Académique Documents
Professionnel Documents
Culture Documents
Korean Woman Mammography Screening
Transféré par
Jesse M. MassieDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Korean Woman Mammography Screening
Transféré par
Jesse M. MassieDroits d'auteur :
Formats disponibles
Health Care for Women International, 29:151164, 2008
Copyright Taylor & Francis Group, LLC
ISSN: 0739-9332 print / 1096-4665 online
DOI: 10.1080/07399330701738176
Stages of Change: Korean Womens Attitudes
and Barriers Toward Mammography Screening
HEE SUN KANG
Department of Nursing, College of Medicine, Chung-Ang University, 221 Heuksukdong
Dongjakku, Seoul, Korea
EILEEN THOMAS
University of Colorado, School of Nursing, Denver, Colorado, USA
BO EUN KWON
Seoul Womens College of Nursing, Seoul, Korea
MYUNG-SUN HYUN
College of Nursing, Ajou University, Suwon, Korea
EUN MI JUN
Department of Nursing, College of Medicine, Dongeui University, Busan, Korea
The positive and negative aspects of breast cancer screening were
measured to gain insight into the barriers that prevent Korean
women from participating in mammography screening. Breast
cancer screening behaviors, attitudes, and barriers were identied
from a convenience sample of 328 Korean women recruited in
Seoul, Gyeonggi, and Jeju, South Korea. Pros, cons, and decisional
balance constructs of the transtheoretical model of behavior change
were used to identify stages of change in attitude related to
mammography screening. There were signicant differences inpros
(F = 5.175, p = .001) and cons (F = 3.357, p = .012) across the
ve stages of change for mammography. Participants indicated
that the major barriers to mammography screening were, in order
of frequency, the belief that an absence of symptoms meant there
was no need for a breast examination, the high cost of breast cancer
screening, lack of time, lack of information, embarrassment, fear
about x-rays and test results, reliance on breast self-examination
Received 22 March 2006; accepted 17 August 2007.
Address correspondence to Eileen Thomas, PhD, RN, Assistant Professor, University
of Colorado, School of Nursing, 4200 E 9th Avenue, C288-18, Denver, CO 80262, USA.
E-mail: Eileen.Thomas@uchsc.edu
151
152 H. S. Kang et al.
(BSE), and discomfort or pain. The benets of breast cancer
screening should be emphasized among Korean women.
Previous studies primarily have focused on Korean womens screening
rates and predictive factors of participation in all three measures of
breast cancer screening. Little information is available, however, on Korean
womens attitudes toward and barriers to mammography. The authors used
the transtheoretical model of behavioral change to explore Korean womens
BSE, clinical breast examination (CBE) and mammography screening
behaviors; examined womens attitudes toward various stages of change
related to mammography screening; and identied barriers to mammography
screening. Findings suggest that attitudes toward breast cancer screening
and barriers to mammography screening should be explored further among
Korean women, but these barriers are not unique to a specic geographical
location. We recommend that future research should take a more global and
interdisciplinary approach.
Breast cancer is the most common form of cancer in Korean women.
Mortality rates are slowly rising in Korea, and the incidence is expected to
increase over time (Ahn, Yoo, & Korean Breast Cancer Society, 2006; Choi,
Kim, Shin, Noh, & Yoo, 2005). Unlike in the United States and Switzerland,
where the incidence does not peak until women are over the age of 50 years,
incidence rates begin to rise when Korean women are in their early thirties
and peak between the ages of 40 and 50 (Bouchardy et al., 2006; Smigal
et al., 2006).
