Académique Documents
Professionnel Documents
Culture Documents
Introduction
Transféré par
raisamahmudah0 évaluation0% ont trouvé ce document utile (0 vote)
17 vues12 pageshemoragic post partum
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documenthemoragic post partum
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
17 vues12 pagesIntroduction
Transféré par
raisamahmudahhemoragic post partum
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 12
INTRODUCTION
Endometriosis is a common gynaecological condition affecting about 610% of women
of reproductive age and can be a debilitating disease. It is the second most common
reason for surgery in premenopausal patients.
It is defined as the presence of endometrial-like tissue outside the uterine cavity,
leading to a chronic inflammatory reaction. The exact aetiology is unknown, but the
retrograde menstruation model is the most widely accepted theory explaining the development
of pelvic endometriosis. According to this model, menstrual blood containing endometrial
fragments passes through the fallopian tubes into the pelvic cavity, resulting
in the formation of peritoneal endometrial deposits. There are three distinctive pathological
types of pelvic endometriosis: superficial peritoneal implants, ovarian endometriomas,
and deep infiltrating nodular lesions. The extent of the disease is very variable
and often does not correlate with the severity of symptoms. Although it can sometimes
be asymptomatic (in about 20% of cases), endometriosis is frequently associated with
severe pain and infertility. Several management options exist for endometriosis and the
choice depends on several factors such as age, fertility, severity of the symptoms, and
extent of the disease.
This review presents three different cases of endometriosis with different complexities
and presentations. The diagnosis and various medical and surgical treatment
options available to the clinician will be discussed.
Pathological Types of Endometriosis
Superficial peritoneal endometriosis: peritoneal implants consist of glandular and
stromal tissue and respond to the hormonal changes associated with the menstrualGYNAECOLOG
cycle showing cyclical changes similar but not identical
to the normal endometrium. These implants
heal by fibrosis.
Deep infiltrating (adenomatous) endometriosis:
this type of endometriosis is characterized
by proliferative fibromuscular tissue with sparse
endometrial glandular and stromal tissue (similar to
adenomyosis), with no surface epithelium. Unlike
the peritoneal endometriosis, deep endometriosis
does not show significant changes during the menstrual
cycle. These nodules are typically present in
the recto-vaginal space and can involve the uterosacral
ligament, the posterior vaginal wall, and the
anterior rectal wall. They can also extend laterally
and affect the ureters.
Ovarian endometriomas: an endometrioma
is an ovarian cyst lined by endometriotic tissue and
containing dark brown or chocolate-coloured fluid,
which results from recurrent chronic bleeding from
the endometriotic implants. In long-standing endometriomas,
the endometriotic tissue is gradually
replaced by fibrotic tissue.
CASE 1
A 17-year-old patient presented to her general
practitioner with a 6-month history of severe and
excruciating dysmenorrhoea. Pelvic examination revealed
no abnormality, and a diagnosis of primary
physiological dysmenorrhoea was made. The general
practitioner prescribed painkillers in the form
of non-steroidal anti-inflammatory drugs, which
provided some benefit. However, the dysmenorrhoea
continued to disrupt the patients life, and
she was eventually referred to the gynaecologist.
Pelvic examination by the gynaecologist revealed
tenderness over the utero-sacral ligaments and on
cervical movement. A transvaginal ultrasound scan
revealed no pelvic abnormality. The gynaecologist
made a provisional diagnosis of endometriosis and
prescribed combined oral contraceptive pill (COCP).
Three months later, the patient reported a significant
improvement of her pain, but continued to experience
some degree of dysmenorrhoea. She was
therefore advised to tricycle the pill.
PRESENTATION
What Are the Main Presenting Symptoms
for Endometriosis?
The main presenting symptoms of endometriosis
include chronic pelvic pain and infertility. Patterns
of chronic pelvic pain caused by endometriosis include
dysmenorrhoea, non-cyclical pelvic pain, and
dyspareunia. The pain may also be associated with
other cyclical symptoms, particularly related to the
involvement of the urinary or gastrointestinal (GI)
tract with endometriosis. The severity of these
symptoms does not necessarily correlate with the
extent of the disease when diagnosed at laparoscopy,
as mild disease can cause severe symptoms.
On the other hand, about 20% of women with advanced
endometriosis have no symptoms.
