Académique Documents
Professionnel Documents
Culture Documents
Copd
Transféré par
KC Palattao0 évaluation0% ont trouvé ce document utile (0 vote)
14 vues3 pagesclinical pharmacy
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentclinical pharmacy
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
14 vues3 pagesCopd
Transféré par
KC Palattaoclinical pharmacy
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 3
PATHOPHYSIOLOGY OF ASTHMA
characterized by fluctuating airways obstruction, with diurnal variation and nocturnal
exacerbations.
SS: the triad of wheeze, cough and breathlessness.
due to a combination of constriction of bronchial smooth muscle, edema of the mucosa lining
the small bronchi, and plugging of the bronchial lumen with viscous mucus and inflammatory
cells
categorized into non-allergic and allergic, but there is considerable overlap.
In allergic asthma, which is usually of early onset, extrinsic allergens produce a type I allergic
reaction in atopic subjects. Type I reactions are triggered via reaginic antibodies (IgE) ,
eosinophils.
Patients with non-allergic (late-onset) asthma do not appear to be sensitive to any single well-
defined antigen, although infection (usually viral) often precipitates an attack.
Inflammatory mediators implicated in asthma include histamine, several leukotrienes (LTC4/D4
and E4) 5-hydroxytrypta- mine (serotonin), prostaglandin D2, platelet-activating factor (PAF),
neuropeptides and tachykinins.
Adrenaline:anticholinergic:muscarinic: bronchoconstriction.
Ach:B receptors:bronchodilation
COPD
Acute exacerbation
Controlled oxygen therapy (e.g. FiO2 2428%);
Nebulized 2-agonists (salbutamol every 24 hours, if needed) or intravenously if refractory;
Nebulized anticholinergics, such as ipratropium bromide;
Antibiotics (e.g. clarithromycin, co-amoxiclav, levofloxacin).
Short-term oral prednisolone.
Chronic disease
Stop smoking cigarettes.
Optimize inhaled bronchodilators (salbutamol/ipratropium bromide) and their administration.
Consider oral theophylline and/or inhaled glucocorticosteroids.
Treat infection early and aggressively with antibiotics.
Offer long-term oxygen therapy (LTOT) for at least 15 hours per day for cor pulmonale.
Diuretics should be used for peripheral oedema.
Consider venesection for severe secondary polycythaemia.
Exercise, within limits of tolerance.
Terbutaline similar to salbutamol
Salmeterol: prophylaxis to exercised induced asthma
Bronchodilator agents
2-Agonists.
Bronchodilate by increasing intracellular cAMP.
Short-acting, rapid-onset agents (e.g. salbutamol) are used as needed to relieve bronchospasm in
asthma.
Long-acting, slower-onset agents (e.g. salmeterol) are used regularly twice daily.
Common side effects include tremor, tachycardias, vasodilatation, hypokalaemia and hyperglycaemia.
Anticholinergics
Antagonist at M2 and M3 muscarinic receptors in the bronchi, causing bronchodilatation.
Slow onset of long-lasting bronchodilatation (given six- to eight-hourly), especially in older patients.
Bitter taste.
Anti-inflammatory agents cromoglicate and glucocorticosteroids
Sodium cromoglicate
Its mechanism of action is unclear. It has an anti- inflammatory effect.
Largely superseded in chronic prophylactic therapy of allergic asthma by glucocorticosteroids.
Prevents exercise-induced asthma.
Inhaled therapy is administered via metered-dose inhaler or dry powder.
Side-effects are minimal (headache, cough).
Its use is very safe in children.
Glucocorticosteroids
Mechanism is anti-inflammatory.
They are administered systemically (i.v./p.o.) in severe acute and chronic asthma.
They are inhaled topically or nebulized in chronic asthma.
Glucocorticosteroids are well absorbed from the gastro- intestinal tracthepatic (CYP3A) metabolism.
Dosing is once daily for oral glucocorticosteroids and twice daily for inhaled agents.
