Académique Documents
Professionnel Documents
Culture Documents
Evaluation and Management of Abnormal Vaginal Bleeding PDF
Transféré par
Anonymous pJfAvlTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Evaluation and Management of Abnormal Vaginal Bleeding PDF
Transféré par
Anonymous pJfAvlDroits d'auteur :
Formats disponibles
www.medscape.
com
From Journal of Pediatric Health Care
Introduction
Abnormal vaginal bleeding is a common cause for concern among adolescents and their families, as well as a frequent
cause of visits to the emergency department and health care provider. While there are many causes of abnormal vaginal
bleeding, the most likely cause among otherwise healthy adolescents is dysfunctional uterine bleeding (DUB) resulting
from an immature hypothalamic-pituitary-ovarian axis, which results in anovulatory cycles and unpredictable bleeding.
However, abnormal vaginal bleeding also may be the presenting symptom of a more serious underlying condition or
problem. Furthermore, depending on the cause and severity of the bleeding, significant morbidity and mortality may be
associated with it. This article will discuss many of the common causes of DUB, as well as the diagnostic work-up and
management for this condition.
Definitions
Normal Bleeding
For most girls, menarche usually occurs within 2 to 3 years after the appearance of breast buds (Carswell &
Stafford, 2008).
The mean age of menarche varies somewhat based on ethnicity: 12.7 years for non-Hispanic White girls, 12.3
years for Black girls, and 12.5 years for Mexican American girls (Wu, Mendola, & Buck, 2002).
Many teens then experience "irregular" periods for 2 to 3 years following menarche because of anovulatory cycles
and an immature hypothalamic-pituitary-ovarian axis (Gray and Emans, 2007, Lavin, 1996).
Once "regular" menses are established, normal menstrual cycles are 21 to 40 days long, with bleeding usually
lasting 2 to 7 days and an average blood loss of 20 to 80 mL (Mitan & Slap, 2008).
Abnormal Bleeding
Menorrhagia is bleeding that lasts more than 7 consecutive days or is more than 80 mL of blood loss but still
occurs at regular intervals.
Bleeding that occurs at irregular intervals is termed metrorrhagia, and heavy irregular bleeding is
menometrorrhagia.
If menstrual cycles occur at intervals from 41 days to 3 months apart, this is considered to be oligomenorrhea.
Dysfunctional uterine bleeding is defined as abnormal shedding of the uterine lining in the absence of a structural
or medical abnormality and is most often due to anovulation (Gray and Emans, 2007, Mitan and Slap, 2008).
Although underlying pathology accounts for less than 10% of abnormal bleeding (Mitan & Slap, 2008), DUB is a
diagnosis of exclusion, and other causes must be ruled out.
Key to diagnosing the etiology of abnormal menstrual bleeding is a good history of the patient's cycles, including an
assessment of the amount of flow, to determine if her experiences are truly outside the realm of normal.
Differential Diagnosis
Of the many causes of abnormal bleeding ( Box ), some causes require immediate exclusion because failure to do so
may result in significant morbidity and mortality.
Authors and Disclosures
Laura J. Benjamins, MD, MPH, Assistant Professor, Department of Pediatrics, The University of Texas Medical School
at Houston, Houston, TX.
Laura J. Benjamins, MD, MPH
Posted: 07/13/2009; J Pediatr Health Care. 2009;23(3):189-193. 2009 Mosby, Inc.
Box. Differential Diagnosis For Abnormal Bleeding in Adolescents
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
1 of 7 30/07/2010 9:25
Pregnancy
Implantation
Ectopic pregnancy
Threatened, spontaneous, or missed abortion
Retained products of conception
Placenta accreta
Hematologic
Thrombocytopenia
von Willebrand disease
Factor deficiencies
Coagulation defects
Platelet dysfunction
Endocrine
Thyroid disorders
Hyperprolactinemia
Polycystic ovarian syndrome
Adrenal disorders
Ovarian failure
Infectious
Cervicitis (especially chlamydia)
Pelvic inflammatory disease
Pathology of the Reproductive Tract
Polyp
Fibroid
Myoma
Cervical dysplasia
Endometriosis
Medication
Hormonal contraceptives
Antipsychotics
Platelet inhibitors
Anticoagulants
Trauma
Sexual abuse
Laceration
Foreign body
Related to abortion or other surgical procedure
Other
Stress
Excessive exercise
Eating disorders
Systemic disease
Intrauterine device
Data from Emans, S. J., 2005.
