Académique Documents
Professionnel Documents
Culture Documents
Immunomodulators For Asthma
Transféré par
darmariantoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Immunomodulators For Asthma
Transféré par
darmariantoDroits d'auteur :
Formats disponibles
228
Copyright The Korean Academy of Asthma, Allergy and Clinical Immunology The Korean Academy of Pediatric Allergy and Respiratory Disease http://e-aair.org
INTRODUCTION
New information regarding the molecular mechanisms of al-
lergic disorders has led to a variety of novel therapeutic ap-
proaches. This article will briefly review the pathogenesis of
asthma and allergic diseases; discuss the rationale behind us-
ing immunomodulators in these diseases; and examine the
therapeutic efects of immunomodulators on allergic diseases.
Tis review will focus on immunomodulators that are in hu-
man clinical trials and not molecules in pre-clinical develop-
ment.
One might question why new treatments are needed when
with the advent of new and better inhaled corticosteroids with
and without long-acting B-agonists many individuals with asth-
ma are well controlled. However, as with all treatments, inhaled
corticosteroids are not efective for all individuals. Indeed, about
30%-35% of individuals, both adult and pediatric patients with
asthma, have a poor or no response to inhaled corticosteroids.
Furthermore, inhaled corticosteroids have not been shown to
prevent the progression of disease or completely reverse airway
remodeling.
1,2
Tus, there is a need for novel therapies that afect critical im-
munopathologic mechanisms and that would induce immune
tolerance; that is, change the immune system such that the ther-
apy might actually be able to be discontinued with continued
maintenance of disease control long term.
Immunomodulators for Asthma
Vesselin V Dimov, Thomas B Casale*
Division of Allergy & Immunology, Department of Medicine, Creighton University, Omaha, NE, USA
ASTHMA PATHOGENESIS
The pathogenesis of asthma involves a number of different
cells, mediators, and cytokines (Figure). It is also apparent that
particular pathways or molecules may be more important in in-
dividual patients. Tus, fnding a universal treatment that would
be clinically benefcial for all patients is a challenge.
One of the frst steps important in the pathogenesis of allergic
respiratory diseases is antigen capture and presentation. Tis is
followed by engagement of the T-cell receptor and CD3 com-
plex by MHC class II molecules on B cells. Subsequently, there
is a chain of molecular events including engagement of CD154
(CD40L) on T2 cells and CD40 on B cells, along with engage-
ment of CD28 and CD80/86 on Th2 and B cells respectively.
Tese events ultimately lead to the release of important cytok-
ines such as IL-4 and IL-13 critical for immunoglobulin E (IgE)
production. Once IgE is produced, it binds to mast cells and ba-
sophils where cross-linking of high afnity IgE receptors bound
by IgE and antigen leads to mediator and cytokine release. Im-
Review
Allergy Asthma Immunol Res. 2010 October;2(4):228-234.
doi: 10.4168/aair.2010.2.4.228
pISSN 2092-7355 eISSN 2092-7363
New information regarding the molecular mechanisms of allergic disorders has led to a variety of novel therapeutic approaches. This article briefy
reviews the pathogenesis of asthma and allergic diseases, discusses the rationale behind using immunomodulators in these diseases; and exam-
ines the therapeutic effects of immunomodulators on allergic diseases. There are a number of immunomodulators that have been developed for the
treatment of allergic disorders. Some have looked very promising in pre-clinical trials, but have not shown signifcant benefts in human clinical trials
thus indicating the disparity between mouse models and human asthma. This review focuses on immunomodulators that are in human clinical trials
and not molecules in pre-clinical development.
Key Words: Asthma; immunomodulators; cytokines; treatment
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits
unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Correspondence to: Thomas B Casale, MD, Division of Allergy &
Immunology, Department of Medicine, Creighton University, 601 North 30th
Street, Suite 5850, Omaha, NE 68131, USA.
Tel: +1-402-280-4403; Fax: +1-402-280-5961; E-mail: tbcasale@creighton.edu
Received: April 9, 2010; Accepted: April 30, 2010
There are no nancial or other issues that might lead to conict of interest.
Immunomodulators for Asthma AAIR
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 229 http://e-aair.org
portant in this process is the release of more IL-4 and IL-13 from
a number of diferent infammatory cells including mast cells,
as well as IL-9. Tese cytokines are important to propagate the
production of IgE and allergic inflammation in general. IL-5
and GM CSF are also produced and these are key molecules for
growth and diferentiation of eosinophils. Eosinophils are key
immune efector cells that can leave the blood vessel through
the interactions of adhesion molecules and chemoattractants
and migrate to the site of infammation. Tis process involves a
number of diferent molecules in addition to those mentioned
above, many of which have been targets of therapeutic inter-
ventions.
Strategies to inhibit infammatory pathways are many and in-
clude targeting the cell of origin of infammatory cytokines and
mediators, targeting the released mediator or cytokine, or in-
hibiting the efects of the released cytokine or mediator by block-
ing the mediated efects on the target cell. All of these approach-
es have been undertaken with various molecules. For example,
soluble receptors and monoclonal antibodies against key cy-
tokines such as IL-4 have undergone clinical trials. Inhibitors of
target cell receptors for these molecules have also been studied.
Tis review will focus on many diferent approaches by exam-
ining the clinical efectiveness of novel immunomodulators in-
volved in key pathogenic mechanisms.
STRATEGIES AIMED AT T-CELLS
Due to the pro-infammatory role of activated T-cells in asth-
matic airways and the observed correlation of increased CD25
expression with asthma severity, attempts have been made to
block this arm of allergic disease pathogenesis. Initial attempts
included monoclonal antibodies against T2 cells such as ke-
liximab. Although this treatment showed some modest im-
provement in patients with severe asthma, because of the po-
tential side efects, it has not been extensively studied.
Cyclosporine and tacrolimus have similar mechanisms inhib-
iting T cells and have been used for the treatment of severe asth-
ma. Cyclosporine in early studies was shown to improve pul-
monary functions in severe asthmatics, but because of side ef-
fects it has not been used extensively. An inhaled form of tac-
rolimus was used in patients with asthma, but was unsuccess-
ful in meeting primary endpoints.
Daclizumab is a humanized monoclonal IgG1 antibody that
is currently approved for the prevention of renal allograft rejec-
tion. It is specifc for CD25 expressed by activated T-cells and
inhibits IL-2 stimulated proliferation by blocking the IL-2 re-
Figure. Asthma pathogenesis adapted from Casale et al.
