Académique Documents
Professionnel Documents
Culture Documents
2011 Poverty Food Insecurity Williams
Transféré par
wahyupujilestari0 évaluation0% ont trouvé ce document utile (0 vote)
16 vues9 pagesabout poverty food insecurity
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentabout poverty food insecurity
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
16 vues9 pages2011 Poverty Food Insecurity Williams
Transféré par
wahyupujilestariabout poverty food insecurity
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 9
NEW RESEARCH
Poverty, Food Insecurity, and the Behavior
for Childhood Internalizing
and Externalizing Disorders
Natalie Slopen, M.A., Garrett Fitzmaurice, Sc.D., David R. Williams, M.P.H., Ph.D.,
Stephen E. Gilman, Sc.D.
Objective: This study investigated the associations of poverty and food insecurity over a
2-year period with internalizing and externalizing problems in a large, community-based
sample. Method: A total of 2,810 children were interviewed between ages 4 and 14 years at
baseline, and between ages 5 and 16 years at follow-up. Primary caregivers reported on
household income, food insecurity, and were administered the Child Behavior Checklist, from
which we derived indicators of clinically signicant internalizing and externalizing problems.
Prevalence ratios for the associations of poverty and food insecurity with behavior problems
were estimated. Results: At baseline, internalizing and externalizing problems were signif-
icantly more prevalent among children who lived in poor households than in nonpoor
households, and among children who lived in food insecure households than in food-secure
households. In adjusted analyses, children from homes that were persistently food insecure
were 1.47 (95% CI 1.12 to 1.94) times more likely to have internalizing problems and 2.01
(95% CI 1.21 to 3.35) times more likely to have externalizing problems compared with
children from households that were never food insecure. Children from homes that moved
from food secure to insecure were 1.78 (95% CI 1.07 to 2.94) times more likely to have
externalizing problems at follow-up. Conclusions: Persistent food insecurity is associated
with internalizing and externalizing problems, even after adjusting for sustained poverty and
other potential confounders. These results implicate food insecurity as a novel risk factor for
child mental well-being; if causal, this represents an important factor in the etiology of child
psychopathology, and potentially a new avenue for prevention. J. Am. Acad. Child Adolesc.
Psychiatry, 2010;49(5):444452. Key Words: Food insecurity, Poverty, Internalizing prob-
lems, Externalizing problems, Prospective.
P
overty and food insecurity have adverse
impacts on the course of child develop-
ment, in part by raising the risk for care-
giver depression
1-3
and for chronic iron de-
ciency and vitamin deciencies.
4,5
According to
the U.S. Census, 37.3 million persons in the
United States (12.5%) were poor in 2007, as
specied by the U.S. federal poverty guidelines,
which take into account total household income
and number of people residing in the household;
for a family of four, this equates to an income
below $21,203.
6
During this time, approximately
18.0% of children were poor, with black (or
African American) and Hispanic children dispro-
portionately affected. Food insecurity, dened as
limited or uncertain availability of food because
of inadequate resources, is one of many difcul-
ties associated with poverty.
7
In a 2007 report, the
U.S. Department of Agriculture estimated that
11% of U.S. households experienced food insecu-
rity in 2005. Food insecurity was almost twice as
common for households with children relative to
households without children (15.6% vs. 8.5%),
and 30% of single female-households were food
insecure.
7
Like poverty, risk of food insecurity is
also patterned by race/ethnicity. In the U.S.,
there is overlap in the populations of individuals
meeting the denitions of poverty and food in-
security; yet, individuals with food insecurity are
This article is discussed in an editorial by Dr. Tamara Dubowitz on
page 437.
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 444 www.jaacap.org
not always poor, and poor individuals are not
always food insecure.
7
For children, experiences
of household poverty and/or food insecurity
may have an impact on numerous domains of
life, including family processes and parental
well-being, cognitive and academic performance,
and general health outcomes; each of these fac-
tors may affect internalizing or externalizing
problems.
8,9
There is limited prospective research that has
considered the relationship among poverty, food
insecurity, and childrens mental health. Prospec-
tive study designs enable a rigorous test of the
effect of these determinants on child mental
health, and are most informative for examining
causal inference; this is of substantial importance
for researchers and clinicians who are interested
in identifying optimal points for intervention.
Several prospective studies on the relationship
between poverty and child psychopathology
suggest that chronic poverty is associated with
an elevated risk of psychopathology.
10-13
For
example, Bor et al.
10
found that chronic low
family income (near or below the poverty line in
Australia) was associated with an increased risk
of internalizing, externalizing, and social, atten-
tional, and thought problems at age 5 years.
10
Costello et al
11
found that an income supplemen-
tation that moved families out of poverty was
associated with a reduction in oppositional de-
ant disorder and conduct disorder symptoms.
After the income supplementation, the level of
behavioral symptoms for children who were
poor at baseline but no longer poor at follow-up
fell to those of children who were never poor,
whereas the level of symptoms among persis-
tently poor children remained elevated in com-
parison to the never-poor children.
We are not aware of any prospective research
on poverty and child mental health that has
addressed the issue of food insecurity; however,
cross-sectional studies suggest an independent
link between food insecurity and higher levels of
child behavioral/emotional problems.
2,14-19
For
example, Whitaker et al.
