Académique Documents
Professionnel Documents
Culture Documents
Generic Medical Care Plan
Transféré par
Jamie SimsCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Generic Medical Care Plan
Transféré par
Jamie SimsDroits d'auteur :
Formats disponibles
Generic Medical Care Plan for the Hospitalized
Adult Client
This care plan (Level I) presents nursing diagnoses and collaborative problems that commonly
apply to clients (and their significant others) undergoing hospitalization for any medical disorder.
Nursing diagnoses and collaborative problems specific to a disorder are presented in the care
plan (Level II) for that disorder.
DIAGNOSTIC CLUST!
Colla"orati#e Pro"le$s
PC Cardiovascular !ysfunction
PC "espiratory Insufficiency
Nursin% Dia%noses
#n$iety related to unfamiliar environment% routines% diagnostic tests% treatments% and loss of
control
"is& for In'ury related to unfamiliar environment and physical and mental limitations secondary
to condition% medications% therapies% and diagnostic tests
"is& for Infection related to increased microorganisms in environment% ris& of person(to(person
transmission% and invasive tests and therapies
()pecify) )elf(Care !eficit related to sensory% cognitive% mobility% endurance% or motivation
problems
"is& for Imbalanced Nutrition Less Than *ody "e+uirements related to decreased appetite
secondary to treatments% fatigue% environment% and changes in usual diet% and to increased
protein and vitamin re+uirements for healing
"is& for Constipation related to change in fluid and food inta&e% routine% and activity level,
effects of medications, and emotional stress
"is& for Impaired )&in Integrity related to prolonged pressure on tissues associated -ith
decreased mobility% increased fragility of the s&in associated -ith dependent edema%
decreased tissue perfusion% malnutrition% and urinary.fecal incontinence
!isturbed )leep Pattern related to unfamiliar% noisy environment% change in bedtime ritual%
emotional stress% and change in circadian rhythm
"is& for )piritual !istress related to separation from religious support system% lac& of privacy% or
inability to practice spiritual rituals
Interrupted /amily Processes related to disruption of routines% change in role responsibilities% and
fatigue associated -ith increased -or&load and visiting hour re+uirements
"is& for Compromised 0uman !ignity related to multiple factors (intrusions% unfamiliar
procedures and personnel% loss of privacy) associated -ith hospitalization
"is& for Ineffective Therapeutic "egimen 1anagement related to comple$ity and cost of
therapeutic regimen% comple$ity of health care system% shortened length of stay%
insufficient &no-ledge of treatment% and barriers to comprehension secondary to
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3
language barriers% cognitive deficits% hearing and.or visual impairment% an$iety and lac&
of motivation
Dischar%e Criteria
)pecific discharge criteria vary depending on the client<s condition. =enerally% all diagnoses in
the above diagnostic cluster should be resolved before discharge.
Colla"orati#e Pro"le$s
PC& Cardio#ascular D'sfunction
PC& !espirator' Insufficienc'
Nursin% Goal
The nurse -ill detect early signs and symptoms of (a) cardiovascular dysfunction% and (b)
respiratory insufficiency% and -ill intervene collaboratively to stabilize the client.
Indicators
> Calm% alert% oriented (a% b)
> "espiration ?@A34 breaths.min% rela$ed and rhythmic (b)
> *reath sounds present all lobes% no rales or -heezing (b)
> Pulse @4A?44 beats.min (a% b)
> *P B54.@4% C?D4.54 mm0g (a% b)
> Capillary refill CE seconds, s&in -arm and dry (a% b)
> Peripheral pulses full% e+ual (a)
> Temperature 5F.;A55G/ (a% b)
Inter#entions !ationales
?. 1onitor cardiovascular status ?. Physiologic mechanisms governing
cardiovascular function are very
sensitive to any change in body
function% ma&ing changes in
cardiovascular status important clinical
indicators.
a. "adial pulse (rate and rhythm) a. Pulse monitoring provides data
to detect cardiac dysrhythmia%
blood volume changes% and
circulatory impairment.
b. #pical pulse (rate and rhythm) b. #pical pulse monitoring is
indicated if the client<s
peripheral pulses are irregular%
-ea&% or e$tremely rapid.
c. *lood pressure c. *lood pressure represents the
force that the blood e$erts
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
E
against the arterial -alls.
0ypertension (systolic pressure
B?D4 mm0g% diastolic pressure
BF; mm0g) may indicate
increased peripheral resistance%
cardiac output% blood volume% or
blood viscosity. 0ypotension
can result from significant blood
or fluid loss% decreased cardiac
output% and certain medications.
d. )&in (color% temperature%
moisture) and temperature
d. )&in assessment provides
information evaluating
circulation% body temperature%
and hydration status.
e. Pulse o$imetry e. Pulse o$imetry is a noninvasive
method (probe sensor on
fingertip) for continuous
monitoring of o$ygen saturation
of hemoglobin.
3. 1onitor respiratory status
a. "ate
b. "hythm
c. *reath sounds
3. "espiratory assessment provides
essential data for evaluating the
effectiveness of breathing and detecting
adventitious or abnormal sounds% -hich
may indicate air-ay moisture%
narro-ing% or obstruction.
!elated Ph'sician(Prescri"ed Inter#entions
!ependent on the underlying pathology
Docu$entation
/lo- records
Pulse rate and rhythm
*lood pressure
"espiratory assessment
Progress notes
#bnormal findings
Interventions
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
D
Nursin% Dia%noses
An)iet' !elated to Unfa$iliar n#iron$ent* !outines* Dia%nostic Tests*
Treat$ents* and Loss of Control
NOC #n$iety Control% Coping% Impulse Control
Goal
The client -ill communicate feelings regarding the condition and hospitalization.
Indicators
> Herbalize% if as&ed% -hat to e$pect regarding routines and procedures.
> I$plain restrictions.
NIC #n$iety "eduction% Impulse Control Training% #nticipatory =uidance
Inter#entions !ationales
?. Introduce yourself and other members
of the health care team% and orient the
client to the room (e.g.% bed controls%
call bell% bathroom).
?. # smooth% professional admission
process and -arm introduction can put
a client at ease and set a positive tone
for his or her hospital stay.
3. I$plain hospital policies and routines
a. Hisiting hours
b. 1ealtimes and availability of
snac&s
3% E. Providing accurate information can
help decrease the client<s an$iety
associated -ith the un&no-n and
unfamiliar.
c. Hital(sign monitoring
d. #vailability of ne-spapers
e. Television rental and operation
f. )torage of valuables
g. Telephone use
h. )mo&ing policy
i. Policy for off(unit trips
E. !etermine the client<s &no-ledge of his
or her condition% its prognosis% and
treatment measures. "einforce and
supplement the physician<s
e$planations as necessary.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
;
D. I$plain any scheduled diagnostic tests%
covering the follo-ing
a. !escription
b. Purpose
c. Pretest routines
DA@. Teaching the client about tests and
treatment measures can help decrease
his or her fear and an$iety associated
-ith the un&no-n% and improve his or
her sense of control over the situation.
d. 6ho -ill perform the procedure
and -here
e. I$pected sensations
f. Posttest routines
g. #vailability of results
;. !iscuss all prescribed medications
a. Name and type
b. Purpose
c. !osage
d. )pecial precautions
e. )ide effects
@. I$plain any prescribed diet
a. Purpose
b. !uration
c. #llo-ed and prohibited foods
J. Provide the client -ith opportunities to
ma&e decisions about his or her care
-henever possible.