25
Dimov et al. Volume 2, Number 4, October 2010
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 230 http://e-aair.org
ceptor alpha chain. It does not deplete circulating CD25+ cells
however. In a study by Busse et al. in 2008,
3
moderate to severe
asthma patients were placed on intravenous daclizumab. Tey
showed improved pulmonary functions, reduced asthma symp-
toms and rescue medication use, increased time to severe ex-
acerbations, and reduced peripheral blood eosinophil and se-
rum eosinophil cationic protein levels. Tese investigators found
greater activity in a refractory asthma subgroup. In that group,
daclizumab resulted in approximately 10% improvement in
FEV1 values, whereas patients on placebo had approximately
10% decrease in FEV1. Tere was also a two-thirds reduction in
the number of asthma exacerbations in patients treated with
daclizumab versus placebo. Tus far, a subcutaneous formula-
tion has not been tried for asthma so it unclear whether or not
this will be a potentially viable treatment for patients with asth-
ma.
Another approach to target T lymphocytes and other key cells
important in the pathogenesis of allergic respiratory diseases is
to use ligands of toll-like receptors (TLR). Tirteen diferent toll-
like receptors have been described in humans. Mycobacteria
activate toll-like receptors 1 and 2, and the use of attenuated
strains has been tried in humans, with minimal to no effect.
Tere is much more information, however, on the use of TLR-4
and TLR-9 agonists.
Te ligand for TLR-4 receptors is endotoxin/lipid A. A specifc
form of this, monophosphoryl lipid A (MPL) has been used as
monotherapy as well as in combination with allergen immuno-
therapy for the treatment of allergic diseases. Ultra short course
vaccines containing MPL have been used since the 1970s for
seasonal allergic rhinitis from grass, tree or ragweed. Te cur-
rent preparation includes a glutaraldehyde-modifed antigen
absorbed onto L-tyrosine depot to enhance tolerability plus
MPL to improve efcacy via activation of toll-4 receptors. Sev-
eral trials have shown that four pre-seasonal injections of this
preparation can reduce symptoms and medication use, elevate
antigen-specifc IgG and blunt seasonal elevations of IgE. Re-
cent United States trials have shown positive results for both
grass and ragweed allergies. In a study presented at the Europe-
an Academy of Allergy and Clinical Immunology meeting in
2008, Zielen et al.,
4
showed that an ultra short course specifc
immunotherapy with Polinex Quattro
TM
in pediatric and ado-
lescent patients resulted in improvement in patients treated
three consecutive years pre-pollen season. In addition, the
amount of improvement in patients was greater in years 2 and
3. Tese data suggest that this approach of four pre-seasonal in-
jections might be appropriate to use in controlling patients who
have signifcant seasonal allergic rhinitis.
Immunostimulatory DNA molecules, CpG, have been used as
well to treat allergic respiratory diseases. TLR-9 agonists have
been used as monotherapy and conjugated to antigen in hu-
man clinical trials. Initial human experiments showed that im-
munostimulatory CpG molecules linked to the predominant
short ragweed allergen, Amb a1, stimulates an antigen-specifc
T2 to T1 shift and improves the safety margin of allergen im-
munotherapy. In a study by Creticos et al.,
5
twenty-fve subjects
with seasonal allergic rhinitis due to ragweed were given six pre-
seasonal injections of Tolamba
TM
, the combination of Amb a1
plus CpG conjugated to each other, in increasing doses from
0.06 to 12 mcg. Te investigators found improvements in symp-
toms in the year the patients were treated as well as the subse-
quent year with no further treatment. There was an approxi-
mate 50% reduction in symptoms in both years with decreased
rescue medication and improvement in quality of life. Howev-
er, large scale clinical trials have been disappointing. Although
there were technical difculties with the larger studies that may
account for the disappointing results, the utility of this approach
has been questioned and further clinical trials are not currently
planned.
However, another approach using a TLR-9 agonist has been
shown to be efective. CYT003-QbG10, is a novel immunother-
apy agent that consists of a virus-like particle, Qb and a short
stretch of DNA from mycrobacteria that activates toll-like re-
ceptor 9 present in dendritic and other cells. In a recent publi-
cation by Senti et al.,
6
CYT003-QbG10 plus house dust mite al-
lergen was given for ten weeks to human subjects with asthma
and allergic rhinitis. Tese investigators found improvements
in symptom scores and quality of life for up to 48 weeks. Inhibi-
tion of skin test responses to house dust mite was also sustained
for up to 48 weeks. Tis implies that long after discontinuing
treatment there is sustained clinical improvement. Interesting-
ly, in an eighty patient seasonal allergic rhinitis study, total rhi-
noconjunctivitis symptom scores were shown to be improved
with QbG10 molecule without allergen.
7
The treatment ap-
peared safe and well tolerated, and efcacious in lowering rhi-
noconjunctivitis symptoms. Since this latter study did not use
an allergen, it is concluded that CYT 003 acts through an aller-
gen-independent mechanism and not through an adjuvant ef-
fect. A phase IIIb study with 300 patients sufering from peren-
nial allergies has recently been started.
Another approach targeting T-cells and the early phases of al-
lergic infammation has been to use peroxisome proliferator-
activated receptor (PPAR) agonists. This approach has been
shown to be efective in murine models.
8
PPAR-gamma ago-
nists inhibit gene expression by binding to AP1 and other co-
activators inhibiting the production of important infammatory
cytokines. PPAR-gamma agonists have a number of potential
mechanisms which could be important.
8
Tese include inhibi-
tion of cytokine production from a number of inflammatory
cells in addition to T-lymphocytes and decreased chemotaxis
of infammatory cells. Human clinical trials are under way and
it will be interesting to see whether these agents, already used
for Type II diabetes mellitus (glitazones), might also be efective
for asthma.
Immunomodulators for Asthma AAIR
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 231 http://e-aair.org
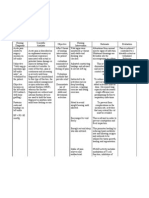
Table. Monoclonal antibodies (mAb) and fusion proteins in trials for treatment
of asthma and allergic diseases
Name Source Target
Development
Status
Omalizumab Humanized IgE FDA-approved
Lumiliximab Chimeric FcERII (CD23) Phase II
Soluble IL-4
receptor
Fusion protein IL-4 Phase II
AMG-317 Human IL-4Ra receptor Phase II
Aerovant Mutein IL-4Ra receptor Phase II
Mepolizumab Humanized IL-5 Phase II
Reslizumab Humanized IL-5 Phase II
Daclizumab Humanized
IL-2 receptor
alpha-chain (CD25)
Phase II
CAT-354 Human IL-13 Phase II
Lebrikizumab Humanized IL-13 Phase II
IMA-638 Humanized IL-13 Phase II
QAX 576 mAb IL-13 Phase II
TH-2 CYTOKINE INHIBITORS
Because of the importance of T-2 cytokines, IL-4, IL-5, IL-9,
and IL-13, strategies aimed at inhibiting their production or ef-
fects have been tried in human clinical trials (Table). Initial at-
tempts to use strategies aimed at IL-4 showed some promise,
but subsequent large scale studies were unrewarding. Tis has
included soluble IL-4 receptors and monoclonal antibodies
against IL-4.
