Académique Documents
Professionnel Documents
Culture Documents
Implications of Designating Obesity As A Disease
Transféré par
sadhna_pTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Implications of Designating Obesity As A Disease
Transféré par
sadhna_pDroits d'auteur :
Formats disponibles
Implications for Plan
Sponsors of Obesitys
Designation as a Disease
Obesity is a major risk factor for
serious chronic diseases and condi-
tions including, but not limited to,
type 2 diabetes, hypertension, sleep
apnea, gallstones, infertility, vari-
cose veins, gout, osteoarthritis and
deep vein thrombosis (DVT). The
fnancial impact of obesity related
diseases and treatments on medi-
cal plan budgets can be signifcant.
Medical care costs associated with
obesity were about $147 billion in
2008, according to a study cited by
the Centers for Disease Control
and Prevention.
1
In June 2013, the American Medical
Association (AMA) voted in favor
of recognizing obesity as a disease
that requires medical treatment.
2
According to the AMA, recognizing
obesity as a disease will help change
the way the medical community
tackles this complex issue that af-
fects more than 78 million American
adults (35.7 percent of adults) and
12 million children (16.9 percent
of children).
3
(The text box below
discusses how obesity is defned.)
The supporters of the move
claim that it makes diagnosis
and treatment of obesity a physicians
professional obligation. More than
half of obese patients have never
been told by a medical profession-
al they need to lose weight.
4
Some
doctors are reluctant to offend their
patients by telling them that they are
obese and/or are unwilling to open a
discussion that will result in a lengthy
consultation for which they might
not be reimbursed.
Calling obesity a disease is not
without controversy. Opponents
of this AMA vote believe it will shift
the nations focus too much toward
expensive drug and surgical treat-
ments and away from measures
to encourage healthy diets and
regular exercise.
IN THIS ISSUE:
Coverage for Obesity
Treatments Today
How Coverage for Obesity
Treatment Is Likely to Change
Based on Obesitys Designation
as a Disease
Should Plan Sponsors Be
Worried About the Additional
Costs of Coverage?
Cost-Management Strategies
Conclusion
Who Is Considered Obese?
According to the Centers for Disease Control and Prevention, an adult is
obese if his or her body mass index (BMI) is 30 or higher. For comparison
purposes, a person with a BMI between 18.5 and 24.9 is considered to
have a healthy weight, while a person with a BMI between 25 and 29.9
is overweight.
BMI for adults is calculated by taking weight (measured in kilograms) and
dividing it by the square of the persons height (measured in meters). For
those who prefer standard measurements, measure weight in pounds, di-
vide it by the square of height measured in inches, and multiply the result
by 703.
It should be noted that these government-set BMI measurements have
limitations. For example, the BMI definition of obesity is not useful for
those who are athletic (because they typically have more muscle mass/
weight and low body fat). Consequently, some medical professionals pre-
fer measuring waist circumference as a measure of obesity. However, the
BMI metric is an adequate starting point for most patients and doctors.
2
The press release announcing this decision is
available on the following page of the AMA
website: http://www.ama-assn.org/ama/pub/news/
news/2013/2013-06-18-new-ama-policies-annual-
meeting.page
3
Cynthia L. Ogden, CL, Carroll, MD, Kit BK, Flegal
KM. Prevalence of obesity in the United States,
20092010, NCHS data brief, no. 82, Hyattsville,
MD: National Center for Health Statistics. 2012:
http://www.cdc.gov/nchs/data/databriefs/db82.pdf
4
Post, Robert E. MD, MS; Mainous III, Arch G. PhD;
Gregorie, Seth H. BS; Knoll, Michele E. MA; Diaz,
Vanessa A. MD, MS; Saxena, Sonia K. MD, The
Infuence of Physician Acknowledgment of Patients
Weight Status on Patient Perceptions of Overweight
and Obesity in the United States.Archives of
Internal Medicine. 171(4) (2011): 316321.
Segal Consulting is a member of The Segal Group (www.segalgroup.net),
which is celebrating its 75
th
anniversary this year.
1
Finkelstein, EA, Trogdon, JG, Cohen, JW, and
Dietz, W. Annual medical spending attributable
to obesity: Payer- and service-specifc estimates.
Health Affairs 2009; 28(5): w822w831.
Benefits, Compensation and HR Consulting JULY 2014
Public Sector Letter
Public Sector Letter
The Internal Revenue Service (IRS) has
long recognized obesity as a disease.
