Académique Documents
Professionnel Documents
Culture Documents
AMI After Adrenaline
Transféré par
Gabriela Frederick0 évaluation0% ont trouvé ce document utile (0 vote)
40 vues1 pageThis letter discusses a previous case report about a patient who experienced an acute myocardial infarction after receiving low-dose intravenous epinephrine for anaphylaxis. The authors acknowledge the delayed onset of symptoms is unusual but believe penicillin is still the most likely cause. They also clarify that the patient did not experience a major heart attack, and their cardiologists chose a CT angiogram over invasive testing due to the minor nature of the infraction and risks to the young patient. The authors hope this case report will educate others about potential harms of intravenous epinephrine and that intramuscular is generally safer, while acknowledging IV may still have a role in extreme cases of anaphylaxis and shock.
Description originale:
wow wow wow
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentThis letter discusses a previous case report about a patient who experienced an acute myocardial infarction after receiving low-dose intravenous epinephrine for anaphylaxis. The authors acknowledge the delayed onset of symptoms is unusual but believe penicillin is still the most likely cause. They also clarify that the patient did not experience a major heart attack, and their cardiologists chose a CT angiogram over invasive testing due to the minor nature of the infraction and risks to the young patient. The authors hope this case report will educate others about potential harms of intravenous epinephrine and that intramuscular is generally safer, while acknowledging IV may still have a role in extreme cases of anaphylaxis and shock.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
40 vues1 pageAMI After Adrenaline
Transféré par
Gabriela FrederickThis letter discusses a previous case report about a patient who experienced an acute myocardial infarction after receiving low-dose intravenous epinephrine for anaphylaxis. The authors acknowledge the delayed onset of symptoms is unusual but believe penicillin is still the most likely cause. They also clarify that the patient did not experience a major heart attack, and their cardiologists chose a CT angiogram over invasive testing due to the minor nature of the infraction and risks to the young patient. The authors hope this case report will educate others about potential harms of intravenous epinephrine and that intramuscular is generally safer, while acknowledging IV may still have a role in extreme cases of anaphylaxis and shock.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 1
AMI after low-dose IV
epinephrine for anaphylaxis
To the editor: The letters
1,2
in Septem-
bers issue of CJEM responding to our
Case Report on the use of IV epineph-
rine in anaphylaxis
3
raise interesting
questions. We agree that a 10-hour on-
set delay seems long, but penicillin re-
mains a more likely cause of anaphy-
laxis than ibuprofen, which the patient
had taken in the past, and regardless of
the inciting agent, the case illustrates
important points. We did not suggest
that our patient suffered a large my-
ocardial infarction. A troponin eleva-
tion to 23 times normal does not sug-
gest major damage, but is consistent
with infarction. Based on the minor na-
ture of this infarct and its presumed
pathogenesis, our cardiologists chose to
do a CT angiogram because they be-
lieved the risks of invasive angiography
were greater than the potential benefits
in this young person without concomi-
tant disease. All acute coronary syn-
dromes (ACS) protocols recommend
ASA in the presence of ST elevation;
however, if in this situation (anaphy-
laxis with epinephrine-induced coro-
nary vasospasm) occurs in the future,
we would not necessarily administer
ASA, since ASA and NSAIDs can ex-
acerbate anaphylaxis.
We have no specific comments
about Dr. Shahs letter
2
as it illustrates
the reason we wrote this case report.
Our hope was that it would educate
others about the potential harm associ-
ated with intravenous (IV) epineph-
rine. (This patient has been advised
that she is never again to receive epi-
nephrine.) We have found the same
opinion split in our emergency depart-
ment community and were surprised
to find no definitive answer in the lit-
erature. We agree that, in all but ex-
treme cases, intramuscular epineph-
rine is the correct choice and that the
lateral thigh is the correct place. We
recognize that this case report does not
rule out a role for IV epinephrine in
extreme anaphylaxis and shock, al-
though the IV route is associated with
a shorter action duration. (It is inter-
esting to speculate that the shorter IV
duration may have been less danger-
ous in a case like this.)