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
2 of 7 30/07/2010 9:25
Pregnancy-related complications can present with any pattern of abnormal bleeding, with ectopic pregnancy being
one of the more serious conditions to consider.
Severe thrombocytopenia can be assessed quickly with a complete blood cell count.
A teen is more likely to have an underlying abnormality if she has to be hospitalized and her hemoglobin is less than
10 g/dL (Claessens & Cowell, 1981).
Pelvic inflammatory disease may present with vaginal bleeding in addition to lower abdominal pain.
While adult women frequently have underlying pathology such as fibroids, dysplasia, or cancer, teens rarely
present with such conditions. However, these conditions are sometimes seen in young women, and they must
remain in the differential of abnormal bleeding (Emans, 2005).
History
Medical and Surgical History
Systemic disease
Anemia
History of abortion and/or dilation and curettage
Current and recent medications: prescribed, over the counter, herbal
Prior chemoth6erapy
Menstrual History
Age at menarche
-The patient who is older at menarche is more likely to have a longer time of anovulatory, "irregular" cycles (Vihko &
Apter, 1984)
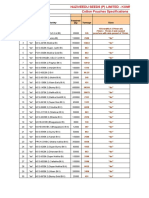
Length of cycles as determined by recording data on a calendar (Figure)
Length of bleeding in days as determined by recording data on a calendar
The number, if any, of "regular" periods experienced by the patient
Number of pads or tampons used in a 24-hour period and for how many days
-More than three soaked pads or six full regular-absorbency tampons a day for 3 or more days likely equates to
greater than 80 mL of blood loss (Brown, 2005)
History of flooding, clots or leaking, especially overnight, because this may be associated with a clotting disorder
(Brown, 2005)
Characteristics of the patient's very first period
-A "heavy" first period may be indicative of a bleeding diathesis, most commonly von Willebrand disease
(Claessens and Cowell, 1981, Brown, 2005)
Figure. Menstrual Calendar
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
3 of 7 30/07/2010 9:25
Social and Sexual History
Risk factors for sexually transmitted infections and pregnancy:
-Age of sexual debut and number of lifetime partners
-Date of last sexual activity and use of protection or not (condoms)
-History of a sexually transmitted infection in patient and partner(s)
-Sexual abuse (may also be associated with trauma)
Bleeding abnormalities may be associated with eating disorders and/or extreme physical activity; therefore, one
should ask about:
-Diet
-Exercise
Stress is associated with anovulation and DUB; therefore, one should inquire about:
-Illicit drug use
-Psychosocial stressors
Family History
Other female relatives with heavy periods or history of hysterectomy after childbirth because of bleeding (common
for von Willebrand disease)
Other family members with clotting problems, such as after circumcision, dental extraction, or a surgical procedure
Autoimmune diseases
Endocrine disorders
Cancer
Review of Systems
In addition to the pattern of bleeding and the amount of flow, other complaints found on the review of symptoms may
identify an underlying etiology (Table).