Breast cancer is dened as a multifactorial disease caused by nongenetic
and genetic factors. Currently, there are no accepted and recognized standard
methods of breast cancer prevention. Although there remains discord
within the healthcare community about appropriate breast cancer screening
measures, currently breast self-examination (BSE), clinical breast examination
(CBE), and mammography offer the greatest hope for reducing mortality and
improving survival (Thomas, 2004, p. 296). For women with an average
risk of getting breast cancer, the American Cancer Society (ACS, 2001)
recommends annual mammography screening beginning at age 40, annual
CBE for women aged 40 and older, and CBE every 3 years for women
between the ages of 20 and 40 (Smith et al., 2003). The Korean Breast
Cancer Society and the Korean National Cancer Center recommend monthly
BSE for women aged 30 and older, CBE every 2 years for women aged 35
and older, and regular mammography screening and CBE at least once every
1 to 2 years for women aged 40 and older (National Cancer Center, 2006).
However, a national survey showed that Korean womens breast cancer
screening rates remain at a low level of 13.3% (Sung, Park, Shin, & Choi,
2005).
Korean Womens Attitudes Toward Mammography 153
BACKGROUND
The transtheoretical model of behavioral change has been used to assess
womens breast cancer screening behaviors and to promote breast cancer
screening (Tu et al., 2002). Developed in 1979, the transtheoretical model is
the result of a comparative analysis of 18 major theories of psychotherapy
and behavioral change and is used to conceptualize the process of intentional
behavior change. According to this model, behavior change is viewed as a
ve-stage process or continuum related to a persons readiness to change.
The ve stages are precontemplation, contemplation, preparation, action,
and maintenance. Each stage is characterized by changes in decisional
balance, or the balance between benets and costs associated with engaging
in a particular behavior (Prochaska, Norcross, & DiClemente, 1994).
Findings from previous studies in diverse age groups and ethnic popula-
tions indicated that the decisional balance between pros and cons regarding
mammography was associated with mammography stage in Filipino, Latino,
African American, Chinese, and White women (Otero-Sabogal, Stewart,
Shema, & Pasick, 2006). However, more research is being recommended:
with more diverse populations (Spencer, Pagell, & Adams, 2005). In addition,
there are inconsistent results on the crossover between the pros and cons of
mammography screening that occurred in the contemplation stage (Chamot,
Charvet, & Perneger, 2001) or in closer to the action stage (Prochaska,
Velicer, et al., 1994). There is also a paucity of research on the decisional
balance and stage of change of mammography among Korean women,
although health care providers must gain a better understanding of the
decisional balance and subsequent stages of change to develop the most
effective screening promotion strategies. Also, efforts to explore barriers
to mammography that have not been examined in previous studies may
increase early diagnosis and treatment of breast cancer among Korean
women. Overall, this study will help bridge the gap in existing knowledge.
METHODS
Setting and Sample
A cross-sectional, descriptive study design was used for this study. A
convenience sample of 328 women aged 30 years and older with no
history of breast cancer was recruited from three urban areas in South
Korea: Seoul, Gyeonggi, and Jeju. Data were collected over a 4-month
period, from June 1 through September 30, 2004, using self-administered
questionnaires. The study was approved by the Human Subjects Committee
of the National Health Insurance Corporation Ilsan Hospital, and all
participants provided informed consent prior to completing the survey. To
154 H. S. Kang et al.
increase the representative nature of our study, we included unemployed
and employed women. All participants were informed about the purpose of
the study and were told that participation was voluntary and anonymous.
Inclusion criteria were women aged 30 and over. Women with a history of
breast cancer were excluded from the study.
Procedure
The study was conducted in a hospital, medical ofces, and apartment
complexes. Women who agreed to take part in the study were provided with
a self-administered questionnaire that took 15 to 20 minutes to complete.
Screening behavior was identied in response to questions concerning BSE,
CBE, and mammography.
Instrument
The questionnaire included questions regarding demographic characteristics,
breast cancer screening behavior, attitudes toward mammography, and
stages of change for mammography. Age was categorized into three
groups: 30 to 34, 35 to 39, and 40+ years. Questions regarding education
(middle school, high school, or college), marital status (married or not
married), and employment (employed or not employed) also were included.