Steve Weiss, MD
Kyle Shaver, MD
Christopher Adams, MD
Department of Emergency Medicine
University of New Mexico
Albuquerque, NM
References
1. Maddison G. AMI after epinephrine
[letter]. Can J Emerg Med 2006;8(5):
315.
2. Shah A. AMI after epinephrine [letter].
Can J Emerg Med 2006;8(5):315-6.
3. Shaver KJ, Adams C, Weiss SJ. Acute
myocardial infarction after administra-
tion of low-dose intravenous epineph-
rine for anaphylaxis. Can J Emerg Med
2006;8(4):289-94.
Erratum
In the Pediatrics Original Research ar-
ticle published in the July 2006 issue
of CJEM, the Competing Interests
statement was incomplete. There were
no competing interests declared by the
author.
Reference
1. Taylor BW. Demography of pediatric
emergency care in Halifax, Canada.
Can J Emerg Med 2006;8(4):269-74.
LETTERS COURRIER
November novembre 2006; 8 (6) CJEM JCMU 387
Letters will be considered for publication if they
relate to topics of interest to emergency physi-
cians in urban, rural, community or academic
settings. Letters responding to a previously
published CJEM article should reach CJEM head
office in Vancouver (see masthead for details)
within 6 weeks of the articles publication.
Letters should be limited to 400 words and
5 references. For reasons of space, letters may
be edited for brevity and clarity.
Les lettres seront considres pour publication si elles sont
pertinentes la mdecine durgence en milieu urbain,
rural, communautaire ou universitaire. Les lettres en
rponse des articles du JCMU publis antrieurement
devraient parvenir au sige social du JCMU Vancouver
(voir titre pour plus de dtails) moins de six semaines aprs
la parution de larticle en question. Les lettres ne devraient
pas avoir plus de 400 mots et cinq rfrences. Pour des
raisons despace et par souci de concision et de clart, cer-
taines lettres pourraient tre modifies.
Vous aimerez peut-être aussi
- Fatovich 2007Document2 pagesFatovich 2007sarah nabilaPas encore d'évaluation
- ECG Diagnosis: Acute Myocardial Infarction in A Ventricular-Paced RhythmDocument3 pagesECG Diagnosis: Acute Myocardial Infarction in A Ventricular-Paced RhythmFlora Eka HeinzendorfPas encore d'évaluation
- 0122 StemiDocument29 pages0122 Stemienfermeras uciPas encore d'évaluation
- Vincent 2009Document6 pagesVincent 2009Guillermo Obando LaraPas encore d'évaluation
- IMP Shock Etiol 5y Outcome VA-ECMO Edit 2023Document3 pagesIMP Shock Etiol 5y Outcome VA-ECMO Edit 2023vladbvs16Pas encore d'évaluation
- The RUSH Exam Rapid Ultrasound in SHock in The Evaluation of The Critically LLLDocument28 pagesThe RUSH Exam Rapid Ultrasound in SHock in The Evaluation of The Critically LLLMiguel Angel Montoya UrreloPas encore d'évaluation
- The RUSH Exam - Rapid Ultrasound in SHock in The Evaluation of The Critically LLLDocument28 pagesThe RUSH Exam - Rapid Ultrasound in SHock in The Evaluation of The Critically LLLCARLOSPas encore d'évaluation
- Pi Is 0091674906002946Document8 pagesPi Is 0091674906002946Petrescu MihaiPas encore d'évaluation
- Accepted Manuscript: American Journal of Emergency MedicineDocument26 pagesAccepted Manuscript: American Journal of Emergency MedicineRober MerazPas encore d'évaluation
