Académique Documents
Professionnel Documents
Culture Documents
Acute Stroke Management by Carlos L Chua
Transféré par
Remaica Hernadez100%(1)100% ont trouvé ce document utile (1 vote)
62 vues61 pagesACUTE STROKE MANAGEMENT BY CARLOS
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentACUTE STROKE MANAGEMENT BY CARLOS
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
100%(1)100% ont trouvé ce document utile (1 vote)
62 vues61 pagesAcute Stroke Management by Carlos L Chua
Transféré par
Remaica HernadezACUTE STROKE MANAGEMENT BY CARLOS
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 61
CARLOS L CHUA, MD, FPNA
UP- PHI LI PPI NE GENERAL HOSPI TAL
PRESI DENT, STROKE SOCI ETY OF THE PHI LI PPI NES
. Before the Specialist
Arrives
ACUTE STROKE
MANAGEMENT
ACTIONS taken during the 1
st
few hours of stroke
will determine the quality of patients existence
for the rest of his LIFE
97% of acute stroke patients are seen initially by non-neurologist
Yu R, San Jose C, Gan R. Journal of Neurological Sciences 2002, 199(1-2): 49-54
N= 259 patients
Infarction
CBF < 10 ml/100 gm/min
Cytotoxic edema
Irreversible ischemia
Ischemic Penumbra
CBF 18 -35ml / 100 gm/min
Neuronal Paralysis
Reversible ischemia
Target of Ischemic Stroke Therapy
Ischemic
Penumbra
Core infarct
How to salvage the Penumbra ?
1. RECANALIZATION STRATEGIES:
THROMBOLYTIC
THERAPY
30 % more likely to have
minimal to no disability at
3 months if given within 3
hrs
rTPA treatment produced
an absolute increase of 11-
13% in favorable outcome
NINDS rTPA Stroke Study Group, N Eng J Med 1995; 333: 1581-57
In carefully selected patients..
How to salvage the Penumbra ?
2. NEUROVASCULAR PROTECTION strategies
singly or in combination that antagonize the injurious
biochemical & molecular events leading to cell death
A. Physiologic BP, Oxygen,
Glucose, Temperature,
Fluid
B. Pharmacologic Citicoline,
Cerebrolysin
5 H OF Neurovascular Protection
The Problem with Ischemic Stroke:
Fate of the Penumbra
Ineffective
Reperfusion & Neuroprotection over Time
Core
Core
The Problem with Hypertensive ICH
Hematoma expansion can occur within the first 24 hours
Frequently associated with early neurological deterioration or
death
RACE against TIME
What to do in acute stroke ?..
IMPORTANT LINKS in STROKE CHAIN of
SURVIVAL & RECOVERY
Rapid recognition and reaction to stroke warning
signs
Rapid EMS dispatch
Rapid EMS transport to facilitates capable of
acute stroke care
Rapid diagnosis & treatment in the hospital
STROKE CHAIN of SURVIVAL &
RECOVERY
Detection Dispatch Delivery
Door Data
Decision
Drugs
US Brain Attack Alert Program, 1996
7 D Program
1 2 3
4
5
6 7
1
Detection by Patient or witness
Recognize : the signs of Stroke
1
Detection by Patient or witness
React !
Call for help or Go immediately to ER
TIME
OF ONSET
ASSESS FOR : ASK FOR:
1
Detection
2
Dispatch
3
Delivery
by EMS
Facial
asymmetry
Arm
weakness
Speech
Difficulty
Cincinnati Prehospital Stroke Scale
Alert : receiving hospital
1
Detection
2
Dispatch
3
Delivery
by EMS
If possible, check glucose and administer oxygen
ManagementPriorities (A,
B, C)
Emergent Diagnostics
Early Specific Treatment
To the Internists & Generalists : Remember
ER Stroke Therapy Timelines :
Before the specialists.
0 min EDarrival. Immediate TRIAGE
< 10 mins
Complete MD evaluation
Assess ABCs
Establish time of onset
Obtain IV access and blood samples
Provide oxygen if hypoxemic
Check glucose. Correct hypo or
hyperglycemia
Obtain 12 L ECG, Neuroimaging
Alert Brain Attack Team
irway
reathing
irculation
ensorium
A
B
C
S
General assessment
4
Door
Immediate stabilization of the ABCs
Secondary assessment of
neurological deficits & other
co-morbidities
Rule out stroke mimickers
Identify other conditions requiring
immediate attention
Determine potential causes of stroke
for early secondary prevention
Sudden, focal, negative signs / deficits
Establish time of onset (single most important info!)