2
analyzed data from the
Fragile Families and Child Wellbeing Study and
found a positive gradient in the prevalence of
child behavior problems with increasing levels of
food insecurity among children at age 3 years
(i.e., 22.7% for those who were fully food inse-
cure, 31.1% for marginally food insecure, and
36.7% for food insecure). Alaimo et al.
14
analyzed
nationally representative adolescent data and
found that food-insufcient adolescents were ap-
proximately four times more likely to meet diag-
nostic criteria for dysthymia and ve times more
likely to have made a suicide attempt; in contrast,
low family income (i.e., 130% of the poverty
line) did not predict these outcomes. We were
able to locate only one study that used a prospec-
tive design to examine the impact of food inse-
curity on child development,
20
although this
study focused on social skills rather than inter-
nalizing and externalizing symptoms. Although
prospective research on food insecurity and child
mental health is lacking, there has been some
work in this area with adults. In a prospective
study over 3 years, Hein et al
1
found that onset
of food insufciency status was positively asso-
ciated with onset of maternal major depression
status while adjusting for many sociodemo-
graphic characteristics, including income. The
Project on Human Development in Chicago
Neighborhoods (PHDCN) provides an opportu-
nity to investigate the role of poverty and food
insecurity on risk for childhood psychopathol-
ogy. The present study used data over a 2 year
period to examine the impact of trajectories of
household poverty and food insecurity on
change in child outcomes. We hypothesized that
(a) persistent poverty and movement into pov-
erty status are positively associated with inter-
nalizing and externalizing problems, and (b) per-
sistent food insecurity and movement into food
insecure status are positively associated with
internalizing and externalizing problems.
METHOD
Sample
The PHDCN includes a prospective study of children
and their families from 80 distinct neighborhoods over
an 8-year period (19952002). A three-stage sampling
design was used to enroll children and their primary
caregivers into the study: rst, 80 neighborhood clus-
ters from all neighborhoods in Chicago were selected
based on a stratied probability sample of neighbor-
hood clusters heterogeneous on race, ethnicity, and
income; second, block groups within each neighbor-
hood cluster were selected; and third, households with
children 6 months post partum, aged 3, 6, 9, 12, 15, and
18 living in the selected block groups, were enrolled in
the study.
21
The participation rate at the time of
recruitment was 75%. The current study uses data
from children aged 4 through 14 years collected be-
tween 1997 and 2001; children and primary caregivers
were interviewed twice, with an average period of 24
months between interviews.
POVERTY, FOOD INSECURITY, AND BEHAVIOR
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 445 www.jaacap.org
Internalizing and Externalizing Problems
Internalizing and externalizing problems were measured
using the Child Behavior Checklist (CBCL) for children 4
through 18 years of age.
22
This measure was adminis-
tered to the primary caregiver at baseline and follow-up.
The CBCL contains questions pertaining to the childs
emotions and behavior in the past 6 months. The care-
giver was asked to identify whether each statement has
been very true, somewhat true, or not true. The
internalizing subscale provides a rating for the extent to
which the child has exhibited symptoms of anxiety,
depression, or withdrawal. The externalizing subscale
provides a rating of the extent to which the child has
exhibited symptoms of aggression, hyperactivity, or non-
compliance. Both scales have satisfactory validity and
internal consistency.
22
We dened problem levels of
internalizing and externalizing as scores at or above the
90
th
percentile (T-score 64, based on published norms).
High scores on the CBCL 1991/4-18 correspond closely
to clinical diagnostic outcomes (i.e., anxiety, mood, dis-
ruptive behavior, and conduct disorders)
23,24
dened by
the Diagnostic and Statistical Manual of Mental Disor-
der(DSM) III-R
25
Poverty Status
Family poverty was dened according to the U.S.
federal poverty threshold, which was originally de-
signed to identify individuals and families with insuf-
cient income to meet basic needs. The federal poverty
threshold takes into account total household income
and number of persons living in the household. We
created a measure of income to needs for this study
by calculating a ratio of household income over the
federal poverty threshold; an income-to-needs ratio of
less than 1 indicates that a family is below the poverty
line. The federal poverty threshold has particular sa-
lience for the current study, given that government
benets such as welfare are linked to it. We dened
family poverty over the course of the study based on
poverty status at both time points (persistently poor,
previously poor, newly poor, and never poor).
Food Insecurity
Food insecurity refers to limited or uncertain access
to nutritionally adequate and safe foods due to lack of
resources (p. 278).
26
The current gold-standard mea-
sure of food insecurity is the 18-item U.S. Food Secu-
rity Scale, which includes eight child-referenced items
that make up the Childrens Food Security Scale.
7
Unfortunately, the PHDCN did not include a validated
measure of food insecurity; only a single item was
included, which may only partially capture the con-
struct of interest. In this study, the primary caregiver
provided information about household food insecurity
status at baseline and follow-up in response to a single
question, which referred to the past 6 months: Has
there been a time when there was not enough money
at home to buy food? (yes/no). This variable was
strongly correlated with caregiver report of having to
cut his/her meal size one or more times in the past 6
months (correlation 0.65, p .0001), which provides
some assurance that our item reect the construct of
interest. These two items were the only interview
questions that measured access to food. We created a
four-category variable to reect trajectory of food
insecurity over time (persistently food insecure, previ-
ously food-insure, newly food insecure, never food
insecure).