- A Strong and Steady Pulse: Stories from a CardiologistD'EverandA Strong and Steady Pulse: Stories from a CardiologistPas encore d'évaluation
- Development of Acute Decompensated Heart Failure Therapies: Is The Journey Over?Document2 pagesDevelopment of Acute Decompensated Heart Failure Therapies: Is The Journey Over?Dewi AyuPas encore d'évaluation
- RECONSIDERING VASOPRESSORS For CARDIOGENIC SHOCK Everything Should Be Made As Simple As Possible, But Not SimplerDocument33 pagesRECONSIDERING VASOPRESSORS For CARDIOGENIC SHOCK Everything Should Be Made As Simple As Possible, But Not Simpleralejandro montesPas encore d'évaluation
- When Your Patient Has A Non Shockable Rhythm WhicDocument2 pagesWhen Your Patient Has A Non Shockable Rhythm Whicaida154Pas encore d'évaluation
- Nejmoa 067373Document11 pagesNejmoa 067373Wend Panga CongoPas encore d'évaluation
- Simplified Pediatric ECGDocument11 pagesSimplified Pediatric ECGSuman MondalPas encore d'évaluation
- NEWS Vs SIRS Vs qSOFA TriageDocument29 pagesNEWS Vs SIRS Vs qSOFA TriagejoelPas encore d'évaluation
- 10 1001@jamaneurol 2019 0591Document7 pages10 1001@jamaneurol 2019 0591Suryati HusinPas encore d'évaluation
- 1tDn nNUqdJMD2ylVCoKmvQ7GfkQ8iGdRDocument8 pages1tDn nNUqdJMD2ylVCoKmvQ7GfkQ8iGdRRossy Viviana Bernabé CastilloPas encore d'évaluation
- ECG Changes During Septic Shock PDFDocument10 pagesECG Changes During Septic Shock PDFandikaisnaeniPas encore d'évaluation
- Sacks, Oliver - A Compulsive Collecting Behavior... (Letter) (2001)Document2 pagesSacks, Oliver - A Compulsive Collecting Behavior... (Letter) (2001)uerico roehePas encore d'évaluation
- Cardiac TamponadDocument3 pagesCardiac TamponadBelinda SuhuyanlyPas encore d'évaluation
- Molecular Investigation Into The Human Atrioventricular Node in Heart Failure 2161 0940.1000164Document8 pagesMolecular Investigation Into The Human Atrioventricular Node in Heart Failure 2161 0940.1000164Mei RieģoPas encore d'évaluation
- Epilepsi Paska StrokeDocument5 pagesEpilepsi Paska StrokerifaiPas encore d'évaluation
- Posterior Circulation Stroke: Advances in Understanding and ManagementD'EverandPosterior Circulation Stroke: Advances in Understanding and ManagementJong S. KimPas encore d'évaluation
- Seiffge 2018Document3 pagesSeiffge 2018barti koksPas encore d'évaluation
- ASA Physical Status Classification System PDFDocument6 pagesASA Physical Status Classification System PDFfbihansipPas encore d'évaluation
- Nej MC 1512716Document3 pagesNej MC 1512716anggiPas encore d'évaluation
- Air Vs Oxygen in STEMPDocument8 pagesAir Vs Oxygen in STEMPTony LeePas encore d'évaluation
- Points & Pearls: Updates and Controversies in The Early Management of Sepsis and Septic ShockDocument2 pagesPoints & Pearls: Updates and Controversies in The Early Management of Sepsis and Septic Shockdogui0071Pas encore d'évaluation
- Burns 2008Document3 pagesBurns 2008Elok Chintya JanisePas encore d'évaluation
- Brown 2019Document3 pagesBrown 2019Elmer MoscosoPas encore d'évaluation
- Antibiotic Timing Sepsis MortalityDocument15 pagesAntibiotic Timing Sepsis MortalityRichard BunPas encore d'évaluation
- Electrocardiographic Artifact MisleadiDocument5 pagesElectrocardiographic Artifact MisleadiMSPas encore d'évaluation
- Vocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDocument4 pagesVocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDivine Jane PurciaPas encore d'évaluation
- Cairns 1976Document14 pagesCairns 1976Direvald WesterosPas encore d'évaluation
- Apixaban For Stroke Prevention in Subclinical AFDocument11 pagesApixaban For Stroke Prevention in Subclinical AFalaahossam591Pas encore d'évaluation
- Eurheartj Ehu033 FullDocument7 pagesEurheartj Ehu033 FullVictor J CadenaPas encore d'évaluation
- Patient's Cures His Snoring: The EditorDocument1 pagePatient's Cures His Snoring: The EditorDiegoPas encore d'évaluation
- Clinical Anesthesiology II: Lessons from Morbidity and Mortality ConferencesD'EverandClinical Anesthesiology II: Lessons from Morbidity and Mortality ConferencesPas encore d'évaluation
- Cardiology Clinic 2006Document620 pagesCardiology Clinic 2006JoNykolasPas encore d'évaluation
- Clinical Practice: History SubtypesDocument6 pagesClinical Practice: History SubtypesRafael Alejandro Marín GuzmánPas encore d'évaluation
- Spine: Essential Neurosurgery For Medical StudentsDocument29 pagesSpine: Essential Neurosurgery For Medical StudentsAndreea IduPas encore d'évaluation
- CRQs and SBAs for the Final FRCA: Questions and detailed answersD'EverandCRQs and SBAs for the Final FRCA: Questions and detailed answersPas encore d'évaluation
- Operating Room Blood Delivery Turnaround Time: Letters To The EditorDocument5 pagesOperating Room Blood Delivery Turnaround Time: Letters To The EditorWilmer UcedaPas encore d'évaluation
- Atlases of Clinical Nuclear Medicine: Series Editor: Douglas Van NostrandDocument149 pagesAtlases of Clinical Nuclear Medicine: Series Editor: Douglas Van NostrandNeide CarvalhoPas encore d'évaluation
- Case Report MisoprostolDocument1 pageCase Report MisoprostolSAID ARCINIEGASPas encore d'évaluation
- Cardiogenic Shock in Children 2024Document14 pagesCardiogenic Shock in Children 2024Pediatrician Suhail NaikPas encore d'évaluation
- Li 1995Document5 pagesLi 1995Mumtaz MaulanaPas encore d'évaluation
- Sacks, Oliver - The Prevalence of Migraine in Neurologists (Letter) (2004)Document1 pageSacks, Oliver - The Prevalence of Migraine in Neurologists (Letter) (2004)uerico roehePas encore d'évaluation
- Trepopnea in CHFDocument4 pagesTrepopnea in CHFprobowurPas encore d'évaluation
- ErrythmiaDocument5 pagesErrythmiaAlen AlanoPas encore d'évaluation
- Emp SyncopeDocument20 pagesEmp SyncopeWilmer JimenezPas encore d'évaluation
- Lin 2009Document7 pagesLin 2009Nur Syamsiah MPas encore d'évaluation
- Research Integration 1Document2 pagesResearch Integration 1Joseph TheThirdPas encore d'évaluation
- Neurology: Self-Assessment for MRCP(UK) Neurology SCED'EverandNeurology: Self-Assessment for MRCP(UK) Neurology SCEÉvaluation : 5 sur 5 étoiles5/5 (1)
- Asma Brittle PDFDocument7 pagesAsma Brittle PDFintankmlsPas encore d'évaluation
- MRCP(UK) and MRCP(I) Part I Best of Fives: Volume ID'EverandMRCP(UK) and MRCP(I) Part I Best of Fives: Volume IPas encore d'évaluation
- Stanford NYU Living Under DronesDocument182 pagesStanford NYU Living Under DronesGabriela FrederickPas encore d'évaluation
- The Best Things in The WorldDocument1 pageThe Best Things in The WorldGabriela FrederickPas encore d'évaluation