General: Fatigue; change in weight; night sweats, or hot flashes
Head, eyes, ears, nose, throat: Gum or nose bleeding
Cardiovascular: Palpitations; tachycardia
Respiratory: Shortness of breath
Gastrointestinal: Diarrhea; constipation
Genitourinary: Dysuria; vaginal discharge; dyspareunia; dysmenorrhea
Hematologic: Easy bleeding or bruising
Neurologic: Headaches; double vision or loss of vision
Table. Review of Systems and Physical Examination Findings and Possible Differential Diagnoses
Review of systems Physical examination Differential diagnoses
Heavy periods since menarche
Signs and symptoms of anemia
tachycardia, flow murmur, pallor
Bleeding disorder; most likely von
Willebrand
Easy bruising, gum bleeding, nose
bleeds
Bruises, petechiae
Platelet dysfunction;
thrombocytopenia
Heat/cold intolerance, weight
changes, diarrhea or constipation
Goiter, brittle hair, and nails Thyroid disorders
Nipple discharge
Galactorrhea, possible peripheral visual
field deficits
Prolactinemia; prolactinoma;
antipsychotic agents
Abnormal hair growth Facial hair, acne Polycystic ovarian syndrome
Dysuria, discharge
Vaginal discharge, inflamed vagina or
cervix
Vaginitis; cervicitis
Abdominal pain
Cervical motion, adnexal or uterine
tenderness
Pelvic inflammatory disease
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
4 of 7 30/07/2010 9:25
Skin: Abnormal hair growth; acne; hair loss
Other: Nipple discharge
Physical Examination
In a patient with prolonged or heavy bleeding, an evaluation should al ways begin with vital signs. Attention is focused on
signs of anemia, as well as clues of other possible underlying causes ( Table ).
Vital signs: Is the patient hemodynamically stable, tachycardic, or hypotensive? Are there orthostatic changes?
General: Is the patient pale, or does she appear tired? Is there altered mental status? Is there obesity, or is the
patient excessively thin?
Head, eyes, ears, nose, throat: Is there conjunctival pallor, epistaxis, or gum bleeding?
Neck: Are lymphadenopathy or thyromegaly noted?
Breast: Is galactorrhea noted? If so, nipple discharge should be evaluated microscopically for fat globules.
Heart: Is a flow murmur present?
Abdomen: Are hepatosplenomegaly or lower abdominal pain identified?
Genitourinary: On external examination, are discharge, inflammation, lacerations, or other signs of trauma found? Is
the clitoris of normal size? Is the bleeding in fact from the vagina? Is a foreign body (e.g., a retained tampon)
present? Is the cervix normal, and does movement of it or the adnexa or uterus result in pain?
-For patients who cannot tolerate a speculum or bimanual examination, a pelvic examination may need to be done
under anesthesia.
Skin: Are findings of bruises, petechiae, acne, hirsutism, acanthosis nigricans, or striae noted?
Neurologic: Are visual field deficits noted?
Laboratory and Other Studies
Initial work-up should include the following:
Urine pregnancy test and/or quantitative serum pregnancy test
Complete blood cell count with differential and platelet count
A pelvic ultrasound also may aid in the diagnosis
If bleeding is severe or an underlying bleeding disorder is suspected because of the history of physical examination, the
following can be ordered (Brown, 2005):
Prothrombin time and partial thromboplastin time
Bleeding time and platelet aggregation
Table. Review of Systems and Physical Examination Findings and Possible Differential Diagnoses
Review of systems Physical examination Differential diagnoses
Heavy periods since menarche
Signs and symptoms of anemia
tachycardia, flow murmur, pallor
Bleeding disorder; most likely von
Willebrand
Easy bruising, gum bleeding, nose
bleeds
Bruises, petechiae
Platelet dysfunction;
thrombocytopenia
Heat/cold intolerance, weight
changes, diarrhea or constipation
Goiter, brittle hair, and nails Thyroid disorders
Nipple discharge
Galactorrhea, possible peripheral visual
field deficits
Prolactinemia; prolactinoma;
antipsychotic agents
Abnormal hair growth Facial hair, acne Polycystic ovarian syndrome
Dysuria, discharge
Vaginal discharge, inflamed vagina or
cervix
Vaginitis; cervicitis
Abdominal pain
Cervical motion, adnexal or uterine
tenderness
Pelvic inflammatory disease
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
5 of 7 30/07/2010 9:25
von Willebrand panel (done prior to initiating hormonal therapy)
Factor levels and activity (depending on family history and ethnicity)
If an endocrine disorder is suspected:
Thyroid-stimulating hormone to screen for thyroid disorders
Prolactin (can be mildly elevated after a breast examination; levels >100 ng/mL suggest a pituitary adenoma)
Total and free testosterone (usually elevated in polycystic ovarian syndrome)
Dehydroepiandrosterone sulfate to assess for adrenal tumors
Luteinizing hormone and follicle-stimulating hormone (may aid in the evaluation of pituitary or ovarian function)
For patients with suspected infectious etiologies:
Wet mount of discharge if bleeding not severe
Urine nucleic amplification test for gonorrhea and chlamydia
Management
The management of abnormal vaginal bleeding is determined by the underlying etiology and by the severity of the
bleeding. The goals of controlling abnormal bleeding include preventing complications, such as anemia, as well as
restoring regular cyclical bleeding. Underlying systemic, endocrine disorders or bleeding disorders are addressed, and
patients may require referral to appropriate specialists for further evaluation and management if one of these conditions is
identified. Guidelines for management of abnormal bleeding related to hormonal contraception, bleeding diatheses, and
polycystic ovarian syndrome can be found elsewhere (see Brown, 2005, Emans, 2005, Mitan and Slap, 2008, Speroff and
Fritz, 2005).
