Académique Documents
Professionnel Documents
Culture Documents
Jurnal Translate
Transféré par
gumilangggDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Jurnal Translate
Transféré par
gumilangggDroits d'auteur :
Formats disponibles
Mrs.
TA, 28 year old and married since 1 year, was anxious to conceive due to her irreg
ular cycles as a result of PCOS. Her age at menarche was 12 years, with menstrual cycle
s being irregular for 1-2 days every 35-45 days. She also had a history of premenstrual
pain, and tension and spotting with dysmenorrhea. She had undergone ureteroscopy f
or renal calculi twice. She also had a family history of hemophilia with two of her broth
ers being affected and her mother was a carrier. Her three maternal uncles also had he
mophilia.
She was obese with moderate hirsutism. Clinically, her uterus was normal sized, firm, a
nd mobile with al I fornices being clear. At her baseline ultrasound, the uterine size wa
s 70.6/ 33.2/42.2 mm; endometrial thickness was 6.1 mm; both ovaries were enlarged
with multiple follicles and increased stroma.
Her baseline hormone levels on day 2 of the cycle were as follows: follicle stimulating h
ormone (FSH)-5.6 mIU/ml, luteinizing hormone (LH)-5.3 mIU/ml, dehydroepiandro sulf
ate (DHEAS)-780 ng/ml, androstenidione-2.7 ng/ ml, estradiol (E2)-20.73 pg,/ml, proge
sterone (P4)-3.68 ng/ml, thyroid stimulating hormone (TSH)-9.4 uRJ/ml, free T4 (FT4)-1
.25, fasting insulin (FI)-15.8 uU/mI. Fasting Insulin levels were repeated after 3 months
of Metformin (500 mg twice a day) which were 3.1 Semen analysis done was normal.
In view of the family history of haemophilia, she was evaluated to rule out a carrier sta
te. Her prothrombin time (PT) was 13.2 s (control 12 s), activated part ialthromboplas t
in time (aPTT) 33 s (control 30 s), factor VIII c activity S6% (60-150), factor IX c assay - 6
0% (60-150), and factor XIII screening showed stable clot. Her results for PCR for carrie
r state revealed that she was not a carrier for hemophilia. Her hysterosalphingography
(HSG) showed a normal uterine cavity with a good filling of both tubes with the bilater
al spill. The right tube was morphologically normal with mild dilatation and clumping of
the distal end of the left tube. Tubal pressures were low.
She was started on 511 )1g of tablet eltroxin and tablet metrofin 50(1 mg BD. Metform
in was discontinued after 2 months due to gastrointestinal side effects.
11w first cycle was monitored without 01 drugs, with no ovulation documented after
monitoring till day 21 of the cycle. In the second cycle, clomiphene citrate (CC) 100 mg
was given from days 2 to 6, and ovulation was documented on day 22.1n the next two
cycles, the dose of CC was increased to 150 mg. Ovulation was documented on days 15
and 17. In the next three cycles letnyzole 5 mg was given from days 3 to 7, and ovulati
on was documented on day 14 or 15 of the cycle. As there was no pregnancy even with
letrazole, CC was given again in the seventh cycle. She had three mature follicles on da
y 12, when KC 5000 IL was given intramuscular, and ovulation was documented on day
s 14 and 15. Micronized progesterone vaginal pessaries were given for In teal support.
A total at 20 days alter ovulation, Il-hUG dune on November 19, 2007, was 410 mil:init.
11-1)CG was repeated again on November 22, 2007, which had increased to 1085 milit
ia USG revealed a single intrauterine (I U) sac with a gestational sac diameter (C,SD) of
4.4 mm (5 weeks 1 day).