5
Consequently, a weight-loss program
prescribed by a physician to treat obe-
sity is considered a medical expense
under Section 213(d) of the Internal
Revenue Code. Moreover, obesity
screening and counseling is a preven-
tive beneft under the Affordable Care
Act,
6
and non-grandfathered plans
must cover such care with no patient
cost-sharing requirement.
After noting how obesity treatments
typically are covered today, this
Public Sector Letter discusses the
implications for plan sponsors of the
AMAs designation of obesity as
a disease.
COVERAGE FOR OBESITY
TREATMENTS TODAY
Today, coverage of obesity-related
treatments is inconsistent. Most plans
either do not cover the treatment or
provide spotty coverage. Sources
vary on the exact percentage of group
plans that cover weight-loss cover-
age with or without covering
bariatric surgery.
Medicare, which insures an estimated
13 million obese Americans who are
age 65 or older or disabled, already
covers the costs of intensive behav-
ioral therapy for obese patients, as
well as bariatric surgery for those
with additional health conditions,
such as diabetes. However, Medicare
Part D, the prescription drug beneft,
does not currently require coverage of
weight-loss drugs.
7
HOW COVERAGE FOR OBESITY
TREATMENT IS LIKELY TO CHANGE
BASED ON OBESITYS DESIGNATION
AS A DISEASE
In response to the AMAs designation
of obesity as a disease, coverage for
obesity treatment is likely to change.
Like most other diseases, there are
three potential treatments for obesity:
Clinical or Non-Clinical Coun-
seling with Group or Personal
Support Services Jenny Craig and
Weight Watchers have been avail-
able to workers for years to help
overweight and obese members
lose weight and keep it off. More
recent weight-loss tools, like FitBit,
use technology to help people track
their progress.
8
A growing body of
expertise around behavior mod-
ifcation is helping clinicians to
improve the effcacy of weight-loss
programs. However, studies suggest
that although very high number of
participants can lose weight, most
have trouble keeping the weight off.
Prescription Drug Therapy
There are two relatively new drugs
approved by the Food and Drug
Administration (FDA) for treating
obesity: Qsymia
and Belviq
.
9
Qsymia was viewed as potentially
a frst-line obesity drug for many
patients, but the current lack of or
restricted mail-order-only coverage
has prevented its widespread adop-
tion. Although these drugs are
expensive (around $200 per prescrip-
tion per month) the duration of the
drug therapy will vary by patient.
Surgical Intervention As more and
more providers perform gastro-
bypass procedures, the effcacy
strengthens and the risks of surgical
complications decline. Bariatric
surgery, which costs, on average,
$20,000 to $25,000,
10
has perhaps
the best data supporting positive
outcomes.
11
The science behind
some of these unexpected favorable
outcomes (e.g., eliminating diabetes
in diabetics) is not clear, but there
are changes that go well beyond
the direct effects of the surgery, and
seem to impact hormonal balance
and change the setpoint that
often works against traditional
weight-loss approaches. Given that
surgery has risks, plan sponsors
should help patients study quality
results by provider and facility.
Other surgical approaches, such
as the gastric sleeve, while not as
effcacious as bariatric surgery,
could gain favor because of the
convenience of performing the
procedures, and potentially lower
risk of surgical complications. Lap
bands may be losing some of their
attraction because of the degree of
post-surgical care required.
12
For the public Marketplaces created
by the Affordable Care Act for indi-
viduals to purchase coverage,
23 states chose benchmark plans that
cover bariatric surgery. Under the
Affordable Care Act, more insurance
plans are expected to start cover-
ing the cost of obesity treatments,
including counseling on diet and
exercise, surgery and medication,
as long as they are approved by the
2
10
This data is from the National Institute of Diabetes
and Digestive and Kidney Diseases, which is part of
the National Institutes of Health: http://win.niddk.
nih.gov/publications/gastric.htm#medicalcosts
11
For example, Cleveland Clinics Bariatric & Meta-
bolic Institute published research in 2013 that found
positive health effects of bariatric surgery lasted
up to nine years after the procedure. See this press
release about the study: http://my.clevelandclinic.org/
media_relations/library/2013/2013-09-19-cleveland-
clinic-study-shows-long-term-effects-bariatric-
surgery-obese-patients-type-2-diabetes.aspx
12
The following post from the Advisory Board
Company on Obesity Week 2013 addresses the
declining popularity of lap bands: http://www.
advisory.com/research/service-line-strategy-advisor/
the-pipeline/2013/11/obesity-week-2013-is-the-lap-
band-still-an-option
5
See IRS Revenue Ruling 200219, 200216 I.R.B.