Dysmenorrhoea is the
most common presenting
symptom, affecting up
to 80% of women
with endometriosis
GYNAECOLOGY I G PYeNerA ERCevOiLeOwGedY
Dysmenorrhoea: this is the most common
presenting symptom, affecting up to 80% of women
with endometriosis. It is often described as severe
and debilitating and does not respond to simple analgesia.
The pain classically starts 12 weeks before
the onset of menstruation and gradually worsens,
reaching a peak in severity during the first 2
days of the menstrual flow. The pain then gradually
lessens until it disappears at the end of the period.
Non-cyclical pelvic pain: this affects up to
a third of patients with endometriosis. It is often
associated with adhesions, large ovarian endometriomas,
peritoneal inflammation, and bladder or
bowel endometriosis. Pain resulting from pelvic adhesions
is usually provoked or worsened by certain
body movements. Other pains may be triggered by
ovulation, bowel movements (dyschezia), or urination.
All types of non-cyclical pains often worsen
around the time of menstruation.
Deep dyspareunia: this affects about a third
of patients with endometriosis and is mainly seen
in advanced disease with deep infiltrating nodules.
It may be severe enough to force the patient to
abstain from intercourse. The pain is usually described
as a stabbing pain on deep penetration. It
is triggered by pressure on the scarred utero-sacral
ligaments, recto-vaginal nodules or adhesions obliterating
the pouch of Douglas, or involving the
ovaries. The symptoms are typically worse before
menstruation.
DIAGNOSIS
How Would You Diagnose Endometriosis in
Adolescents?
Symptoms: adolescents with endometriosis often
present with acyclic and/or cyclic pelvic pain.
Bowel and bladder symptoms are also common in
this group of patients. Chronic pelvic pain severe
enough to disrupt normal activities and school at-
tendance in adolescents is suggestive of endometriosis.
The presence of the classical patterns of
pain described above has a sensitivity of 76% and
a specificity of 58% in detecting endometriosis.
Around 30% of adolescents with chronic pelvic pain
have endometriosis. Adolescents with pelvic pain
not responding to analgesia and/or the COCP have
about a 70% prevalence of endometriosis.
Analysing the pattern of pelvic pain is crucial
in establishing the diagnosis of endometriosis in
adolescents. A pain diary documenting the frequency
and character of the pain will help to determine
whether the pain is cyclical and if it is related to
bowel or bladder function. A family history of endometriosis
is correlated with a higher likelihood of
endometriosis in these patients.
Although, endometriosis is the commonest
cause of chronic pelvic pain in adolescents, otherGYNAECOLOGY I Peer Reviewed
causes such as sexual abuse, ovarian tumour or
genital tract anomalies, eg, imperforate hymen
should be considered.
Examination: pelvic examination, which may
not be possible in adolescents, does not usually reveal
specific signs in most patients with endometriosis.
However, this examination is important mainly
to rule out other causes of chronic pelvic pain such
as ovarian tumour or genital tract anomalies. In
adolescents who are not sexually active, bimanual
rectalabdominal examination may be considered
as it is better tolerated than a bimanual vaginal
abdominal examination. A number of signs can be
detected in some patients with endometriosis, including
thickening, nodularity and tenderness over
the uterosacral ligaments, fixation and retroversion
of the uterus, and fullness or a mass in the pouch
of Douglas.
Differential diagnosis: this includes all gynaecological
and non-gynaecological conditions
that cause chronic pelvic pain. Gynaecological
disorders include primary dysmenorrhoea, sexual
abuse, ovarian cysts/tumours, and genital tract
anomalies. In sexually active adolescents, pelvic
adhesions should also be considered (due to a
previous pelvic inflammatory infection) in the differential
diagnosis. Non-gynaecological diseases to
be considered in the differential diagnosis include
irritable bowel syndrome, inflammatory bowel disease,
interstitial cystitis, and musculoskeletal pain.
Imaging: this is of limited value in the diagnosis
of endometriosis. A transvaginal ultrasound
scan is useful in detecting endometriomas; however,
endometriomas are rarely seen in adolescents.
Magnetic resonance imaging is of value in identifying
the presence and the extent of deeply infiltrating
lesions. It may also help in detecting bowel and
ureteric involvement.