On November 26, 2007, a repeat TVS did not show any increase in GSD (5.13 mm - 5 w
eeks 2 days). No yolk sac or fetal pole was seen. Repeat TVS after a week on December
3, 2007, documented a gestational sac of 8.4 net (5 weeks 4 days) with no yolk sac or f
etal pole seen. There was minimal tenderness in the right fomix, but no ectopic gestati
onal sac (GS) seen in either fomix. The 13-KG level on that day was 9515 which was too
high for an anembryonic pregnancy it-hce was repeated on December 6, 2C07, and W
AS 11342 mfUltrd; WS documented a GS of 10.5 nun (5 weeks 6 days) with no fetal pol
e or yolk sac seen. There was another small GS seen measuring 4 mm . There were also
two small sacs measuring 4 and 6 mm, seen in the right adenexa, the left adenexa app
earing normal with no free fluid in POD. There was no abdominal tenderness or guardi
ng or tenderness in all fornices. On December 8, 2007, the p-hCG was 12947 mIU/ ml
with IU GS of 10.5 mm (5 weeks 6 days) with no fetal pole or yolk sac The two sacs in t
he right adenexa had increased in size to 8 and 6 mm, respectively. There was no free f
luid in POD. The patient was clinically asymptomatic and stable so a decision to start m
edical therapy was taken. Inj MTX 1 mg/kg was given IM with inj. leucovorine 0.1/kg gi
ven IM on alternate days.
The patient was followed up on a regular basis clinically and by TVS. She was also closel
y monitored for -hCG, hemoglobin (HB), complete blood count (CBC), liver function te
st (LFT), and peripheral smears.
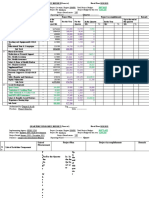
The (3-hCG levels after MTX injection were as follows:
December 12, 2007, 11,967 mIU/ml
December 14, 2007, 10,164 mIU/m1
December 17, 2007, 6292 mIU/m1
December 20, 2007, 3232 mIU/ml
December 22, 2007, 1088 mIU/ml
December 24, 2007, 791 mIU/m1
December 28, 2007, 90 mIU/m1
January 2, 2008, 9 mIU/ml.
Serial TVS done showed regression of intrauterine and right adenexal sacs. Once the
hCG levels were less than 1000 mIU/ml, the patient had per vaginal bleeding. TVS sho
wed the products in the cervical canal which were then removed under aseptic precaut
ions.
A total of six injections of MTX were given. All her blood parameters were normal thro
ughout the treatment.
Once j3-hCG was below 10 mIU/ml, she was advised not to conceive for 6 months, wit
h follow-up of p-hCG after 1 and
2 months which was normal.
After 6 months, she was again given CC for OI, and ovulation was documented on day
15. She conceived in the second treatment cycle with timed intercourse. Her -hCG 20 d
ays after ovulation was 3571 mIU/ml with an IU GS of 9 mm corresponding to 5 weeks
3 days seen on TVS. Corpus luteum was seen on the right side with no other adenexal
pathology. Repeat -hCG after 1 week was 15,000 mIU/m1. A gestational sac with yolk
sac and fetal pole corresponding to 6 weeks and 5 days was seen. Fetal heart was also
documented. She had a normal vaginal delivery at 39 weeks of gestation. She delivered
a female baby weighing 3.4 kg.
Case 2
Mrs SS presented with secondary infertility for 6 months. She had a full-term normal d
elivery female baby aged 4.5 years alive and health); after which she used harrier contr
aception fur 3 years and IUCD for 1.5 years for spacing. 1-15G done outside on Februar
y 7, 2007, showed right tubal block with the left tube filling poorly. Cannulation was do
ne under fluoroscopic guidance, after which both the tubes showed free spill. Endomet
rium was positive Ibr tuberculosis PCR. She had undergone four cycles of ovulation ind
uction, two citrate and two with gonad otrophias. She ovulated in all the cycles but her
endometrium was thin and lesser than 7.5 mm in all four cycles.
Her first scan done at our clinic was on day 19 of the menstrual cycle. The uterus was n
ormal, but the endometrium was only 7.R nun thick. Both ovaries were normal with a v
olume of 4.96 and 4.20 cm and an antral follicle count (AFC} of seven. With this histor
y and investigation report, the patient was planned for 01 with RH. Two cycles of Ur w
ere performed with tablet I .Ct razolc 5 mg, given from days 3-7. The dermal applicatio
n of EstroGel was done once the follicles were 16 mm for the treatment of thin endo
metrium. The ovulation occurred on days 13 and 15. The endometrial thickness on the
day of 1111 was 12.8 and 12.3 mm. We did two inure cycles of 1U1 with gonad ot roph
ins. Ovulation was documented on days 11 and 14 of the cycle and the endometrial thi
ckness was 11.6 and 11.1 mm. As there was no pregnancy, the patient was counselled
for in vitro teriilizatinn ([VF). Hysteroscopy was done prior to JIFF, which revealed adhe
sions at the &MILLS and both cornu. The codonwtrium was fibrotic and pearly white in
color except for a small portion oil the :Interior wall. he cavity was stnaller Ohm Hun m
at in size. Adhesiolysis was done and the patient was put on conjugated estrogen (Pre
marin) 1.25 mg twice a day for 25 days with medrosyprogesterone 10 mg twice a day f
or the last ID days. This hormone replacement therapy (I IRT) was given for 3 months.