Demographic Characteristics
We included several child and primary caregiver co-
variates in the analyses. Child covariates included age
at interview, gender, and race/ethnicity (black, white,
Hispanic, and other). Household characteristics in-
cluded the number of people residing in the house-
hold, and caregiver cohabitation status over time
(never partnered/married; newly partnered/married;
previously partnered/married; always partnered/
married). Primary caregiver covariates included age at
baseline and follow-up, education at baseline (high
school degree vs. less than high school), major depres-
sion at baseline (based on an adapted version of the
Composite International Diagnostic Interview short
form for DSM-IV
27
), and alcohol problems at baseline
(dened as a scoring 3 on the Short Michigan Alco-
hol Screening Test
28
).
Statistical Analyses
Regression analyses were used to relate internalizing
and externalizing problems to patterns of poverty and
food insecurity. Our rst set of models examined
baseline associations among poverty, food insecurity,
and problem status while adjusting for sociodemo-
graphic characteristics of the child (age, gender, and
race/ethnicity), household (cohabitation status, num-
ber of persons in the household), and caregiver (age,
depression, education, and alcohol problem). Our sec-
ond set of models examined the effect of poverty and
food insecurity trajectories on internalizing and exter-
nalizing problems at follow-up, controlling for base-
line problem status, and child, household and care-
giver covariates. The prospective models for
internalizing and externalizing problems followed the
same model-building strategy: the rst two models
estimated the separate effects of poverty and food
insecurity, and the third model included poverty and
food insecurity simultaneously. All analyses were
based on Poisson regression models, which yield prev-
alence ratios for the relation between the risk factors of
interest and child internalizing and externalizing prob-
lems.
29-31
Generalized estimating equations were used
to obtain variance estimates that account for the nested
structured of the data.
SLOPEN et al.
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 446 www.jaacap.org
Across the variables in our analysis, the percentage
of participants with missing data ranged from 0% to
27%; more than half of our sample had at least one
missing value, and the overall participation rate at
wave 3 was 79.5%. Multiple imputation of missing
data was performed using IVEware,
32
retaining all
respondents who were enrolled in age cohorts 3, 6, and
9 at wave 1 (N 2,810). This strategy best preserved
the original sample characteristics and reduced bias
that could result from attrition. PROC MIANALYZE in
SAS v.9.1 was used to combine the results from the 10
imputed datasets for all analyses.
RESULTS
The mean age of the child participants was 8.2
years at baseline, and 10.7 years at follow-up
(Table 1). Female participants comprised slightly
more than half of the sample (50.5%). Approxi-
mately 32% of the sample was non-Hispanic
black, 14% was non-Hispanic white, 42% was
Hispanic, and 12% was coded as other race.
The mean age of the primary caregivers in the
sample was 35.6 years at baseline and 38.1 years
at follow-up. The prevalence of poverty and food
insecurity declined between baseline and follow-
up: at baseline, 40% of families in the study were
below the poverty line, and 23% of families were
food insecure; at follow-up, the prevalences fell
to 30% and 18%, respectively. Although poverty
and food insecurity have some degree of overlap,
these constructs are not entirely overlapping: at
baseline, 52% of the sample was neither food
insecure or poor, whereas 15% of our sample was
both food insecure and poor; 8% was food inse-
cure but not poor, whereas 25% was poor but not
food insecure.
The prevalence of internalizing and externaliz-
ing problems was stable across waves, with ap-
proximately 18% of children categorized as having
internalizing problems, and 7% of children catego-
rized as having externalizing problems at both time
points. There was a relatively high degree of co-
morbidity between internalizing and externalizing
problems: at baseline, 27% of children with inter-
nalizing problems also met criteria for externalizing
problems; at follow-up, 25% of children with inter-
TABLE 1 Characteristics of Study Participants (N 2,810)
Characteristic
Baseline Follow-up
N % Mean (SE) N % Mean (SE)
Below poverty line 1,135 40.38 856 30.48
Food insecure 643 22.90 516 18.36
Total household income ($ US) 2,810 31,1163 (481.11) 2810 37,669 (1101.54)
Child characteristics
Internalizing problems 508 18.07 482 17.16
Externalizing problems 213 7.57 191 6.79
Child age (years) 2,810 8.16 (0.05) 2810 10.67 (0.08)
Gender
Male 1,391 49.50
Female 1,419 50.50
Race
Non-Hispanic black 897 31.92
Non-Hispanic white 388 13.82
Hispanic 1,195 42.54
Other 329 11.72
Primary caregiver
characteristics
Caregiver age, years 2,810 35.58 (0.31) 2810 38.09 (0.29)
Less than high school
education
1059 37.70
Caregiver depression 416 14.82
Caregiver alcohol problem 96 3.43
No live-in partner/spouse 915 32.57 907 32.28
Number in household 2810 5.34 (0.05) 2810 5.22 (0.14)
Note: N values are based on multiply imputed data, and are shown rounded to full numbers. SE standard error for parameter estimates.
POVERTY, FOOD INSECURITY, AND BEHAVIOR
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 447 www.jaacap.org
nalizing problems also met criteria for externalizing
problems. Internalizing and externalizing problems
were signicantly more prevalent among children
who lived in poor households as compared with
nonpoor households (internalizing problems:
22.3% vs. 15.2%, p .0001; externalizing problems:
10.3% vs. 5.7%, p .0001), and among children
who lived in food-insecure households as com-
pared with food-secure households (internalizing
problems: 27.6% vs. 15.4%, p .0001; externalizing
problems: 10.6% vs. 6.7%, p 0.002). Children
exposed to poverty and food insecurity at the same
time had the greatest prevalence of internalizing
problems (30.0%) and externalizing problems
(12.3%) relative to all other groups.
