Académique Documents
Professionnel Documents
Culture Documents
Aspek Medikolegal
Transféré par
Erin DestriniTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Aspek Medikolegal
Transféré par
Erin DestriniDroits d'auteur :
Formats disponibles
Medicolegal aspects of reproductive medicine
William L Ledger
Abstract
This paper is a review of current techniques and best practice in reproductive medicine, including
preimplantation genetic diagnosis and embryo freezing, and management of pregnancy after in vitro
fertilization. It discusses medicolegal aspects that can arise from failure to follow best practice
including ovarian hyperstimulation syndrome and mistakes occurring in the embryology laboratory.
Human in vitro fertilization (IVF) is just over 30 years old.
Many will remember the furore surrounding the birth of
Louise Brown after years of effort by Patrick Steptoe and
Bob Edwards, a clinician from Oldham and a scientist from
Cambridge. IVF was the rst truly effective treatment for
many forms of infertility and its use has blossomed over the
past three decades. Variations on the theme, such as intracy-
toplasmic sperm injection (ICSI) for male infertility and
preimplantation genetic diagnosis (PGD) to allow selection
of healthy rather than affected embryos for couples who
carry severe genetic disorders have widened the scope of
IVF and there are now over 3 million IVF children in the
world and over 40,000 IVF treatment cycles performed
annually in UK.
Like all medical advances, the advent of the assisted
reproductive technologies (ART) brought a downside. The
techniques brought a plethora of unforeseen ethical and
legal challenges that continue to vex professionals, the
public and journalists to this day. In response to widespread
anxiety about the potential for abuse of ART and its
impacts on society, the UK Government passed the Human
Fertilisation and Embryology (HF & E) Bill in 1990 which
established the Human Fertilisation and Embryology
Authority and created a legal framework within which
medical practitioners and their colleagues were expected to
practise. Despite setbacks, this system has stood the test of
time and has been widely emulated around the world. The
HF & E Act has now been updated and the revised Act is
due to become law later this year.
Modern treatment of infertility is a complex, time-
consuming, often expensive and frequently fruitless endea-
vour for patients. Even the best IVF clinics will fail to
establish a healthy pregnancy for their clients in over 50% of
cases leaving many with a deep sense of failure, unhappiness
and, in a minority of cases, feeling let down by their doctors
and the system. The NHS has consistently failed to support
infertile patients, leaving many to pay for treatment with
large sums from their own pockets. The new science of
ART has many controversies and disagreements between
professionals as to the best approach to take for different cat-
egories of patient are common. Intricate laboratory science is
inevitably error prone even in the best laboratories, and these
and other pitfalls can provoke dissatised patients to seek
legal redress. Although difcult to quantify, there appear to
be an increasing number of legal cases in this area of medi-
cine, some of which involve allegation of serious harm to
the woman or her child, or even premature death.
This article will discuss a number of IVF-related medi-
colegal issues derived from cases known to the authors. It
will not cover the wider practice of medical or surgical
treatment of infertility, although this is another area fraught
with difculty, and represents the personal opinion of the
author and is not in any way the opinion or policy of the
Human Fertilisation and Embryology Authority.
How does IVF work?
Louise Browns conception followed the collection of a
single human oocyte (egg) during the natural menstrual
cycle of Louise mother. However scientists rapidly learned
that using drugs to stimulate the ovaries to produce multiple
oocytes gave a much better chance of pregnancy. Human
oocytes grow within small uid lled structures within
the ovaries, termed follicles. These will reach a diameter of
about 2 cm before they rupture to release the egg, and can
be both seen on a vaginal ultrasound scan and detected by
their output of oestrogen hormones, particularly oestradiol.
Early work used oral agents such as Clomifene citrate
(Clomid) to stimulate multiple follicle development but
research in the early 1960s led to use of human-derived
gonadotropin hormones, follicle-stimulating hormone
(FSH) and luteinizing hormone (LH) given by injection
for 1014 days to produce anything up to 50 eggs from a
single stimulation cycle.