A repeat hysteroscopy done after 3 months revealed reformation of adhesions at the Il
unduS which were rut using scissors and Fifa given again for 3 months. Before IVF, hys
teroscopy did not show any adhesions but the endometrium was thin and fibrotic on t
he posterior wall.
The protocol used fur IVF was long luteal down-regulation from day 21 with gunadotro
phins started on day 3 of the gels when the cstradiol was 18 pg/MI and progesterone
was 1.15 ng/ml. She was started on urinary FSH 30U 1U and as the estradiol level on d
ay 8 of the cycle was 6 pg/ nil and the tollicular size was 8-12 mm, the dose was increas
ed by 75 Hi and continued till day 13. On day 14, Rec. hCG 250 meg will; given subcuta
neously when there were SIX follicles 16-18 mm in d iameter. On the day tit heG, estra
diol was 3265 pg/ml and progesterone was 2.8 ng/ml. Oocyte retrieval was done 35 h l
ater. Luteal phase support was given with intramuscular inj. Gestone 100 mg (Ferring P
harmaceuticals, India). The luteal phase was monitored for ovarian hyperstimulation sy
ndrome (OHSS). Ten days after ET, -hCG was 53 mIU/m1 and a repeat level after 7 da
ys was 1030 mIU/ml. At that time, a single gestational sac was seen with a mean gestat
ional sac diameter (MGSD) of 4.5 mm corresponding to 5 weeks and 1 day. Two days la
ter, the patient complained of minimal bleeding per vaginum. The -hCG level was 125
8 mIU/ml, the MGSD was 4.6 mm and both adenexa showed multiple corpora lutea. N
o gestational sac was seen in the adenexa. One week later, the MGSD had increased to
8.5 mm which corresponded to 5 weeks and 5 days, but no fetal pole was seen and th
e bleeding had stopped. Despite the increase in the MGSD, there was no correspondin
g increase in the p-HCG levels which were 1567 mIU/ml. Two days later, the patient ha
d three syncopal attacks. On examination, the vitals were normal but there was tender
ness in the right iliac fossa and fornix. On TVS, the IU sac with yolk sac was seen, but th
ere was also a complex mass of 90 x 70 mm in the right adenexa with free fluid in POD,
which was turbid. Diagnosis of right EP with coexisting IU pregnancy was made. In vie
w of an IU pregnancy and right adenexal mass, the decision for laparoscopy was taken.