Tere are several strategies aimed at IL-4Ra, the common re-
ceptor chain important for both IL-4 and IL-13 signaling. AMG
317, is a humanized monoclonal antibody to IL-4Ra that has
undergone initial human clinical trials.
9
Early trials have been
disappointing with some minor biologic activity but no clinical
efects. Nonetheless, further development of this molecule is
warranted since diferent routes and dosages may be important
in showing clinical efectiveness. An inhaled anti-sense mole-
cule to IL-4Ra, AIR645 has also undergone very early clinical tri-
als, but no positive clinical efects have been reported thus far.
A 14 kD IL-4 mutein that blocks IL-4Ra has been shown to be
efective for both atopic dermatitis when given subcutaneously
and asthma when given by inhalation. Te inhaled form of this
molecule, pitrakinra (AEROVANT
TM
) was reported to block ear-
ly and late phase allergen responses in patients with asthma.
10
Its efcacy in large scale clinical trials with traditional primary
endpoints has yet to be determined.
Murine model studies have shown that IL-13 plays an impor-
tant role in airway hyperresponsiveness, mucus production, se-
cretion of eotaxin, and airway remodeling. Tere are several hu-
manized monoclonal antibodies against IL-13 that are currently
under development in phase I or phase II human clinical trials.
CAT-354 is a human monoclonal anti-IL-13 antibody that is in
a phase IIa parallel-arm study to evaluate the efcacy and safe-
ty of three subcutaneous treatment regimens in adult subjects
with uncontrolled, moderate-to-severe, persistent asthma (Clin-
icalTrials.gov Identifer: NCT00873860).
Lebrikizumab is a humanized monoclonal antibody that binds
to IL-13 and is currently in development for asthma (ClinicalTri-
als.gov Identifer: NCT00930163). A phase II clinical trial evalu-
ating the efects of this antibody in patients with asthma is on-
going However, mono-specifc anti-IL-13 strategies have been
disappointing in recently reported trials despite IL-13s putative
importance in asthma pathogenesis. It is unclear if there is a
problem with the specific monoclonal antibodies that have
been developed or if there is too much redundancy in the im-
mune system such that inhibiting either IL-4 or IL-13 is insuf-
cient. Indeed, strategies aimed at both IL-4 and IL-13 may be a
better option.
A monoclonal antibody aimed at interleukin-9 is in early phase
clinical trials. However, no published data are available to ascer-
tain its potential efcacy and safety.
Suplatast tosilate is an oral agent that has been shown to in-
hibit the synthesis of both IL-4 and IL-5.
11
Suplatast has been
shown in early clinical trials to decrease serum IgE and periph-
eral blood eosinophil counts.
12
Suplatast has also been shown
to improve traditional asthma outcomes and decrease airway
inflammation.
13
However, this molecule has to be used in a
three times per day regimen making its utility somewhat prob-
lematic since compliance would clearly be an issue.
ANTI-EOSINOPHIL STRATEGIES
Considering the prominence of eosinophils in many patients
with asthma and their putative role in the pathogenesis of aller-
gic respiratory disorders, several therapeutic approaches have
been developed to block eosinophil-mediated effects. Initial
strategies have involved using humanized monoclonal anti-
bodies against interleukin-5, an important cytokine for both
chemotaxis and differentiation of eosinophils. Several older
studies have confirmed reductions in blood and sputum eo-
sinophils without signifcant changes in airway hyperrespon-
siveness, lung functions or symptoms in patients treated with
anti-Il-5 monoclonal antibodies. Two recent studies investigat-
ed diferent aspects of mepolizumab therapy in patients with
refractory asthma and sputum eosinophilia.
14,15
Unlike previous
studies, in order to enroll in these two studies, subjects had to
have a high sputum eosinophil count, greater than 3%. Te in-
vestigators once again found a reduction in peripheral blood
eosinophil counts. However, clinical efects were modest with
either no or little efects on FEV1, airway hyperresponsiveness
or symptoms. There were however significant reductions in
asthma exacerbations. Nonetheless, it is unclear how useful
this strategy will be given that in these two studies, less than 5%
of uncontrolled asthma patients met the entry criteria of having
Dimov et al. Volume 2, Number 4, October 2010
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 232 http://e-aair.org
greater than 3% sputum eosinophils. Tus, the treatment ap-
pears efective for a small segment of uncontrolled asthma pa-
tients, and even in those subjects, therapeutic efectiveness was
somewhat modest.
TPIASM8 is an oligonucleotide using RNA silencing. It con-
tains two modified phosphorothioate anti-sense oligonucle-
otides designed to inhibit allergic infammation by down-regu-
lating human CCR3 and the common beta-chain of IL-3, IL-5
and GM CSF. A recent study examined the efects of inhaled
TPIASM8 on sputum cellular influx, CCR3 and beta-chain
mRNA in protein levels and airway physiologic responses after
inhaled allergen challenge.
16
Compared with placebo, TPI-
ASM8 inhibited sputum eosinophil infux by 46% and blunted
the increase in total cells after allergen challenge. TPIASM8 sig-
nifcantly reduced the early asthmatic response, but not the late
asthmatic response. Te allergen-induced levels of beta-chain
mRNA and CCR3 mRNA in sputum-derived cells were inhibit-
ed by TPIASM8, but no signifcant efects on cell surface pro-
tein expression of CCR3 and the beta-chain were found. Larger
scale clinical trials are necessary to discern the efectiveness of
this treatment for asthma.
A humanized monoclonal antibody against GM CSF is also
undergoing very early clinical trials. However, no data have
been published to date.
ANTI-TNF-a STRATEGIES
TNF-a has a number of efects that could be important in asth-
ma. TNF-a can increase airway hyperresponsiveness and in-
crease the expression of key adhesion molecules important for
eosinophil and neutrophil chemotaxis. Moreover, TNF-a can
stimulate both epithelial and endothelial cells to synthesize and
release chemokines and other cytokines. Several small studies
in patients with severe asthma have shown that patients treated
with TNF-a blockers have some improvements in lung func-
tion, quality of life, exacerbation rates and airway hyperrespon-
siveness. However, larger multi-site studies have been disap-
pointing. Not only has efcacy been difcult to show, but in-
creased adverse events were recorded indicating a relatively
poor risk to beneft ratio.
17
Tus, anti-TNF strategies have been
placed on hold for further development in the management of
asthma and allergic disorders.