Laparoscopy: this is the gold-standard for
the diagnosis of endometriosis. However, in adolescents,
this procedure should only be considered
in patients with disabling pain not responding to
analgesia and/or the COCP. Ideally, a laparoscopic
surgeon competent in managing endometriosis surgically
should perform the procedure. The surgeon
should also be comfortable operating on adolescents
and be familiar with all the various morphologies
of endometriosis. Clear, red, white, and/or
yellow-brown lesions are more frequently found in
adolescents than black or blue lesions. The procedure
carries a 3% risk of minor complications and
a 0.61.8/1,000 risk of major complications such as
bowel perforation and vascular damage (Box 1).
MEDICAL TREATMENT OF
ENDOMETRIOSIS IN ADOLESCENTS
What Are the Available Medical Treatment
Options That You Would Like to Discuss
With This Young Patient?
Non-hormonal medical therapy (analgesia):
empirical treatment with analgesics for chronic
pelvic pain with a pattern suggestive of endometriosis
(without a definitive diagnosis) should be
considered as a first-line treatment option in adolescents.
Non-steroidal anti-inflammatory drugs
(eg, mefenamic acid or diclofenac) can be effective.
The administration of these medications should be
limited to episodes of pains lasting for a few days,
eg, dysmenorrhoea.
Hormonal therapy:
1. The COCP is a good choice for adolescents withGYNAECOLOGY I G PYeNerA ERCevO
possible endometriosis and can be used as an alternate
first-line therapy. It improves dysmenorrhoea
and offers a reliable method of contraception. COCP
is generally well tolerated, safe, and inexpensive.
Another advantage of the pill is that it can be used
as long-term therapy. Tricycling the pill reduces the
number of bleeds and the associated pain. Possible
side effects include weight gain, headaches,
nausea, breast enlargement, and depression. Patients
should be warned about the increased risk of
thromboembolism during COCP administration.
2. Gonadotrophin-releasing hormone (GnRH) agonists:
the empirical use of GnRH agonists in adolescents
without a definitive diagnosis of endometriosis
is controversial. Although, it may help to
avoid laparoscopic surgery, GnRH agonists could
adversely affect the final bone density formation,
particularly in patients younger than 17 years. Furthermore,
a definitive diagnosis and staging with
laparoscopy may be necessary to plan long-term
management of endometriosis, which is potentially
a progressive disease with no cure (Boxes 2 and 3).
CASE 2
A 38-year-old woman presented to the gynaecology
outpatient clinic with a 12-month history of
worsening intermittent lower abdominal and pelvic
pain, and severe dyspareunia. The pains were
severe enough to disrupt her life and sexual relationship.
A recent severe episode of the pain led to
an emergency admission to the hospital. She had
no previous surgery and had completed her family,
having had one child delivered vaginally in the past.
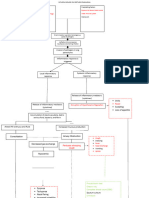
Box 3. Management options
Medical
Non-hormonal: simple analgesia (paracetamol, NSAID, codeine)
Hormonal treatment: COCP, progestogens, GnRH analogues
Surgery
Conservative: excision or ablation of endometriotic deposits,
excision or ablation of ovarian endometriomas and excision of
deep infiltrating endometriosis
Radical: TAH BSO
BSO= bilateral salpingo-oophorectomy; COCP = combined oral contraceptive pill ; GnRH = gonadotrophin-releasing
hormone; NSAID = non-steroidal anti-inflammatory drug; TAH = total abdominal hysterectomy.
Box 2. Factors to consider when planning endometriosis
treatment
Age
Need to preserve fertility
Need for contraception
Presenting symptoms (pain, infertility)
Severity of pain and impact on quality of life
Type, extent and location of endometriotic lesions
Involvement of other non-gynaecological systems
Expertise of clinician
Availability of resources
Patients preference
The empirical use of
GnRH agonists in adolescents
without a definitive
diagnosis of endometriosis
is controversial
JPOG MAY/JUN 2012 98
GYNAECOLOGY I Peer Reviewed
Pelvic examination revealed tenderness affecting
the right adnexa and the pouch of Douglas. She
underwent a laparoscopy, which revealed widely
spread deposits of active peritoneal endometriosis
affecting both ovarian fossae, the utero-sacral ligaments,
the pouch of Douglas, and the utero-vesical
peritoneal fold. Extensive adhesions were also
present between the bowel and anterior abdominal
wall. All endometriotic deposits were ablated with
electro-diathermy, and the adhesions were divided
with scissors. At post-operative follow-up, her pain
and dyspareunia were much improved. However, 6
months later she experienced a recurrence of her
symptoms. She was then counselled regarding
further management options and decided to take
a 6-month course of GnRH agonist. This improved
her pain dramatically, and she found the side effects
manageable. However, a few months after the
completion of GnRH agonist therapy, the symptoms
started to recur. The patient returned to clinic requesting
a hysterectomy as a more definitive treatment
for her pain.