Perform focused neurological exam (GCS, NIHSS)
4
Door
5
Data
Diagnosis of Stroke
4
Door
5
Data
Inquire from History & rule out Mimickers
Risk factors for atherosclerosis
Previous stroke (Infarct / ICH)
Seizures
Migraine
Infection
Head Trauma
Psychiatric or conversion disorder
Previous or recent surgery
History of Bleeding
Recent MI
Medications
Stroke vs stroke mimicker
Stroke / TIA likely Stroke/TIA less likely
(+) stroke risk factor No vascular risk factor
Definite focal signs/symptoms Isolated facial nerve involvement
Clear, exact time of onset Isolated dizziness, vertigo
Irregular cardiac rhythm Seizures at onset; fever at onset
Abnormal visual fields Weakness with atrophy
Abnormal eye movements Signs & symptoms not consistent
with neuroanatomic or vascular
distribution
Check if patient fulfills criteria for dx of stroke : acute onset, neurological syndrome
referable to a vascular territory , lasting for few minutes (TIA) or hours
ROSIER SCORE
Recognition of Stroke in the Emergency Room
NEW SYMPTOMS Score
Unilateral facial weakness 1
Unilateral arm weakness 1
Unilateral leg weakness 1
Speech disturbance 1
Visual field defect 1
Loss of consciousness or syncope - 1
Any seizures - 1
Score > 0 strongly suggests acute stroke
Score -2 to 0 are less likely to be stroke
IN THE ER, prioritize:
1.CBC with platelet count
2. PT-INR, PTT
3. CBG
4. Non-contrast
Cranial CT scan
or Cranial MRI-DWI
5. 12 L ECG
4
Door
5
Data
Identify the lesion (is it a stroke?)
Determine the type of stroke (ischemic or hemorrhage?)
Localize the stroke (where is it?)
Quantify the lesion (how large is it?)
Determine the age of the lesion (old or new?)
If hemorrhagic, what is the possible etiology ?
Rationale of Early Neuroimaging
Assessment
Conventional Non-Contrast CT scan
Fast, widely available, relatively inexpensive
Easily obtained on patients with monitors
Excludes hemorrhage, mimickers such as tumors
Used to determine eligibility for rTPA treatment
BUT may be normal in 60% in the first 0-6 hrs
of ischemic stroke (limited sensitivity)
Cranial MRI in Acute Stroke
Markedly increased sensitivity for acute ischemic stroke
DWI positive within 90 minutes of stroke
Must include GRE sequence to rule out hemorrhage
CT scan at 1.5 hrs MRI-DWI scan at 2.5 hrs
0 min EDarrival. Immediate TRIAGE
< 10 mins
ED staff
< 15 mins
Neurologist Assessment
Review history
Review Neuro exam
ER Stroke Therapy Timelines :
With the Neurology specialists.
4
Door
5
Data
6
Decision
for IV rTPA
THERAPY of ACUTE STROKE means more
than just THROMBOLYSIS ..
PHYSIOLOGIC
5H
CONCEPT OF NEUROVASCULAR PROTECTION
PHARMACOLOGIC
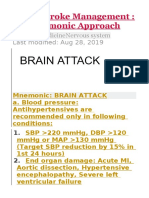
Hypertension
Hyperglycemia
Hypoxia
Hyperthermia
Hypovolemia
Citicoline
Cerebrolysin
Allow permissive
hypertension please !