For the patient in whom no other etiology is found, management of DUB will in part be directed by the amount of flow, the
degree of associated anemia, and patient and family comfort with different treatment modalities (Gray and Emans, 2007,
Mitan and Slap, 2008, Speroff and Fritz, 2005).
Light to Moderate Flow; Hemoglobin >12 g/dL
Reassurance
Multivitamin with iron
A nonsteroidal anti-inflammatory drug may help to decrease flow
Re-evaluate patient in 3 months; sooner if bleeding persists or becomes more severe
Moderate Flow; Hemoglobin 10 to 12 g/dL
Oral contraceptive pills (OCPs) (e.g., monophasic with 30 to 35 g of ethinyl estradiol)
-One pill twice daily for 1 to 5 days, until the bleeding stops
Once the bleeding stops, continue OCPs with a new pack, one pill daily, for 3 to 6 months
Iron supplementation (e.g., ferrous sulfate 325 mg twice daily) for 6 months to replenish iron stores
Nonsteroidal anti-inflammatory drugs may be helpful
Heavy Flow; Hemoglobin 8 to 10 g/dL; Hemodynamically Stable
May be able to manage the patient as under "Moderate Flow" if the family can assist with the management plan and
follow-up
If bleeding persists, increase the OCP to 3 or 4 times a day for a few days until the bleeding slows, then taper to
two then one pill daily; patient may require an antiemetic prior to each pill to help prevent nausea
Follow closely; once bleeding stops, continue daily pills for 6 months
Heavy Flow; Hemoglobin <7 g/dL or if Hemodynamically Unstable
Admit to the hospital
Consider blood transfusion depending on degree and persistence of bleeding, as well as severity of hemodynamic
instability
Begin OCP with 50 g of ethinyl estradiol every 6 hours until bleeding slows
Taper administration of pills to one pill a day over the next 7 days (e.g., one pill every 6 hours for 2 days, then every
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
6 of 7 30/07/2010 9:25
8 hours for 2 days, every 12 hours for 2 days, then once daily)
Anti-emetic agents likely will be needed
If bleeding does not slow after the first two doses of the 50 g OCP, conjugated estrogens given intramuscularly or
intravenously at a dose of 25 mg every 6 hours to a maximum 6 doses may be initiated
If bleeding still persists, consider dilation and curettage
For patients with a contraindication to estrogen-containing regimens, progesterone, 10 mg once daily for 5 to 10 days,
may be effective for light to moderate flow. Patients also may be cycled monthly on a progesterone-only regimen. Other
alternatives include depot medroxyprogesterone acetate, 150 mg intramuscularly every 3 months, or a levonorgestrel
intrauterine device (which lasts for 5 years). These latter methods, however, often are associated with irregular bleeding
and spotting themselves.
Summary
Abnormal vaginal bleeding in adolescents is a common occurrence, and the primary care provider should be comfortable
with its evaluation and management. While most adolescents will require only outpatient management and reassurance as
their cycles become ovulatory over time, health care providers must evaluate each teen closely so that significant
pathology can be quickly identified and treated appropriately.