Side effects are minimal with topical therapy (oral thrush, hoarse voice, HPA suppression only at high
dose).
Side effects with systemic therapy are the features of Cushings syndrome.
Leukotriene modulation in asthma
Leukotriene B4 is a powerful chemo-attractant (eosinophils and neutrophils) and increases vascular
permeability producing mucosal oedema.
Leukotrienes C4, D4 and E4 (cysteinyl leukotrienes) are potent spasmogens and pro-inflammatory
substances (SRS-A).
Clinically used agents that modulate leukotrienes are leukotriene antagonists (which antagonize
cysteinyl leukotrienes LTD4, LTC4 at the Cys-LT1 receptor)
Leukotriene antagonists (e.g. montelukast) are effective as oral maintenance therapy in chronic
persistent asthma. Montelukast has antiinflammatory properties and is a mild, slow-onset
bronchodilator.
Accolate (zafirlukast) is a leukotriene modifier and is used for the prophylaxis and chronic treatment
of asthma
Adverse Effects of Theophylline:
- Dose related acute toxicities include: tachycardia, nausea and vomiting, tachyarrhythmias
(SVT), central nervous system stimulation, headache, seizures, hematemesis, hyperglycemia, and
hypokalemia.
- Adverse effects at usual therapeutic doses: insomnia, gastric upset, aggravation of ulcer or
reflux, increase in hyperactivity in some children, and difficulty in urination in elderly males with
prostatism.
Respiratory failure
Type I (hypocapnic hypoxaemia) and type II (hypercapnic hypoxaemia).
Therapy for type I is supportive with high-percentage oxygen (FiO2 4060%).
Therapy for type II is low-percentage oxygen (FiO2 2428%) and treatment of reversible factors
infection and bronchospasm (with antibiotics, bronchodilators and glucocorticosteroids).
Type I or type II respiratory failure may necessitate mechanical ventilation.
Central nervous system (CNS)-depressant drugs (e.g. opiates, benzodiazepines) may exacerbate or
precipitate respiratory failure, usually type II.
Sedatives are absolutely contraindicated (unless the patient is already undergoing mechanical
ventilation).
FVC: Forced Vital Capacity - This is the total amount of air that you can forcibly blow out after full
inspiration, measured in liters.
FEV
1
: Forced Expiratory Volume in 1 Second - This is the amount of air that you can forcibly blow out in
one second, measured in liters. Along with FVC it is considered one of the primary indicators of lung
function.
FEV
1
/ FVC - This is the ratio of FEV 1 and FVC, which showing the amount of the FVC that can be
expelled in one second. In healthy adults this should be approximately 80%.
PEF: Peak Expiratory Flow - This is the speed of the air moving out of your lungs at the beginning of the
expiration, measured in liters per second.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Cherokee Herbal RemediesDocument292 pagesCherokee Herbal RemediesAlek Phabiovsky100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Rxprep TablesDocument73 pagesRxprep Tablessexiilexie00796% (49)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Types of AgarDocument12 pagesTypes of AgarRoyle LolingPas encore d'évaluation
- BANERJEE P Materia Medica of Indian DrugsDocument133 pagesBANERJEE P Materia Medica of Indian DrugsRipudaman Mahajan89% (9)
- Portfolio Template for Diploma in Occupational MedicineDocument11 pagesPortfolio Template for Diploma in Occupational MedicineChengyuan ZhangPas encore d'évaluation