Treat only if with any of the ff:
SBP > 220 or DBP > 120 or
MAP > 130mm Hg
BP Management in Ischemic Stroke
MAP = SYSTOLIC + 2X DIASTOLIC
3
Why Rapid Lowering of BP in Acute
Stroke is NOT Recommended
1. In acute ischemic stroke, autoregulation is paralyzed
in the affected tissues with CBF passively following
MAP. Rapid BP lowering can lead to further
perfusion in the penumbra
2. HPN is typically present in acute stroke, with
spontaneous decline within the first 5 - 7 days
3. ICP during the acute phase of large infarcts
reduces the net CPP
4. Several reports document neurological
deterioration from significant
pharmacologic lowering of BP
Britton, M. et al. Acta Med Scandinavia 1980
Ahmed, N. et al. INWEST. Stroke 2000: 31: 1250 - 1255
Oliveiria - Filho J. et al. Neurology 2003
Castillo, J et al. Stroke 2004
Why Rapid Lowering of BP in Acute
Stroke is NOT Recommended
Candesartan for the Treatment of Acute
Stroke (SCAST)
Sandset, E et al. Lancet 2011: 377:741-750
Candesartan 4 mg day 1
to 16 mg day 3 - 7
Placebo
R
Outcome: MI, Stroke & vascular Death during the 1st
6 months
: Functional outcome (mRS) at 6 months
2029 pts within
30 hrs of stroke
SBP > 140
N = 1017
N = 1012
Sandset, E et al. Lancet 2011: 377:741-750
Candesartan 147 / 82
Placebo 152 / 84
Candesartan 170 / 90
Placebo 171 / 90
Candesartan for the Treatment of Acute
Stroke (SCAST)
Candesartan Placebo HR P
Stroke, MI
/Vascular
Death
120
(12%)
111
(11%)
1.09 0.52
Progressive
Stroke
65
(6 %)
44
(4%)
1.47 0.04
Poor
Functional
Outcome
1.17 0.048
Sandset, E et al. Lancet 2011: 377:741-750
Candesartan for the Treatment of Acute
Stroke (SCAST)
How to lower BP in Acute Ischemic Stroke
BP GOAL : MAP 110
Not > 10 15 % lowering
from baseline MAP
AGENT : Use easily titratable IV
or short acting oral antiHPN
meds
Remember .
No sublingual agents
please !
C
e
r
e
b
r
a
l
B
l
o
o
d
F
l
o
w
(
m
l
/
1
0
0
g
/
m
i
n
u
t
e
)
Mean Arterial BP ( mmHg)
20 60 80 100 120 140 160
25
0
50
100
75
Normotensive
Hypertensive
Cerebral Autoregulatory Curve
& Target MAP
Sample Computation
BP = 210/110
MAP = 143 mmHg
15% of 143 = 21
Compute for the desired MAP:
143 21 = 122
The desired BP should not be lower
than 180/90.
In Hypertensive ICH : Goal is to miminize hematoma expansion &
limit tissue injury
Treat only if with any of the ff:
SBP > 180 MAP > 130mm Hg
Target MAP 110 or SBP 160
*Acute BP lowering to SBP = 140 is safe and can help
limit
hematoma expansion (INTERACT). BUT Clinical benefit
remains to be determined
BP Management in Acute ICH
Prompt determination &
monitoring of blood sugar
Treat with insulin titration if CBG
> 180 mg %
Avoid glucose containing IV fluids
Target normoglycemia
(110 - 180 mg / dl as early as the 1st
24 hrs up to first 3-5 days)
Hypo-hyperglycemia in Stroke
Parsons M, et al. Ann Neuro 2002 ; 52; 20 - 28
Hyperglycemia decreases Penumbral
salvage
1. Use normal saline (0.9% NaCl) to maintain a balanced
fluid status
2. Correct dehydration promptly, if present
3. Start IVF rate of 75 100 ml / hr
4. Avoid glucose containing or hypotonic solutions
5. Monitor intake & output regularly. Include Mannitol,
IV fluids & NGT flushes in the computation of total fluid
intake
Fluid Management in Stroke
Hypotonic solutions may worsen cerebral edema
D5 containing IVFs may promote
lactic acidosis, increase free radical production,
worsens cerebral edema and weakens blood vessels