J. Participating in decision(ma&ing can
help give a client a sense of control%
-hich enhances his or her coping
ability. Perception of loss of control can
result in a sense of po-erlessness% then
hopelessness.
F. Provide reassurance and comfort.
)pend time -ith the client% encourage
him or her to share feelings and
concerns% listen attentively% and convey
empathy and understanding.
F. Providing emotional support and
encouraging sharing may help a client
clarify and verbalize his or her fears%
allo-ing the nurse to get realistic
feedbac& and reassurance.
5. Correct any misconceptions and
inaccurate information the client may
e$press.
5. # common contributing factor to fear
and an$iety is incomplete or inaccurate
information, providing ade+uate%
accurate information can help allay
client fears.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
@
?4. #llo- the client<s support people to
share their fears and concerns% and
encourage them in providing
meaningful and productive support.
?4. )upporting the client<s support people
can enhance their ability to help the
client.
Docu$entation
Progress notes
Knusual responses or situations
1ultidisciplinary client education record
Client<s &no-ledge.information provided related to diagnosis% treatment% and hospital
routine
!is+ for In,ur' !elated to Unfa$iliar n#iron$ent and Ph'sical or Mental
Li$itations Secondar' to the Condition* Medications* Therapies* and Dia%nostic
Tests
NOC "is& Control% )afety )tatus /alls Lccurrence
Goal
The client -ill not in'ure him( or herself during hospital stay.
Indicators
> Identify factors that increase ris& of in'ury.
> !escribe appropriate safety measures.
NIC /all Prevention% Invironmental 1anagement )afety% 0ealth Iducation%
)urveillance )afety% "is& Identification
Inter#entions !ationales
?. Lrient the client to his or her
environment (e.g.% location of
bathroom% bed controls% call bell).
Leave a light on in the bathroom at
night.
?. Lrientation helps provide familiarity, a
light at night helps the client find his or
her -ay safely.
3. Instruct the client to -ear slippers -ith
nons&id soles and to avoid ne-ly
-ashed floors.
3. These precautions can help prevent foot
in'uries and falls from slipping.
E. Teach him or her to &eep the bed in the
lo- position -ith side rails up at night.
E. The lo- position ma&es it easier for the
client to get in and out of bed.
D. 1a&e sure that the telephone%
eyeglasses% and fre+uently used
D. 7eeping ob'ects at hand helps prevent
falls from overreaching and
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
J
personal belongings are -ithin easy
reach.
overe$tending.
;. Instruct the client to re+uest assistance
-henever needed.
;. =etting needed help -ith ambulation
and other activities reduces a client<s
ris& of in'ury.
@. I$plain the hospital<s smo&ing policy. @. The hospital is a nonsmo&ing
institution.
J. /or an uncooperative% high(ris& client%
consult -ith the physician for a 3D(hour
sitter or restraints% as indicated.
J. In some cases% e$tra measures are
necessary to ensure a client<s safety and
prevent in'ury to him or her and others.
Docu$entation
Progress notes
1ultidisciplinary client education record
Client teaching
"esponse to teaching
!is+ for Infection !elated to Increased Microor%anis$s in the n#iron$ent* !is+ of
Person(to(Person Trans$ission* and In#asi#e Tests or Therapies
NOC Infection )tatus% 6ound 0ealing Primary Intention% Immune )tatus
Goal
The client -ill describe or demonstrate appropriate precautions to prevent infection.
NIC Infection Control% 6ound Care% Incision )ite Care% 0ealth Iducation
Inter#entions !ationales
?. Teach the client to -ash his or her
hands regularly% especially before meals
and after toileting.
?. Proper hand -ashing deters the spread
of microorganisms.
3. Teach the client to avoid coughing%
sneezing% or breathing on others% and to
use disposable tissues.
3. These techni+ues help prevent
transmission of infection through
airborne droplets.
E. /ollo- institutional policies for IH and
ind-elling urinary catheter insertion
and care.
E. Proper insertion and care reduce the
ris& of inflammation and infection.
D. Teach a client undergoing IH therapy
not to bump or disturb the IH
catheterization site.
D. 1ovement of the device can cause
tissue trauma and possible
inflammation.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
F
;. Teach a client -ith an ind-elling
catheter in place to do the follo-ing
a. #void pressure on the catheter.
b. 6ipe from front to bac& after a
bo-el movement.
;. Catheter movement can cause tissue
trauma% predisposing to inflammation.
/eces can readily contaminate an
ind-elling catheter.
@. Instruct the client to -atch for and
report immediately any signs and
symptoms of inflammation
a. "edness or pain at the catheter
insertion site
@. Nosocomial infections occur in ;A@M
of all hospitalized clients. Iarly
detection enables prompt intervention
to prevent serious complications and a
prolonged hospital stay.
b. *ladder spasms and cloudy
urine (for a client -ith an
ind-elling urinary catheter)
c. /eelings of -armth and malaise
Docu$entation
/lo- records
Catheter and insertion site care
Progress notes
#bnormal findings
1ultidisciplinary client education record
-Specif'. Self(Care Deficit !elated to Sensor'* Co%niti#e* Mo"ilit'* ndurance* or
Moti#ational Pro"le$s
NOC )ee )elf(Care *athing% )elf(Care 0ygiene% )elf(Care Iating% )elf(Care
!ressing% )elf(Care Toileting% and.or )elf(Care Instrumental #ctivities of !aily Living
for NLC
Goal
The client -ill perform self(care activities (feeding% toileting% dressing% grooming% bathing)% -ith
assistance as needed.
Indicators
> !emonstrate optimal hygiene after care is provided.
> !escribe restrictions or precautions needed.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
5
NIC )ee /eeding% *athing% !ressing% and.or Instrumental )elf(Care !eficit for NIC
Inter#entions !ationales
?. Promote the client<s ma$imum
involvement in self(feeding
a. !etermine the client<s favorite
foods and provide them% -hen
possible.
?AD. Inhancing a client<s self(care abilities
can increase his or her sense of
control and independence% promoting
overall -ell(being.
b. #s feasible% arrange for meals to
be served in a pleasant% rela$ed%
and familiar setting -ithout too
many distractions.
c. Insure good oral hygiene before
and after meals.
d. Incourage the client to -ear his
or her dentures and eyeglasses
-hen eating% as appropriate.
e. 0ave the client sit upright in a
chair at a table% if possible. If not%
position him or her as close to
upright as he or she can be.
f. Provide some social contact
during meals.
g. Incourage a client -ho has
trouble handling utensils to eat
Nfinger foodsO (e.g.% bread%
sand-iches% fruit% nuts).
h. Provide needed adaptive devices
for eating% such as a plate guard%
suction device under the plate or
bo-l% padded(handle utensils%
-rist or hand splints -ith clamp%
and special drin&ing cup.
i. #ssist -ith meal setup as needed
Popen containers% nap&ins and
condiment pac&ages% cut meat%
and butter bread.
'. #rrange foods so the client can
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?4
eat them easily.
3. Promote the client<s ma$imum
involvement in bathing.
a. Incourage and help set up a
regular bathing schedule.
b. 7eep the bathroom and bath -ater
-arm.
c. Insure privacy.
d. Provide needed adaptive
e+uipment% such as bath board%
tub chair or stool% -ashing mitts%
and hand(held sho-er spray.
e. 1a&e sure the call bell is -ithin
easy reach of a client -ho is
bathing alone.