MEDICAL MANAGEMENT
What Is the Current Role of GnRH Agonists
in Endometriosis?
How Do GnRH Agonists Work and What
Should You Warn the Patient About?
How Can You Treat Potential Side Effects
and How Long Would You Prescribe the
Treatment for?
GnRH agonists are usually offered as a second-line
medical therapy for endometriosis in patients with
severe symptoms not responding to analgesics or
COCP. They are also a good option for women experiencing
persistence or recurrence of severe symptoms after conservative surgery as is in our case.
GnRH agonists cause an initial stimulation of
the GnRH receptors on the gonadotrophs of the anterior
pituitary gland, followed by inhibition due to
loss of these receptors (known as receptor downregulation).
The resulting fall in follicle-stimulating
hormone leads to a pseudo-menopausal status with
oestrogen deficiency due to ovarian suppression.
Prolonged oestrogen deficiency eventually causes
atrophy of the ectopic endometrial tissue with subsequent
relief of pain. The initial stimulation often
causes worsening of the symptoms during the first
2 weeks of treatment. Patients may also experience
irregular bleeding during the first 2 months of
GnRH agonist therapy, but amenorrhoea then usually
ensues. About 80% of patients start to experience
improvement or complete relief of pain about
4 weeks after the initiation of treatment. This improvement
will continue throughout the 6-month
course of GnRH analogue therapy. However, the
majority of patients will experience a recurrence
of symptoms few months after discontinuation of
treatment. GnRH agonists are given as injections
either on a monthly or 3-monthly basis. Side effects
include menopausal symptoms of hot flushes, night
sweats, mood changes, and vaginal dryness. The
most worrying potential side effect is a 56% loss
of bone mineral density. This limits the safe use of
GnRH agonists to 6 months. The bone loss usually
recovers partially after 612 months of discontinuation
of GnRH agonists. The hypo-oestrogenic side
effects and bone mineral loss can be significantly
reduced by the daily administration of tibolone
2.5 mg as an add-back therapy. In some patients,
it may be necessary to continue the GnRH agonist
therapy beyond 6 months (unlicensed use). It is recommended
in these cases to monitor bone density
on a yearly base.
CONSERVATIVE SURGERY
Compared with medical therapy, surgery offers
a more definitive treatment of endometriosis and
tends to achieve longer lasting improvement of
symptoms. The principles of surgical treatment of
endometriosis include ablation, vaporization or excision
of peritoneal implants, excision or ablation
of endometriomas, excision of deep infiltrating
nodular endometriosis, and restoration of pelvic
anatomy by adhesiolysis. The reported incidence
of disease recurrence at 5-year follow-up is about
20% for surgery compared with about 50% for
medical treatment. However, about 30% of patients
will not experience any improvement in symptoms
after surgery. Also of note is that surgery is more
effective in reducing pain in patients with more advanced
endometriosis.
A laparoscopic approach for endometriosis
surgery is superior to laparotomy as it allows a
more thorough inspection of the pelvis with higher
Surgery is more
effective in
reducing pain
in patients with
more advanced
endometriosis
JPOG MAY/JUN 2012 100
GYNAECOLOGY I Peer Reviewed
magnification, allowing the detection of subtle endometriotic
lesions. In addition, laparoscopic surgery
minimizes trauma to tissues, resulting in less
post-operative adhesion formation. Laparoscopy is
also associated with less blood loss, and with its
magnification it allows good detection and control
of small bleeders. From the patients perspective,
laparoscopic surgery shortens hospital stay and allows
quicker return to normal activities.