STRATEGIES AIMED AT IGE AND MAST CELLS
An attractive target for efectively managing allergic infam-
mation is the mast cell. One target in the mast cell that is critical
for degranulation is Syk kinase. Syk kinase is an intracellular pro-
tein tyrosine kinase that is important in mast cell and basophil
activation and mediator release. Upon cross-linking of IgE
bound high afnity IgE receptors, Syk kinase is activated and
leads to degranulation, cytokine synthesis and leukotriene syn-
thesis. Two antagonists, R112 and R343, have been tried in hu-
man studies. R112 demonstrated statistically signifcant efca-
cy in ameliorating symptoms of allergic rhinitis including nasal
congestion, nasal discharge, sneezing, nasal and throat pruri-
tus, post nasal drip, cough, headache and facial pain in a two-
day seasonal allergic rhinitis park study setting.
18
Te onset of
action was observed within 30 to 90 minutes and the overall
clinical improvement over placebo was approximately 25%. An
inhaled formulation, R343, is currently being developed for the
management of allergic asthma.
19
Omalizumab, the humanized monoclonal anti-IgE antibody,
has been shown to have a number of anti-infammatory and
clinical benefts in patients.
19,20
In patients on inhaled corticos-
teroids alone or in combination with other agents, the addition
of omalizumab has been shown to reduce asthma exacerba-
tions, improve symptom scores, reduce the need for inhaled
and oral corticosteroids and decrease the necessity of rescue
medication.
21-24
Efcacy has also been demonstrated in patients
who have concomitant allergic rhinitis and asthma.
20
Omalizumab has been shown in several small studies or case
reports to have some benefts in the following disorders: sea-
sonal and perennial allergic rhinitis with and without asthma;
atopic dermatitis; food allergies; insect allergy; chronic urticar-
ia with auto-antibodies to either the high afnity IgE receptor
or IgE itself; allergic broncho-pulmonary aspergillosis; latex al-
lergy; chronic hyperplastic sinusitis; recurrent nasal polyposis;
drug allergy; and idiopathic anaphylaxis.
21
Omalizumab decreases free IgE levels rapidly and the expres-
sion of the high afnity IgE receptor expression on key efector
cells, including mast cells, basophils, dendritic cells and mono-
cytes. In addition, lung infammation has been shown to de-
crease after only sixteen weeks of omalizumab treatment. How-
ever, omalizumab has been reported to cause anaphylaxis
through unknown mechanisms in frst as well as subsequent
doses.
22
Observation of patients for 2 hours after they received each of
the frst three injections and for 30 minutes after they received
subsequent injections would capture 75% of the anaphylactic
reactions according to the current recommendation of the
American Academy of Allergy, Asthma & Immunology/Ameri-
can College of Allergy, Asthma & Immunology Joint Task
Force.
23
MAST CELL MEDIATOR ANTAGONISTS
There have been many attempts to develop antagonists to
mast cell mediators that play a signifcant role in airway hyper-
reactivity in asthma. Antagonists to CRTH2 (a G protein cou-
pled receptor) are currently under investigation. CRTH2 is pres-
ent on T2-cells, eosinophils and basophils mediating activa-
tion and chemotaxis to PGD2. A recent 28-day phase II study in
mild to moderate asthma patients with FEV1 values between
Immunomodulators for Asthma AAIR
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 233 http://e-aair.org
60 and 80% showed promising trends with ACT-129968, an oral
antagonist.
24
Bronchoprovocation to both adenosine mono-
phosphate and methacholine decreased by one to one and a
half doubling doses, FEV1 increased by 10 to 14%, and there
was a decrease in sputum eosinophils and IgE. Moreover, pa-
tients had an improved quality of life. Further studies examin-
ing the efcacy of this approach will be necessary to determine
true therapeutic potential.
SUMMARY
There are a number of immunomodulators that have been
developed for the treatment of allergic disorders. Some have
looked very promising in pre-clinical trials, but have not shown
signifcant benefts in human clinical trials indicating the dis-
parity between murine models and human asthma.
It is difcult to predict which of these pharmaceutical agents
other than omalizumab will achieve success. Ultimately, the
use of these putative therapeutics in human clinical trials should
help defne the pathogenesis of asthma and determine the im-
portance of specifc molecules in large patient populations. It is
possible that some of these agents could be efective for only a
small sub-population of patients which potentially would make
them unlikely to be commercially viable.
Te search for better therapeutics options is focused on de-
creasing the symptoms and improving the quality of life while
preventing or altering disease course. Tese molecules should
also have a favorable risk beneft ratio which would lead to wid-
er use. In addition, cost efective strategies are clearly indicated
as monoclonal antibodies are very expensive to manufacture
and to administer.
Te use of immunomodulators for the treatment of allergic
respiratory disorders represents an exciting new era for the ther-
apy of allergic disorders. Human clinical trials are essential for
the development and to determine their ultimate place in our
therapeutic armamentarium.
REFERENCES
1. Malmstrom K, Rodriguez-Gomez G, Guerra J, Villaran C, Pineiro A,
Wei LX, Seidenberg BC, Reiss TF. Oral montelukast, inhaled be-
clomethasone, and placebo for chronic asthma. A randomized,
controlled trial. Montelukast/Beclomethasone Study Group. Ann
Intern Med 1999;130:487-95.
2. Tantisira KG, Lake S, Silverman ES, Palmer LJ, Lazarus R, Silverman
EK, Liggett SB, Gelfand EW, Rosenwasser LJ, Richter B, Israel E,
Wechsler M, Gabriel S, Altshuler D, Lander E, Drazen J, Weiss ST.
Corticosteroid pharmacogenetics: association of sequence vari-
ants in CRHR1 with improved lung function in asthmatics treated
with inhaled corticosteroids. Hum Mol Genet 2004;13:1353-9.
3. Busse WW, Israel E, Nelson HS, Baker JW, Charous BL, Young DY,
Vexler V, Shames RS. Daclizumab improves asthma control in pa-
tients with moderate to severe persistent asthma: a randomized,
controlled trial. Am J Respir Crit Care Med 2008;178:1002-8.
4. Salapatek AM, Patel P, Schulze J, Fischer von Weikersthal-Drachen-
berg KJ, Zielen S. Comparison of outcomes following ultra short
course specifc immunotherapy (uSCIT) in juvenile and adult pa-
tients with asthma. Proceedings of the XXVIIth Congress of the Eu-
ropean Academy of Allergology and Clinical Immunology (EAA-
CI); 2008 Jun 7-11; Barcelona, Spain.
5. Creticos PS, Schroeder JT, Hamilton RG, Balcer-Whaley SL, Khattig-
navong AP, Lindblad R, Li H, Cofman R, Seyfert V, Eiden JJ, Broide
D. Immunotherapy with a ragweed-toll-like receptor 9 agonist vac-
cine for allergic rhinitis. N Engl J Med 2006;355:1445-55.
6. Senti G, Johansen P, Haug S, Bull C, Gottschaller C, Mu_ ller P, Pfster
T, Maurer P, Bachmann MF, Graf N, Ku_ ndig TM. Use of A-type CpG
oligodeoxynucleotides as an adjuvant in allergen-specifc immu-
notherapy in humans: a phase I/IIa clinical trial. Clin Exp Allergy
2009;39:562-70.