778: http://www.irs.gov/pub/irs-drop/rr-02-19.pdf
6
The Affordable Care Act is the shorthand name
for the Patient Protection and Affordable Care Act
(PPACA), as modifed by the subsequently enacted
Health Care and Education Reconciliation
Act (HCERA).
7
In February 2014, the Agency for Healthcare
Research & Quality published a document,
Therapeutic Options for Obesity in the Medicare
Population: http://www.ahrq.gov/research/fndings/
ta/topicrefnement/obesity_topic_refnement.pdf
8
FitBit uses wearable wireless-enabled devices, like
wristbands, to track activity. Data can be saved to
smartphones and secure websites.
9
For information about these drugs, refer to an online
supplement to this Public Sector Letter:
http://www.segalco.com/publications/
publicsectorletters/714supp.pdf
Public Sector Letter
FDA and the treatment is prescribed
by a physician. The U.S. Preventive
Services Task Force recommends that
health care providers offer or refer
patients with a BMI of at least 30 to
intensive, multi-component behavior-
al interventions, which would include
weight-loss programs that have 12 to
26 sessions in a year and that include
a variety of activities and strategies
to help them lose weight.
13
The federal
agencies responsible for implementing
the Affordable Care Act have not yet
directed plan sponsors to pay for
12 to 26 sessions per year, but the pre-
ventive services coverage requirements
are subject to change, and should be
monitored for future developments.
The Affordable Care Act also ad-
dressed wellness programs. The fnal
rule implementing those provisions
increased the amount of a reward that
may be provided through a wellness
program and tightened requirements
for health-contingent wellness
programs that require individuals to
achieve specifc health targets, such
as weight loss, before they are eligible
for a reward.
14
SHOULD PLAN SPONSORS BE
WORRIED ABOUT THE ADDITIONAL
COSTS OF COVERAGE?
To some extent, the designation of
obesity as a disease will increase
plans immediate costs. However, over
the long term, covering obesity treat-
ments is likely to save plans money by
avoiding serious and costly chronic
diseases and conditions for which
obesity is a major risk factor.
Designating obesity a disease will
reduce the stigma that stems from
the widespread perception that it is
simply the result of eating too much
or exercising too little, when in reality
some people do not have full con-
trol over their weight. Recognizing
this, more people will seek treatment
under the diagnosis of obesity, as op-
posed to waiting to receive treatment
until they develop one of the obesi-
ty-related conditions.
Ultimately, prudent plan sponsors will
get ahead of this issue and structure
beneft coverage to support effective
weight reduction and management
programs in a manner that reduces
wasteful spending and holds providers
and patients accountable for taking ac-
tion to best manage this disease. When
signifcant weight loss occurs, by any
means, the result is highly observable
to co-workers. The risk of regaining
weight is real. An organizational
culture that supports health improve-
ment, empathy and respect toward
others will go a long way toward help-
ing individuals develop and maintain
new positive health habits.
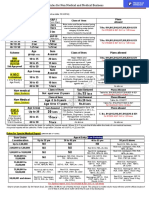
The potential savings are substantial.
As shown in Graph 1, the Mayo clinic
found that annual medical costs for
its obese employees and adult depen-
dents were thousands of dollars more
than for non-obese employees and
dependents. Graph 2 on the next page
shows how a Segal clients monthly
per-participant costs break down by
participants waist size.
COST-MANAGEMENT STRATEGIES
Plan design can be used to ration
spending in a prudent fashion (e.g.,
reference-based pricing of surgery
linked to target provider costs,
prior-authorization for approval of
prescription drug therapy). There are
several strategies for dealing with
the short-term cost increase associat-
ed with obesitys designation as
a disease:
Institute step-therapy for obesity
treatment. This approach might
start with nutrition and exercise
counseling. If that proves insuff-
cient, the plan might cover one or
both of the FDA-approved prescrip-
tion drugs. Surgeries can be the last
resort if everything else fails.
Graph 1: Amount by Which Annual
Medical Costs for Overweight and
Obese Employees and their Adult
Dependents Exceed the Costs for
Healthy Weight Employees and
their Adult Dependents
Source: Moriarty, James P. MSc; Branda, Megan
E. MS; Olsen, Kerry D. MD; Shah, Nilay D. PhD;
Borah, Bijan J. PhD; Wagie, Amy E. BS; Egginton,
Jason S. MPH; Naessens, James M. ScD.