- Analytical Method Validation of Clopidogrel Tablets BR HPLCDocument48 pagesAnalytical Method Validation of Clopidogrel Tablets BR HPLCAman ThakurPas encore d'évaluation
- Respiratory System Disorders (Asthma & COPD ..)Document5 pagesRespiratory System Disorders (Asthma & COPD ..)KC PalattaoPas encore d'évaluation
- Respiratory System Disorders (Asthma & COPD ..)Document5 pagesRespiratory System Disorders (Asthma & COPD ..)KC PalattaoPas encore d'évaluation
- Lecture 11 Anticancer & Immunomodulators.Document14 pagesLecture 11 Anticancer & Immunomodulators.KC Palattao100% (1)
- Lecture 15 Other TherapiesDocument10 pagesLecture 15 Other TherapiesKC PalattaoPas encore d'évaluation
- Antibiotics &anti-Infective AgentsDocument39 pagesAntibiotics &anti-Infective AgentsKC PalattaoPas encore d'évaluation
- Lecture 9 Endocrine HormonesDocument18 pagesLecture 9 Endocrine HormonesKC PalattaoPas encore d'évaluation
- Lecture 12 GIT & Anti-Emetic DrugsDocument10 pagesLecture 12 GIT & Anti-Emetic DrugsKC PalattaoPas encore d'évaluation
- Autonomic Nervous SystemDocument17 pagesAutonomic Nervous SystemKC PalattaoPas encore d'évaluation
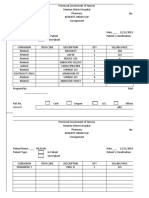
- Ss Coupon Slip Ss Coupon Slip Ss Coupon Slip: Mauban District Hospital Mauban District Hospital Mauban District HospitalDocument1 pageSs Coupon Slip Ss Coupon Slip Ss Coupon Slip: Mauban District Hospital Mauban District Hospital Mauban District HospitalKC PalattaoPas encore d'évaluation
- Organic chemistry lectureDocument16 pagesOrganic chemistry lectureKC PalattaoPas encore d'évaluation
- Philippines FDA course registrationDocument2 pagesPhilippines FDA course registrationKC PalattaoPas encore d'évaluation
- General Physiology: APEC Exam Study NotesDocument9 pagesGeneral Physiology: APEC Exam Study NotesKC PalattaoPas encore d'évaluation
- Lecture 3 PharmaceuticsDocument31 pagesLecture 3 PharmaceuticsKC PalattaoPas encore d'évaluation
- Cell Wall SynthesisDocument7 pagesCell Wall SynthesisKC PalattaoPas encore d'évaluation
- Pos-Fola 70Document28 pagesPos-Fola 70KC PalattaoPas encore d'évaluation
- Employee shift change request form Mauban District Hospital pharmacyDocument1 pageEmployee shift change request form Mauban District Hospital pharmacyKC PalattaoPas encore d'évaluation
- Mauban District Hospital Supplies LedgerDocument1 pageMauban District Hospital Supplies LedgerKC PalattaoPas encore d'évaluation
- ReviewerDocument20 pagesReviewerKC PalattaoPas encore d'évaluation
- PHIC SlipDocument1 pagePHIC SlipKC PalattaoPas encore d'évaluation
- Request For PaymentDocument1 pageRequest For PaymentKC Palattao100% (1)
- Accp Clinical Pharmacy ChalleDocument6 pagesAccp Clinical Pharmacy ChalleKC PalattaoPas encore d'évaluation
- Promissory Note Promissory Note: Mauban District Hospital Mauban District HospitalDocument2 pagesPromissory Note Promissory Note: Mauban District Hospital Mauban District HospitalKC PalattaoPas encore d'évaluation
- Pos-Fola 68Document28 pagesPos-Fola 68KC PalattaoPas encore d'évaluation
- Maximum dose of Donepizil and other Alzheimer recallsDocument111 pagesMaximum dose of Donepizil and other Alzheimer recallsKC PalattaoPas encore d'évaluation
- Accp Clinical Pharmacy ChalleDocument6 pagesAccp Clinical Pharmacy ChalleKC PalattaoPas encore d'évaluation
- SpiriDocument12 pagesSpiriKC PalattaoPas encore d'évaluation
- BiblioDocument4 pagesBiblioKC PalattaoPas encore d'évaluation