- MIS HersheysDocument31 pagesMIS HersheysKaustubh Kirti100% (1)
- Cadbury SuccessDocument30 pagesCadbury SuccessGabriela FrederickPas encore d'évaluation
- MIS HersheysDocument31 pagesMIS HersheysKaustubh Kirti100% (1)
- RANBAXYDocument76 pagesRANBAXYRickyMartynPas encore d'évaluation
- Macroeconomics QuestionsDocument2 pagesMacroeconomics QuestionsGabriela FrederickPas encore d'évaluation
- LitfibaDocument6 pagesLitfibaGabriela FrederickPas encore d'évaluation
- Full Circle Magazine - Issue 1Document42 pagesFull Circle Magazine - Issue 1ChiChiChen100% (3)
- DissertationJunaisHabeebMokkath PDFDocument144 pagesDissertationJunaisHabeebMokkath PDFGabriela FrederickPas encore d'évaluation
- Robert MusilDocument7 pagesRobert MusilGabriela Frederick0% (1)
- Barb:ClericDocument4 pagesBarb:ClericGabriela FrederickPas encore d'évaluation
- Full Circle Magazine Issue 89Document56 pagesFull Circle Magazine Issue 89Gabriela FrederickPas encore d'évaluation
- MAIC Medical DirectorDocument1 pageMAIC Medical DirectorGabriela FrederickPas encore d'évaluation
- Scribd TestDocument3 pagesScribd TestGabriela FrederickPas encore d'évaluation
- Idwd 2. Lies 3. BST 4. Existence 5. I Will Be 6. MortalDocument1 pageIdwd 2. Lies 3. BST 4. Existence 5. I Will Be 6. MortalGabriela FrederickPas encore d'évaluation
- HGFHFGVBC, DSF, DSG, 337-Chap-003Document38 pagesHGFHFGVBC, DSF, DSG, 337-Chap-003Gabriela FrederickPas encore d'évaluation
- Black Widow Spider BiteDocument1 pageBlack Widow Spider BiteGabriela FrederickPas encore d'évaluation
- HP Z27Document6 pagesHP Z27Gabriela FrederickPas encore d'évaluation
- GeneticsDocument25 pagesGeneticsGabriela FrederickPas encore d'évaluation
- Isolation: To Marguerite: by Matthew ArnoldDocument1 pageIsolation: To Marguerite: by Matthew ArnoldGabriela FrederickPas encore d'évaluation
- Scribd TestDocument3 pagesScribd TestGabriela FrederickPas encore d'évaluation
- If You Forget Me by Pablo NerudaDocument2 pagesIf You Forget Me by Pablo NerudaWesleyPas encore d'évaluation
- Protect A.: Uninterruptible Security For PCS, Workstations and Telephone SystemsDocument2 pagesProtect A.: Uninterruptible Security For PCS, Workstations and Telephone SystemsGabriela FrederickPas encore d'évaluation
- Kronig Penney ModelDocument10 pagesKronig Penney ModelPhạm Hầu Thanh ViệtPas encore d'évaluation
- HiilimurtumiaDocument8 pagesHiilimurtumiaGabriela FrederickPas encore d'évaluation
- Cadmium Selenide (CdSe) SemiconductorsDocument2 pagesCadmium Selenide (CdSe) SemiconductorsGabriela FrederickPas encore d'évaluation
- HP Z27Document6 pagesHP Z27Gabriela FrederickPas encore d'évaluation
- Helm PCB - 8088 ComputerDocument9 pagesHelm PCB - 8088 ComputerGabriela FrederickPas encore d'évaluation
- SpagoBI 4.x Quick Installation Guide (English)Document13 pagesSpagoBI 4.x Quick Installation Guide (English)h_20Pas encore d'évaluation
- P CS 32 Anaphylaxis Recognition and Treatment PolicyDocument29 pagesP CS 32 Anaphylaxis Recognition and Treatment Policygeorgios kouvariotisPas encore d'évaluation
- Allergy Free Zone and List of AllergensDocument3 pagesAllergy Free Zone and List of AllergensPatsy YazdiPas encore d'évaluation