Before examining the prospective associations
among poverty, food insecurity, and childhood
internalizing and externalizing problems, we ex-
amined the baseline associations, adjusted for
child, household, and caregiver characteristics
(child age, gender, race/ethnicity; caregiver age,
cohabitation status, depression, alcohol prob-
lems, education; and number in the household).
In this analysis, poverty status was signicantly
associated with internalizing problems: children
from households below the poverty line were
1.32 (95% CI 1.08 to 1.62) times more likely to
have internalizing problems, relative to children
from households above the poverty line. Poverty
status was also associated with externalizing
problems (prevalence ratio [PR] 1.38, CI 0.99
to 1.92). Children in food insecure households
were 1.49 (95% CI 1.24 to 1.79) times more
likely to have internalizing problems, and 1.47
(95% CI 1.10 to 1.97) times more likely to have
externalizing problems, relative to children in
food secure households.
Internalizing and Externalizing Problems Over the
Follow-Up Period
Internalizing Problems. In the prospective models
adjusted for prior problem status and sociode-
mographic characteristics (Table 2), persistent
poverty was marginally associated with internal-
izing problems at follow-up (PR 1.33, 95% CI
0.99 to 1.77). Movement into poverty status was
not signicantly associated with internalizing
problems, although the effect estimate was in the
expected direction (PR 1.35, 95% CI 0.94 to
1.93). In contrast, there was a signicant associa-
tion between persistent food insecurity and inter-
nalizing problems: children from homes that
were food insecure at baseline and follow-up
(i.e., persistent food insecurity) were 1.56 (95% CI
1.20 to 2.02) times more likely to have inter-
nalizing problems, relative to children from
homes that were never food insecure. Children
from homes that moved from food secure at
baseline to food insecure at follow-up were 1.39
times more likely to have internalizing problems
at follow up, although this association did not
TABLE 2 Estimated Prevalence Ratios (and 95% Condence Intervals) for Internalizing Problems at Follow-up
(N 2,810)
a
Number with
Internalizing
Problems
% with Internalizing
Problems in Each
Category Model 1 Model 2 Model 3
Poverty Status
Persistently poor 150 22.38 1.33 (0.99, 1.77) 1.21 (0.89, 1.65)
Previously poor 88 18.94 1.13 (0.84, 1.51) 1.08 (0.80, 1.46)
Newly poor 38 20.62 1.35 (0.94, 1.93) 1.25 (0.87, 1.81)
Never poor 206 13.83 1.00 1.00
Food Insecurity Status
Persistently food insecure 83 31.24 1.56 (1.20, 2.02)** 1.47 (1.12, 1.94)*
Previously food insecure 81 21.26 1.22 (0.93, 1.59) 1.19 (0.90, 1.56)
Newly food insecure 56 22.34 1.39 (0.98, 1.99) 1.37 (0.96, 1.96)
Never food insecure 263 13.72 1.00 1.00
Note: N values are based on multiply imputed data, and are shown rounded to full numbers.
a
In addition to covariates presented, all models adjusted for child characteristics (gender, age, race, and internalizing problems at baseline), caregiver
characteristics (age, education, cohabitation status, depression, and alcohol problem), and number people living in the household. Prevalence ratios
should be interpreted as the increase or decrease in the probability of internalizing or externalizing problems, in comparison to the reference level.
*p 0.05; **p 0.01.
SLOPEN et al.
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 448 www.jaacap.org
reach statistical signicance (95% CI 0.98 to
1.99). As shown in model 3, persistent food
insecurity was a signicant predictor of internal-
izing problems at follow-up, even when poverty
trajectory is included in the model (PR 1.47,
95% CI 1.12 to 1.94).
Externalizing Problems. Persistent poverty and
movement into poverty status were not signi-
cantly associated with externalizing problems at
follow-up (Table 3). However, signicant associ-
ations were observed for trajectories of house-
hold food insecurity. Children from homes that
were food insecure at baseline and follow-up
(i.e., that experienced persistent food insecurity)
were 2.11 (95% CI 1.30 to 3.45) times more
likely to have externalizing problems at follow-
up, relative to children from homes that were
never food insecure. In addition, children from
homes that moved from food secure at baseline
to food insecure at follow-up were 1.80 (95% CI
to 1.09 to 2.98) times more likely to have exter-
nalizing problems at follow-up, relative to chil-
dren from homes that were food secure at both
times. The associations between persistent food
insecurity and movement into food insecurity
status with externalizing problems remained sig-
nicant even when trajectory of poverty status
was included in the model (model 3). Of note, a
comparable set of analyses of the continuous
scores for internalizing and externalizing symp-
toms yielded similar results.
Finally, to test the sensitivity of the poverty
threshold used in the prospective analyses, we
reanalyzed the data with the threshold for pov-
erty status set to 130% of the federal poverty line
(the eligibility standard for the federal Supple-
mental Nutrition Assistance Program); in these
analyses, the prevalence ratios were largely
unchanged.
DISCUSSION
The present study used data from two waves of
the PHDCN to investigate associations among
poverty, food insecurity, and child mental health.
Our ndings are of importance from a preven-
tion standpoint, because both poverty and food
insecurity are modiable conditions that can be
addressed through social and economic interven-
tions at the level of the community, state, or
federal government.