E. Promote or provide assistance -ith
grooming and dressing
a. !eodorant application
b. Cosmetic application
c. 0air care shampooing and styling
d. )having and beard care
e. Nail and foot care
D. Promote the client<s ma$imum
involvement in toileting activities.
a. Ivaluate his or her ability to
move to and use the toilet
unassisted.
b. Provide assistance and
supervision only as needed.
c. Provide needed adaptive devices
(e.g.% commode chair% spill(proof
urinal% fracture bedpan% raised
toilet seat% support rails).
d. 6henever possible% encourage a
regular elimination routine using
the toilet and avoiding a bedpan
or urinal.
Docu$entation
/lo- records
#ssistance needed for self(care
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
??
!is+ for I$"alanced Nutrition& Less Than /od' !e0uire$ents !elated to Decreased
Appetite Secondar' to Treat$ents* 1ati%ue* n#iron$ent* and Chan%es in Usual
Diet* and to Increased Protein and 2ita$in !e0uire$ents for Healin%
NOC Nutritional )tatus% Teaching Nutrition
Goal
The client -ill ingest daily nutritional re+uirements in accordance -ith activity level% metabolic
needs% and restrictions.
Indicators
> "elate the importance of good nutrition.
> "elate restrictions% if any.
NIC Nutrition 1anagement% Nutritional 1onitoring
Inter#entions !ationales
?. I$plain the need for ade+uate
consumption of carbohydrates% fats%
protein% vitamins% minerals% and fluids.
?. !uring illness% good nutrition can
reduce the ris& of complications and
speed up recovery.
3. Consult -ith a nutritionist to establish
appropriate daily caloric and food type
re+uirements for the client.
3. Consultation can help ensure a diet that
provides optimal caloric and nutrient
inta&e.
E. !iscuss -ith the client possible causes
of his or her decreased appetite.
E. /actors such as pain% fatigue% analgesic
use% and immobility can contribute to
anore$ia. Identifying a possible cause
enables interventions to eliminate or
minimize it.
D. Incourage the client to rest before
meals.
D. /atigue further reduces an anore$ic
client<s desire and ability to eat.
;. Lffer fre+uent small meals instead of a
fe- large ones.
;. Iven distribution of total daily caloric
inta&e throughout the day helps prevent
gastric distention% possibly increasing
appetite.
@. "estrict li+uids -ith meals and avoid
fluids one hour before and after meals.
@. These fluid restrictions help prevent
gastric distention.
J. Incourage and help the client to
maintain good oral hygiene.
J. Poor oral hygiene leads to bad odor and
taste% -hich can diminish appetite.
F. #rrange to have high(calorie and high(
protein foods served at the times that
F. This measure increases the li&elihood
of the client<s consuming ade+uate
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?3
the client usually feels most li&e eating. calories and protein.
5. Ta&e steps to promote appetite
a. !etermine the client<s food
preferences and arrange to have
those foods provided% as
appropriate.
5. These measures can improve appetite
and lead to increased inta&e.
b. Iliminate any offensive odors
and sights from the eating area.
c. Control any pain or nausea
before meals.
d. Incourage the client<s family
and.or support persons to bring
allo-ed foods from home% if
possible.
e. Provide a rela$ed atmosphere
and some socialization during
meals.
?4. =ive the client printed materials
outlining a nutritious diet that includes
the follo-ing
a. 0igh inta&e of comple$
carbohydrates and fiber
?4. Today% diet planning focuses on
avoiding nutritional e$cesses. "educing
fats% salt% and sugar can reduce the ris&
of heart disease% diabetes% certain
cancers% and hypertension.
b. !ecreased inta&e of sugar%
simple carbohydrates% salt%
cholesterol% total fat% and
saturated fats
c. 1oderate use of alcohol
d. Proper caloric inta&e to
maintain ideal -eight
e. #ppro$imately ?4 cups of -ater
daily% unless contraindicated
Docu$entation
/lo- records
!ietary inta&e
!aily -eight
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?E
1ultidisciplinary client education record
!iet instruction
Kse of assistive devices
!is+ for Constipation !elated to Chan%e in 1luid or 1ood Inta+e* !outine* or
Acti#it' Le#el3 ffects of Medications3 and $otional Stress
NOC *o-el Ilimination% 0ydration% )ymptom Control
Goal
The client -ill maintain pre(hospitalization bo-el patterns.
Indicators
> )tate the importance of fluids% fiber% and activity.
> "eport difficulty promptly.
NIC *o-el 1anagement% /luid management% Constipation.Impaction 1anagement
Inter#entions !ationales
?. #uscultate bo-el sounds. ?. *o-el sounds indicate the nature of
peristaltic activity.
3. Implement measures to eat a balanced
diet that promotes regular elimination
a. Incourage increased inta&e of
high(fiber foods% such as fresh
fruit -ith s&in% bran% nuts and
seeds% -hole(grain breads and
cereals% coo&ed fruits and
vegetables% and fruit 'uices.
(Note If the client<s diet is lo-
in fiber% introduce fiber slo-ly
to reduce irritation to the
bo-el.)
3. # -ell(balanced high(fiber diet
stimulates peristalsis and regular
elimination.
b. !iscuss the client<s dietary
preferences and plan diet
modifications to accommodate
them% -henever possible.
c. Incourage the client to eat
appro$imately F44 grams of
fruits and vegetablesPthe
e+uivalent of about four pieces
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?D
of fresh fruit and a large saladP
daily to promote regular bo-el
movements.
E. Promote ade+uate daily fluid inta&e
a. Incourage inta&e of at least 3
liters (F to ?4 glasses) per day%
unless contraindicated.
E. #de+uate fluid inta&e helps maintain
proper stool consistency in the bo-el
and aids regular elimination.
b. Identify and accommodate fluid
preferences% -henever possible.
c. )et up a schedule for regular
fluid inta&e.
D. Istablish a regular routine for
elimination
a. Identify the client<s usual
elimination pattern before the
onset of constipation.
D. !evising an elimination routine based
on the body<s natural circadian rhythms
can help stimulate regular defecation.
b. "evie- the client<s daily routine
to find an optimal time for
elimination% and schedule
ade+uate time.
c. )uggest that the client attempt
defecation about one hour
follo-ing meals, instruct him or
her to remain on the toilet for a
sufficient length of time.
;. #ttempt to simulate the client<s home
environment for elimination
a. 0ave the client use the toilet
rather than a bedpan or
commode% if possible. Lffer a
bedpan or commode only -hen
necessary.
;. # sense of normalcy and familiarity can
help reduce embarrassment and
promote rela$ation% -hich may aid
defecation.
b. #ssist the client into proper
position on the toilet% bedpan% or
commode% as necessary.
c. Provide privacy during
elimination attemptsPclose the
bathroom door or dra- curtains
around the bed% play the
television or radio to mas&
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?;
sounds% use a room deodorizer.
d. Provide ade+uate comfort%
reading material as a diversion%
and a call bell for safety
reasons.
@. Teach the client to assume an optimal
position on the toilet or commode
(sitting upright% leaning for-ard
slightly) or bedpan (head of bed
elevated to put the client in high
/o-ler<s position or at permitted
elevation), assist him or her in
assuming this position as necessary.
@. Proper positioning ta&es full advantage
of abdominal muscle action and the
force of gravity to promote defecation.
J. I$plain ho- physical activity affects
daily elimination. Incourage and% as
necessary% assist -ith regular
ambulation% unless contraindicated.
J. "egular physical activity aids
elimination by improving abdominal
muscle tone and stimulating appetite
and peristalsis.
