Académique Documents
Professionnel Documents
Culture Documents
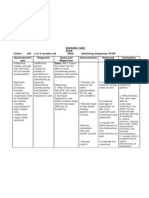
Activity intolerance nursing care cervical cancer chemotherapy
Transféré par
Ivy Mina0 évaluation0% ont trouvé ce document utile (0 vote)
1K vues4 pagesThis is a nursing diagnosis for a client with cervical cancer. This includes dependent, independent and collaborative nursing interventions.
Titre original
Activity Intolerance related to generalized weakness
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentThis is a nursing diagnosis for a client with cervical cancer. This includes dependent, independent and collaborative nursing interventions.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
1K vues4 pagesActivity intolerance nursing care cervical cancer chemotherapy
Transféré par
Ivy MinaThis is a nursing diagnosis for a client with cervical cancer. This includes dependent, independent and collaborative nursing interventions.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 4
Activity Intolerance related to generalized weakness secondary to side
effects of chemotherapy for advanced stage of cervical cancer
Independent Nsg Interventions
(i) Determine patient's perception of causes of fatigue or activity intolerance.
May be temporary or permanent, physical, or psychological. Assessment guides
treatment.
(i) Assess patient's level of mobility.
Aids in defining what patient is capable of, which is necessary before setting realistic
goals.
(i) Assess nutritional status.
Adequate energy reserves are required for activity.
(i) Assess potential for physical injury with activity.
Injury may be related to falls or overexertion.
(i) Assess need for ambulation aids: bracing, cane, walker, equipment modification for
activities of daily living (ADLs).
Some aids may require more energy expenditure (walking with crutches) for patients who
have reduced upper arm strength. Adequate assessment of energy requirements is
indicated.
(i) Assess patient's cardiopulmonary status before activity using the following measures:
Heart rate
o Heart rate should not increase greater than 20 to 30 beats above resting with
routine activities. This number will change depending on the intensity of exercise
the patient is attempting (climbing four flights of stairs versus shoveling snow).
Orthostatic BP changes
o Elderly patients are more prone to drops in blood pressure with position changes.
Need for oxygen with increased activity
o Portable pulse oximetry can be used to assess for oxygen desaturation.
Supplemental oxygen may help compensate for the increased oxygen demands.
How Valsalva's maneuver affects heart rate when patient moves in bed
o Valsalva's maneuver, which requires breath holding and bearing down, can cause
bradycardia and related reduced cardiac output.
(i) Monitor patient's sleep pattern and amount of sleep achieved over past few days.
Difficulties sleeping need to be addressed before activity progression can be achieved.
(i) Observe and document response to activity.
Close monitoring serves as a guide for optimal progression of activity.
Report any of the following:
Rapid pulse (20 beats over resting rate or 120 beats per minute [BPM])
Palpitations
Significant increase in systolic BP (20 mm Hg)
Significant decrease in systolic BP (drop of 20 mm Hg)
Dyspnea, labored breathing, wheezing
Weakness, fatigue
Lightheadedness, dizziness, pallor, diaphoresis
(i) Assess emotional response to change in physical status.
Depression over inability to perform required activities can further aggravate the activity
intolerance.
(i) Establish guidelines and goals of activity with the patient and caregiver.
Motivation is enhanced if the patient participates in goal setting. Depending on the
etiologic factors of the activity intolerance, some patients may be able to live
independently and work outside the home. Other patients with chronic debilitating
disease may remain homebound.
(i) Encourage adequate rest periods, especially before meals, other activities of daily living,
exercise sessions, and ambulation.
To reduce cardiac workload.
(i) Refrain from performing nonessential procedures.
To promote rest. Patients with limited activity tolerance need to prioritize tasks.
(i) Anticipate patient's needs (e.g., keep telephone and tissues within reach).
(i) Assist with ADLs as indicated.
To reduce energy expenditure.
However, avoid doing for patient what he or she can do for self.
To optimize patient's self-esteem.
(i) Provide bedside commode as indicated.
To reduce energy expenditure. NOTE: Bedpans require more energy than commode.