33,34
The analyses of baseline
data revealed that children from households be-
low the poverty line were signicantly more
likely to have internalizing problems, and that
children from food insecure households were
signicantly more likely to have internalizing
and externalizing problems, independent of pov-
erty status.
TABLE 3 Estimated Prevalence Ratios (and 95% Condence Intervals) for Externalizing Problems at Follow-up
(N 2,810)
a
Number With
Externalizing
Problems
Percent With
Externalizing
Problems in
Each Category Model 1 Model 2 Model 3
Poverty status
Persistently poor 75 11.16 1.37 (0.91, 2.06) 1.17 (0.76, 1.80)
Previously poor 26 5.52 0.88 (0.49, 1.58) 0.83 (0.47, 1.45)
Newly poor 18 9.88 1.31 (0.70, 2.45) 1.21 (0.67, 2.18)
Never poor 72 4.84 1.00 1.00
Food insecurity status
Persistently food insecure 38 14.49 2.11 (1.30, 3.45)** 2.01 (1.21, 3.35)**
Previously food insecure 31 8.20 1.52 (0.91, 2.54) 1.51 (0.88, 2.56)
Newly food insecure 30 11.76 1.80 (1.09, 2.98)* 1.78 (1.07, 2.94)*
Never food insecure 92 4.80 1.00 1.00
Note: N values are based on multiply imputed data, and are shown rounded to full numbers.
a
In addition to covariates presented, all models adjusted for child characteristics (gender, age, race/ethnicity, and externalizing problems at baseline),
caregiver characteristics (age, education, cohabitation status, depression, and alcohol problem), and number of persons living in household. Prevalence
ratios should be interpreted as the increase or decrease in the probability of internalizing or externalizing problems, in comparison to the reference level.
*p 0.05; **p 0.01.
POVERTY, FOOD INSECURITY, AND BEHAVIOR
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 449 www.jaacap.org
In the prospective analysis, although the asso-
ciations were in the expected direction, trajectory
of poverty status did not signicantly predict
internalizing or externalizing problems, control-
ling for prior problem status, and other charac-
teristics. This nding was contrary to our rst
hypothesis and was inconsistent with prior re-
search that has documented an association be-
tween poverty trajectory and change in mental
health.
11,13
These results may differ from previ-
ous research because of study design: our study
included only two waves of data, with approxi-
mately 2 years between data collection, whereas
other studies have had a longer observation
period and/or more frequent assessment and
have used symptom scores rather than diagnostic
outcomes.
11,13,35
Our ndings for the trajectory of
food insecurity provided support for our second
hypothesisnamely, that children who lived in
households that were food insecure at both time
points had a greater likelihood of internalizing
and externalizing problems at follow-up, inde-
pendent of problem status at baseline. The strong
and signicant associations between persistent
food insecurity and internalizing and externaliz-
ing problems after adjustment for poverty status
indicates that the associations between food in-
security and internalizing and externalizing
problems are not confounded by poverty status.
Our pattern of results raises several questions.
In particular, it is noteworthy that household
poverty is signicantly associated with internal-
izing problems and marginally associated with
externalizing problems in the cross-sectional
analysis of the baseline data, but that persistent
poverty or movement into poverty status was not
a statistically signicant predictor of internaliz-
ing or externalizing problems at follow-up. This
inconsistency may be caused by unadjusted con-
founding in the cross-sectional results that is
accounted for in the prospective analyses by
control of prior internalizing or externalizing
problem status. Alternatively, it could also be
linked to length of follow-up. It is also challeng-
ing to reconcile our ndings that trajectory of
food insecurity is predictive of internalizing and
externalizing problems at follow-up, yet trajec-
tory of poverty status is not. It is possible that
food insecurity is a more proximal measure of
stress load in the household, which may ulti-
mately lead to the associations we observe. Fi-
nally, it is puzzling that caregiver depression
(measured at baseline) is a signicant predictor
of internalizing and externalizing problems at
baseline but not at follow-up; this may suggest
that the effects of caregiver depression on child
outcomes are largely contemporaneous in nature,
rather than persisting over the long term. Unfor-
tunately, we are unable to examine the associa-
tion between caregiver depression at follow-up
and behavior at follow-up because we do not
have a usable measure of caregiver depression at
this time.
Several mechanisms may explain the associ-
ations between food insecurity and mental
health problems that we observed. Food and
nutrition are important aspects of daily life;
psychologically, routines involving food are
important for the childs comfort and feelings
of security. Moreover, all individuals in the
household are potentially affected by food in-
security; therefore mental and physical well-
being of family members may be compromised,
which may have an impact on familial efcacy
for a wide range of activities.
9
In addition, food
insecurity may have negative consequences for
a childs nutrient balance and physical health,
as well as cognitive and academic outcomes,
which place children at risk for the develop-
ment of behavior problems.
9,36
Each of these
potential mechanisms represents an important
direction for future research.
The ndings for this study should be consid-
ered in the context of several limitations. First,
household food insecurity was measured using a
single dichotomous question; this crude measure
is not able to capture the full extent of food
insecurity that a child has experienced, and does
not measure child hunger experiences. However,
within our data, this single-item measure is
strongly correlated with caregiver report of cut-
ting meal sizes, which indicates a lack of food
available to members in the household. Evidence
suggests that even slight forms of food insecurity
and undernutrition can have lasting effects;
37
therefore we believe that the available measure is
a useful, albeit imperfect, indicator. Second, our
study is limited by incomplete data and loss to
follow-up. We controlled for variables associated
with attrition, which should prevent bias; in
addition, we used multiple imputation to pre-
serve the original sample composition. Third, the
federal poverty line is not specic to region or
urban/rural location; it is possible that the pov-
erty line does not accurately represent the
amount of money that a family requires to be
SLOPEN et al.