Docu$entation
/lo- records
*o-el movements
*o-el sounds
1ultidisciplinary client education record
Instructions for obtaining regular elimination pattern
!is+ for I$paired S+in Inte%rit' !elated to Prolon%ed Pressure on Tissues
Associated 4ith Decreased Mo"ilit'* Increased 1ra%ilit' of the S+in Associated 4ith
Dependent de$a* Decreased Tissue Perfusion* Malnutrition* Urinar'51ecal
Incontinence
NOC Tissue Integrity )&in and 1ucous 1embranes
Goal
The client -ill maintain present intact s&in.tissue.
Indicators
> No redness (erythema)
> "elate ris& factors to s&in.tissue trauma.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?@
NIC Pressure 1anagement% Pressure Klcer Care% )&in )urveillance% Positioning
Inter#entions !ationales
?. )&in assessment
a. Assessment. #ll clients -ill be
assessed upon admission for
ris& factors that predispose to
s&in brea&do-n. These ris&
factors include% but are not
limited to% the follo-ing
?. To prevent pressure ulcers% individuals
at ris& must be identified so that ris&
factors can be reduced through
intervention.
> #ltered level of
consciousness
> Poor nutrition.hydration
> Impaired mobility
> Impaired sensation
(paralysis)
> Incontinence
> 1ultisystem failure
> )teroid or
immunosuppressive
therapy
> #ge over @;
b. Inspection. Kpon admission%
bony prominences and s&in
folds -ill be inspected for
evidence of redness or s&in
brea&do-n.
c. Documentation. 6ithin F hours
of admission% document the
follo-ing information on the
s&in section of the Nursing
#dmission 0istory
> Indicate by chec&ing
appropriate bo$es
-hether the client is at
ris& for s&in brea&do-n
and the ris& factors
present.
> !escribe e$isting areas
of brea&do-n and
indicate their location on
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?J
the body.
3. Prevention protocol 3.
a. Pressure relief
> Change client<s position
-hen in bed at least
every t-o hours around
the cloc&. Kse large and
small shifts of -eight.
> The critical time period for
tissue changes due to pressure is
bet-een ? and 3 hours% after
-hich irreversible changes can
occur.
> Post position change
schedule (Nturn cloc&O)
at bedside.
> Ktilize prevention mode
on specialty beds.
> The Nturn cloc&O alerts the nurse
to recommended position
changes and appropriate time
intervals for turning.
> Kse foam -ith cushion
in chair, no donuts.
b. Limit shearing forces.friction
> 7eep the head of the bed
at or belo- E4 degrees
-henever possible.
> #void dragging the
client in bed. Kse lift
sheet or overhead
trapeze.
> Kse elbo- protectors.
"emove to inspect at
every shift.
> #pply transparent film
dressing (Tegaderm)
over bony prominences%
as appropriate.
> The ris& of developing a
pressure ulcer can be
diminished by reducing the
mechanical loading on the
tissue. This can be
accomplished by using pressure(
reducing devices. !onuts are
&no-n to cause venous
congestion and edema. # study
of at(ris& clients found that ring
cushions are more li&ely to
cause pressure ulcers than
prevent them. The donut
relieves pressure in one area but
increases pressure in the
surrounding areas.
> Clinically% shear is e$erted on
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?F
the body -hen the head of the
bed is elevated. In this position%
the s&in and superficial fascia
remain fi$ed against the bed
linens -hile the deep fascia and
s&eleton slide do-n to-ard the
foot of the bed. #s a result of
shear% blood vessels in the sacral
area are li&ely to become
t-isted and distorted and tissue
may become ischemic and
necrotic (Porth% 344;).
> /riction in'uries to the s&in
occur -hen it moves across a
coarse surface such as bed
linens. 1ost friction in'uries can
be avoided by using appropriate
techni+ues -hen moving
individuals so that their s&in is
never dragged across the bed
linens.
> Holuntary and involuntary
movements by the individuals
themselves can lead to friction
in'uries% especially on elbo-s
and heels. #ny agent that
eliminates this contact or
decreases the friction bet-een
the s&in and the bed linens -ill
reduce the potential for in'ury.
E. Nutritional assessment
> 1onitor inta&e and consider
consultation -ith physician.
dietary if the client
> Iats less than ;4M of
meals for E or more days
> Is NPL or on a clear
li+uid diet for ; days
> 0as a serum albumin of
CE.;
> Place on inta&e and output. If
E. Nutritional deficit is a &no-n ris&
factor for the development of pressure
ulcers. Poor general nutrition is
fre+uently associated -ith loss of
-eight and muscle atrophy. The
reduction in subcutaneous tissue and
muscle reduces the mechanical padding
bet-een the s&in and the underlying
bony prominences% thus increasing
susceptibility to pressure ulcers. Poor
nutrition also leads to decreased
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
?5
inta&e is less than 3444 mL.3D
hours% force fluids unless
contraindicated.
resistance to infection and interferes
-ith -ound healing.
> "ecord actual -eight on
admission and -ee&ly
thereafter.
> "e+uest multivitamin.mineral
supplement and.or dietary
supplements (*urnsha&es%
Insure) if indicated.
> #ssess lab values
> C*C
> #lbumin
> 0emoglobin.hematocrit
D. )&in care
> Inspect s&in at least daily during
bath for reddened areas or
brea&do-n. Chec& bony
prominences for redness -ith
each position change.
> 7eep s&in clean and dry. =ently
apply moisturizers such as
Iucerin% Lubriderm% or )-een
Cream% as needed.
> #void massage over bony
prominences.
D. )&in inspection is fundamental to any
plan for preventing pressure ulcers.
)&in inspection provides the
information essential for designing
interventions to reduce ris& and for
evaluating the outcomes of those
interventions.
> /or ma$imum s&in vitality%
metabolic -astes and
environmental contaminants
that accumulate on the s&in
should be removed fre+uently. It
is prudent to treat clinical signs
and symptoms of dry s&in -ith
a topical moisturizer.
> There is research evidence to
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
34
suggest that massage over bony
prominences may be harmful.
;. Incontinence care ;.
> #ssess the cause of
incontinence
0istory of incontinence
Change in medications
#ntibiotic therapy
Client disoriented at night
> Chec& client for incontinence
every ? to 3 hours.
> Ta&e client to bathroom or offer
bedpan every 3 hours -hile
a-a&e and at bedtime
> If diapers are used% chec& every
3 hours and prn for -etness.
> If plastic protectors are used%
place inside lift sheet% never in
direct contact -ith the client<s
s&in.
> 1oist s&in due to incontinence
leads to maceration% -hich can
ma&e the s&in more susceptible
to in'ury. 1oisture from urine or
fecal incontinence also reduces
the resistance of the s&in to
bacteria. *acteria and to$ins in
the stool increase the ris& of
s&in brea&do-n.
> Plastic pads hold moisture ne$t
to the s&in. They are not
absorbent and serve only as
Nbed protectors.O Never use
plastic pads unless they are
covered -ith smooth linen to
absorb moisture.
> Cleanse perineal area after each
incontinent episode% follo-ed
by the application of a moisture
barrier ointment (!esitin%
Haseline% # 9 ! Lintment%
*aza.)
> # moisture barrier is a petrolatum(
based ointment that repels urine and
fecal material and moisturizes the s&in
to assist in healing reddened% irritated
areas resulting from incontinence.
Docu$entation
/lo- record
Turning and repositioning
)&in assessment
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3?
Distur"ed Sleep Pattern !elated to an Unfa$iliar* Nois' n#iron$ent* a Chan%e in
/edti$e !itual* $otional Stress* and a Chan%e in Circadian !h'th$
NOC "est% )leep% 6ell(*eing
Goal
The client -ill report a satisfactory balance of rest and activity.