Correspondence: Laura J. Benjamins, MD, MPH, University of Texas Medical School at Houston, 1133 John Freeman Blvd, JJL 495, Houston, TX
70030; E-mail: laura.j.benjamins@uth.tmc.edu
J Pediatr Health Care. 2009;23(3):189-193. 2009 Mosby, Inc.
References
Brown, D. L. (2005). Congenital bleeding disorders. Current Problems in Pediatric & Adolescent Health Care, 35,
38-62.
Carswell, J. M., & Stafford, D. E. J. (2008). Normal physical growth and development. In L. S. Neinstein, C. N.
Gordon, D. K. Katzman, D. S. Rosen, & E. R. Woods (Eds.), Adolescent health care: A practical guide (5th ed.)
(pp. 3-26) Philadelphia: Lippincott Williams & Wilkins.
Claessens, E. A., & Cowell, C. A. (1981). Dysfunctional uterine bleeding in the adolescent. Pediatric Clinics of
North America, 28, 369-378.
Emans, S. J. (2005). Dysfunctional uterine bleeding. In S. J. Emans, M. R. Laufer, & D. P. Goldstein (Eds.),
Pediatric and adolescent gynecology (5th ed., pp. 270286). Philadelphia: Lippincott Williams & Wilkins.
Gray, S. H., & Emans, S. J. (2007). Abnormal vaginal bleeding in adolescents. Pediatrics in Review, 28, 175-182.
Lavin, C. (1996). Dysfunctional uterine bleeding in adolescents. Current Opinion in Pediatrics, 8, 328-332.
Mitan, L. A. P., & Slap, G. B. (2008). Dysfunctional uterine bleeding. In L. S. Neinstein, C. N. Gordon, D. K.
Katzman, D. S. Rosen, & E. R. Woods (Eds.), Adolescent health care:Apractical guide (5th ed.) (pp. 687-690).
Philadelphia: Lippincott Williams & Wilkins.
Speroff, L., & Fritz, M. A. (2005). Dysfunctional uterine bleeding. Clinical gynecologic endocrinology and infertility
(7th ed., pp. 547571). Philadelphia: Lippincott Williams & Wilkins.
Vihko, R., & Apter, D. (1984). Endocrine characteristics of adolescent menstrual cycles: Impact of early menarche.
Journal of Steroid Biochemistry, 20, 231-236.
Wu, T., Mendola, P., & Buck, G. M. (2002). Ethnic differences in the presence of secondary sex characteristics and
menarche among US girls: The third national health and nutrition examination survey, 1988-1994. Pediatrics, 110,
752-757.
Evaluation and Management of Abnormal Vaginal Bleeding in Adolesce... http://www.medscape.com/viewarticle/704152_print
7 of 7 30/07/2010 9:25
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- D. Michael Quinn-Same-Sex Dynamics Among Nineteenth-Century Americans - A MORMON EXAMPLE-University of Illinois Press (2001)Document500 pagesD. Michael Quinn-Same-Sex Dynamics Among Nineteenth-Century Americans - A MORMON EXAMPLE-University of Illinois Press (2001)xavirreta100% (3)
- Analysis of The Tata Consultancy ServiceDocument20 pagesAnalysis of The Tata Consultancy ServiceamalremeshPas encore d'évaluation
- 7 CAAT-AIR-GM03 Guidance-Material-for-Foreign-Approved-Maintenance-Organization - I3R0 - 30oct2019 PDFDocument59 pages7 CAAT-AIR-GM03 Guidance-Material-for-Foreign-Approved-Maintenance-Organization - I3R0 - 30oct2019 PDFJindarat KasemsooksakulPas encore d'évaluation
- IsaiahDocument7 pagesIsaiahJett Rovee Navarro100% (1)
- 2nd Quarter Exam All Source g12Document314 pages2nd Quarter Exam All Source g12Bobo Ka100% (1)
- Value Chain AnalaysisDocument100 pagesValue Chain AnalaysisDaguale Melaku AyelePas encore d'évaluation
- Task Performance Valeros Roeul GDocument6 pagesTask Performance Valeros Roeul GAnthony Gili100% (3)
- 06 Ankit Jain - Current Scenario of Venture CapitalDocument38 pages06 Ankit Jain - Current Scenario of Venture CapitalSanjay KashyapPas encore d'évaluation