Modern IVF frequently begins with pituitary desensi-
tization with gonadotropin-releasing hormones (GnRH)
agonist started on day 21 of the menstrual cycle preceding
ovarian stimulation in the so-called long protocol. This
pretreatment, a daily nasal sniff or injection, prevents a
natural LH surge and avoids unwanted early ovulation with
loss of all the eggs before they can be collected. The
woman will use the GnRH agonist for about two weeks Email: w.ledger@shefeld.ac.uk
William L Ledger, Professor of Obstetrics and Gynaecology and Head of
Unit, Academic Unit of Reproductive and Developmental Medicine,
Room 5, Level 4, Jessop Wing, Tree Root Walk, Shefeld S10 2SF, UK
AvMA Medical & Legal Journal 197
DOI: 10.1258/cr.2009.090061 The AvMA Medical & Legal Journal 2009 Volume 15 Number 5
after which she will add a daily injection of FSH hormone.
GnRH agonist treatment produces a pseudo menopause
with hot ushes, mood swings and sleep disturbance that
many nd unpleasant and disruptive of their normal activi-
ties. These symptoms will dissipate when the FSH injection
is started, and are rarely severe enough to lead to discon-
tinuation of treatment.
FSH hormones can now be derived either from
humans isolated from the urine of postmenopausal
women from a bioreactor as a recombinant product of
genetically modied hamster ovary cells. They are given by
daily injection using an autoinjector device and are remark-
ably free of troublesome side-effects. The ovaries respond
to this treatment by growing multiple follicles, each con-
taining an oocyte. Follicle growth is monitored by blood
tests for oestradiol, and vaginal ultrasound to count and
measure the follicles.
Once the follicles are deemed mature, a nal injection
of a second hormone, human chorionic gonadotropin
(hCG) is given. This injection is essential as it induces nal
oocyte maturation and prepares the oocyte to be fertilized.
After hCG the woman will ovulate naturally about 40
hours later so oocyte collection has to be timed to allow
sufcient time for the maturation process to complete but
before ovulation occurs. In practice, injection of hCG is
usually given late at night to allow egg collection in the
morning about 36 hours later.
Eggs are almost universally collected by transvaginal
ultrasound-guided needle aspiration of the ovarian follicles.
This is done under a light general anaesthetic or using seda-
tion, and involves insertion of a needle through the skin at
the top of the vagina and into the ovary. Using ultrasound,
the needle is guided into a follicle which is aspirated using
a gentle suction apparatus. The uid from the follicle is col-
lected and the embryologist isolates the egg from the uid
using a microscope. The egg is placed into culture medium
and incubated in a temperature- and atmosphere-controlled
incubator. Each follicle is aspirated in turn and then the
other ovary is aspirated in a process that takes 1030
minutes and is usually done as a day case.
At the same time, the male partner produces a sperm
sample, either by masturbation or through use of a needle
biopsy of the testis or epididymis for men who are severely
infertile and need ICSI. The embryologist will strip the
oocyte from its surrounding cumulus cells and either
expose the egg to about 50,000 sperm to allow natural
fertilization, or perform ICSI with a single sperm being
injected into each egg. The fertilized egg will then be
incubated for 25 days before replacement into the uterus
using a transfer catheter passed through the cervix into the
uterine cavity. This is no more painful than a cervical
smear, takes a few minutes and is followed by two weeks of
waiting to see if pregnancy will ensue.
Where can it go wrong?
The above 700 words describe a process that many women
and men nd both physically and psychologically taxing.
Things can go wrong at every stage and the HFEA database
(see http://www.hfea.gov.uk) clearly shows the low chances
of a live birth even for best prognosis young patients. In
one sense the most important task for the reproductive
medicine specialist is not to deliver top quality laboratory
and clinical science but to ensure that his/her patients
understand the process, its pitfalls and the likely chance of
success. To begin at the beginning, some men and
women will not be suitable for IVF at all. Some women
have an early menopause, effectively running out of eggs
before the age of 40 years, and IVF science cannot help
them. They may consider treatment with eggs donated by
another person, a difcult decision for many, or adoption,
and will be diagnosed as having early menopause by blood
test and ultrasound scan. Some men have no sperm, or have
sperm that are too immature or damaged to allow for fetal
health. Other couples may be turned down for treatment
because of serious concern for the welfare of the future off-
spring, an often painful decision that may lead to a request
for legal intervention. Many, well over 50%, will be denied
NHS funding for IVF and those who are supported will
frequently only be offered one or two attempts before
being asked to pay themselves. The majority of couples
remain unaware of this until seen in clinic to discuss treat-
ment, and will frequently react angrily to the news that
they will have to part with 3000 to 5000 or more per
attempt. Reasons for exclusion from NHS treatment vary
across the country, being determined locally by Primary
Care Trusts, and the disparity in provision frequently leads
to dissatisfaction.