- D5 W
- D5NM
- D5 0.3% NaCl
- D5LR
Rationale for Normal Saline
Monitor by pulse oximeter, ABG
determination
Use O2 supplementation if
hypoxic - target O
2
saturation > 95%
Secure airway in patients with
impaired sensorium or with
brainstem dysfunction
Proper head positioning
(neutral, 30 degree)
Airway Support & Oxygen in Stroke
Adams, HP et al Stroke 2007 ; 38; 1655 - 1711
Hyperpyrexia and Stroke Outcome
Fever burden maximum temperature measured during hospitalization minus
100 F (37.8 C) X no of days with temp. > 100 F
Percent In hospital mortality and fever burden
Phipps, M et al. Stroke 2011: 47:3357-3362
Cohort study 1,361 stroke patients
Search and treat source of
fever
Use paracetamol, surface
cooling measures & cold
saline IVF if temp >37.5
Endovascular cooling
Maintain normothermia
Temperature Management in Stroke
Davalos, et al. Stroke 2002;33: 2850 - 2857
OR 1.33 [1.10 - 1.62];
p = 0.0034
25.2
20.2
(n= 789) (n= 583)
Citicoline treatment
among pts with moderate
to severe stroke within 24
hours results in 33% odds
of complete recovery at 3
mos
Essential intermediate in synthesis of phospholipids
(phosphatidylcholine)
which are important constituents of neuronal membranes
Citicoline
Citicoline
(CDP choline)
Cytidine
Choline
Cytidine triphosphate
Phospho
Choline
Citicoline
(CDP choline)
PtdCho
DAG
PCCT
Death
Dependency
Need for chronic
institutional care
BMJ 1997, 314; 1151 - 1159
Stroke Unit Trialists Collaboration
25 trials , N = 4195 pts
Organized care in Acute Stroke Unit
BMJ 1997, 314; 1151 - 1159
REDUCTION IN :
SUMMARY
1. Early recognition & intervention is needed in
all acute stroke patients with the goal of
salvaging the penumbra in Cerebral infarct
while addressing hematoma expansion and
edema in ICH
2. Because of time constraint, diagnostic
investigations should be prioritized in the ER
SUMMARY
3. While rTPA therapy is best decided on by the
specialist, neuroprotective strategies remain as
important in acute stroke.
4. For patients who are rTPA ineligible,
administration of neuroprotectant drugs and
careful management of physiologic parameters
(5H) can be easily done even by internists and
generalists.
It would be wonderful if all physicians & personnel
were to work closely together
Louie Caplan, 2003
Thank you !
Neurotrophic peptide-based drug that mimics
the activity of endogenous Neurotrophic
Factors.
Neurotrophic factors
(Endogenous Brains Defense Mechanism)
- regulate processes of development and
modeling of CNS
- Regulatory role and guide recovery processes
in the brain tissue as important part of natural
response to injury
Cerebrolysin
R
Cerebolysin 30 mg IV x 10
days; n = 509
Placebo (0.9% NaCl)
N= 541
N =1070 pts with
ischemic
stroke
Can be randomized within 12 hrs
NIHSS 6 - 22
Primary Efficacy Criteria
Modified Rankin Scale, Barthel Index, NIH Stroke Scale
Evaluation as scales (as global scale) at day 90
Global test resulted in MW = 0.5002
(no significant difference found
between the study groups)
Mann Whitney test statistic
Global test of Efficacy Variable
(1- sided test for superiority, 97.5 % CI)
0.50 = equality
0.56 = slight superiority
0.64 = relevant superiority
0.71 = large superiority
CASTA Results
It is a well known fact that patients with
mildstrokes might recover with receiving
standard of care only.. & no further
improvement can be shown with the use of
Cerebrolysin
Ceiling Effect ?