- EScholarship UC Item 8k05n5csDocument10 pagesEScholarship UC Item 8k05n5csAnonymous pJfAvlPas encore d'évaluation
- Left Ovarian Brenner Tumor: Key-Word: Ovary, NeoplasmsDocument2 pagesLeft Ovarian Brenner Tumor: Key-Word: Ovary, NeoplasmsAnonymous pJfAvlPas encore d'évaluation
- Aafp PDFDocument8 pagesAafp PDFAnonymous umFOIQIMBAPas encore d'évaluation
- Executive Summary of Methanol Poisoning - 03Document13 pagesExecutive Summary of Methanol Poisoning - 03Anonymous pJfAvl100% (1)
- Oxygen-Free Radicals Impair Fracture Healing in Rats: A Were ofDocument3 pagesOxygen-Free Radicals Impair Fracture Healing in Rats: A Were ofAnonymous pJfAvlPas encore d'évaluation
- Determination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriaDocument5 pagesDetermination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriamiguelPas encore d'évaluation
- Kangaroo High Build Zinc Phosphate PrimerDocument2 pagesKangaroo High Build Zinc Phosphate PrimerChoice OrganoPas encore d'évaluation
- HP MSM775 ZL Controller Installation GuideDocument21 pagesHP MSM775 ZL Controller Installation GuidezarandijaPas encore d'évaluation
- Task 2 - The Nature of Linguistics and LanguageDocument8 pagesTask 2 - The Nature of Linguistics and LanguageValentina Cardenas VilleroPas encore d'évaluation
- Venue:: Alberta Electrical System Alberta Electrical System OperatorDocument48 pagesVenue:: Alberta Electrical System Alberta Electrical System OperatorOmar fethiPas encore d'évaluation
- Solution Document For Link LoadBalancerDocument10 pagesSolution Document For Link LoadBalanceraralPas encore d'évaluation
- RPS Manajemen Keuangan IIDocument2 pagesRPS Manajemen Keuangan IIaulia endiniPas encore d'évaluation
- Budget ProposalDocument1 pageBudget ProposalXean miPas encore d'évaluation
- أثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Document17 pagesأثر البحث والتطوير على النمو الاقتصادي - دراسة قياسية لحالة الجزائر (1990 -2014)Star FleurPas encore d'évaluation
- Mbtruck Accessories BrochureDocument69 pagesMbtruck Accessories BrochureJoel AgbekponouPas encore d'évaluation
- Indiabix PDFDocument273 pagesIndiabix PDFMehedi Hasan ShuvoPas encore d'évaluation
- Evolution Epidemiology and Etiology of Temporomandibular Joint DisordersDocument6 pagesEvolution Epidemiology and Etiology of Temporomandibular Joint DisordersCM Panda CedeesPas encore d'évaluation
- For Printing Week 5 PerdevDocument8 pagesFor Printing Week 5 PerdevmariPas encore d'évaluation
- Julian BanzonDocument10 pagesJulian BanzonEhra Madriaga100% (1)
- Agitha Diva Winampi - Childhood MemoriesDocument2 pagesAgitha Diva Winampi - Childhood MemoriesAgitha Diva WinampiPas encore d'évaluation
- Cotton Pouches SpecificationsDocument2 pagesCotton Pouches SpecificationspunnareddytPas encore d'évaluation
- Lyndhurst OPRA Request FormDocument4 pagesLyndhurst OPRA Request FormThe Citizens CampaignPas encore d'évaluation
- Did Angels Have WingsDocument14 pagesDid Angels Have WingsArnaldo Esteves HofileñaPas encore d'évaluation
- DLL Week 7 MathDocument7 pagesDLL Week 7 MathMitchz TrinosPas encore d'évaluation
- Social Networking ProjectDocument11 pagesSocial Networking Projectapi-463256826Pas encore d'évaluation
- Peptic UlcerDocument48 pagesPeptic Ulcerscribd225Pas encore d'évaluation
- Forensic BallisticsDocument23 pagesForensic BallisticsCristiana Jsu DandanPas encore d'évaluation