At laproscopy, right partial salpingectomy for ruptured EP was done. One week later, t
he TVS showed a irregular gestational sac with MGSD of 5.8 min and the p-hCG level w
as 820 mIU/ml. The repeat hCG level after 5 days was 418 mIU/m1 and the gestational
sac had not increased in size. Decision for a curettage was taken. One week later, the p
-hCG level was 5 mIU/ml. A frozen embryo transfer was done in a natural cycle, and a b
iochemical pregnancy was documented with the 3-hCG level going to 378 mIU/ml.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Revised List of Maharashtra HospitalsDocument16 pagesRevised List of Maharashtra Hospitalsdummy data100% (1)
- Community Medicine DissertationDocument7 pagesCommunity Medicine DissertationCollegePaperGhostWriterSterlingHeights100% (1)
- B65a RRH2x40-4R UHGC SPDocument71 pagesB65a RRH2x40-4R UHGC SPNicolás RuedaPas encore d'évaluation
- SSN Melaka SMK Seri Kota 2021 Annual Training Plan: Athletes Name Training ObjectivesDocument2 pagesSSN Melaka SMK Seri Kota 2021 Annual Training Plan: Athletes Name Training Objectivessiapa kahPas encore d'évaluation
- Capacitor BanksDocument49 pagesCapacitor BanksAmal P RaviPas encore d'évaluation
- 2022.08.09 Rickenbacker ComprehensiveDocument180 pages2022.08.09 Rickenbacker ComprehensiveTony WintonPas encore d'évaluation
- VOC & CO - EnglishDocument50 pagesVOC & CO - EnglishAnandKumarPPas encore d'évaluation
- Optical Fiber Communication Unit 3 NotesDocument33 pagesOptical Fiber Communication Unit 3 NotesEr SarbeshPas encore d'évaluation
- Mbs KatalogDocument68 pagesMbs KatalogDobroslav SoskicPas encore d'évaluation
- Benefits of Silicone Coated Glass InsulatorsDocument10 pagesBenefits of Silicone Coated Glass InsulatorsMuhammad Waseem AhmadPas encore d'évaluation
- Water TreatmentDocument27 pagesWater TreatmentArya Singh Rathod100% (1)
- Wago PCB Terminal Blocks and Connectors Catalog 7Document105 pagesWago PCB Terminal Blocks and Connectors Catalog 7alinupPas encore d'évaluation
- Virtual or Face To Face Classes Ecuadorian University Students' Perceptions During The Pandemic by Julia Sevy-BiloonDocument1 pageVirtual or Face To Face Classes Ecuadorian University Students' Perceptions During The Pandemic by Julia Sevy-BiloonPlay Dos ChipeadaPas encore d'évaluation
- LWT - Food Science and Technology: A A B ADocument6 pagesLWT - Food Science and Technology: A A B ACarlos BispoPas encore d'évaluation
- DSM-5 Personality Disorders PDFDocument2 pagesDSM-5 Personality Disorders PDFIqbal Baryar0% (1)
- SAT Subject Chemistry SummaryDocument25 pagesSAT Subject Chemistry SummaryYoonho LeePas encore d'évaluation
- Hasil Pemeriksaan Laboratorium: Laboratory Test ResultDocument1 pageHasil Pemeriksaan Laboratorium: Laboratory Test ResultsandraPas encore d'évaluation
- Current and Voltage Controls 3-Phase AC Max. Current Control Type S 178Document3 pagesCurrent and Voltage Controls 3-Phase AC Max. Current Control Type S 178Felipe FarfanPas encore d'évaluation
- Cooling Tower (Genius)Document7 pagesCooling Tower (Genius)JeghiPas encore d'évaluation
- Unit 9 Organic Law On Provincial and Local-Level Government (OLPLLG) - SlidesDocument29 pagesUnit 9 Organic Law On Provincial and Local-Level Government (OLPLLG) - SlidesMark DemPas encore d'évaluation
- Kes MahkamahDocument16 pagesKes Mahkamahfirdaus azinunPas encore d'évaluation
- This Unit Group Contains The Following Occupations Included On The 2012 Skilled Occupation List (SOL)Document4 pagesThis Unit Group Contains The Following Occupations Included On The 2012 Skilled Occupation List (SOL)Abdul Rahim QhurramPas encore d'évaluation
- Vicat Apparatus PrimoDocument10 pagesVicat Apparatus PrimoMoreno, Leanne B.Pas encore d'évaluation
- Environmental Product Declaration: Plasterboard Knauf Diamant GKFIDocument11 pagesEnvironmental Product Declaration: Plasterboard Knauf Diamant GKFIIoana CPas encore d'évaluation
- MSU-Iligan Institute of TechnologyDocument5 pagesMSU-Iligan Institute of TechnologyYuvi Rociandel LUARDOPas encore d'évaluation
- 812571-006 RevB (GPC3000 Service)Document270 pages812571-006 RevB (GPC3000 Service)BPPas encore d'évaluation
- Quarterly Progress Report FormatDocument7 pagesQuarterly Progress Report FormatDegnesh AssefaPas encore d'évaluation
- UK FreshTECH Jammer RecipeBook 0Document24 pagesUK FreshTECH Jammer RecipeBook 0Temet NoschePas encore d'évaluation
- For Hand Grip Strength: NormsDocument7 pagesFor Hand Grip Strength: NormsPraneethaPas encore d'évaluation
- Rar Vol11 Nro3Document21 pagesRar Vol11 Nro3Valentine WijayaPas encore d'évaluation