Indicators
> Complete at least four sleep cycles (?44 min) undisturbed.
> )tate factors that increase or decrease the +uality of sleep.
NIC Inergy 1anagement% )leep Inhancement% Invironmental 1anagement
Inter#entions !ationales
?. !iscuss the reasons for differing
individual sleep re+uirements%
including age% life style% activity level%
and other possible factors.
?. #lthough many believe that a person
needs F hours of sleep each night% no
scientific evidence supports this.
Individual sleep re+uirements vary
greatly. =enerally% a person -ho can
rela$ and rest easily re+uires less sleep
to feel refreshed. 6ith age% total sleep
time usually decreases (especially )tage
IH sleep) and )tage I sleep increases.
3. Institute measures to promote
rela$ation
a. 1aintain a dar&% +uiet
environment.
3. )leep is difficult -ithout rela$ation.
The unfamiliar hospital environment
can hinder rela$ation.
b. #llo- the client to choose
pillo-s% linens% and covers% as
appropriate.
E. )chedule procedures to minimize the
times you need to -a&e the client at
night. If possible% plan for at least t-o(
hour periods of uninterrupted sleep.
E. In order to feel rested% a person usually
must complete an entire sleep cycle (J4
to ?44 min) four or five times a night.
D. I$plain the need to avoid sedative and
hypnotic drugs.
D. These medications begin to lose their
effectiveness after a -ee& of use%
re+uiring increased dosages and leading
to the ris& of dependence.
;. #ssist -ith usual bedtime routines as ;. # familiar bedtime ritual may promote
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
33
necessary% such as personal hygiene%
snac&% or music for rela$ation.
rela$ation and sleep.
@. Teach the client sleep(promoting
measures
@. These practices may help promote
sleep.
a. Iating a high(protein snac&
(such as cheese or mil&) before
bedtime
a. !igested protein produces
tryptophan% -hich has a sedative
effect.
b. #voiding caffeine b. Caffeine stimulates metabolism
and deters rela$ation.
c. #ttempting to sleep only -hen
feeling sleepy
c. /rustration may result if the
client attempts to sleep -hen
not sleepy or rela$ed.
d. Trying to maintain consistent
nightly sleep habits
d. Irregular sleeping patterns can
disrupt normal circadian
rhythms% possibly leading to
sleep difficulties.
J. I$plain the importance of regular
e$ercise in promoting good sleep.
J. "egular e$ercise not only increases
endurance and enhances the ability to
tolerate psychological stress% but also
promotes rela$ation.
Docu$entation
Progress notes
"eports of unsatisfactory sleep
!is+ for Spiritual Distress !elated to Separation fro$ !eli%ious Support S'ste$*
Lac+ of Pri#ac'* or Ina"ilit' to Practice Spiritual !ituals
NOC 0ope% )piritual 6ell(*eing
Goal
The client -ill maintain usual spiritual practices not detrimental to health.
Indicators
> #s& for assistance as needed.
> "elate support from staff as needed.
NIC )piritual =ro-th /acilitation% 0ope Instillation% #ctive Listening% Presence%
Imotional )upport% )piritual )upport
Inter#entions !ationales
?. I$plore -hether the client desires to ?. /or a client -ho places a high value on
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3E
engage in an allo-able religious or
spiritual practice or ritual. If so% provide
opportunities for him or her to do so.
prayer or other spiritual practices% these
practices can provide meaning and
purpose and can be a source of comfort
and strength.
3. I$press your understanding and
acceptance of the importance of the
client<s religious or spiritual beliefs and
practices.
3. Conveying a non'udgmental attitude
may help reduce the client<s uneasiness
about e$pressing his or her belief and
practices.
E. Provide privacy and +uiet for spiritual
rituals% as the client desires and as
practicable.
E. Privacy and +uiet provide an
environment that enables reflection and
contemplation.
D. If you -ish% offer to pray -ith the client
or read from a religious te$t.
D. The nursePeven one -ho does not
subscribe to the same religious beliefs
or values as the clientPcan still help
that client meet his or her spiritual
needs.
;. Lffer to contact a religious leader or
hospital clergy to arrange for a visit.
I$plain available services (e.g.%
hospital chapel% *ible).
;. These measures can help the client
maintain spiritual ties and practice
important rituals.
@. I$plore -hether any usual hospital
practices conflict -ith the client<s
beliefs (e.g.% diet% hygiene% treatments).
If so% try to accommodate the client<s
beliefs to the e$tent that policy and
safety allo-.
@. 1any religions prohibit certain
behaviors, complying -ith restrictions
may be an important part of the client<s
-orship.
Docu$entation
Progress notes
)piritual concerns
Interrupted 1a$il' Processes !elated to Disruption of !outines* Chan%es in !ole
!esponsi"ilities* and 1ati%ue Associated 4ith Increased 6or+load* and 2isitin%
Hour !e0uire$ents
NOC /amily Coping% /amily Normalization% /amily Invironment Internal% Parenting
Goal
The client and family members -ill verbalize feelings regarding the diagnosis and
hospitalization.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3D
Indicators
> Identify signs of family dysfunction.
> Identify appropriate resources to see& -hen needed.
NIC /amily Involvement Promotion% Coping Inhancement% /amily Integrity
Promotion% /amily Therapy% Counseling% "eferral
Inter#entions !ationales
?. #pproach the family and attempt to
create a private and supportive
environment.
?. #pproaching a family communicates a
sense of caring and concern.
3. Provide accurate information using
simple terms.
3. 1oderate or high an$iety impairs the
ability to process information. )imple
e$planations impart useful information
most effectively.
E. I$plore the family members<
perceptions of the situation.
E. Ivaluating family members<
understanding can help identify any
learning needs they may have.
D. #ssess their current emotional response
Pguilt% anger% blame% griefPto the
stresses of hospitalization.
D. # family member<s response to another
member<s illness is influenced by the
e$tent to -hich the illness interferes
-ith his or her goal(directed activity%
the significance of the goal interfered
-ith% and the +uality of the relationship.
;. Lbserve the dynamics of clientAfamily
interaction during visitations. Ivaluate
the follo-ing
a. #pparent desire for visit
b. Iffects of visit
c. Interactions
;. These observations provide information
regarding family roles and
interrelationships and the +uality of
support family members provide for
each other.
d. Physical contact
@. !etermine -hether the family<s current
coping mechanism is effective.
@. Illness of a family member may
necessitate significant role changes%
putting a family at high ris& for
maladaptation.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3;
J. Promote family strengths
a. Involve family members in
caring for the client.
J. These measures may help maintain an
e$isting family structure% allo-ing it to
function as a supportive unit.
b. #c&no-ledge their assistance.
c. Incourage a sense of humor and
perspective.
F. #s appropriate% assist the family in
reorganizing roles at home% resetting
priorities% and reallocating
responsibilities.
F. "eordering priorities may help reduce
stress and maintain family integrity.
5. 6arn family members to be prepared
for signs of depression% an$iety% anger%
and dependency in the client and other
family members.
5. #nticipatory guidance can alert family
members to impending problems%
enabling intervention to prevent the
problems from occurring.
?4. Incourage and help the family to call
on their social net-or& (friends%
relatives% church members) for support.
?4. #de+uate support can eliminate or
minimize family members< feelings that
they must Ngo it alone.O
??. Imphasize the need for family
members to address their o-n physical
and psychological needs. To provide
time for this% suggest measures such as
a. Ta&ing a brea& and having
someone else visit the client for
a change
??. # family member -ho ignores his or
her o-n needs for sleep% rela$ation% or
nutrition and changes his or her usual
health practices for the -orse impairs
his or her o-n effectiveness as a
support person.
b. Calling the unit for a status
report rather than traveling to
the hospital every day
?3. If the family becomes over-helmed%
help them prioritize their duties and
problems and act accordingly.