The Effects of Incremental Costs of Smoking
and Obesity on Health Care Costs Among
Adults: A 7-Year Longitudinal Study. Journal of
Occupational & Environmental Medicine 54.3
(2012): 286291.
3
A
d
d
i
t
i
o
n
a
l
A
n
n
u
a
l
C
o
s
t
P
e
r
c
e
n
t
Overweight 3540
BMI
40+
BMI
Obese
0
1,500
3,000
$1,850
$3,086
$5,530
4,500
$6,000
13
See http://www.uspreventiveservicestaskforce.org/
uspstf11/obeseadult/obesers.htm
14
The fnal rule on wellness programs offered by group
health plans is summarized in Segal Consultings
July 11, 2013 Capital Checkup: http://www.segalco.
com/publications-and-resources/public-sector-
publications/capital-checkup/archives/?id=2386
Over the long term, covering obesity treatments is likely to save
plans money by avoiding serious and costly chronic diseases and
conditions for which obesity is a major risk factor.
Public Sector Letter
Require prior authorization for
covering obesity treatments. Under
this approach, physicians must
report information to the plan on
a patients biometrics and prior
efforts, in order to seek approval
of a treatment plan.
Choose narrow networks or Centers
of Excellence for complex surger-
ies, such as bariatric surgery. These
highly experienced providers typical-
ly yield the best outcomes from both
a clinical and cost perspective.
Introduce reference-based pric-
ing. This approach sets maximum
payment amounts to be reimbursed
based on reference provider(s) or
drug(s), meaning individuals pay
the cost above the reference price.
Reference-based pricing creates
market controls to mitigate exces-
sive pricing set by some providers
or drug makers.
Plan sponsors may want to enlist the
support and expertise of specialty well-
ness vendors to help lead the process
to design, implement and monitor an
effective weight management program
that best fts their needs. Segal can
help clients review current popular
design strategies and help clients fnd
the right specialty vendors to adminis-
ter the program.
CONCLUSION
While many diseases can be defeated
with a pill or vaccine, tackling obesity
is considerably more complex because
it requires people to change the way
they eat and live. That makes obesity
harder to treat than other diseases.
Changing patient behavior plays a
pivotal role in conquering obesity.
Plan communications can play an
important role in helping participants
to understand the serious health risks
associated with obesity and to modify
their behavior.
Nevertheless, the effort and the
additional short-term costs are
worthwhile because the long-term
health benefts and the associated
savings can be substantial. For plan
sponsors with long-term employment
relationships, reducing the prevalence
and severity of obesity among a plans
population should result in both plan
cost savings and healthier workers a
few years down the road.
Segal Consulting can help plan spon-
sors to design coverage for treating
obesity that best meets their objectives
and to identify the right vendors to
provide effective participant support
and counseling for weight loss. For
more information about or assistance
with these services, contact your
Segal consultant, Rick Johnson,
National Public Sector Health
Practice Leader, at 202.833.6470
or rjohnson@segalco.com or one
of the authors:
Sadhna Paralkar, MD
312.933.7808
sparalkar@segalco.com
Edward A. Kaplan
212.251.5212
ekaplan@segalco.com
Copyright 2014 by The Segal Group, Inc. All rights reserved.
www.segalco.com
To receive Public Sector
Letters and other Segal
Consulting publications of
interest to state and local
government employers as
soon as they are available
online, register your e-mail
address via Segals website:
www.segalco.com
For a list of Segals ofces,
visit www.segalco.com/about-
us/contact-us-locations/
Segal Consulting is a
member of The Segal Group
(www.segalgroup.net).