(i) Encourage physical activity consistent with patient's energy resources.
(i) Assist patient to plan activities for times when he or she has the most energy.
Not all self-care and hygiene activities need to be completed in the morning. Likewise,
not all housecleaning needs to be completed in one day.
(i) Encourage verbalization of feelings regarding limitations.
Acknowledgment that living with activity intolerance is both physically and emotionally
difficult aids coping.
(i) Progress activity gradually.
To prevent overexerting the heart and promote attainment of short-range goals, as with
the following:
Active range-of-motion (ROM) exercises in bed, progressing to sitting and standing.
Dangling 10 to 15 minutes three times daily
Deep breathing exercises three times daily
Sitting up in chair 30 minutes three times daily
Walking in room 1 to 2 minutes three times daily
Walking in hall 25 feet or walking around the house, then slowly progressing, saving
energy for return trip.
(i) Encourage active ROM exercises three times daily. If further reconditioning is needed,
confer with rehabilitation personnel.
To maintain muscle strength and joint range of motion.
(i) Provide emotional support while increasing activity. Promote a positive attitude
regarding abilities.
(i) Encourage patient to choose activities that gradually build endurance.
(i) Improvise in adapting ADL equipment or environment.
Appropriate aids will enable the patient to achieve optimal independence for self-care.
(i) Teach patient/caregivers to recognize signs of physical overactivity.
Promotes awareness of when to reduce activity.
(i) Involve patient and caregivers in goal setting and care planning.
Setting small attainable goals can increase self-confidence and self-esteem.
(i) When hospitalized, encourage significant others to bring ambulation aid: walker or
cane.
(i) Teach the importance of continued activity at home.
To maintain strength, ROM, and endurance gain.
(i) Assist in assigning priority to activities to accommodate energy levels.
(i) Teach energy conservation techniques.
They reduce oxygen consumption, allowing more prolonged activity.
Some examples include the following:
Sitting to do tasks.
o Standing requires more work.
Changing positions often.
o Distributes work to different muscles to avoid fatigue.
Pushing rather than pulling.
Sliding rather than lifting.
Working at an even pace.
o Allows enough time so not all work is completed in a short period of time.
Storing frequently used items within easy reach.
o To avoid bending and reaching.
Resting for at least 1 hour after meals before starting a new activity.
o Because energy is needed to digest food.
Using wheeled carts for laundry, shopping, and cleaning needs.
Organizing a work-rest-work schedule.
(i) Teach appropriate use of environmental aids (e.g., bed rails, elevation of head of bed
while patient gets out of bed, chair in bathroom, hall rails).
To conserve energy and prevent injury from fall.
(i) Teach ROM and strengthening exercises.
(i) Encourage patient to verbalize concerns about discharge and home environment
To reduce feelings of anxiety and fear.
Dependent Nsg Interventions
Check physicians order then administer drugs
Rationale: To prevent any errors. Only privileged physicians and residents under their
supervision can order medications.