The stage and severity of endometriosis should
be assessed and documented at laparoscopy by describing
the findings and using the revised American
Fertility Society classification system (stages
IIV). Systematic inspection of the whole pelvis and
abdominal cavity is essential. The laparoscopic surgeon
should be familiar with the different typical
and atypical forms of pelvic endometriosis. Typical
peritoneal implants are pigmented lesions including
dark powder-burn, black puckered, brown, blueblack,
and yellow deposits. Atypical non-pigmented
lesions include clear, white or red polypoid or
flame-like lesions. Other lesions include defects
(windows) in the peritoneum. Ovarian endometriomas
are thick-walled unilocular or multilocular
cysts of varying sizes (usually < 12 cm in diameter)
containing chocolate-coloured fluid due to repeated
bleeding from the endometriotic tissue. They are
typically associated with advanced endometriosis
and extensive adhesions between the affected
ovary and pelvic sidewall, back of the uterus, and
broad ligament. However, about 12% of endometriomas
are not associated with adhesions or severe
disease. Deep infiltrating endometriosis (> 5 mm
depth of infiltration) usually affects the recto-vaginal septum and uterosacral ligaments. Utero-sacral
ligament endometriosis is usually characterized by
thickening and firmness of the ligament with visible
scarring. It is therefore necessary to palpate
the utero-sacral ligament either with the end of a
blunt laparoscopic probe or by vaginal examination.
Obliteration of the pouch of Douglas occurs when
the affected rectum is pulled upwards and becomes
fixed to the back of the uterus, causing partial or
complete obliteration of the pouch of Douglas.
Minimal-to-mild peritoneal endometriosis can
either be excised or ablated with electro-coagulation
or laser vaporization. Care should be taken to
avoid thermal damage to the ureters when treating
the pelvic sidewall. Both ablation and excision of
mild endometriotic implants have been shown to be
equally effective in improving post-operative pain.
Deep infiltrating endometriosis affecting the
utero-sacral ligaments and/or recto-vaginal septum
should be completely excised.
RADICAL SURGERY
This includes total abdominal hysterectomy with
or without bilateral oophorectomy. This treatment
option should only be considered in patients who
have completed their family and have had failed
medical or conservative surgical treatments. A preoperative
trial of GnRH analogues may be helpful
in determining whether this treatment will be successful
and whether oophorectomy should also be
performed. All deep-seated endometriosis should be
removed during the hysterectomy to prevent remaining
disease from causing persistent pain. Bilateral
salpingo-oophorectomy may result in a better pain
relief with reduced chances of further surgery in
the future. However, this benefit has to be balanced
against the disadvantage of inducing menopause
with the need of hormone replacement therapy
(HRT), especially in patients under 40 (Box 4).
CASE 3
A 26-year-old lady presented with a long-standing
history of severe dysmenorrhoea and dyspareunia.
The pattern of dysmenorrhoea was typical of endometriosis
(as described above). She had been trying
to conceive for the previous 15 months without
success. She had also been troubled with indigestion
and constipation. Her GI symptoms gradually
worsened until she became unable to have solid
food and survived on fluids only. As a result, her
weight dropped dramatically from 58 to 38 kg over
a period of 6 months.
Pelvic examination revealed a fixed and retroverted
uterus, but no recto-vaginal nodules were
found.
A transvaginal ultrasound scan showed a
thick-walled, 7-cm, right ovarian cyst with internal
echoes, suggestive of an endometrioma. A diagnostic
laparoscopy was performed and showed grade
IV endometriosis with extensive adhesions involving
the bowel and completely covering the pelvic
organs. Only the superficial part of a right-sided
ovarian cyst was seen firmly adherent to the bowel,
uterus, and abdominal wall. The tubes and ovaries
could not be visualized. In view of the extent and
severity of the endometriosis and the involvement
of the bowel, no treatment was performed on that
occasion.
Post-operatively, a magnetic resonance imaging
scan was performed showing an 8-cm multi-
Box 4. Indications for surgery for endometriosis
Endometriosis detected during diagnostic laparoscopy
Presence of an endometrioma > 3 cm
Deep infiltrating disease causing significant symptoms
Endometriosis associated with severe symptoms in subfertile
patients
After failure of medical treatment to control symptoms
JPOG MAY/JUN 2012 102
GYNAECOLOGY I Peer Reviewed
Practice points
Careful assessment of the pattern of chronic pelvic pain
together with laparoscopy is the key to establishing an accurate
diagnosis of endometriosis.
Treatment should be tailored according to patients age, disease
severity and extent, fertility requirements, contraception, and
patients wishes.
In adolescents with symptoms of endometriosis, empirical
treatment with analgesics and/or combined oral contraceptive
pill (COCP) is recommended before resorting to laparoscopy.
Gonadotrophin-releasing hormone (GnRH) agonists may
adversely affect the final bone density formation in adolescents
especially those under 17.
First-line hormonal treatments include the COCP and continuous
progestogens.