Socioeconomic status was categorized into three groups according to
monthly income: <2000000, 2000000 to <3000000, and 3000000 won
(< $2,135, $2,135 to 3,202, and $3202 [USD]).
Women were asked whether they had ever had a CBE or mammogram
and whether they were practicing monthly BSE. The questions were
answered by checking yes or no. BSE was categorized as monthly,
irregular, or never had.
Attitude (pros, cons, and decisional balance) toward mammography and
the ve changes in attitude toward mammography screening were measured
using an instrument developed by Rakowski and colleagues (1997) and
translated by Lee (2003). This scale has 13 items and consists of two subscales
that represent the positive (pros, six items) and negative (cons, seven items)
aspects of mammography screening. The pros include statements regarding
the benets of mammograms, such as, Having a mammogram every year
or two will give me a feeling of control over my health. The cons include
negative statements about mammograms, such as, Mammograms have a
high chance of leading to breast surgery that is not needed. Responses were
measured on a 5-point Likert scale that ranged from 1 (strongly disagree) to
5 (strongly agree). Scores on the pros and cons subscale are calculated
by averaging the six pro and seven con items, respectively. The possible
score for pros ranged from 6 to 30, with a higher score indicating a more
favorable view of mammography. Scores on the cons subscale are calculated
Korean Womens Attitudes Toward Mammography 155
by averaging the seven con items. The possible score for cons ranged
from 7 to 35, with a higher score indicating a more unfavorable view of
mammography. The validity for pros and cons has been established (Lee,
2003; Rakowski et al., 1997). The reliability of the original scales was.74 for
pros and.73 for cons. The reliability of the translated scales was.74 for pros
and.72 for cons (Lee, 2003) and.77 and.69 for pros and cons, respectively,
in this study. Scores on pros and cons were converted into standardized
T scores (M = 50, SD = 10), and then decisional balance was calculated
by subtracting the T score for the cons scale from the T score for the
pros scale. Positive values of decisional balance reect a globally favorable
attitude toward mammography, and negative values reect an unfavorable
attitude.
The stages of change for mammography screening were examined
using an algorithm that has ve stages: precontemplation, contemplation,
relapse, action, and maintenance (Lee, 2003). Each stage of change denes
individuals readiness to alter their behavior based on actions they have taken
and their future plans. Women were classied in the precontemplation stage
if they reported never having had a mammogram and were not planning
to have one that year. Women were classied in the contemplation stage
if they had never received a mammogram but were planning to have one
within a year. Women were considered relapsed if they had received a
mammogram previously and were not planning to have one within a year.
Women were classied in the action stage if they had had a mammogram
and were planning to have another within a year. Women were dened as
regular users in the maintenance stage if they had received a mammogram
regularly and were planning to have another within a year.
At the end of the questionnaire, participants were asked to describe
from one to three barriers that prevent them from following recommended
guidelines for mammography screening.
Data Analysis
Data were analyzed using the SPSS for Windows program (version 12.0).
Attitude toward mammography, distribution of the ve stages of change,
and selected demographic factors were expressed using descriptive statistics
that included frequencies, percentages, means, and standard deviations.
Cronbachs alpha was used to measure internal consistency for the scales
on each instrument. One-way analysis of variance was performed to assess
differences in mean scores of pros and cons in the different stages of
mammography adoption, and post-hoc analysis was used to determine at
which stages mean differences existed. Content analysis was used for analysis
of the open-ended questionnaire to determine barriers that prevent women
from obtaining mammography exams.
156 H. S. Kang et al.
The current breast cancer screening guidelines of the Korean Breast
Cancer Society and Korean National Cancer Center recommend that women
aged 35 years and older should have a CBE and women aged 40 years and
older should have regular mammograms. Based on recommended breast
cancer screening guidelines, we analyzed CBE only in women aged 35 and
over and mammography screening behavior in women aged 40 years and
over.