- Iryu.4 Team - Medical.Dragon.E09.720p.Web ENGDocument45 pagesIryu.4 Team - Medical.Dragon.E09.720p.Web ENGcintoyPas encore d'évaluation
- RAV Admission Notice for Ayurveda CoursesDocument4 pagesRAV Admission Notice for Ayurveda CoursesBhargav KalalPas encore d'évaluation
- Integrating Modern Dermatology and AyurvedaDocument25 pagesIntegrating Modern Dermatology and AyurvedachandusgPas encore d'évaluation
- Wallen Et Al-2006-Australian Occupational Therapy JournalDocument1 pageWallen Et Al-2006-Australian Occupational Therapy Journal胡知行Pas encore d'évaluation
- Kinesiology Elbow Joint PDFDocument8 pagesKinesiology Elbow Joint PDFRozyPas encore d'évaluation
- The LungsDocument6 pagesThe LungsnandaPas encore d'évaluation
- Aa 1 MasterRQsDocument93 pagesAa 1 MasterRQsSadhana SabhandasaniPas encore d'évaluation
- Europe PMC study finds computerized ADHD test improves diagnostic accuracyDocument22 pagesEurope PMC study finds computerized ADHD test improves diagnostic accuracyBudi RahardjoPas encore d'évaluation
- HSPK 2021Document270 pagesHSPK 2021Sabrina Agustien SimanungkalitPas encore d'évaluation
- Wave One Brochure 0Document18 pagesWave One Brochure 0Shivendra Nath TripathiPas encore d'évaluation
- Pharmaceutical Development and Compatibility Studies On Cytarabine InjectionDocument4 pagesPharmaceutical Development and Compatibility Studies On Cytarabine InjectionAmit KhuntPas encore d'évaluation
- Modified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeDocument4 pagesModified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeChepe LemusPas encore d'évaluation
- Diatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDocument13 pagesDiatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDani Daniela100% (1)
- Basic Principles of Pediatric Mechanical VentilationDocument39 pagesBasic Principles of Pediatric Mechanical VentilationNav KovPas encore d'évaluation
- LMA Fast TrackDocument2 pagesLMA Fast TrackLeandro AlmeidaPas encore d'évaluation
- Masterlist SummaryDocument6 pagesMasterlist Summarykentclark03Pas encore d'évaluation
- Raising Dengue Awareness in the PhilippinesDocument4 pagesRaising Dengue Awareness in the PhilippinesAlyssa Hazza Membrano MayonadoPas encore d'évaluation
- Gardens For Patients With Alzheimer's DiseaseDocument3 pagesGardens For Patients With Alzheimer's DiseaseKritikou1547Pas encore d'évaluation
- Diagnostic Imaging Equipment & Consumables Laser PrintersDocument5 pagesDiagnostic Imaging Equipment & Consumables Laser Printersnanu_gomezPas encore d'évaluation
- A Review On Acacia Arabica - An Indian Medicinal Plant: IJPSR (2012), Vol. 3, Issue 07 (Review Article)Document11 pagesA Review On Acacia Arabica - An Indian Medicinal Plant: IJPSR (2012), Vol. 3, Issue 07 (Review Article)amit chavanPas encore d'évaluation
- Laughter Discussion TopicDocument3 pagesLaughter Discussion Topicjelenap221219950% (1)
- Psychological Point of ViewDocument3 pagesPsychological Point of ViewForam PatelPas encore d'évaluation
- References Style and Writing GuideDocument23 pagesReferences Style and Writing GuideHarshal SabanePas encore d'évaluation
- CCMP 2020 Batch Cardiovascular MCQsDocument2 pagesCCMP 2020 Batch Cardiovascular MCQsharshad patelPas encore d'évaluation
- Essential and Non-Essential Fatty Acids PDFDocument4 pagesEssential and Non-Essential Fatty Acids PDFBj Delacruz100% (2)
- Pivas 2018Document46 pagesPivas 2018Denny PaatPas encore d'évaluation