Provide/monitor response to supplemental oxygen and medications and changes in
treatment regimen
Monitor any abnormal sign and symptoms
Rationale: To prevent further complications
Monitor laboratory studies, Hb or Hct and RBC count, arterial blood gas (ABGs)
Rationale: Identifies deficiencies in RBC components affecting oxygen transport and
treatment needs or response to therapy
Collaborative Nsg Interventions
Receive/transfer client from the O.R. (if applicable)
Provide referral to other disciplines like physical or occupational therapists
Rationale: To develop individually appropriate therapeutic regimens
Vous aimerez peut-être aussi
- NCP - Activity IntoleranceDocument3 pagesNCP - Activity Intolerancejanelee2824Pas encore d'évaluation
- Bladder Infection Nursing CareDocument8 pagesBladder Infection Nursing CareJoseph Anthony Benitez VerzosaPas encore d'évaluation
- Saldana - Fdar Lung CancerDocument2 pagesSaldana - Fdar Lung CancerMika SaldañaPas encore d'évaluation
- NCP Acitivity IntoleranceDocument3 pagesNCP Acitivity IntolerancegizellePas encore d'évaluation
- Nursing Care Plan for Cholelithiasis Patient Undergoing ECGDocument2 pagesNursing Care Plan for Cholelithiasis Patient Undergoing ECGJenny Ajoc0% (1)
- DP For Acute Respiratory FailureDocument1 pageDP For Acute Respiratory FailurePauline SalgadoPas encore d'évaluation
- Appendectomy NCPDocument4 pagesAppendectomy NCPPersha Perez ArabaniPas encore d'évaluation
- NCP For CTTDocument1 pageNCP For CTTJen Rhae LimPas encore d'évaluation
- NCP Proper - Obstructive JaundiceDocument8 pagesNCP Proper - Obstructive JaundiceWyen Cabatbat100% (1)
- NCP UtiDocument1 pageNCP UtiAgentpiinkkPas encore d'évaluation
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananPas encore d'évaluation
- Activity IntoleranceDocument3 pagesActivity IntoleranceRaidis PangilinanPas encore d'évaluation
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDocument4 pagesNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3APas encore d'évaluation
- Aiza NCPDocument6 pagesAiza NCPponponolmedoPas encore d'évaluation
- Combivent Nursing Care and Side EffectsDocument1 pageCombivent Nursing Care and Side Effectsleroux2890Pas encore d'évaluation
- Nursing Care Plan for Hypertension and Knee PainDocument3 pagesNursing Care Plan for Hypertension and Knee PainEzron Kendrick Duran50% (2)
- Gi-Rle - NCP For Deficient Fluid VolumeDocument2 pagesGi-Rle - NCP For Deficient Fluid VolumeEvangeline Villa de Gracia100% (1)
- Nursing Care Plan Priorities for Hemodialysis PatientsDocument6 pagesNursing Care Plan Priorities for Hemodialysis PatientsPauling FrezPas encore d'évaluation
- NCPDocument6 pagesNCPJoni Lyn Ba-as BayengPas encore d'évaluation
- Final Course in The WardDocument4 pagesFinal Course in The WardMichael Boado100% (1)
- Discharge Instructions - Laparoscopic Cholecystectomy: ActivityDocument2 pagesDischarge Instructions - Laparoscopic Cholecystectomy: ActivityAnne Marie Angelica BilonoPas encore d'évaluation
- Nursing Diagnosis: Ineffective Tissue PerfusionDocument2 pagesNursing Diagnosis: Ineffective Tissue PerfusionIan RamaPas encore d'évaluation
- NCP For CipDocument22 pagesNCP For CipBing DayaoPas encore d'évaluation
- LFD CommunityDocument1 pageLFD Communityjai2x100% (1)
- NcpsDocument10 pagesNcpskotoirPas encore d'évaluation
- Case Study NCP ActualDocument3 pagesCase Study NCP Actualdhamy florPas encore d'évaluation
- 2 Teaching Plan For AppendicictisDocument1 page2 Teaching Plan For AppendicictisHarris CacanindinPas encore d'évaluation
- Impaired Urinary EliminationDocument2 pagesImpaired Urinary EliminationMatty-b AskalaniPas encore d'évaluation
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceKen RegalaPas encore d'évaluation
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaPas encore d'évaluation