In Trials : High proportion of subjects have maximum
scores on the observed variable
-4.0
-3.0
-2.0
-1.0
0.0
1.0
1 2 5 10 30 90
C
h
a
n
g
e
f
r
o
m
B
a
s
e
l
i
n
e
(
v
i
s
i
t
1
)
Day
NIHSS baseline <= 7
Cerebrolysin
Placebo
-6
-5
-4
-3
-2
-1
0
1 2 5 10 30 90
C
h
a
n
g
e
f
r
o
m
B
a
s
e
l
i
n
e
(
v
i
s
i
t
1
)
Day
NIHSS baseline > 12
Cerebrolysin
Placebo
Applying NIHSS outcome criteria among those with
baseline NIHSS > 12 indicate trend for beneficial effects
of Cerebrolysin
OR = 1.2724; 95 % CI LB 0.97 p= 0.04 )
CASTA Subgroup Analysis Results
Vous aimerez peut-être aussi
- Allen 2017Document22 pagesAllen 2017Jere AyerbePas encore d'évaluation
- ACLS Primary Survey Guide for Respiratory ArrestDocument34 pagesACLS Primary Survey Guide for Respiratory Arrest강기연100% (1)
- Approach To Ataxia: DR Jithesh R M6Document30 pagesApproach To Ataxia: DR Jithesh R M6jitheshPas encore d'évaluation
- CPG Management of StrokeDocument51 pagesCPG Management of Strokeapalaginih0% (1)
- Approach To Refractory Childhood SeizuresDocument10 pagesApproach To Refractory Childhood SeizureskholisahnasutionPas encore d'évaluation
- Seizures in Children JULIO 2020Document29 pagesSeizures in Children JULIO 2020Elizabeth HendersonPas encore d'évaluation
- Current News in CardiologyDocument428 pagesCurrent News in CardiologyDenisa DiaconuPas encore d'évaluation
- Acute COPD ExacerbationDocument65 pagesAcute COPD ExacerbationMaryam FadahPas encore d'évaluation
- Anti-Parkinsonism Drugs PDFDocument75 pagesAnti-Parkinsonism Drugs PDFSayan NagPas encore d'évaluation
- Oncology Nursing StudDocument267 pagesOncology Nursing StudMaviel Maratas SarsabaPas encore d'évaluation
- Chorea Approach PDFDocument1 pageChorea Approach PDFdrsushmakPas encore d'évaluation
- Acute Stroke Management Mnemonic ApproachDocument8 pagesAcute Stroke Management Mnemonic ApproachГурам ЧахвадзеPas encore d'évaluation
- Case 36 AscitesDocument4 pagesCase 36 AscitesMichaelPas encore d'évaluation
- GP Reg - Asthma and Spirometry 2011Document114 pagesGP Reg - Asthma and Spirometry 2011minerva_stanciuPas encore d'évaluation
- Intravenous Nutrient SolutionsDocument28 pagesIntravenous Nutrient SolutionsElsayed AhmedPas encore d'évaluation
- Anesthesiology GuideDocument4 pagesAnesthesiology GuideGeorge Wang100% (1)
- CPG Management of Atrial Fibrillation PDFDocument119 pagesCPG Management of Atrial Fibrillation PDFZee YongPas encore d'évaluation
- Nipple DischargeDocument8 pagesNipple DischargeGabriela Zavaleta CamachoPas encore d'évaluation
- Approach To TruamaDocument29 pagesApproach To TruamaIbsa ShumaPas encore d'évaluation
- Source NotesDocument30 pagesSource NotesChris Jardine Li100% (1)
- Venous ThromboembolismDocument49 pagesVenous Thromboembolismadamu mohammadPas encore d'évaluation
- Altered Tissue PerfusionDocument10 pagesAltered Tissue PerfusionLaurence ZernaPas encore d'évaluation
- Head Injury SymptomsDocument3 pagesHead Injury SymptomsMay NitayakulPas encore d'évaluation
- Diabetes Clinical GuidelinesDocument66 pagesDiabetes Clinical GuidelinesfamtaluPas encore d'évaluation
- Paediatrics PDFDocument44 pagesPaediatrics PDFNeha OberoiPas encore d'évaluation
- 10.08.07 Cardiac Tamponade HaagDocument16 pages10.08.07 Cardiac Tamponade HaagfoetorPas encore d'évaluation
- Perinatal Nurses and Eating Disorders: Examining Our Role Michelle L. LoucksDocument7 pagesPerinatal Nurses and Eating Disorders: Examining Our Role Michelle L. LoucksMichelle LoucksPas encore d'évaluation
- 03-Spinal Cord Phys & AnatDocument9 pages03-Spinal Cord Phys & AnatAzwar Arsyad S SiPas encore d'évaluation
- Cognitive Disorders Due to Medical ConditionsDocument18 pagesCognitive Disorders Due to Medical ConditionsSri HazizahPas encore d'évaluation