Second-line medical treatment includes GnRH agonists.
Conservative surgical treatment reduces pain, improves fertility,
and offers a more definitive treatment with less chances of
recurrence.
locular cyst on the right ovary with several pelvic
deposits of endometriosis involving the bowel. In
view of the bowel involvement with endometriosis
and the severe GI symptoms, the patient was
reviewed by a colorectal surgeon who discussed
various surgical options for bowel endometriosis.
The patient was also counselled about the possible
need of a colostomy.
The patient was offered conservative surgery
through laparotomy for her extensive endometriosis.
The procedure was carried out jointly with the
colorectal surgeon.
At laparotomy, extensive adhesiolysis was carried
out freeing the bowel, uterus, tubes, and ovaries.
The right ovarian endometrioma was opened
and drained. The cyst wall was then stripped off
and sent for histology. A large segment of the colon
was found to be affected by the disease. A hemicolectomy
was therefore performed. Interestingly,
the histological examination of the resected colon
revealed coexisting Crohns disease in addition to
the endometriosis.
Two months after surgery, the patient recovered
very well, and all her pain and GI symptoms
have completely resolved. She was able to eat normally
and gradually gained weight. At this stage,
she was referred to have in vitro fertilization (IVF)
treatment.
SURGERY FOR EXTENSIVE DISEASE
What Is the Importance of Pre-operative
Assessment?
Pre-operative assessment helps to achieve an accurate
diagnosis of the stage of the disease and to assess
patients fitness for the surgery. This will help
to choose the best surgical approach and to anticipate
possible difficulties. In patients with suspected
deep infiltrating endometriosis, it is important
to exclude ureteric, bladder or bowel involvement.
A magnetic resonance imaging scan is of value in
determining the extent of deeply infiltrating lesions
and the involvement of bowel and bladder. Other investigations
of value may be a contrast enema and
intravenous urogram. The management of deeply
infiltrating lesions is very complex. Patients should
be referred to centres with the necessary expertise
and a multidisciplinary team should be involved
in the treatment. Pre-operative bowel preparation
should be considered.
What Is the Association Between Endometriosis
and Infertility and What Treatment
Option Should You Offer These Patients?
Infertility: 3040% of women with endometriosis
suffer from infertility. The mechanism of infertility
in mild endometriosis is not fully understood.
In moderate-to-severe endometriosis, infertility
results from anatomical distortion of the fallopian
tubes and the tubo-ovarian relationship due to adhesions.
Medical treatment of endometriosis does not
improve fertility. Surgery, on the other hand can
improve fertility in women with moderate-to-severe
endometriosis. Subfertile women with severe
endometriosis who have minimal or no symptoms
are better treated with IVF, which gives them a
higher pregnancy rate than surgery. On the other
hand, subfertile women with severe symptoms or
who have large endometriomas should be offered
surgery. Post-operative hormonal treatment has no
beneficial effect on pregnancy rates after surgery.
However, down-regulation with GnRH analogues
after debulking surgery for stage IIIIV disease may
be required prior to IVF. If satisfactory anatomical
restoration has been achieved with surgery, the
patient could be advised to try to conceive naturally
for 612 months before resorting to IVF. If the
anatomical outcome of surgery is suboptimal, IVF
should be considered shortly after surgery.
How Would You Treat an Endometrioma
Seen on Scan?
The management of endometriomas in patients receiving
fertility treatment is controversial. Whilst
some reproductive specialists believe that endometriomas
(> 3 cm) should be treated surgically before
assisted reproductive treatment, others argue that
surgery could significantly damage ovarian reserve,
which could consequently compromise success of
treatment. On the other hand, advocates of surgery
claim that untreated endometriomas could adversely
affect ovarian response to follicle-stimulating
hormone stimulation and could make egg retrieval
difficult. In addition, inadvertent insertion of the
egg retrieval needle into an endometrioma could
cause severe pelvic infection with abscess formation.
However, most fertility specialists would surgically
treat very large endometriomas (> 8 cm). The
optimal type of surgery for endometriomas remains
controversial. There are two main surgical approaches
to endometriomas, including excision or
ablation of the cyst wall after drainage and irrigation.