- NCPDocument3 pagesNCPJezza RequilmePas encore d'évaluation
- Llacer FdarDocument2 pagesLlacer FdarRaidis PangilinanPas encore d'évaluation
- Cardiovascular Conditioning Monitoring ChartDocument2 pagesCardiovascular Conditioning Monitoring ChartDanielle Patricia Valencia OtedaPas encore d'évaluation
- Hyperthermia NCPDocument3 pagesHyperthermia NCPJayr DiazPas encore d'évaluation
- Nursing Diagnosis Rationale Interventions Rationale EvaluationDocument2 pagesNursing Diagnosis Rationale Interventions Rationale EvaluationJobie CasipongPas encore d'évaluation
- Nursing Assessment Rationale and InterventionsDocument7 pagesNursing Assessment Rationale and InterventionsPJPas encore d'évaluation
- Nursing Care Plan for Activity Intolerance and Nutrition ImbalanceDocument4 pagesNursing Care Plan for Activity Intolerance and Nutrition ImbalanceEjie Boy Isaga100% (1)
- SunStar News Doctors May Lose Their Licenses Over Surgery ScandalDocument4 pagesSunStar News Doctors May Lose Their Licenses Over Surgery Scandalseigelystic100% (12)
- Bilirubin Assessment and Nursing DiagnosisDocument2 pagesBilirubin Assessment and Nursing DiagnosisJonica CamposPas encore d'évaluation
- NCP Con ConstipationDocument2 pagesNCP Con ConstipationChristine Marie Bucio OraizPas encore d'évaluation
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument2 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestPas encore d'évaluation
- Emj Cases : Questions For Case 1Document8 pagesEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- NCP HyperthermiaDocument6 pagesNCP HyperthermiaGrax DeePas encore d'évaluation
- Nursing Care Plan: Wong's Nursing Care of Infants and Children, 8 Ed. Pg. 324Document3 pagesNursing Care Plan: Wong's Nursing Care of Infants and Children, 8 Ed. Pg. 324Erle Gray CadangenPas encore d'évaluation
- Reflection: Name: Semester: Assignment: Submitted To: Submission DateDocument2 pagesReflection: Name: Semester: Assignment: Submitted To: Submission DateWednesdayPas encore d'évaluation
- Cancer Nursing Care Plan (NCP) - Risk For InfectionDocument2 pagesCancer Nursing Care Plan (NCP) - Risk For InfectionAngie MandeoyaPas encore d'évaluation
- Risk for Aspiration Nursing Care Plan During CholecystectomyDocument1 pageRisk for Aspiration Nursing Care Plan During CholecystectomyJess GoPas encore d'évaluation
- NCP PSHDocument17 pagesNCP PSHMargareth OrtizPas encore d'évaluation
- Betty Impaired Skin IntegrityDocument2 pagesBetty Impaired Skin IntegrityBenjie DimayacyacPas encore d'évaluation
- Planning: NCP #1 Chronic Pain Related To Compression of Spinal Nerves As Evidenced byDocument10 pagesPlanning: NCP #1 Chronic Pain Related To Compression of Spinal Nerves As Evidenced byNicole Anne TungolPas encore d'évaluation
- DP Discharge Plan@@@@@@@@Document6 pagesDP Discharge Plan@@@@@@@@Maemae SumalinogPas encore d'évaluation
- Nursing Care Plan for Skin AbscessDocument1 pageNursing Care Plan for Skin AbscessKriz_sakuradreamPas encore d'évaluation
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonPas encore d'évaluation
- Sine CodDocument2 pagesSine CodshaynePas encore d'évaluation
- Subjective Cues:: Nursing Care ProcessDocument8 pagesSubjective Cues:: Nursing Care ProcessBianca Marithè RejanoPas encore d'évaluation
- Discharge Plan CapDocument3 pagesDischarge Plan Capalexander abasPas encore d'évaluation
- Activity IntoleranceDocument6 pagesActivity IntoleranceDenvEr CabaniLlasPas encore d'évaluation
- NCP Nursing Diagnosis: Activity IntoleranceDocument4 pagesNCP Nursing Diagnosis: Activity IntoleranceAngelica Orbase BelmontePas encore d'évaluation
- Activity IntoleranceDocument4 pagesActivity IntoleranceDianne MacaraigPas encore d'évaluation