Ovarian hyperstimulation syndrome
The most serious threat to the health of the woman during
and after IVF treatment is that of ovarian hyperstimulation
syndrome (OHSS). This occurs when the ovaries are over-
stimulated by gonadotropin drugs. Many follicles develop
and oestradiol levels exceed 10 times those ever seen
normally. OHSS is a complex multisystem disorder that
leads to accumulation of uid in the abdomen and chest
along with dehydration of the vascular compartment.
Complications include arterial and venous thrombosis,
respiratory and cardiac failure and stroke. Several recent
well-publicized cases have resulted in permanent handicap
or death of previously healthy young women after severe
OHSS. Clinics can adopt several strategies to reduce risk of
OHSS, although the condition is not completely avoidable
even in expert hands. The dilemma is that strategies to
minimize risk of OHSS may reduce the chances of a live
birth from this expensive and stressful treatment, leading to
pressure from patients that can lead an unwary clinician to
over-stimulate, fail to cancel a cycle or freeze all embryos
when clinically prudent. Recently the concept of mild
stimulation has been introduced into ART practice. This
uses low doses of gonadotropin drugs with a GnRH antag-
onist instead of an agonist. GnRH antagonists act more
directly and hence much more quickly to suppress
hormone levels, and have improved IVF safety and
198 AvMA Medical & Legal Journal
The AvMA Medical & Legal Journal 2009 Volume 15 Number 5
acceptibility over the older generation of agonists. Mild
IVF is quicker and less stressful than conventional treatment,
with a 50% reduction in incidence of OHSS. It is likely
that this will become a more widely used approach in the
future, particularly for women at particular risk of OHSS.
Further details of OHSS and its management can be found
at http://www.rcog.org.uk.
Provided that OHSS is avoided, the process of IVF
carries low risk of physical harm to patients. Gonadotropin
injection can lead to local skin reaction or bruising
although this is mild and self-limiting, and the blood tests
and vaginal scans are undeniably unpleasant but not danger-
ous. Transvaginal egg collection is surprisingly free of fre-
quent complications although the proximity of the ovaries
to the major iliac vessels can rarely lead to signicant haem-
orrhage after collection that may require abdominal surgery.
There are the usual hazards of anaesthesia and some patients
treated under sedation only may nd the process unaccepta-
bly painful.
Equally, production of sperm is usually straightforward
although needle aspiration to obtain sperm may be followed
by extensive bruising, pain and swelling of the scrotum.
Embryology
The major area of potential hazard is in the embryology lab-
oratory. Cases in which the wrong sperm and eggs were
mixed, or in which the wrong embryos were transferred
led to the HFEA requiring that a second person witness all
parts of gamete and embryo handling and labelling. This has
been followed by systems for automatic labelling of speci-
mens using bar coding or radiofrequency tagging which
should minimize such incidents. Embryology is a tightly
regulated profession with a well-run system of training and
qualication which produces reliable and conscientious
practitioners. However a laboratory suffering staff shortage
or poor staff relations may still produce errors, the conse-
quences of which are long-lasting and profound. There are
many other potential problems in embryology, ranging from
unexpected failure of any eggs to fertilize to incubator
infection necessitating disposal of embryos before transfer,
or loss of frozen embryos. While scientically justiable,
patients may see their investment, and more importantly
their chances of a child, disappear when such accidents
happen and poor explanation by the clinic can lead to
complaint.
As IVF science has progressed, the need to transfer
several embryos in a single treatment cycle in order to have
a reasonable chance of a pregnancy has diminished. At the
same time, the hazards of twin and triplet pregnancy have
become clear as the number of multiple births has increased
because of the contribution of ART. The burden of iatro-
genic multiple pregnancy has clear economic consequences
for the NHS, particularly since private clinics do not
provide antenatal, intrapartum or neonatal intensive care
and instead pass these problems back to the State to fund.
