert Dan High Risk: Instalasi Farmasi Rumah Sakit Baptis BatudindaPas encore d'évaluation
- Peripheral Arterial DiseaseDocument32 pagesPeripheral Arterial DiseaseNiko YuandikaPas encore d'évaluation
- TOPIC E Principles of BioethicsDocument12 pagesTOPIC E Principles of BioethicsblairePas encore d'évaluation
- Anatomy & Physiology of Anal Canal: Dr. Nadan KandelDocument29 pagesAnatomy & Physiology of Anal Canal: Dr. Nadan Kandelजीवनशैलीव्यवस्थापनकार्यक्रम रवि पाँचथरPas encore d'évaluation
- Falso Tendão No VE e Repolarização VentricularDocument1 pageFalso Tendão No VE e Repolarização VentricularNITACORDEIROPas encore d'évaluation
- Ix - (Revised) Med Cert ValidationDocument5 pagesIx - (Revised) Med Cert ValidationAlvin Xtian NucumPas encore d'évaluation