?3. Prioritizing can help a family under
stress focus on and problem(solve
situations re+uiring immediate
attention.
?E. #t the appropriate time% have family
members list perceived problems and
concerns. Then% develop a plan of
action to address each item.
?E. #ddressing each problem separately
allo-s the family to identify resources
and reduce feelings of being
over-helmed.
?D. Incourage the family to continue their
usual method of decision(ma&ing%
including the client -hen appropriate.
?D. :oint decision(ma&ing reduces the
client<s feelings of dependency and
reinforces the availability of continued
support.
?;. #s possible% ad'ust visiting hours to ?;. This measure may help promote regular
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3@
accommodate family schedules. visitation% -hich can help maintain
family integrity.
?@. Identify any dysfunctional coping
mechanisms
a. )ubstance abuse
b. Continued denial
c. I$ploitation of one or more
family members
?@. /amilies -ith a history of unsuccessful
coping may need additional resources.
/amilies -ith unresolved conflicts prior
to a member<s hospitalization are at
high ris&.
d. )eparation or avoidance
e. #ssess for domestic
abuse.violence
> Any person who has
been physically,
emotionally, or sexually
abused by an intimate
partner or former
intimate partner.
> Involves infliction or
threat of infliction of
any bodily inury!
harmful physical
contact! the destruction
of property or threat
thereof as a method of
coercion, control,
revenge, or punishment.
> )ubcategories of
domestic abuse.violence
Physical
)e$ual
0arassment
Intimidation of a
dependent
Interference -ith
personal liberty or
-illful deprivation
> 0igh ris& indicators for
suspected abuse )hould
you notice any of the
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3J
follo-ing indicators in
combination -ith each
other% it may -arrant a
referral to either the
1edical )ocial 6or&
!epartment (clients
admitted to medical
units) or Crisis
Intervention.
"hysical indicators:
> Physician<s e$am reveals that
the client has in'uries the
spouse.intimate partner.client
had not divulged
> Too many Nune$plainedO
in'uries or e$planations
inconsistent -ith in'uries
> Lver time% e$planations for
in'uries become inconsistent
> Prolonged interval bet-een
trauma or illness and
presentation for medical care
> Conflicting or implausible
accounts regarding in'uries or
incidents
> 0istory of 1! shopping or I"
shopping
#ocial indicators:
> #ge
Qoung (chronologically or
developmentally)
Llder
> )pouse.intimate partner is
forced by circumstances to care
for client -ho is un-anted
> )pouse.intimate partner
inappropriately -ill not allo-
you to intervie- the client alone
despite e$planation
> Client.spouse.intimate partner
socially isolated or alienated
> Client.spouse.intimate partner
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
3F
demonstrates poor self(image
> /inancial difficulties
> Client claims to have been
abused
$ehavioral indicators:
> Client.spouse.intimate partner
presents vague e$planation
regarding in'uries -ith
implausible stories
> Client.spouse.intimate partner is
very evasive in providing
e$planations
> Client has difficulty maintaining
eye contact and appears
shameful about in'uries
> Client appears very fearful%
possibly trembling
> Client e$presses ambivalence
regarding relationship -ith
spouse.intimate partner
> Client +uic&ly blames
himself.herself for in'uries
> Client is very passive or
-ithdra-n
> )pouse.intimate partner appears
NoverprotectiveO
> Client appears fearful of
spouse.intimate partner
"efer for counseling if necessary.
?J. !irect the family to community
agencies and other sources of emotional
and financial assistance% as needed.
?J. #dditional resources may be needed to
help -ith management at home.
?F. #s appropriate% e$plore -hether the
client and family have discussed end(
of(life decisions, if not% encourage them
to do so.
?F. Intense stress is e$perienced -hen
families and health care providers are
faced -ith decisions regarding either
initiation or discontinuation of life(
support systems or other medical
interventions that prolong life (e.g.%
nasogastric tube feeding). If the client<s
-ishes are un&no-n% additional
conflicts may arise% especially if the
family disagrees -ith decisions made
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
35
by the health care providers% or vice
versa.
?5. 6hen appropriate% instruct the client or
family members to provide the
follo-ing information
a. Person to contact in the event of
emergency
b. Person -hom the client trusts
-ith personal decisions
c. !ecision -hether to maintain
life support if the client -ere to
become mentally incompetent
d. #ny preference for dying at
home or in the hospital
e. !esire to sign a living -ill
f. !ecision on organ donation
g. /uneral arrangements, burial%
cremation
?5. !uring an episode of acute illness%
these discussions may not be
appropriate. Clients and families should
be encouraged to discuss their
directions to be used to guide future
clinical decisions% and their decisions
should be documented. Lne copy
should be given to the person
designated as the decision(ma&er in the
event the client becomes incapacitated
or incompetent% -ith another copy
retained in a safe deposit bo$ and one
copy on the chart.
Docu$entation
Progress notes
Interactions -ith family
#ssessment of family functioning
Ind(of(life decisions% if &no-n
#dvance directive in chart
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
E4
!is+ for Co$pro$ised Hu$an Di%nit' !elated to Multiple 1actors -Intrusions*
Unfa$iliar n#iron$ent and Personnel* Loss of Pri#ac'. Associated 6ith
Hospitalization
NOC #buse Protection% Comfort Level% 7no-ledge Illness Care% )elf(Isteem%
!ignified !ying% )piritual 6ell(*eing% Information Processing
Goal
The individual -ill report respectful and considerate care.
Indicators
> "espect for privacy
> Consideration of emotions
> #s&ed for permission
> =iven options
> 1inimization of body part e$posure
NIC Patient "ights Protection% #nticipatory =uidance% Counseling% Imotional )upport%
Preparatory )ensory Information% /amily )upport% 0umor% 1utual =oal )etting%
Teaching Procedure.Treatment% Touch
Inter#entions !ationales
?. !etermine if the agency.hospital has a
policy for prevention of compromised
human dignity (Note This type of
policy or standard may be titled
differently Re.g.% 1ission )tatementS).
?. #gency policies can assist the nurse
-hen problematic situations occur.
0o-ever% the moral obligation to
protect and defend the dignity of clients
and their families does not depend on
the e$istence (or lac&) of a policy.
3. "evie- the policy. !oes it include
(6alsh 9 7o-an&o% 3443)
> Protection of privacy and
private space
> #c+uiring the client<s and
family<s permission for planned
care% treatments and procedures
3. This type of policy can pro'ect the
philosophy and culture of moral and
respectful care of the institution among
its personnel.
> Providing ade+uate time for the
client and family to ma&e
decisions regarding the planned
care% treatments and procedures
> #dvocating for the client
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
E?
> Clear guidelines regarding the
number of personnel (e.g.%
students% nurses% physicians
Rresidents% internsS) that can be
present -hen confidential
and.or stressful information is
discussed% or -hen procedures
that leave a client e$posed need
to be done.
E. 1inimize e$posure of the client<s body
-ith the use of drapes. Insure that the
client is not e$posed to the gaze of
others -hose presence is not needed for
the procedure.
E. Individuals have reported being
physically e$posed as their central
source of humiliation and indignity
(6alsh 9 7o-an&o% 3443).
D. Provide care to each client and family
as you -ould e$pect or demand for
your family% partner% child% friend% or
colleague.