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 450 www.jaacap.org
self-sufcient in an urban area such as Chicago.
As a result, some individuals categorized as
nonpoor might meet criteria for poor if the
threshold was adjusted for city-specic costs of
living. However, as noted in the results section,
our sensitivity analysis indicated that the results
were largely unchanged when we altered the
threshold for poverty status. Fourth, our mea-
sures of internalizing and externalizing problems
are limited to caregiver report; these ratings may
be biased as the result of caregiver mental health.
Although some researchers have hypothesized
that depressed mothers report distorted percep-
tions of childrens behavior, a review on this
topic did not nd evidence to support this hy-
pothesis.
38
Nevertheless, to rule out this possibil-
ity, we repeated our analyses excluding children
that had caregivers with major depression at
baseline; our ndings remain largely the same.
Finally, although we adjusted for a broad set of
caregiver characteristics, it is important to con-
sider the possibility that unmeasured factors re-
lated to parenting characteristics may predict
both food insecurity and psychological symp-
toms in children. The above limitations highlight
the need for additional prospective research that
includes frequent and detailed measures of chil-
dren and caregivers.
39
The present study has several implications for
understanding the etiology of child psychiatric
disorders, given that CBCL scores converge with
DSM psychiatric diagnoses and reect substan-
tial psychopathology.
23,24
This set of ndings
contributes to our understanding about the etiol-
ogy of childhood disorders, as it demonstrates
that (a) continued exposure to household food
insecurity is predictive of internalizing and ex-
ternalizing problems, and (b) excess risk for
internalizing and externalizing disorders is not
discernible among children who lived in house-
holds that were food insecure at baseline and
then became food secure at follow-up. This sug-
gests that interventions that alleviate household
poverty and food insecurity among families ex-
periencing these conditions may be effective in
reducing the prevalence of childhood behavior
problems. Our ndings illustrate the importance
of screening children and caregivers about their
access to food within the clinical setting, and
developing an infrastructure to connect clients
with nutritional resources (e.g., Supplemental
Nutrition Assistance Program [SNAP], food pan-
tries) when household food insecurity is present.
Our results suggest that in addition to fullling a
physical need, food has an important role in
psychological well-being; therefore, food insecu-
rity may be an important trait for clinicians to
assess, as it may have a role in the development
of behavioral problems.
In conclusion, poverty and food insecurity are
risk factors that can be targeted for intervention.
An example of a successful poverty intervention
is the Minnesota Family Investment Program.
34
This program has demonstrated that increased
employment rates and small increases in income
for working poor parents can reduce child pov-
erty and lead to reductions in externalizing prob-
lems among children. Research has also docu-
mented that the Food Stamp Program (now
referred to as SNAP) and the Special Supplement
Nutrition Program for Women, Infants, and Chil-
dren are able to increase nutrient intake among
low income children.
39
Additional research is
required to expand our ability to effectively pro-
vide adequate nutrition to children and families
that have poor access to high-quality foods, and
to improve our understanding of adequate nu-
trition in relation to child mental health. In
summary, our ndings provide evidence for a
prospective association between food insecurity
and increased risk for internalizing and external-
izing problems. This study highlights the impor-
tance of efforts to develop and strengthen pro-
grams that protect vulnerable families from the
experiences and consequences of poverty and
food insecurity. &
Accepted February 16, 2010.
Ms. Slopen and Drs. Fitzmaurice, Williams, and Gilman are with the
Harvard School of Public Health. Dr. Williams is also with Harvard
University.
This work was supported by a doctoral research award from the
Canadian Institutes of Health Research (Award 200610MDR-
168591-163832).
Disclosure: Ms. Slopen and Drs. Fitzmaurice, Williams, and Gilman
report no biomedical nancial interests or potential conicts of interest.
Correspondence to Natalie Slopen: Department of Society, Human
Development, and Health, Harvard School of Public Health, 677
Huntington Avenue, Boston, MA 02115; e-mail: nslopen@hsph.
harvard.edu
0890-8567/10/2010 American Academy of Child and Adoles-
cent Psychiatry
DOI: 10.1016/j.jaac.2010.01.018
POVERTY, FOOD INSECURITY, AND BEHAVIOR
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 451 www.jaacap.org
REFERENCES
1. Hein CM, Siefert K, Williams DR. Food insufciency and
womens mental health: ndings from a 3-year panel of welfare
recipients. Soc Sci Med. 2005;61:1971-1982.
2. Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks
of depression and anxiety in mothers and behavior problems in their
preschool-aged children. Pediatrics. 2006;118:e859-e868.
3. Beardslee WR, Versage EM, Gladstone TRG. Children of affec-
tively ill parents: a review of the past 10 years. J Am Acad Child
Adolesc Psychiatry. 1998;37:1134-1141.
4. Heseker H, Kubler W, Pudel V, et al. Psychological disorders as
early symptoms of a mild-to-moderate vitamin deciency. Ann N
Y Acad Sci. 1992;669:352-357.
5. Lozoff B, Jimenez E, Hagen J, et al. Poorer behavioral and
developmental outcome more than 10 years after treatment for
iron deciency in infancy. Pediatrics. 2000;105:E51.