Most surgeons would excise the cyst wall as
this has been shown to be superior to ablation with
fewer recurrences. Excision of the cyst is achieved
by stripping the cyst wall off from the underlying
ovarian tissue. Bleeding points are then secured
with diathermy. Ablation of the cyst could be
achieved by laser vaporization or electrocoagulation
of the inner cyst wall. Simple aspiration of the
endometrioma is not sufficient as it is associated
with a high recurrence rate. A biopsy of the cyst
wall should always be sent for histology to exclude
rare cases of malignancy.
How Should Dyspareunia Caused by Severe
Recto-vaginal Endometriosis Be Treated?
Surgery is usually the only effective treatment for
women with severe debilitating symptoms due to
recto-vaginal endometriosis, which do not usually
respond to medical therapy. Surgery for recto-
vaginal septum endometriosis is very difficult and
requires considerable skill and experience. Traditionally,
this surgery has been performed through
laparotomy. However, more recently, a laparoscopic
approach has been developed in a few centres.
Whilst laparoscopy offers several advantages over
open surgery, it takes a considerably longer time,
which increases the risk of compartment syndrome
(an acute calf muscle ischaemia due to prolonged
pressure within the confined fascial compartment
leading to muscle necrosis). In addition to reducing
the operating time, open surgery allows careful palpation
for nodular disease, which is necessary for
accurate determination of the extent of the disease.
This type of surgery is usually carried out jointly
with a colorectal surgeon (and sometimes an urologist)
who may not be comfortable performing this
complicated surgery laparoscopically.
The recto-vaginal space is accessed by mobilizing
the rectum and the nodules removed until normal
tissue is identified. Depending on the extent of
rectal involvement, removal of endometriotic tissue
from the rectum can be achieved by shaving the anterior
wall, disc resection, anterior wall resection,
or segment resection. Occasionally, a temporary colostomy
may be necessary in severe cases.
CONCLUSION
Endometriosis can be a very complex condition to
treat, and it is important to tailor the treatment to
the individual patient. As we have seen, medical
treatment may be a very good option for an adolescent
like Case 1 but would not be appropriate in
someone seeking to get pregnant like Case 3. More
invasive treatment is necessary if the initial conservative
therapy is not effective or if the disease
is more advanced. Again, in these cases, patients
wishes must be kept into consideration. A hysterectomy,
although a good option for Case 2, would not
be appropriate for Case 1 or 3.
2011 Elsevier Ltd. Initially published in Obstetrics, Gynaecology &
Reproductive Medicine 2011; 21(4):112117.
About the Authors
Francesca Raffi is a Clinical Research Fellow at Royal Derby Hospital,
Derby, UK. Saad Amer is Associate Professor of Obstetrics and Gynaecology
at Royal Derby Hospital, Derby, UK
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- 3 Silhouet SignDocument79 pages3 Silhouet Signricky rdnPas encore d'évaluation
- Istc Report Short VersionDocument4 pagesIstc Report Short Versiontri_wahyudianto_1Pas encore d'évaluation
- ADocument1 pageAraisamahmudahPas encore d'évaluation
- Buku Harian: Internsip Dokter IndonesiaDocument1 pageBuku Harian: Internsip Dokter IndonesiaraisamahmudahPas encore d'évaluation
- PSQI ScoringDocument2 pagesPSQI ScoringNita HerdiantiPas encore d'évaluation
- Jadwal Pos THTDocument1 pageJadwal Pos THTraisamahmudahPas encore d'évaluation
- NoteDocument1 pageNoteraisamahmudahPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Neonatology Thesis TopicsDocument7 pagesNeonatology Thesis Topicspwqlnolkd100% (1)
- Positive and Negative Syndrome Scale (Panss)Document2 pagesPositive and Negative Syndrome Scale (Panss)Cruizer Davis100% (1)
- MCQs LADocument29 pagesMCQs LAPadmavathi C100% (1)
- I Nengah Kundera, Mursito Bialangi: 1. PendahuluanDocument6 pagesI Nengah Kundera, Mursito Bialangi: 1. PendahuluanDesak Putu Widya AprilianiPas encore d'évaluation