- Adjuvant AnalgesicsDocument44 pagesAdjuvant AnalgesicsZulfan EfendiPas encore d'évaluation
- Acutely Ill ChildDocument50 pagesAcutely Ill ChildAhmed KhanPas encore d'évaluation
- Everything You Need to Know About DiabetesDocument39 pagesEverything You Need to Know About DiabetesSubramaniam RamanPas encore d'évaluation
- MS Brain and Neurological DisordersDocument5 pagesMS Brain and Neurological DisordershaxxxessPas encore d'évaluation
- Treatment Algorithm For Autonomic Dysreflexia (Hypertensive Crisis) in Spinal Cord InjuryDocument1 pageTreatment Algorithm For Autonomic Dysreflexia (Hypertensive Crisis) in Spinal Cord InjuryHAYME THARRISPas encore d'évaluation
- TPNDocument69 pagesTPNMylz MendozaPas encore d'évaluation
- ACP PocketbookDocument91 pagesACP PocketbookjamesbeaudoinPas encore d'évaluation
- A Simple Guide to Pneumothorax (Collapsed Lungs), Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Pneumothorax (Collapsed Lungs), Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- COPD Acute Management ABCDEDocument11 pagesCOPD Acute Management ABCDESSPas encore d'évaluation
- Preventive CardiologyDocument28 pagesPreventive CardiologyerizonPas encore d'évaluation
- Inflammatory Muscle Diseases NEJM 2015 Marinos DalakasDocument14 pagesInflammatory Muscle Diseases NEJM 2015 Marinos DalakasWalther Seven VGPas encore d'évaluation
- Endocrine and Metabolic EmergenciesDocument320 pagesEndocrine and Metabolic EmergenciesReem Ben Omran100% (1)
- Hospital Acquired Infection p2Document155 pagesHospital Acquired Infection p2BethanyPas encore d'évaluation
- CTSP Case 2 - Managing Hypoglycemia and Hyperglycemia in DiabetesDocument2 pagesCTSP Case 2 - Managing Hypoglycemia and Hyperglycemia in DiabetesVanessa HermionePas encore d'évaluation
- Stroke Pathway For Acute Care ProvidersDocument5 pagesStroke Pathway For Acute Care Providersdremad1974100% (1)
- Medpage Guide To Epi and BiostatisticsDocument11 pagesMedpage Guide To Epi and Biostatisticsnet2020100% (1)
- Chronic Inflammatory Demyelinating PolyneuropathyDocument7 pagesChronic Inflammatory Demyelinating PolyneuropathyApriliaPas encore d'évaluation
- Blood Pressure Regulation SummaryDocument42 pagesBlood Pressure Regulation SummaryLouis JinPas encore d'évaluation
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDocument2 pagesDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- Fluid Resuscitation and Organ Perfusion EvaluationDocument66 pagesFluid Resuscitation and Organ Perfusion EvaluationDewiRatnasariPas encore d'évaluation
- Tubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterDocument11 pagesTubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterJeremy HamptonPas encore d'évaluation
- Pediatric Cardio-Respiratory AssessmentDocument9 pagesPediatric Cardio-Respiratory AssessmentRicky SpideyPas encore d'évaluation
- Simulation Acute Coronary Syndrome (Learner)Document2 pagesSimulation Acute Coronary Syndrome (Learner)Wanda Nowell0% (1)
- Myocardial Infarction (MI) Guide: Causes, Symptoms, Diagnosis & TreatmentDocument29 pagesMyocardial Infarction (MI) Guide: Causes, Symptoms, Diagnosis & Treatmentناصر دويكاتPas encore d'évaluation
- Head Trauma: Will/Grundy EMS 2009 2 Trimester May CMEDocument100 pagesHead Trauma: Will/Grundy EMS 2009 2 Trimester May CMESytrose Morales100% (1)
- Disasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesD'EverandDisasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesMauricio LynnPas encore d'évaluation
- Anesthesia Complications in the Dental OfficeD'EverandAnesthesia Complications in the Dental OfficeRobert C. BosackPas encore d'évaluation
- Lung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyD'EverandLung Development Biological and Clinical Perspectives: Biochemistry and PhysiologyPhilip FarrellPas encore d'évaluation