6. Bishaw A, Semega J. American Community Survey Reports,
ACS-09, Income, Earnings, and Poverty Data from the 2007
American Community Survey. Washington, DC: U.S. Census
Bureau, U.S. Government Printing Ofce; 2008.
7. Nord M, Andrews M, Carlson S. Measuring Food Security in the
United States: Household Food Security in the United States,
2005. Washington, DC: USDA Economic Research Service. Eco-
nomic Research Report No. 29; 2007.
8. Brooks-Gunn J, Duncan GJ. The effects of poverty on children.
Future Child. 1997;7:55-71.
9. Ashiabi GS, ONeal KK. A framework for understanding the
association between food insecurity and childrens developmen-
tal outcomes. Child Develop Perspect. 2008;2:71-77.
10. Bor W, Najman JM, Andersen MJ, et al. The relationship between
low family income and psychological disturbance in young
children: an Australian longitudinal study. Aust N Z J Psychiatry.
1997;31:664-675.
11. Costello EJ, Compton SN, Keeler G, et al. Relationships between
poverty and psychopathology: a natural experiment. J Am Med
Assoc. 2003;290:2023-2029.
12. Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation
and early child development. Child Dev. 1994;65:296-318.
13. McLeod JD, Shanahan MJ. Trajectories of poverty and childrens
mental health. J Health Soc Behav. 1996;37:207-220.
14. Alaimo K, Olson CM, Frongillo EA. Family food insufciency, but
not low family income, is positively associated with dysthymia
and suicide symptoms in adolescents. J Nutr. 2002;132:719-725.
15. Alaimo K, Olson CM, Frongillo EA, Jr.Food insufciency and
American school-aged childrens cognitive, academic, and psy-
chosocial development. Pediatrics. 2001;108:44-53.
16. Cook JT, Frank DA. Food security, poverty, and human develop-
ment in the United States. Ann N Y Acad Sci. 2008;1136:193-209.
17. Murphy JM, Wehler CA, Pagano ME, et al. Relationship between
hunger and psychosocial functioning in low-income American
children. J Am Acad Child Adolesc Psychiatry. 1998;37:163-170.
18. Rose-Jacobs R, Black MM, Casey PH, et al. Household food
insecurity: associations with at-risk infant and toddler develop-
ment. Pediatrics. 2008;121:65-72.
19. Weinreb L, Wehler C, Perloff J, et al. Hunger: its impact on
childrens health and mental health. Pediatrics. 2002;110:e41.
20. Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school
childrens academic performance, weight gain, and social skills. J
Nutr. 2005;135:2831-2839.
21. Earls F, Buka SL. Project on Human Development in Chicago
Neighborhoods. Washington, DC: National Institute of Justice;
1997.
22. Achenbach TM. Manual for the Child Behavior Checklist/4-18
and 1991 Prole. Burlington, VT: Department of Psychiatry,
University of Vermont; 1991.
23. Kasius MC, Ferdinand RF, van den Berg H, et al. Associations
between different diagnostic approaches for child and adolescent
psychopathology. J Child Psychol Psychiatry. 1997;38:625-632.
24. Ferdinand RF. Validity of the CBCL/YSR DSM-IV scales anxiety
problems and affective problems. J Anxiety Disord. 2008;22:126-
134.
25. American Psychiatric Association. Diagnostic and Statistical Man-
ual of Mental Disorders: DSM-III-R. Washington, DC: American
Psychiatric Association; 1987.
26. Kleinman RE, Murphy JM, Wieneke KM, et al. Use of a single-
question screening tool to detect hunger in families attending a
neighborhood health center. Ambul Pediatr. 2007;7:278-284.
27. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H. The
World Health Organization Composite International Diagnostic
Interview short-form (CIDI-SF). Int J Methods Psychiatr Res.
1998;7:171-185.
28. Selzer ML, Vinokur A, van Rooijen L. A self-administered Short
Michigan Alcoholism Screening Test (SMAST). J Stud Alcohol.
1975;36:117-126.
29. McNutt LA, Wu C, Xue X, et al. Estimating the relative risk in
cohort studies and clinical trials of common outcomes. Am J
Epidemiol. 2003;157:940-943.
30. Zou G. A modied Poisson regression approach to prospective
studies with binary data. Am J Epidemiol. 2004;159:702-706.
31. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or
prevalence ratios and differences. Am J Epidemiol. 2005;162:199-
200.
32. Raghunathan TE, Lepkowski JM, Van Hoewyk J, et al. A multi-
variate technique for multiply imputing missing values using a
sequence of regression models. Survey Methodol. 2001;27:85-95.
33. Siefert K, Finlayson TL, Williams DR, et al. Modiable risk and
protective factors for depressive symptoms in low-income Afri-
can American mothers. Am J Orthopsychiatry. 2007;77:113-123.
34. Gennetian LA, Miller C. Children and welfare reform: a view
from an experimental welfare program in Minnesota. Child Dev.
2002;73:601-620.
35. Dearing E, McCartney K, Taylor BA. Change in family income-
to-needs matters more for children with less. Child Dev. 2001;72:
1779-1793.
36. Skalicky A, Meyers AF, Adams WG, et al. Child food insecurity
and iron deciency anemia in low-income infants and toddlers in
the United States. Matern Child Health J. 2006;10:177-185.