Graph 2: A Segal Clients Monthly Health Costs by Participants Waist
Measurements and Percent of Participants in Each Measurement Group
Source: Segal Consulting
$-
100
200
300
$400
0
10
20
30
40
50%
M
o
n
t
h
l
y
C
o
s
t
P
e
r
P
a
r
t
i
c
i
p
a
n
t
P
e
r
c
e
n
t
o
f
P
a
r
t
i
c
i
p
a
n
t
s
Medical
Participants with
Waist <35 Inches
Participants with
Waist 3540 Inches
Participants with
Waist >40 Inches
Rx % of Participants
Obesity [is] harder to treat than
other diseases.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Concepts Underlying The Design of Health ProgramsDocument31 pagesConcepts Underlying The Design of Health ProgramsMUTHUKUMARAN100% (1)
- IMIST TrainingDocument31 pagesIMIST TrainingSetiadi Margono80% (5)
- AP GeographyDocument95 pagesAP GeographyKhimavathBharathNaik88% (8)
- Health and Wellness Programs For CVommercial Truck Drivers 144 PagesDocument91 pagesHealth and Wellness Programs For CVommercial Truck Drivers 144 PagesDenise Mathre100% (1)
- Mean Arterial PressureDocument3 pagesMean Arterial Pressureleslie vasquez lucumiPas encore d'évaluation
- Blue Modern Medical Center Z-Fold BrochureDocument2 pagesBlue Modern Medical Center Z-Fold BrochureAngela Shaine CruzPas encore d'évaluation
- Penlon Absorbedor A200Document68 pagesPenlon Absorbedor A200Manuel FloresPas encore d'évaluation
- PAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Document28 pagesPAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Narendrakumar100% (2)
- SRP Batch 1Document32 pagesSRP Batch 1eenahPas encore d'évaluation
- Rules For Non Medical BusinessDocument1 pageRules For Non Medical BusinessAbhijit AminpurPas encore d'évaluation
- 2019 EC 006 REORGANIZING BADAC Zone - 1Document5 pages2019 EC 006 REORGANIZING BADAC Zone - 1Barangay BotongonPas encore d'évaluation
- Freud's Psychosexual Stages of DevelopmentDocument30 pagesFreud's Psychosexual Stages of DevelopmentjessaPas encore d'évaluation
- Boq Lahan Parkir Hotel BogorDocument2 pagesBoq Lahan Parkir Hotel BogorFariz MemetPas encore d'évaluation
- Harga Obat Generik E-KatalogueDocument4 pagesHarga Obat Generik E-KatalogueMuhammad FarilPas encore d'évaluation
- Migrants' Election ManifestoDocument2 pagesMigrants' Election ManifestoMimi Panes - CorosPas encore d'évaluation
- THE Center: Anxiety DisordersDocument13 pagesTHE Center: Anxiety DisordersOti VuraPas encore d'évaluation
- Unit Iv: Community Health Nursing Approaches, Concepts and Roles and Responsibilities of Nursing PersonnelDocument17 pagesUnit Iv: Community Health Nursing Approaches, Concepts and Roles and Responsibilities of Nursing Personnelkles insgkkPas encore d'évaluation
- Prevention of Foodborne Disease: The Five Keys To Safer FoodDocument2 pagesPrevention of Foodborne Disease: The Five Keys To Safer FoodThong Boon LeongPas encore d'évaluation
- Transcript Emily Fletcher Greater Sex Better Sleep With Ziva Meditation 224 PDFDocument40 pagesTranscript Emily Fletcher Greater Sex Better Sleep With Ziva Meditation 224 PDFLacramioara Ionescu100% (1)
- Tibetan Medicine and The CoronavirusDocument1 pageTibetan Medicine and The CoronavirusIvan IvanicPas encore d'évaluation
- Analisis Keberhasilan Implementasi RME Mutu PelayananDocument8 pagesAnalisis Keberhasilan Implementasi RME Mutu PelayananWinda PurbaPas encore d'évaluation
- hsg261 Health and Safety in Motor Vehicle Repair and Associated Industries PDFDocument101 pageshsg261 Health and Safety in Motor Vehicle Repair and Associated Industries PDFpranksterboyPas encore d'évaluation
- CertificateDocument1 pageCertificateriteshPas encore d'évaluation
- Relationship Among Levels of DFDsDocument8 pagesRelationship Among Levels of DFDssunny_242574Pas encore d'évaluation
- Turner 1st SEM at FinalDocument102 pagesTurner 1st SEM at FinalSashikant Sharma100% (1)
- Surgeons in Rangpur, Bangladesh - SOSBDocument11 pagesSurgeons in Rangpur, Bangladesh - SOSBWadood Md ZahedPas encore d'évaluation
- Slu Brochure Ay 2014-2015Document2 pagesSlu Brochure Ay 2014-2015Michael BermudoPas encore d'évaluation
- Chemistry, Manufacturing and ControlDocument11 pagesChemistry, Manufacturing and ControlHk HkPas encore d'évaluation
- Daftar Obat Generik Klinik Citalang Medika Golongan Nama Obat Komposisi Golongan Nama ObatDocument2 pagesDaftar Obat Generik Klinik Citalang Medika Golongan Nama Obat Komposisi Golongan Nama ObattomiPas encore d'évaluation
- 70 Questions For The FDA Inspection - Dietary SupplementsDocument8 pages70 Questions For The FDA Inspection - Dietary SupplementsSamuel ChewPas encore d'évaluation