7. Blaziene A. CYT003-QbG10, a novel allergen-independent immu-
notherapy, shown to be safe and efcacious in placebo-controlled
phase II study. Proceedings of the American College of Allergy,
Asthma & Immunology Annual Scientifc Meeting; 2008 Nov 6-11;
Seattle, USA.
8. Belvisi MG, Hele DJ. Peroxisome proliferator-activated receptors as
novel targets in lung disease. Chest 2008;134:152-7.
9. Corren J, Busse W, Meltzer E, Mansfeld L, Bensch G, Chon Y, Dunn
M, Weng H, Lin S. Efcacy and safety of AMG 317, an IL-4Ra antag-
onist, in atopic asthmatic subjects: a randomized, double-blind,
placebo-controlled study. J Allergy Clin Immunol 2009;123:732.
10. Wenzel S, Wilbraham D, Fuller R, Getz EB, Longphre M. Efect of an
interleukin-4 variant on late phase asthmatic response to allergen
challenge in asthmatic patients: results of two phase 2a studies.
Lancet 2007;370:1422-31.
11. Ishiura Y, Fujimura M, Yamamoto H, Nobata K, Ishiguro T, Ogawa
H, Myou S. Effect of an orally active Th2 cytokine inhibitor, su-
platast on atopic cough tosilate. Arzneimittelforschung 2008;58:
297-302.
12. Agrawal DK, Cheng G, Kim MJ, Kiniwa M. Interaction of suplatast
tosilate (IPD) with chloride channels in human blood eosinophils:
a potential mechanism underlying its anti-allergic and anti-asth-
matic efects. Clin Exp Allergy 2008;38:305-12.
13. Tanaka A, Minoguchi K, Samson KT, Oda N, Yokoe T, Tazaki T, Ya-
mamoto Y, Yamamoto M, Ohta S, Adachi M. Inhibitory efects of
suplatast tosilate on the diferentiation and function of monocyte-
derived dendritic cells from patients with asthma. Clin Exp Allergy
2007;37:1083-9.
14. Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A,
Marshall RP, Bradding P, Green RH, Wardlaw AJ, Pavord ID. Me-
polizumab and exacerbations of refractory eosinophilic asthma. N
Engl J Med 2009;360:973-84.
15. Nair P, Pizzichini MM, Kjarsgaard M, Inman MD, Efthimiadis A,
Pizzichini E, Hargreave FE, OByrne PM. Mepolizumab for predni-
sone-dependent asthma with sputum eosinophilia. N Engl J Med
2009;360:985-93.
16. Gauvreau GM, Boulet LP, Cockcroft DW, Baatjes A, Cote J, De-
schesnes F, Davis B, Strinich T, Howie K, Duong M, Watson RM,
Renzi PM, OByrne PM. Antisense therapy against CCR3 and the
common beta chain attenuates allergen-induced eosinophilic re-
sponses. Am J Respir Crit Care Med 2008;177:952-8.
17. Wenzel SE, Barnes PJ, Bleecker ER, Bousquet J, Busse W, Dahlen SE,
Holgate ST, Meyers DA, Rabe KF, Antczak A, Baker J, Horvath I,
Dimov et al. Volume 2, Number 4, October 2010
Allergy Asthma Immunol Res. 2010 October;2(4):228-234. doi: 10.4168/aair.2010.2.4.228 234 http://e-aair.org
Mark Z, Bernstein D, Kerwin E, Schlenker-Herceg R, Lo KH, Watt R,
Barnathan ES, Chanez P. A randomized, double-blind, placebo-
controlled study of tumor necrosis factor-alpha blockade in severe
persistent asthma. Am J Respir Crit Care Med 2009;179:549-58.
18. Meltzer EO, Berkowitz RB, Grossbard EB. An intranasal Syk-kinase
inhibitor (R112) improves the symptoms of seasonal allergic rhini-
tis in a park environment. J Allergy Clin Immunol 2005;115:791-6.
19. Rigel Pharmaceuticals, Inc. Rigel announces initiation of phase 1
clinical trial of R343 for allergic asthma by its partner Pfzer [In-
ternt]. [cited 2009 Jun 12]. Available from: http://ir.rigel.com/phoe-
nix.zhtml?c=120936&p=irol-newsArticle&ID=1084738.
20. Casale TB, Condemi J, LaForce C, Nayak A, Rowe M, Watrous M,
McAlary M, Fowler-Taylor A, Racine A, Gupta N, Fick R, Della Ciop-
pa G. Efect of omalizumab on symptoms of seasonal allergic rhini-
tis: a randomized controlled trial. JAMA 2001;286:2956-67.
21. Casale TB, Stokes J. Anti-IgE therapy: clinical utility beyond asthma.
J Allergy Clin Immunol 2009;123:770-1. e1.
22. Limb SL, Starke PR, Lee CE, Chowdhury BA. Delayed onset and
protracted progression of anaphylaxis after omalizumab adminis-
tration in patients with asthma. J Allergy Clin Immunol 2007;120:
1378-81.
23. Cox L, Platts-Mills TA, Finegold I, Schwartz LB, Simons FE, Wallace
DV. American Academy of Allergy, Asthma & Immunology/Ameri-
can College of Allergy, Asthma and Immunology Joint Task Force
Report on omalizumab-associated anaphylaxis. J Allergy Clin Im-
munol 2007;120:1373-7.
24. Actelion Pharmaceuticals Ltd. CRTH2 antagonist [Internet]. [cited
2010 Feb 24]. Available from: http://www.actelion.com/en/scien-
tists/development-pipeline/phase-2/crth2-antagonist.page.
25. Casale TB, Stokes JR. Immunomodulators for allergic respiratory
disorders. J Allergy Clin Immunol 2008;121:288-96; quiz 97-8.