- Electrical Alternans: - Prof.M.K.Sudhakar's UnitDocument19 pagesElectrical Alternans: - Prof.M.K.Sudhakar's UnitVivek AnandanPas encore d'évaluation
- Body PartsDocument4 pagesBody PartsMatthias Dos SantosPas encore d'évaluation
- English Paper 2 UPSRDocument10 pagesEnglish Paper 2 UPSRJaya Chitra Degala RamaluPas encore d'évaluation
- Cardiac Arrest ISMKI 23 April 2021Document46 pagesCardiac Arrest ISMKI 23 April 2021KM Habil SPas encore d'évaluation
- Cheetsheet 6Document1 pageCheetsheet 6Rick Frea92% (12)
- Pig Heart Dissection Lab 2012-2013finaldraftpdfDocument21 pagesPig Heart Dissection Lab 2012-2013finaldraftpdfapi-169518406Pas encore d'évaluation
- Q4 Week 3 4 GenBio2 EditedDocument12 pagesQ4 Week 3 4 GenBio2 EditedXyreen GalicinaoPas encore d'évaluation
- Pediatric Board Certification and Recertification Review and - PDF Version 1Document822 pagesPediatric Board Certification and Recertification Review and - PDF Version 1della mouradPas encore d'évaluation
- Student Medical DeclarationDocument1 pageStudent Medical DeclarationDandreb Magnaye AliasPas encore d'évaluation
- General Biology 2 Quarter 2 Module 2 VER 4Document47 pagesGeneral Biology 2 Quarter 2 Module 2 VER 4Merlojane Tecson TaliwananPas encore d'évaluation
- Cardiofax Ecg 9020k ManualDocument36 pagesCardiofax Ecg 9020k ManualViviana Páez RojasPas encore d'évaluation
- Science 9 ReviewerDocument22 pagesScience 9 ReviewerRio OrpianoPas encore d'évaluation
- Celom and digestive system labDocument134 pagesCelom and digestive system labLisa WolskiPas encore d'évaluation
- Cardiovascular DisordersDocument20 pagesCardiovascular DisordersHampson MalekanoPas encore d'évaluation
- HDL Cholesterol KitDocument2 pagesHDL Cholesterol KitZumaira AbbasPas encore d'évaluation
- Heart Rate LabDocument6 pagesHeart Rate LabSteve RodriguesPas encore d'évaluation
- Heart Failure Clinical Presentation - History, Physical Examination, Predominant Right-Sided Heart Failure PDFDocument11 pagesHeart Failure Clinical Presentation - History, Physical Examination, Predominant Right-Sided Heart Failure PDFislamiah 89Pas encore d'évaluation
- By James W. Grier Department of Biological Sciences North Dakota State University Fargo, ND 58102-3400Document33 pagesBy James W. Grier Department of Biological Sciences North Dakota State University Fargo, ND 58102-3400bsirisha415100% (1)
- Neonatal Respiratory Distress Syndrome TreatmentDocument12 pagesNeonatal Respiratory Distress Syndrome TreatmentRazelVillanueva67% (3)
- Class X Science Pre Board Sample PaperDocument23 pagesClass X Science Pre Board Sample PaperNasla ShiyasPas encore d'évaluation
- 5-Minute EKG Interpretation GuideDocument1 page5-Minute EKG Interpretation GuideMark Norriel CajandabPas encore d'évaluation
- Physiology questions topic wiseDocument18 pagesPhysiology questions topic wisekoutharapu lasyapriyankaPas encore d'évaluation
- 2022ABFM ITEMultChoiceDocument71 pages2022ABFM ITEMultChoiceMaryam FadahPas encore d'évaluation
- Notes in PE and HEALTH (Grade 11)Document9 pagesNotes in PE and HEALTH (Grade 11)disneymovies143Pas encore d'évaluation
- Krok2 - Medicine - 2014Document24 pagesKrok2 - Medicine - 2014ashighaPas encore d'évaluation
- PulsioFlex PiCCO Data InterpretationDocument8 pagesPulsioFlex PiCCO Data InterpretationghuoiPas encore d'évaluation
- Cardiac Care Nursing PlanDocument4 pagesCardiac Care Nursing PlanAl GreigPas encore d'évaluation
- Jose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseDocument2 pagesJose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseRaymond SantiagoPas encore d'évaluation
- Grand Case Presentation Repaired)Document45 pagesGrand Case Presentation Repaired)hulaanmuakoPas encore d'évaluation
- Human Physiology in An Aquatic EnvironmentDocument47 pagesHuman Physiology in An Aquatic EnvironmentMARIA CAMILA RENGIFO CAICEDOPas encore d'évaluation