37. Chilton M, Chyatte M, Breauz J. The negative effects of poverty
and food insecurity on child development. Indian J Med Res.
2007;126:262-272.
38. Richters JE. Depressed mothers as informants about their chil-
dren: a critical review of the evidence for distortion. Psychol Bull.
1992;112:485-499.
39. Rose D, Habicht JP, Devaney B. Household participation in the
Food Stamp and WIC programs increases the nutrient intakes of
preschool children. J Nutr. 1998;128:548-555.
SLOPEN et al.
JOURNAL OF THE AMERICAN ACADEMY OF CHILD & ADOLESCENT PSYCHIATRY
VOLUME 49 NUMBER 5 MAY 2010 452 www.jaacap.org
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 2022 WR Extended VersionDocument71 pages2022 WR Extended Versionpavankawade63Pas encore d'évaluation
- Configuring BGP On Cisco Routers Lab Guide 3.2Document106 pagesConfiguring BGP On Cisco Routers Lab Guide 3.2skuzurov67% (3)
- PC Model Answer Paper Winter 2016Document27 pagesPC Model Answer Paper Winter 2016Deepak VermaPas encore d'évaluation
- Injections Quiz 2Document6 pagesInjections Quiz 2Allysa MacalinoPas encore d'évaluation
- YIC Chapter 1 (2) MKTDocument63 pagesYIC Chapter 1 (2) MKTMebre WelduPas encore d'évaluation
- Siemens Make Motor Manual PDFDocument10 pagesSiemens Make Motor Manual PDFArindam SamantaPas encore d'évaluation
- Core ValuesDocument1 pageCore ValuesIan Abel AntiverosPas encore d'évaluation
- Skills Checklist - Gastrostomy Tube FeedingDocument2 pagesSkills Checklist - Gastrostomy Tube Feedingpunam todkar100% (1)
- Determination Rules SAP SDDocument2 pagesDetermination Rules SAP SDkssumanthPas encore d'évaluation
- Notes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0MDocument1 pageNotes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0Mسجى وليدPas encore d'évaluation
- Fds-Ofite Edta 0,1MDocument7 pagesFds-Ofite Edta 0,1MVeinte Años Sin VosPas encore d'évaluation
- MMS - IMCOST (RANJAN) Managing Early Growth of Business and New Venture ExpansionDocument13 pagesMMS - IMCOST (RANJAN) Managing Early Growth of Business and New Venture ExpansionDhananjay Parshuram SawantPas encore d'évaluation
- B I o G R A P H yDocument17 pagesB I o G R A P H yRizqia FitriPas encore d'évaluation
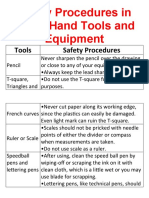
- Safety Procedures in Using Hand Tools and EquipmentDocument12 pagesSafety Procedures in Using Hand Tools and EquipmentJan IcejimenezPas encore d'évaluation
- PDFDocument10 pagesPDFerbariumPas encore d'évaluation
- Chapter 13 (Automatic Transmission)Document26 pagesChapter 13 (Automatic Transmission)ZIBA KHADIBIPas encore d'évaluation
- Shakespeare Sonnet EssayDocument3 pagesShakespeare Sonnet Essayapi-5058594660% (1)
- Disassembly Procedures: 1 DELL U2422HB - U2422HXBDocument6 pagesDisassembly Procedures: 1 DELL U2422HB - U2422HXBIonela CristinaPas encore d'évaluation
- Sample Monologues PDFDocument5 pagesSample Monologues PDFChristina Cannilla100% (1)
- Amount of Casien in Diff Samples of Milk (U)Document15 pagesAmount of Casien in Diff Samples of Milk (U)VijayPas encore d'évaluation
- What's New in CAESAR II: Piping and Equipment CodesDocument1 pageWhat's New in CAESAR II: Piping and Equipment CodeslnacerPas encore d'évaluation
- Health Post - Exploring The Intersection of Work and Well-Being - A Guide To Occupational Health PsychologyDocument3 pagesHealth Post - Exploring The Intersection of Work and Well-Being - A Guide To Occupational Health PsychologyihealthmailboxPas encore d'évaluation
- Apron CapacityDocument10 pagesApron CapacityMuchammad Ulil AidiPas encore d'évaluation
- Congenital Cardiac Disease: A Guide To Evaluation, Treatment and Anesthetic ManagementDocument87 pagesCongenital Cardiac Disease: A Guide To Evaluation, Treatment and Anesthetic ManagementJZPas encore d'évaluation
- Toeic: Check Your English Vocabulary ForDocument41 pagesToeic: Check Your English Vocabulary ForEva Ibáñez RamosPas encore d'évaluation
- CHAPTER 1 SBL NotesDocument13 pagesCHAPTER 1 SBL NotesPrieiya WilliamPas encore d'évaluation
- Recitation Math 001 - Term 221 (26166)Document36 pagesRecitation Math 001 - Term 221 (26166)Ma NaPas encore d'évaluation
- Micro EvolutionDocument9 pagesMicro EvolutionBryan TanPas encore d'évaluation
- Radon-222 Exhalation From Danish Building Material PDFDocument63 pagesRadon-222 Exhalation From Danish Building Material PDFdanpalaciosPas encore d'évaluation
- Government College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniqueDocument11 pagesGovernment College of Nursing Jodhpur: Practice Teaching On-Probability Sampling TechniquepriyankaPas encore d'évaluation