Vous aimerez peut-être aussi
- Fast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlD'EverandFast Facts: Asthma: Improve patient self-management and drug use, achieve asthma controlPas encore d'évaluation
- 1-s2.0-S0952791517301036-Willem_van_de_Veen_Immune_Tolerance_2017Document22 pages1-s2.0-S0952791517301036-Willem_van_de_Veen_Immune_Tolerance_2017vivekverma3509Pas encore d'évaluation
- Essay: Rethinking The Pathogenesis of AsthmaDocument6 pagesEssay: Rethinking The Pathogenesis of AsthmaConstanza Rada Von FurstenbergPas encore d'évaluation
- Omalizumab For Asthma Nejm 2006Document7 pagesOmalizumab For Asthma Nejm 2006Sachin VermaPas encore d'évaluation
- Advances in treating allergic diseases and asthma through immunological approachesDocument17 pagesAdvances in treating allergic diseases and asthma through immunological approachesSam SonPas encore d'évaluation
- Tailored Therapy For Severe Asthma: Review Open AccessDocument8 pagesTailored Therapy For Severe Asthma: Review Open AccessSardar IjlalPas encore d'évaluation
- Concise Clinical Review: Role of Biologics in AsthmaDocument13 pagesConcise Clinical Review: Role of Biologics in AsthmaHossam HamzaPas encore d'évaluation
- Allergen ImmunotherapyDocument7 pagesAllergen ImmunotherapyHector Javier BurgosPas encore d'évaluation
- Bernstein 2016Document18 pagesBernstein 2016Hafid RakasdianPas encore d'évaluation
- Mohapatra 2010Document13 pagesMohapatra 2010zavoianu.diana21Pas encore d'évaluation
- Up To Date. Asthma PathogenesisDocument22 pagesUp To Date. Asthma PathogenesisGuardito PequeñoPas encore d'évaluation
- Cea 13169 PDFDocument15 pagesCea 13169 PDFrisanataliasiburianPas encore d'évaluation
- Omalizumab: Clinical Use For The Management of AsthmaDocument14 pagesOmalizumab: Clinical Use For The Management of Asthmaall_dedicatePas encore d'évaluation
- 1 s2.0 S2095881118301379 MainDocument7 pages1 s2.0 S2095881118301379 MainAnita DewiPas encore d'évaluation
- 2022 Lin Sun - Difference of Serum Cytokine Profile in Allergic A RetrieveDocument12 pages2022 Lin Sun - Difference of Serum Cytokine Profile in Allergic A RetrieveSteve aokiPas encore d'évaluation
- Update On Severe Asthma: What We Know and What We NeedDocument8 pagesUpdate On Severe Asthma: What We Know and What We Needtaksim2011Pas encore d'évaluation
- 2b PDFDocument4 pages2b PDFAndrea Il MiodoPas encore d'évaluation
- Improved Pulmonary Function Test (PFT) After 1 One Year of Sublingual Immunotherapy (SLIT) in Unison With Pharmacotherapy in Mild Allergic AsthmaticsDocument7 pagesImproved Pulmonary Function Test (PFT) After 1 One Year of Sublingual Immunotherapy (SLIT) in Unison With Pharmacotherapy in Mild Allergic AsthmaticsRoohi WaniPas encore d'évaluation
- J. Antimicrob. Chemother. 2012 Kovaleva 530 40Document11 pagesJ. Antimicrob. Chemother. 2012 Kovaleva 530 40Bases De Datos MédicasPas encore d'évaluation
- Neutrophils and Asthma: J MonteseirínDocument15 pagesNeutrophils and Asthma: J MonteseirínRupa2811Pas encore d'évaluation
- Citocinas e AsmaDocument14 pagesCitocinas e AsmaFabiula AbreuPas encore d'évaluation
- English - Basic Immunological Mechanism in Uveitis To Explain The Efficacy of Steroid and Immunosuppressive TreatmentDocument8 pagesEnglish - Basic Immunological Mechanism in Uveitis To Explain The Efficacy of Steroid and Immunosuppressive TreatmentardiansyahPas encore d'évaluation
- The Potential of Biologics For The Treatment of Asthma: Girolamo Pelaia, Alessandro Vatrella and Rosario MaselliDocument15 pagesThe Potential of Biologics For The Treatment of Asthma: Girolamo Pelaia, Alessandro Vatrella and Rosario MaselliSanjeev SaxenaPas encore d'évaluation
- New Insights Into The Pathophysiology of Allergic Rhinitis: SymposiumDocument6 pagesNew Insights Into The Pathophysiology of Allergic Rhinitis: SymposiumHarry KurniaPas encore d'évaluation
- Nature of Regulatory T Cells in The Context of Allergic DiseaseDocument6 pagesNature of Regulatory T Cells in The Context of Allergic DiseaseLuckybeauty storePas encore d'évaluation
- 2a PDFDocument11 pages2a PDFAndrea Il MiodoPas encore d'évaluation
- Immuno Log IDocument20 pagesImmuno Log Idini rustiawatiPas encore d'évaluation
- Asma NewsDocument31 pagesAsma NewsEmmanuel HernandezPas encore d'évaluation
- SEO GUIDEDocument15 pagesSEO GUIDEhebert ramos100% (1)
- New Treatments For Severe Treatment-Resistant Asthma - Lancet Resp Med 2013Document14 pagesNew Treatments For Severe Treatment-Resistant Asthma - Lancet Resp Med 2013Azan Al RasyidPas encore d'évaluation
- Pi Is 0091674917316652Document14 pagesPi Is 0091674917316652tata wattimuryPas encore d'évaluation
- Anti IL 4 13 Based Therapy in AsthmaDocument5 pagesAnti IL 4 13 Based Therapy in AsthmaMoch Ridwan Pujiar PamungkasPas encore d'évaluation
- Seminario 1Document13 pagesSeminario 1cristhian cuevaPas encore d'évaluation
- Immunologic and Non-Immunologic Mechanisms Leading To Airway Remodeling in AsthmaDocument19 pagesImmunologic and Non-Immunologic Mechanisms Leading To Airway Remodeling in AsthmaHow ToPas encore d'évaluation
- Allergy - 2022 - Gauvreau - Sounding The Alarmins The Role of Alarmin Cytokines in AsthmaDocument16 pagesAllergy - 2022 - Gauvreau - Sounding The Alarmins The Role of Alarmin Cytokines in AsthmaNóra FerenczyPas encore d'évaluation
- Mechanisms of Sublingual Immunotherapy: Guy Scadding,, Stephen R. DurhamDocument19 pagesMechanisms of Sublingual Immunotherapy: Guy Scadding,, Stephen R. DurhamBrîndușa PetruțescuPas encore d'évaluation
- Volk Imunitate in SepsisDocument3 pagesVolk Imunitate in SepsisIna PoianaPas encore d'évaluation
- Immunotherapy - What Lies BeyondDocument8 pagesImmunotherapy - What Lies BeyondSagar Das ChoudhuryPas encore d'évaluation
- Immunology of Asthma and Chronic Obstructive Pulmonary DiseaseDocument10 pagesImmunology of Asthma and Chronic Obstructive Pulmonary DiseaseClaudio Luis VenturiniPas encore d'évaluation