FINDINGS
A total of 328 women participated in the study. The average age was
37.69 years (SD = 6.09), with a range of 30 to 61 years. Two-thirds
of the participants (66.8%; n = 219) had at least a college education,
and approximately one-third (30.2%) had a high school education. Most
participants were married (89.6%, n = 294), with 30% reporting a monthly
household income below 2,000,000 won (1,000 won is equivalent to
approximately U.S. $1), 30.4% reporting an income of between 2,000,000
and 3,000,000 won, and 39.6% reporting an income of more than 3,000,000
won. Over half of the participants (52.7%) were employed.
BSE, CBE, and Mammography Behaviors
Only 2.7% of women reported following recommended screening guidelines
for monthly BSE, 62.2% practiced BSE irregularly, and 35% had never
performed a BSE. The majority of participants had never had a CBE, and
only 25.7% (n = 53) of women aged 35 years and older had ever received a
CBE. Among participants aged 40 years and older, almost half (48.3%) had
never had a mammogram.
Stages of Change
Among women aged 40 years and older, 30% (n = 36) were precontempla-
tors, 18.3% (n = 22) were contemplators, 23.3% (n = 28) were in the relapse
stage, 13.3% (n = 16) were in the action stage, and 15% (n = 18) were in
the maintenance stage.
Attitude (Pros, Cons, and Decisional Balance)
The item mean scores for pros, cons, and decisional balance were 3.48
(SD = .63), 2.81 (SD = .67), and 1.66 (SD = 16.19), respectively. The
mean scores for women aged 3034, 3539, and 40 and over were 3.35
(SD = .56), 3.57 (SD = .56), and 3.54 (SD = .71) for pros and 2.83 (SD
= .63), 2.84 (SD = .69), and 2.76 (SD = .71) for cons, respectively. There
Korean Womens Attitudes Toward Mammography 157
were statistically signicant differences only in pros among three age groups
(F = 4.06, p = .018). Tukeys post-hoc tests revealed that the pro scores of
30- to 34-year-olds were signicantly lower than that of 35- to 39-year-old
age groups ( p = .047). The scores for decisional balance varied from 6.89
to 15.52.
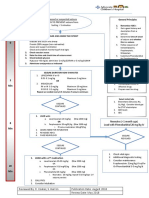
Pros and Cons Within the Stages of Change
There were signicant differences in pros (F = 5.175, p = .001) and cons (F
= 3.357, p = .012) across the ve stages of change for mammography (Table
1). Tukeys post-hoc tests revealed that individuals in the precontemplation
stage had a signicantly lower mean pro score than those in the maintenance
( p< .0001) stage. In contrast, individuals in the precontemplation stage had
a signicantly higher mean con score than those in the maintenance ( p =
.030) stage. Mean T-scores of pros increased from the precontemplation to
the maintenance stage. The scores of decisional balance varied from 6.89 in
the precontemplation stage to 15.52 in the maintenance stage. The crossover
occurred between precontemplation and contemplation stage.
Perceived Mammography Screening Barriers
Participants were asked to describe barriers that prevented them from having
regular mammograms. A belief that an absence of symptoms means that there
is no need for a breast examination was the most cited reason, followed by
the high cost of breast cancer screening, lack of time, lack of information,
embarrassment, fear about x-rays and test results, reliance on BSE, and
discomfort or pain (Table 2).
DISCUSSION
The ndings from this study indicate that most Korean women perform BSE
irregularly or not at all. According to the recent American Cancer Society
guidelines for breast cancer screening (Smith et al., 2003), it is acceptable
for women to choose not to perform BSE because the ability of this method
to reduce breast cancer mortality remains controversial. Helping women to
gain familiarity with their own breast composition and encouraging women
to be aware of changes in their breasts may be more effective than BSE.
Furthermore, the importance of recognizing and reporting these changes, as
well as any symptoms, to a health professional should be emphasized.