More importantly, the chance of long-term handicap to a
child born from a multiple gestation is signicantly raised
compared with that of a singleton and hence HFEA and
the majority of responsible fertility practitioners have
recently promoted the concept of single embryo transfer
(SET). The HFEA website (http://www.oneatatime.org.uk)
clearly describes the rationale for this approach in selected
cases, namely younger women with good prospect of preg-
nancy after IVF. However, as ever in IVF, others disagree
with this opinion and some patients may feel that their
chances of a pregnancy have been diminished by application
of an overly prescriptive single embryo transfer policy.
Equally, those who conceive a multiple pregnancy after
transfer of more than one embryo may later claim to have
been inadequately counselled about the medical and other
risks of multiple gestation. The current system of HFEA
reporting of live-birth rate per cycle started pressurizes
some clinicians into advising multiple embryo transfer in
order to achieve a high position in the annual league
table, creating a potential conict between medical best
practice and commercial success of the clinic.
Embryo freezing
The corollary to widespread use of SET is that more
embryos are available for cryopreservation (freezing).
Embryo freezing technology is well-developed and the
health of children born from cryopreserved embryos
seems equivalent to their naturally conceived counterparts.
However, freezing offers another possibility for disaster
none of the embryos may survive freeze-thawing, embryo
quality after thawing may be signicantly and surprisingly
impaired or the embryos may be transferred in repeated
cycles and pregnancy not result. Recently, the novel tech-
nology of vitrication, ultra-rapid freezing, has been
applied to both embryo and egg freezing. While the
benets of vitrication in embryo freezing are unclear,
there is denite benet when eggs are frozen with this
technique. Conventional slow freezing has not been par-
ticularly successful when applied to eggs they are very
large cells and ice crystals form which later disrupt the deli-
cate architecture of the cell when thawing occurs. In con-
trast, vitrication avoids this problem, and pregnancy rates
when frozen eggs are thawed and fertilized with ICSI are
relatively high. The use of relative in this context is
important. Vitrication is a new process and still has to
establish its place in routine practice. Its benets are
obvious when used to freeze the oocytes of young women
who are about to undergo sterilizing treatment for cancer
after cure they have at least a chance of having children later
in life. The benets are less clear, at least to this author,
when this technology is offered to healthy young women
who wish to defer their childbearing until after the natural
reproductive lifespan has passed. This may offer false hope
the customer may return years later to use her frozen eggs
but fail to conceive, only to nd that natural pregnancy is
no longer possible and that she and her partner will not be
able to have their family. The consequences if careful, well-
documented counselling about this risk has not been
carried out are obvious.
AvMA Medical & Legal Journal 199
The AvMA Medical & Legal Journal 2009 Volume 15 Number 5
Pregnancy after IVF
IVF pregnancies are high-risk pregnancies. Women preg-
nant after IVF are often older than average and may have
co-existant medical disorders that contribute to their infer-
tility. The care of these patients provided by the IVF clinic
should not cease on the day of a positive pregnancy test.
The possibility of miscarriage or, more medically worrying,
ectopic pregnancy, are increased compared with spon-
taneous pregnancy and hence a responsible clinic should at
least offer a ultrasound scan a few weeks after conception to
rule this out. Failure to diagnose ectopic pregnancy can
lead to catastrophic intraperitoneal bleeding, and rupture of
an ectopic pregnancy remains the leading cause of death in
the rst trimester of pregnancy. Women who conceive after
ART should be regarded as high risk obstetrically as there
is good evidence of a higher than average obstetric compli-
cation rate and of Caesarean delivery.