- JAT - CHT 13Document68 pagesJAT - CHT 13j_smith24Pas encore d'évaluation
- GC-#1580121-V1-Naphcare #70624-23 Inmate Health Care Services AgreementDocument110 pagesGC-#1580121-V1-Naphcare #70624-23 Inmate Health Care Services AgreementActionNewsJaxPas encore d'évaluation
- Epilepsy and Pregnancy Gynae Course 2013Document57 pagesEpilepsy and Pregnancy Gynae Course 2013Anas KhanPas encore d'évaluation
- General Physiology: APEC Exam Study NotesDocument9 pagesGeneral Physiology: APEC Exam Study NotesKC PalattaoPas encore d'évaluation
- What Causes Oral HematomaDocument2 pagesWhat Causes Oral HematomaAlvia D L CaninaPas encore d'évaluation
- Alan Immerman - Health Unlimitred PDFDocument95 pagesAlan Immerman - Health Unlimitred PDFHMPas encore d'évaluation
- Test Bank For Equipment Theory For Respiratory Care 5th Edition by WhiteDocument11 pagesTest Bank For Equipment Theory For Respiratory Care 5th Edition by Whiteharoldbrownorcnxeijgd100% (29)
- The Organism Prearranged Recognition Theory: By: Luz P. Blanco PH.DDocument32 pagesThe Organism Prearranged Recognition Theory: By: Luz P. Blanco PH.Dlwinntech100% (1)
- Total Relaxation: The Complete Program For Overcoming Stress, Tension, Worry, and FatigueDocument0 pageTotal Relaxation: The Complete Program For Overcoming Stress, Tension, Worry, and FatigueadtadPas encore d'évaluation
- GRANDPAR-PATHOPHYSIOLOGY-4 (1) Pertusis Whooping Cough Secondary To PneumoniaDocument5 pagesGRANDPAR-PATHOPHYSIOLOGY-4 (1) Pertusis Whooping Cough Secondary To PneumoniaJustin AlejoPas encore d'évaluation
- Orthopedic NursingDocument201 pagesOrthopedic NursingMitch Hellgirl Almonte100% (2)
- Crio Na Artite ReumatoideDocument13 pagesCrio Na Artite ReumatoideThiago Penna ChavesPas encore d'évaluation
- Tetralogy of Fallot Case PresentationDocument32 pagesTetralogy of Fallot Case PresentationUday Kumar50% (2)
- Clinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyDocument9 pagesClinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyAsmat BurhanPas encore d'évaluation
- MRSPTU M. Sc. (Anaesthesia and Operation Theater Technology) (1-4 Sem Scheme) (1st Sem Syllabus) 2021 Batch OnwardsDocument12 pagesMRSPTU M. Sc. (Anaesthesia and Operation Theater Technology) (1-4 Sem Scheme) (1st Sem Syllabus) 2021 Batch OnwardsMamta SharmaPas encore d'évaluation
- Principles of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998Document1 144 pagesPrinciples of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998BOC100% (1)
- Sinus TachycardiaDocument87 pagesSinus TachycardiaMartin huntPas encore d'évaluation
- Faktor-Faktor Yang Berhubungan Dengan Kejadian Dermatitis Atopik Di Puskesmas Bangkinang KotaDocument10 pagesFaktor-Faktor Yang Berhubungan Dengan Kejadian Dermatitis Atopik Di Puskesmas Bangkinang KotaAsha NopatiPas encore d'évaluation
- Congenital Anomaly 15-09-2015Document116 pagesCongenital Anomaly 15-09-2015gibranPas encore d'évaluation
- Gender Identity Disorder Not Otherwise SpecifiedDocument4 pagesGender Identity Disorder Not Otherwise SpecifiedJona AddatuPas encore d'évaluation
- The Effect of Iron (Fe) Tablets To The Anemia Status of Adolescent WomenDocument5 pagesThe Effect of Iron (Fe) Tablets To The Anemia Status of Adolescent WomenNani MulyatiPas encore d'évaluation
- Care PlanDocument2 pagesCare PlanLorina Lynne ApelacioPas encore d'évaluation
- 4 2 HomeworkDocument8 pages4 2 HomeworkShawntel IsordiaPas encore d'évaluation
- Barry S. Fogel, Donna B. Greenberg-Psychiatric Care of The Medical Patient-Oxford University Press (2015) PDFDocument1 813 pagesBarry S. Fogel, Donna B. Greenberg-Psychiatric Care of The Medical Patient-Oxford University Press (2015) PDFhalamadrid77100% (2)
- How I Use The Evidence in Dysphagia Management (2) : A Question of TasteDocument3 pagesHow I Use The Evidence in Dysphagia Management (2) : A Question of TasteSpeech & Language Therapy in Practice100% (3)
- Acute Stress Disorder 1Document22 pagesAcute Stress Disorder 1Seiska MegaPas encore d'évaluation