- Dexamethasone inhibits IL-9 production by human T cellsDocument9 pagesDexamethasone inhibits IL-9 production by human T cellsciara babyPas encore d'évaluation
- Asthma MedscapeDocument21 pagesAsthma MedscapeDnyanesh LimayePas encore d'évaluation
- Asthma Endotyping and Biomarkers in Childhood Asthma 2018Document12 pagesAsthma Endotyping and Biomarkers in Childhood Asthma 2018wawa chenPas encore d'évaluation
- 12erny (Full Permission)Document15 pages12erny (Full Permission)Peter SalimPas encore d'évaluation
- CSS TPO Dan TGDocument7 pagesCSS TPO Dan TGSeruni Allisa AslimPas encore d'évaluation
- 1 Melatonin Prevents Allergic Airway Inflammation in Epicutaneously Sensitized MiceDocument12 pages1 Melatonin Prevents Allergic Airway Inflammation in Epicutaneously Sensitized Micebemfisio.cristianeribeiroPas encore d'évaluation
- Novel Anti-Inflammatory Treatments For Asthma: ReviewDocument13 pagesNovel Anti-Inflammatory Treatments For Asthma: Reviewnopera kurnia watiPas encore d'évaluation
- New and Emerging Therapies For AsthmaDocument4 pagesNew and Emerging Therapies For AsthmaAtef AlbooqPas encore d'évaluation
- Pathophysiology of AsthmaDocument71 pagesPathophysiology of AsthmaChin ChanPas encore d'évaluation
- Fimmu 14 1149203Document13 pagesFimmu 14 1149203Claudia Alejandra Gutierrez InzunzaPas encore d'évaluation
- New developments in allergy immunotherapyDocument10 pagesNew developments in allergy immunotherapyWinda HidayatiPas encore d'évaluation
- Asthma Pathophysiology, Diagnosis and TreatmentDocument18 pagesAsthma Pathophysiology, Diagnosis and TreatmentsanasharPas encore d'évaluation
- Cardona Et Al 2017 AllergyDocument8 pagesCardona Et Al 2017 AllergyAnasthasia hutagalungPas encore d'évaluation
- Autoantibodies Against Complement C1q Correlate With The Thyroid Function in Patients With Autoimmune Thyroid DiseaseDocument6 pagesAutoantibodies Against Complement C1q Correlate With The Thyroid Function in Patients With Autoimmune Thyroid DiseaseSaad MotawéaPas encore d'évaluation
- Targeting Mast Cells in Allergic Disease: Current Therapies and Drug RepurposingDocument30 pagesTargeting Mast Cells in Allergic Disease: Current Therapies and Drug RepurposingAlyanna Louise CastroPas encore d'évaluation
- Annurev Immunol 26 021607 090312Document30 pagesAnnurev Immunol 26 021607 090312Jamil KitokoPas encore d'évaluation
- Jurnal Antihistamin 1Document16 pagesJurnal Antihistamin 1Nur SulistiyaningsihPas encore d'évaluation
- Review: Peter J Barnes, Ian M AdcockDocument13 pagesReview: Peter J Barnes, Ian M AdcockYylfordt GranzPas encore d'évaluation
- Autoimmune Rheumatic Diseases An IntroductionDocument2 pagesAutoimmune Rheumatic Diseases An IntroductionsobanPas encore d'évaluation
- Soluble Immunological Markers of Disease Activity in TuberculosisDocument2 pagesSoluble Immunological Markers of Disease Activity in TuberculosisMartin Lorenzo Miguel BaquilodPas encore d'évaluation
- Huang 2017Document10 pagesHuang 2017ritik jainPas encore d'évaluation
- Comorbidities of AsthmaDocument6 pagesComorbidities of AsthmadarmariantoPas encore d'évaluation
- Revisión DressDocument10 pagesRevisión Dressvintage20Pas encore d'évaluation
- Simulation of Pulmonary Breathing PDFDocument4 pagesSimulation of Pulmonary Breathing PDFdarmariantoPas encore d'évaluation
- Jurnal Kekerapan Esofagitis-Dr - AgusDocument15 pagesJurnal Kekerapan Esofagitis-Dr - AgusJamaluddin Ahmad100% (1)
- An Unexpected Consequence of ElectronicDocument4 pagesAn Unexpected Consequence of ElectronicdarmariantoPas encore d'évaluation
- CDC Tuberculosis - What The Physician Should KnowDocument320 pagesCDC Tuberculosis - What The Physician Should KnowbillyPas encore d'évaluation
- Cytokine Polymorphisms, Their Influence and LevelsDocument14 pagesCytokine Polymorphisms, Their Influence and LevelsdarmariantoPas encore d'évaluation
- Irritant Induced Asthma and Reactive Airways Dysfunction Syndrome Rads 2155 6121.1000174Document7 pagesIrritant Induced Asthma and Reactive Airways Dysfunction Syndrome Rads 2155 6121.1000174darmariantoPas encore d'évaluation
- Aetiological Agents in Occupational AsthmaDocument26 pagesAetiological Agents in Occupational AsthmadarmariantoPas encore d'évaluation
- A Study of Sputum Conversion in New Smear Positive Pulmonary Tuberculosis Cases at The Monthly Intervals of 1st, 2nd & 3rd Month Under Directly Observed Treatment, Short Course (Dots) RegimenDocument11 pagesA Study of Sputum Conversion in New Smear Positive Pulmonary Tuberculosis Cases at The Monthly Intervals of 1st, 2nd & 3rd Month Under Directly Observed Treatment, Short Course (Dots) RegimendarmariantoPas encore d'évaluation
- TB ImmunotherapyDocument25 pagesTB ImmunotherapydarmariantoPas encore d'évaluation
- Cepheid OnDemand Report Vol 4 Issue 1 Spring 2011Document12 pagesCepheid OnDemand Report Vol 4 Issue 1 Spring 2011darmariantoPas encore d'évaluation
- Glucocorticoid Effects On The Immune SystemDocument92 pagesGlucocorticoid Effects On The Immune SystemdarmariantoPas encore d'évaluation
- Diaphragmatic Dysfunction and Respiratory Illness (Review) - PulmCCMDocument4 pagesDiaphragmatic Dysfunction and Respiratory Illness (Review) - PulmCCMdarmariantoPas encore d'évaluation
- LungIndia TB and NutrtionDocument8 pagesLungIndia TB and NutrtiondarmariantoPas encore d'évaluation
- Cancer Care Ontario's Symptom Management Guide-To-Practice Loss of AppetiteDocument31 pagesCancer Care Ontario's Symptom Management Guide-To-Practice Loss of AppetitedarmariantoPas encore d'évaluation
- Molecular Origin Lung CancerDocument14 pagesMolecular Origin Lung CancerdarmariantoPas encore d'évaluation
- Anatomy of The Thorax (CT)Document7 pagesAnatomy of The Thorax (CT)darmariantoPas encore d'évaluation
- Prognostic Values of Serum IP-10 and IL-17 inDocument10 pagesPrognostic Values of Serum IP-10 and IL-17 indarmariantoPas encore d'évaluation
- Updating The International Standards For Tuberculosis CareDocument9 pagesUpdating The International Standards For Tuberculosis CaredarmariantoPas encore d'évaluation