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Section 5. Atherosclerotic Peripheral Vascular Disease and Aortic AneurysmDocument23 pagesSection 5. Atherosclerotic Peripheral Vascular Disease and Aortic AneurysmsidoniavidicanPas encore d'évaluation
- Gastroenterology PT MRCP I 2019 2nd Edition PDF HXP DR NotesDocument1 142 pagesGastroenterology PT MRCP I 2019 2nd Edition PDF HXP DR NotesRami NaousPas encore d'évaluation
- Steal SyndromeDocument6 pagesSteal SyndromeDina RyantiPas encore d'évaluation
- 24 - Arterial Access - Umbilical Artery CatheterizationDocument10 pages24 - Arterial Access - Umbilical Artery CatheterizationJesica DiazPas encore d'évaluation
- Vertebral Artery Stenosis and OcclusionDocument37 pagesVertebral Artery Stenosis and OcclusionGamer MadaPas encore d'évaluation
- Dietary Management of GI DiseasesDocument12 pagesDietary Management of GI DiseasesMiguel Cuevas DolotPas encore d'évaluation
- VastarelDocument20 pagesVastarelKristen FieldsPas encore d'évaluation
- Monica Fawzy - Plastic Surgery Vivas For The FRCS (Plast) - An Essential Guide-CRC Press (2022)Document283 pagesMonica Fawzy - Plastic Surgery Vivas For The FRCS (Plast) - An Essential Guide-CRC Press (2022)TahaniPas encore d'évaluation
- Cerebrovascular AccidentDocument48 pagesCerebrovascular AccidentDr. Jayesh Patidar100% (2)
- Features of Covid Related StrokeDocument10 pagesFeatures of Covid Related StrokeAbdul AzeezPas encore d'évaluation
- Stroke Iskemik (Dr. Dr. Syahrul, SPS (K) )Document14 pagesStroke Iskemik (Dr. Dr. Syahrul, SPS (K) )YogaPas encore d'évaluation
- Ischemic Cardiac Disease: Causes, Symptoms, Diagnosis and TreatmentDocument34 pagesIschemic Cardiac Disease: Causes, Symptoms, Diagnosis and TreatmentGopala HariPas encore d'évaluation
- Hemorrhagic Stroke: Darpen Subhashbhai Mori Group 2, MD 3BDocument13 pagesHemorrhagic Stroke: Darpen Subhashbhai Mori Group 2, MD 3BDarpen MoriPas encore d'évaluation
- Pharmacology-II NIRALIDocument244 pagesPharmacology-II NIRALIRock Patel93% (29)
- Managing Medical EmergenciesDocument42 pagesManaging Medical EmergenciesRichard Starr100% (2)
- Corydalis YanhusuoDocument4 pagesCorydalis YanhusuomiadelfiorPas encore d'évaluation
- Molecules 28 05624Document30 pagesMolecules 28 05624Sayed Newaj ChowdhuryPas encore d'évaluation
- Cardiogenic ShockDocument21 pagesCardiogenic ShockIslamOteshPas encore d'évaluation
- Exercise Standards For Testing and TrainingDocument62 pagesExercise Standards For Testing and TrainingRelviGuzmanApazaPas encore d'évaluation
- Chapter Four HealingDocument70 pagesChapter Four HealingAhmed AzeezPas encore d'évaluation
- Types of StrokeDocument12 pagesTypes of Strokefakher adnanPas encore d'évaluation
- Pharmacological Management of Acute Coronary Syndromes (ACS) and Acute Limb Ischemia (ALI)Document44 pagesPharmacological Management of Acute Coronary Syndromes (ACS) and Acute Limb Ischemia (ALI)hendratj90Pas encore d'évaluation
- Dent Clin N Am 50 (2006) 625-633Document9 pagesDent Clin N Am 50 (2006) 625-633lalajanPas encore d'évaluation
- Acute Miocard InfarkDocument32 pagesAcute Miocard InfarkhansPas encore d'évaluation
- Herbs CampDocument42 pagesHerbs CampJohn JohnPas encore d'évaluation
- Acute ST Elevation Myocardial Infarction - StatPearls - NCBI BookshelfDocument9 pagesAcute ST Elevation Myocardial Infarction - StatPearls - NCBI BookshelfZ Siclayi AtlPas encore d'évaluation
- PathologyDocument30 pagesPathologyTenorski baritonPas encore d'évaluation
- Mcqs Faculty of General Medicine VI YearDocument110 pagesMcqs Faculty of General Medicine VI YearAbdimajiid100% (2)
- Cerebrovascular DiseaseDocument29 pagesCerebrovascular DiseaseKamsha UyPas encore d'évaluation
- CVA Case PresentationDocument16 pagesCVA Case PresentationgolokipokPas encore d'évaluation