- Mustard Allergy: The FactsDocument5 pagesMustard Allergy: The FactsAnonymous GBge2ED1OPas encore d'évaluation
- AnaphylaxisDocument10 pagesAnaphylaxisMadyline VictoryaPas encore d'évaluation
- Case Presentation AnaphylaxisDocument14 pagesCase Presentation AnaphylaxisKevin GarciaPas encore d'évaluation
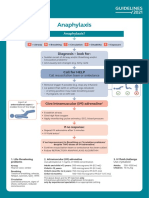
- Anaphylaxis Algorithm 2021Document1 pageAnaphylaxis Algorithm 2021Shawn Gaurav JhaPas encore d'évaluation
- Adverse EffectsDocument27 pagesAdverse EffectsNoha AzzamPas encore d'évaluation
- For COT 4th QDocument12 pagesFor COT 4th QMelbourneSinisinPas encore d'évaluation
- Betahistine Drug InfoDocument3 pagesBetahistine Drug InfoAshish KarnPas encore d'évaluation
- Bee Stings Immunology Allergy and Treatment Marterre PDFDocument9 pagesBee Stings Immunology Allergy and Treatment Marterre PDFOktaviana Sari DewiPas encore d'évaluation
- First Aid - NSTPDocument47 pagesFirst Aid - NSTPGoryo ErmitaPas encore d'évaluation
- Compliment-Mediated Immune Responses: Response EffectsDocument12 pagesCompliment-Mediated Immune Responses: Response EffectsbiancameePas encore d'évaluation
- Care of Client in Acute Biologic CrisisDocument16 pagesCare of Client in Acute Biologic CrisisMerlene Sarmiento SalungaPas encore d'évaluation
- SympatheticDocument10 pagesSympatheticSharneeshriyaPas encore d'évaluation
- Root Cause AnalysisDocument8 pagesRoot Cause Analysisapi-533686691Pas encore d'évaluation
- Drug Name Indication Mode of Action Contraindications Side Effects Nursing ConsiderationsDocument3 pagesDrug Name Indication Mode of Action Contraindications Side Effects Nursing ConsiderationsAlyssa RodriguezPas encore d'évaluation
- AnaphylaxisDocument15 pagesAnaphylaxisThaer ZabenPas encore d'évaluation
- Managing Anaphylactic Shock Journal of Modern Pharmacy 2006Document3 pagesManaging Anaphylactic Shock Journal of Modern Pharmacy 2006Saputro AbdiPas encore d'évaluation
- AnaphylaxisDocument17 pagesAnaphylaxisPutriAyuWidyastutiRPas encore d'évaluation
- CefepimeDocument2 pagesCefepimeshendae cosmianoPas encore d'évaluation
- Insects Bites and StingsDocument13 pagesInsects Bites and StingsRisavina Dorothy CondorPas encore d'évaluation
- Sementis IM June 2011Document21 pagesSementis IM June 2011zozareliPas encore d'évaluation
- Anafilaktik ShockDocument14 pagesAnafilaktik ShockFattan GemsPas encore d'évaluation
- Quick Reference GuideDocument5 pagesQuick Reference GuidePatsy YazdiPas encore d'évaluation
- Summary of Product Characteristics (SMPC)Document13 pagesSummary of Product Characteristics (SMPC)Asif ZamanPas encore d'évaluation
- Data Sheet Data Sheet: Gelafusal GelafusalDocument2 pagesData Sheet Data Sheet: Gelafusal Gelafusalfahri azwarPas encore d'évaluation
- Anaphylaxis: Article OutlineDocument47 pagesAnaphylaxis: Article OutlineJhovan AcePas encore d'évaluation
- Drug Allergy: DR Sana Nisar ZaidiDocument34 pagesDrug Allergy: DR Sana Nisar ZaidisaraPas encore d'évaluation
- Emergencies in Dental Clinic: How To DealDocument94 pagesEmergencies in Dental Clinic: How To DealhassonamonaPas encore d'évaluation
- Immuno and InfectiousDocument17 pagesImmuno and Infectiousgreen_archerPas encore d'évaluation