D. )etting this personal standard can spur
you to defend the dignity of a
client.family% especially -hen they do
not belong to the same socio(economic
group as you.
;. 6hen performing a procedure% engage
the client in conversation. #ct li&e the
situation is matter(of(fact for you% to
reduce embarrassment. In a-&-ard
situations% tal& to the client even if she
or he is unresponsive. Kse humor if
appropriate.
;. Clients have reported that in
unavoidable% embarrassing situations
(e.g.% bo-el or bladder accident)% a
nurse -ho -as matter(of(fact and -ho
made them feel at ease -ith small tal&
or humor made the situation better
(6alsh 9 7o-an&o% 3443).
@. I$plain the procedure to the client.
!uring painful or embarrassing
procedures% sho- that you understand
and accept ho- the client feels.
@. Clients reported they did not li&e being
rushed and needed time to understand
the upcoming procedure.
J. !etermine if unnecessary personnel are
present before a vulnerable or stressful
event is initiated (e.g.% code as painful
procedure% embarrassing) and advise
them that they are not needed at this
time.
J. Protecting dignity and privacy al-ays
includes unconscious or deceased
clients (1airis% ?55D).
F. #llo- the client an opportunity to share
his or her feelings after a difficult
situation. 1aintain privacy of client<s
information and emotional responses.
F. #llo-ing the client to share their
feelings can help them maintain or
regain dignity. "ecognition of the client
as a living% thin&ing% and e$periencing
human being enhances dignity (6alsh
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
E3
9 7o-an&o% 3443).
5. *e a role model and an advocate for the
preservation of the client<s dignity after
death.
5. "ole(modeling considerate and
respectful care can lead others to a
heightened a-areness and encourage
them to emulate this care themselves.
?4. !iscuss -ith involved personnel any
incident that -as disrespectful to the
client or his or her family and report
repetitive incidents or any incident that
is a violation of client<s dignity to the
appropriate personnel.
?4%??. Professionals have a responsibility to
practice ethical and moral care and to
address situations and personnel that
compromise human dignity.
??. Ingage in dialogue -ith client and
family regarding their thoughts on the
present plan of care and decisions that
may need e$planation.
?3. 6hen e$treme measures are planned or
are being provided for a client -hich
are futile% refer to 1oral !istress.
?3%?E. NI$treme measures% -hen futile% are an
infringement of the basic respect for the
dignity innate in being a personO
(6alsh 9 7o-an&o% 3443 p.?D@).
?E. NPractice e$pecting that honoring and
protecting the dignity of
individual.groups is not a value but a
-ay of being.O ()odenberg et al% ?55F)
Docu$entation
Care plan
)pecify preferences
!is+ for Ineffecti#e Therapeutic !e%i$en Mana%e$ent !elated to Co$ple)it' and
Cost of Therapeutic !e%i$en* Co$ple)it' of Health Care S'ste$* Insufficient
7no4led%e of Treat$ent* and /arriers to Co$prehension Secondar' to Lan%ua%e
/arriers* Co%niti#e Deficits* Hearin% and5or 2isual I$pair$ent* An)iet'* and Lac+
of Moti#ation
NOC Compliance *ehavior% 7no-ledge Treatment "egimen% Participation in 0ealth
Care !ecisions% Treatment *ehavior Illness or In'ury
Goal
The client or primary care giver -ill describe disease process% causes% and factors contributing to
symptoms% and the regimen for disease or symptom control.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
EE
Indicators
> "elate the intent to practice health behaviors needed or desired for recovery from
illness.symptom management and prevention of recurrence or complications.
> !escribe signs and symptoms that need reporting.
NIC #nticipatory =uidance% Learning /acilitation% "is& Identification% 0ealth
Iducation% Teaching Procedure.Treatment% 0ealth )ystem =uidance
Inter#entions !ationales
?. !etermine the client<s &no-ledge of his
or her condition% prognosis% and
treatment measures. "einforce and
supplement the physician<s
e$planations as necessary.
?. #ssessing the client<s level of
&no-ledge -ill assist in the
development of an individualized
learning program. Providing accurate
information can decrease the client<s
an$iety associated -ith the un&no-n
and unfamiliar.
3. Identify factors that influence learning. 3. The client<s ability to learn -ill be
affected by a number of variables that
need to be considered. !enial of illness%
lac& of financial resources% and
depression may affect the client<s
ability and motivation to learn.
Cognitive changes associated -ith this
might influence the client<s ability to
learn ne- information.
E. Provide the client and family -ith
information about ho- to utilize the
health care system (billing and
payment% ma&ing appointments% follo-(
up care% resources available% etc.).
E. Information on ho- to N-or& the
systemO -ill help the client and family
feel more comfortable and more in
control of client<s health care. This -ill
positively influence compliance -ith
the health care regimen.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
ED
D. I$plain and discuss -ith client and
family.caregiver (-hen possible)
a. !isease process
b. Treatment regimen
(medications% diet% procedures%
e$ercises% e+uipment use)
c. "ationale for regimen
d. )ide effects of regimen
e. Lifestyle changes needed
f. /ollo-(up care needed
g. )igns or symptoms of
complications
h. "esources and support available
D. !epending on client<s physical and
cognitive limitations% it may be
necessary to provide the
family.caregiver -ith the necessary
information for managing the treatment
regimen. In order to assist the client
-ith postdischarge care% the client
needs information about the disease
process% treatment regimen% symptoms
of complications% etc.% as -ell as
resources available for assistance.
i. 0ome environment alterations
needed
;. Promote a positive attitude and active
participation of the client and family.
a. )olicit e$pression of feelings%
concerns% and +uestions from
client and family.
b. Incourage client and family to
see& information and ma&e
informed decisions.
;. #ctive participation in the treatment
regimen helps the client and family feel
more in control of the illness% -hich
enhances the effective management of
the therapeutic regimen.
c. I$plain responsibilities of client.family
and ho- these can be assumed.
@. Insure that a client -ith visual and.or
hearing impairments has glasses and a
hearing aid available and uses them
during teaching sessions. Provide
ade+uate lighting and a +uiet place for
teaching sessions. Provide -ritten
teaching materials in the client<s first
language -hen possible.
@. Hision and hearing aids% ade+uate
lighting% -ritten materials in client<s
primary language% etc.% -ill help to
compensate for barriers to learning.
!ecreasing e$ternal stimuli -ill assist
the client to correctly perceive -hat is
being said.
J. I$plain that changes in lifestyle and
needed learning -ill ta&e time to
integrate.
J. I$plaining that changes are e$pected to
ta&e time to integrate -ill provide
reassurance for the client that he or she
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
E;
a. Provide printed material (in
client<s primary language -hen
possible).
b. I$plain -hom to contact -ith
+uestions.
c. Identify referrals or community
services needed for follo-(up.
does not have to ma&e changes all at
once. )upport and reassurance -ill
assist the client -ith compliance.
Providing information about available
resources also helps the client to feel
supported in his or her efforts.
Docu$entation
Progress notes
)pecific discharge needs and plans
!ischarge instructions
"eferrals made
1ultidisciplinary client education record
Client and family teaching about disease% plan of treatment% referrals% etc.
2 3445 6olters 7lu-er 0ealth 8 Lippincott 6illiams 9 6il&ins. /rom Carpenito(1oyet% L. :. Nursing care plans &
documentation: Nursing diagnoses and collaborative problems (;
th
ed.).