Preimplantation genetic diagnosis
One of the new growth areas for ART involves the use of
IVF to allow access to embryonic DNA. Although the
media have characterized techniques of preimplantation
genetic diagnosis (PGD) as leading to designer babies, the
reality in 2009 is that this technology is being used to
prevent conception of pregnancies affected by serious
genetic disorders that would lead to premature death and/
or severe disability in the child. PGD avoids the alternative
of prenatal diagnosis by amniocentesis or chorionic villus
sampling. The latter approach provides a diagnosis only
after a pregnancy is established, leading in many cases to
late rst trimester or second trimester abortion. Although
PGD has obvious advantage over prenatal diagnosis, tech-
niques for analysing the single cell collected by embryo
biopsy remain at the cutting edge of science, and a misdiag-
nosis can produce disastrous consequences. Responsible
laboratories take great care to minimize this risk but as in
other areas of clinical embryology, the processes used are
complex, involving many intricate steps and demanding
considerable skill from the operator.
IVF has come a long way since the almost miraculous
conception of Louise Brown. Clinics can now offer effec-
tive treatment to couples suffering from most of the
common causes of subfertility. However it is not a universal
panacea and should not be used where there is little or no
chance of success. The National Institute for Health and
Clinical Excellence (NICE) Guidelines on the management
of the infertile couple highlight the position of IVF as one
aspect of the holistic care of infertile patients. Some couples
should be advised to try naturally for a longer period
before entering treatment, others can be offered reproduc-
tive surgery or simpler techniques such as intrauterine inse-
mination (IUI) with good results, avoiding the cost and
stress of IVF. However, again, conict may sometimes occur
in a clinic that cannot offer surgical approaches or IUI, or
where the prot per case is signicantly greater after IVF.
Additionally, IVF techniques do not work well in women
aged over 40 years. For example, the United States SART
registry gives live birth rates for women aged 43 and 44
years at time of treatment as 5.1% and 3.0%, respectively,
and live birth after IVF in women over 44 years is vanish-
ingly rare. The profound demographic changes that have
occurred over the last three decades have resulted in an
increasing number of women in their 40s wishing to con-
ceive a child. Many nd this impossible naturally and
consult a fertility specialist while most will be pessimistic,
advise consideration of alternative approaches such as
oocyte donation from a younger woman or adoption. A
minority will offer repeated IVF cycles, often with multiple
adjuvant treatments in an attempt to achieve implantation.
Even in the rare cases where embryo implantation occurs,
miscarriage rates in this group are approximately 50% and
hence chance of live birth is low and potential for later dis-
satisfaction high. Despite considerable effort, techniques
such as co-treatment with steroids, Sildenal, heparin,
immunoglobulins or growth hormone, or attempts to select
the best embryo using preimplantation genetic selection
(PGS) have consistently failed to show evidence of benet
when subjected to randomized controlled trials and such
treatments should not be offered without research studies.
The image of IVF treatment purveyed by the media
invariably involves pictures of babies. In my view this
entirely misses the point of the process. IVF is about
helping infertile couples start or complete their family,
allowing them to raise, educate and enjoy children, giving
them the likelihood of support in old age and continuance
of their family line. These are among the most important
reasons for existence and drive the most powerful of all
human emotions. It is not surprising that the enormous
reward that success brings to many couples is mirrored by
the huge disappointment of failure. A good quality IVF
clinic will spend far more time managing expectations,
injecting realism and supporting those who have a negative
pregnancy test at the end of an arduous treatment pro-
gramme than on the happy minority who conceive after
treatment. Given the complexity of the science and the
profundity of the emotional burden of infertility it is hardly
surprising that litigation in this area of medicine is on the
increase.