- Inventory of Culture and DST Methods - July 31 2011 - FinalDocument15 pagesInventory of Culture and DST Methods - July 31 2011 - FinaldarmariantoPas encore d'évaluation
- Physiotherapy in Intensive Care An Updated Systematic ReviewDocument23 pagesPhysiotherapy in Intensive Care An Updated Systematic ReviewdarmariantoPas encore d'évaluation
- Body weight changes in tuberculosis patients during chemotherapyDocument8 pagesBody weight changes in tuberculosis patients during chemotherapyNiar MarhaliPas encore d'évaluation
- Relationship Between Body Mass Index and Asthma Severity in AdultsDocument6 pagesRelationship Between Body Mass Index and Asthma Severity in AdultsdarmariantoPas encore d'évaluation
- ISTC 3rdedDocument92 pagesISTC 3rdedmichaelqurtisPas encore d'évaluation
- Cytokine Polymorphisms, Their Influence and LevelsDocument14 pagesCytokine Polymorphisms, Their Influence and LevelsdarmariantoPas encore d'évaluation
- Manual Hyperinflation (MHI)Document7 pagesManual Hyperinflation (MHI)darmariantoPas encore d'évaluation
- Sopori 2002 PDFDocument7 pagesSopori 2002 PDFVasilScherbaPas encore d'évaluation
- Perbandingan Validasi APACHE II Dan SOFA ScoreDocument10 pagesPerbandingan Validasi APACHE II Dan SOFA ScoredarmariantoPas encore d'évaluation
- Article Tuberculosis Among Diabetic PatientDocument14 pagesArticle Tuberculosis Among Diabetic PatientdarmariantoPas encore d'évaluation
- Regional Studies in Marine ScienceDocument11 pagesRegional Studies in Marine ScienceBOUCHNANPas encore d'évaluation
- Complaints Handling: BDA AdviceDocument8 pagesComplaints Handling: BDA Advicedruzair007Pas encore d'évaluation
- Journal Homepage: - : IntroductionDocument3 pagesJournal Homepage: - : IntroductionIJAR JOURNALPas encore d'évaluation
- Breakfast of ChampionsDocument34 pagesBreakfast of ChampionsTamanna TabassumPas encore d'évaluation
- Newborn Care Volume 1 2020-1Document192 pagesNewborn Care Volume 1 2020-1Shyvonne PeirisPas encore d'évaluation
- Immunology Serology Blood BankingDocument5 pagesImmunology Serology Blood BankingEdsss Villar100% (3)
- Birads PosterDocument1 pageBirads PosterGopalarathnam BalachandranPas encore d'évaluation
- 31congenital GlaucomasDocument12 pages31congenital GlaucomasShari' Si WahyuPas encore d'évaluation
- Google CardboardDocument3 pagesGoogle CardboardMartínJiménezPas encore d'évaluation
- The Effect of Warm Ginger Compress on Hypertension Headache Scale in the ElderlyDocument7 pagesThe Effect of Warm Ginger Compress on Hypertension Headache Scale in the Elderlyjembatan gantungPas encore d'évaluation
- Stein Corporation Wants To Find An Equation To Estimate Some of Their Monthly Operating Costs For The Operating Budget For 2018Document2 pagesStein Corporation Wants To Find An Equation To Estimate Some of Their Monthly Operating Costs For The Operating Budget For 2018Elliot RichardPas encore d'évaluation
- Stress Amongst Healthcare Professionals and Migrant Workers During Covid-19 PandemicDocument6 pagesStress Amongst Healthcare Professionals and Migrant Workers During Covid-19 PandemicIJAR JOURNALPas encore d'évaluation
- Biology 3rd ESO Full DossierDocument54 pagesBiology 3rd ESO Full DossierNinaPas encore d'évaluation
- Psychoeducational and Family Therapy in Relapse PreventionDocument4 pagesPsychoeducational and Family Therapy in Relapse PreventionEdson HilárioPas encore d'évaluation
- ASP ProductsDocument33 pagesASP ProductsSerghei Barba100% (1)
- Personality Disorders Cluster CDocument19 pagesPersonality Disorders Cluster CPahw BaluisPas encore d'évaluation
- Q1. Read The Passage Given Below and Answer The Questions That FollowDocument2 pagesQ1. Read The Passage Given Below and Answer The Questions That FollowUdikshaPas encore d'évaluation
- Family Nursing Care PlanDocument1 pageFamily Nursing Care PlanDersly LanePas encore d'évaluation
- The NBCP Referral Code SubDocument4 pagesThe NBCP Referral Code SubArcon Solite BarbanidaPas encore d'évaluation
- Oet Reading Part A Additional - GlucomaDocument8 pagesOet Reading Part A Additional - Glucomaafacean25% (8)
- GoalSettingWorkbookFinal PDFDocument21 pagesGoalSettingWorkbookFinal PDFDato KhutsishviliPas encore d'évaluation
- Technology and Livelihood Education: Quarter 1 - Module 4: CaregivingDocument20 pagesTechnology and Livelihood Education: Quarter 1 - Module 4: CaregivingIrine Irine100% (1)
- Abbott Rabeprazole PM e PDFDocument45 pagesAbbott Rabeprazole PM e PDFdonobacaPas encore d'évaluation
- Prepositions of Time ExplainedDocument18 pagesPrepositions of Time ExplainedyuèPas encore d'évaluation
- UV-VIS Method for Estimating Fat-Soluble Vitamins in MultivitaminsDocument6 pagesUV-VIS Method for Estimating Fat-Soluble Vitamins in MultivitaminsTisenda TimiselaPas encore d'évaluation
- 11 - Comfort, Rest and Sleep Copy 6Document28 pages11 - Comfort, Rest and Sleep Copy 6Abdallah AlasalPas encore d'évaluation
- Eo No. 013 - 2018 Reorganization of BhertDocument2 pagesEo No. 013 - 2018 Reorganization of BhertAnne Kimberly Peñalba BabaanPas encore d'évaluation
- Being A Medical DoctorDocument14 pagesBeing A Medical DoctorMichael Bill GihonPas encore d'évaluation
- NCP - Acute Pain - FractureDocument1 pageNCP - Acute Pain - Fracturemawel73% (22)
- College of Physicians and Surgeons of Alberta QB1803-01472 Certified Record of Proceedings - Illegal sabotage of Alberta Cancer Therapy Programs and abuse (physical violence, harassment, verbal abuse) of frontline healthcare staff by Alberta NDP and their AHS and CPSA Officials, covered-up by CPSADocument908 pagesCollege of Physicians and Surgeons of Alberta QB1803-01472 Certified Record of Proceedings - Illegal sabotage of Alberta Cancer Therapy Programs and abuse (physical violence, harassment, verbal abuse) of frontline healthcare staff by Alberta NDP and their AHS and CPSA Officials, covered-up by CPSAWilliam MakisPas encore d'évaluation