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- A Will Eternal - Book 1Document1 295 pagesA Will Eternal - Book 1Hitsuin Movies100% (1)
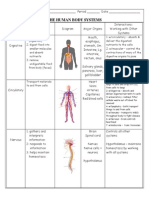
- Human Body Systems Chart With Pictures Answers-Option ADocument3 pagesHuman Body Systems Chart With Pictures Answers-Option AJamie Sims100% (2)
- Human Body Systems Chart With Pictures Answers-Option ADocument3 pagesHuman Body Systems Chart With Pictures Answers-Option AJamie Sims100% (2)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Body Systems Chart KeyDocument2 pagesBody Systems Chart KeyJamie Sims75% (4)
- Concept Care MapDocument3 pagesConcept Care MapJamie SimsPas encore d'évaluation
- Solve, The Mckinsey GameDocument47 pagesSolve, The Mckinsey GamesjPas encore d'évaluation
- Req For NursingDocument2 pagesReq For NursingJamie SimsPas encore d'évaluation
- Kent State University Student Name - College of Nursing N20030 Drug Information Sheet DateDocument1 pageKent State University Student Name - College of Nursing N20030 Drug Information Sheet DateJamie SimsPas encore d'évaluation
- How To Manage A School ChapterDocument8 pagesHow To Manage A School ChapterJamie SimsPas encore d'évaluation
- Membership DetailsDocument1 pageMembership DetailsJamie SimsPas encore d'évaluation
- Req For NursingDocument2 pagesReq For NursingJamie SimsPas encore d'évaluation
- Req For NursingDocument2 pagesReq For NursingJamie SimsPas encore d'évaluation
- Body System Study SheetDocument5 pagesBody System Study SheetJamie SimsPas encore d'évaluation
- Kent State University College of Nursing N20020 Head To Toe Assessment Documentation Guide General SurveyDocument3 pagesKent State University College of Nursing N20020 Head To Toe Assessment Documentation Guide General SurveyJamie SimsPas encore d'évaluation
- Mind MapDocument1 pageMind MapJamie SimsPas encore d'évaluation
- Mind MapDocument1 pageMind MapJamie SimsPas encore d'évaluation
- Math Practice #1 AnswersDocument4 pagesMath Practice #1 AnswersJamie SimsPas encore d'évaluation
- Math Practice #1Document4 pagesMath Practice #1Jamie SimsPas encore d'évaluation
- SSRR X Ssrr. Determine The Expected Progeny Phenotypes and What FractionDocument2 pagesSSRR X Ssrr. Determine The Expected Progeny Phenotypes and What FractionJamie SimsPas encore d'évaluation
- Initiating IV TherapyDocument3 pagesInitiating IV TherapyJamie SimsPas encore d'évaluation
- Auscultating Bowel SoundsDocument1 pageAuscultating Bowel SoundsJamie SimsPas encore d'évaluation
- Drug Template CHPT 30-33Document2 pagesDrug Template CHPT 30-33Jamie SimsPas encore d'évaluation
- Assessing Body Temperature: Goal: Obtain Baseline Temperature Data For Comparing Future CommentsDocument3 pagesAssessing Body Temperature: Goal: Obtain Baseline Temperature Data For Comparing Future CommentsJamie SimsPas encore d'évaluation
- Withdrawing Medication From Am AmpuleDocument1 pageWithdrawing Medication From Am AmpuleJamie SimsPas encore d'évaluation
- Disediakan Oleh: Keetha Naganthiran: Set Induction (Starter) Main ActivitiesDocument1 pageDisediakan Oleh: Keetha Naganthiran: Set Induction (Starter) Main ActivitiesnandyshaPas encore d'évaluation
- Standard Operating Procedures in Drafting July1Document21 pagesStandard Operating Procedures in Drafting July1Edel VilladolidPas encore d'évaluation
- Body Repairs - General Body RepairsDocument49 pagesBody Repairs - General Body RepairsjomialhePas encore d'évaluation
- Diss PDFDocument321 pagesDiss PDFAbdullah GhannamPas encore d'évaluation
- Excuse Letter For MerchandiserDocument7 pagesExcuse Letter For MerchandiserJolly PostadanPas encore d'évaluation
- 21st CENTURY LIT (ILOCOS DEITIES)Document2 pages21st CENTURY LIT (ILOCOS DEITIES)Louise GermainePas encore d'évaluation
- Contoh MOTIVATION LETTERDocument19 pagesContoh MOTIVATION LETTERDavin Tiska AbrianiPas encore d'évaluation
- The BoxDocument6 pagesThe BoxDemian GaylordPas encore d'évaluation
- Npcih IDocument2 pagesNpcih IRoYaL RaJpOoTPas encore d'évaluation
- Airworthiness Directive: Design Approval Holder's Name: Type/Model Designation(s)Document4 pagesAirworthiness Directive: Design Approval Holder's Name: Type/Model Designation(s)Kris Wuthrich BatarioPas encore d'évaluation
- Tata Steel Europe LTDDocument22 pagesTata Steel Europe LTDEntertainment OverloadedPas encore d'évaluation
- IEEE Romania SectionDocument14 pagesIEEE Romania SectionLucian TomaPas encore d'évaluation
- Excuse Letter For Grade 7 ElectionsDocument4 pagesExcuse Letter For Grade 7 ElectionsRaymund ArcosPas encore d'évaluation
- The Lucid Dream Exchange Magazine Issue 36Document36 pagesThe Lucid Dream Exchange Magazine Issue 36api-384230967% (3)
- Natelco Vs CADocument10 pagesNatelco Vs CAcharmdelmoPas encore d'évaluation
- 4.08 Intermediate Category of Taxation and Attorney and Own Client CostsDocument4 pages4.08 Intermediate Category of Taxation and Attorney and Own Client CostsBarbraPas encore d'évaluation
- LP Understanding The Writing ProcessDocument8 pagesLP Understanding The Writing Processargus.dump11Pas encore d'évaluation
- Greetings From Freehold: How Bruce Springsteen's Hometown Shaped His Life and WorkDocument57 pagesGreetings From Freehold: How Bruce Springsteen's Hometown Shaped His Life and WorkDavid WilsonPas encore d'évaluation
- Writing Kafani or AlfiDocument5 pagesWriting Kafani or AlfisahebjuPas encore d'évaluation
- India Is My CountryDocument2 pagesIndia Is My CountryAbi MuthukumarPas encore d'évaluation
- Salt Iodine WYD Iodine Checker Instruction ManualDocument13 pagesSalt Iodine WYD Iodine Checker Instruction ManualCatherine LargaPas encore d'évaluation
- 4-Malayalam InternationalDocument51 pages4-Malayalam InternationalSASHMIRA MENONPas encore d'évaluation
- Technipfmc Corporate Brochure en 2018Document7 pagesTechnipfmc Corporate Brochure en 2018Sivaji RajinikanthPas encore d'évaluation
- HFY-GEN-CP-SPC-0001 - D Specification For Piping and Pipeline Coating Code-ADocument37 pagesHFY-GEN-CP-SPC-0001 - D Specification For Piping and Pipeline Coating Code-ATahir FadhilPas encore d'évaluation
- Batch Fed BatchDocument60 pagesBatch Fed BatchAyesha RalliyaPas encore d'évaluation
- Daftar PustakaDocument2 pagesDaftar PustakaBang UsopPas encore d'évaluation
- 2016 May Virginia Medical Law ReportDocument20 pages2016 May Virginia Medical Law ReportMichael DuntzPas encore d'évaluation
- CAC Policy-FFL - HRD-PM-IMS-011 - Rev05Document13 pagesCAC Policy-FFL - HRD-PM-IMS-011 - Rev05Zaid Bin HishamPas encore d'évaluation