200 AvMA Medical & Legal Journal
The AvMA Medical & Legal Journal 2009 Volume 15 Number 5
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Case Report MyelopathyDocument29 pagesCase Report MyelopathyNurul Hasanah SururyPas encore d'évaluation
- Outbreak of S. Weltevreden Linked To Fermented Cashew Nut Cheese in Victoria, BCDocument8 pagesOutbreak of S. Weltevreden Linked To Fermented Cashew Nut Cheese in Victoria, BCLeila RochaPas encore d'évaluation
- WRAS MarinasDocument4 pagesWRAS MarinasAdam ReesPas encore d'évaluation
- Body Image: Marika Tiggemann, Kristy HageDocument7 pagesBody Image: Marika Tiggemann, Kristy HageRachel VictorianaPas encore d'évaluation
- Food Systems For ChildrenDocument12 pagesFood Systems For ChildrenPaulin koffiPas encore d'évaluation
- APLS Scenario OSCE PDFDocument5 pagesAPLS Scenario OSCE PDFNikita JacobsPas encore d'évaluation
- JHU Press Fall 2013 CatalogDocument99 pagesJHU Press Fall 2013 CatalogjhupressPas encore d'évaluation
- Referral Letter To Specialist From GPDocument74 pagesReferral Letter To Specialist From GPyazz80% (5)
- Survey QuestionnaireDocument2 pagesSurvey Questionnairecyrusbatayan100% (1)
- Physical Fitness Test Individual Score CardDocument12 pagesPhysical Fitness Test Individual Score CardJunessa TadinaPas encore d'évaluation
- BURNS SoftDocument3 pagesBURNS SoftErlo John Asentista0% (1)
- MarriottDocument4 pagesMarriottSheikh Farhan AliPas encore d'évaluation
- 3M Disposable Filtering Facepiece Respirator Fitting Poster English and SpanishDocument2 pages3M Disposable Filtering Facepiece Respirator Fitting Poster English and SpanishTrunggana AbdulPas encore d'évaluation
- Mangune v. Ermita (2016)Document3 pagesMangune v. Ermita (2016)Cristelle Elaine Collera100% (1)
- Tano Vs SocratesDocument3 pagesTano Vs SocratesNimpa PichayPas encore d'évaluation
- 12 Week ProgramDocument45 pages12 Week ProgramCow SapiPas encore d'évaluation
- Ateneo de Zamboanga University: Course Outline (Second Semester) ZOO 208Document1 pageAteneo de Zamboanga University: Course Outline (Second Semester) ZOO 208Almira AhamadPas encore d'évaluation
- Infant Tub RationaleDocument4 pagesInfant Tub RationaleAllen Kenneth PacisPas encore d'évaluation
- Experiment 9 - Hydrolysis of CarbohydratesDocument2 pagesExperiment 9 - Hydrolysis of CarbohydratesJuren LasagaPas encore d'évaluation
- Lecture #3 - Carbohydrates & LipidsDocument23 pagesLecture #3 - Carbohydrates & Lipidsogangurel100% (3)
- Hazard Scale: 0 Minimal 1 Slight 2 Moderate 3 Serious 4 Severe Chronic HazardDocument4 pagesHazard Scale: 0 Minimal 1 Slight 2 Moderate 3 Serious 4 Severe Chronic HazardNazirAhmadBashiriPas encore d'évaluation
- 429-Article Text-1894-2-10-20210715Document12 pages429-Article Text-1894-2-10-20210715Ziya AstgaPas encore d'évaluation
- Colorado Department of Public Health and Environment: November 14 Public-Health Order UpdateDocument9 pagesColorado Department of Public Health and Environment: November 14 Public-Health Order UpdateMichael_Roberts2019Pas encore d'évaluation
- Procedure Checklist On OxygenationDocument2 pagesProcedure Checklist On OxygenationKhatlen BagaresPas encore d'évaluation
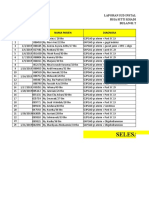
- Laporan Iud 2019Document91 pagesLaporan Iud 2019Yuli AntiPas encore d'évaluation
- YakultDocument15 pagesYakultMlb T. De TorresPas encore d'évaluation
- Ganglions Clinical Presentation - History and Physical ExaminationDocument3 pagesGanglions Clinical Presentation - History and Physical ExaminationAnonymous vOJH2hLMh6Pas encore d'évaluation
- MODULE 8: Settings, Processes, Methods, and Tools in Social WorkDocument4 pagesMODULE 8: Settings, Processes, Methods, and Tools in Social WorkAlexandra Nicole RugaPas encore d'évaluation
- MSDS PDFDocument5 pagesMSDS PDFdang2172014Pas encore d'évaluation
- Location: Capacity: Architect: Mr. Anil Yadav: Qutub Institutional Area 150 PatientsDocument18 pagesLocation: Capacity: Architect: Mr. Anil Yadav: Qutub Institutional Area 150 PatientsManishaDhimanPas encore d'évaluation