There is a paucity of studies that explore CBE in Korean women. It also
has been difcult to assess CBE performance. Our estimate of the percentage
of Korean women who have ever received a CBE, however, was far below
that of Korean American women (53%; Lee, Fogg, & Sadler, 2006). There
T
A
B
L
E
1
P
r
o
s
,
C
o
n
s
,
a
n
d
D
e
c
i
s
i
o
n
a
l
B
a
l
a
n
c
e
A
c
r
o
s
s
S
t
a
g
e
s
o
f
C
h
a
n
g
e
(
N
=
1
2
0
)
5
s
t
a
g
e
s
o
f
r
e
a
d
i
n
e
s
s
t
o
C
h
a
n
g
e
P
r
e
c
o
n
t
e
m
p
l
a
t
i
o
n
C
o
n
t
e
m
p
l
a
t
i
o
n
R
e
l
a
p
s
e
A
c
t
i
o
n
M
a
i
n
t
e
n
a
n
c
e
(
n
=
3
6
)
(
n
=
2
2
)
(
n
=
2
8
)
(
n
=
1
6
)
(
n
=
1
8
)
V
a
r
i
a
b
l
e
M
(
S
D
)
M
(
S
D
)
M
(
S
D
)
M
(
S
D
)
M
(
S
D
)
F
(
p
)
T
u
k
e
y
H
S
D
P
r
o
s
3
.
2
1
3
.
5
2
3
.
6
0
3
.
6
0
4
.
0
7
5
.
1
7
5
P
C
<
M
(
.
7
8
)
(
.
4
4
)
(
.
5
7
)
(
.
6
0
)
(
.
8
3
)
(
.
0
0
1
)
C
o
n
s
2
.
9
9
2
.
6
8
2
.
9
3
2
.
4
9
2
.
4
0
3
.
3
5
7
P
C
<
M
(
.
5
9
)
(
.
6
9
)
(
.
7
4
)
(
.
8
7
)
(
.
5
5
)
(
.
0
1
2
)
T
p
r
o
s
4
5
.
7
8
5
0
.
6
1
5
1
.
9
8
5
2
.
0
3
5
9
.
5
3
5
.
1
7
5
P
C
<
M
(
1
2
.
4
3
)
(
6
.
9
7
)
(
9
.
0
6
)
(
9
.
6
2
)
(
1
3
.
2
1
)
(
.
0
0
1
)
T
c
o
n
s
5
2
.
6
7
4
8
.
1
3
5
1
.
7
9
4
5
.
3
0
4
4
.
0
2
3
.
3
5
7
P
C
<
M
(
8
.
7
4
)
(
1
0
.
2
2
)
(
1
0
.
9
2
)
(
1
2
.
9
3
)
(
8
.
2
3
)
(
.
0
1
2
)
D
e
c
i
s
i
o
n
a
l
b
a
l
a
n
c
e
6
.
8
9
2
.
4
8
.
1
9
6
.
7
3
1
5
.
5
2
7
.
6
7
6
P
C
<
A
,
M
(
1
4
.
4
6
)
(
1
3
.
7
2
)
(
1
4
.
0
4
)
(
1
9
.
1
9
)
(
1
2
.
1
8
)
(
<
.
0
0
0
1
)
C
,
R
<
M
T
p
r
o
s
a
n
d
T
c
o
n
s
:
s
t
a
n
d
a
r
d
i
z
e
d
T
s
c
o
r
e
s
(
M
=
5
0
,
S
D
=
1
0
)
;
D
e
c
i
s
i
o
n
a
l
b
a
l
a
n
c
e
:
T
p
r
o
s
T
c
o
n
s
.
158
Korean Womens Attitudes Toward Mammography 159
TABLE 2 Perceived Mammography Screening Barriers (N = 208)
Barriers n (%)
No need for a breast exam and no symptoms 88 (30.6)
Cost of breast cancer screening 54 (18.8)
Lack of time 39 (13.5)
Lack of information 30 (10.4)
Embarrassment 25 (8.7)
Fear about x-ray and test results 22 (7.6)
Reliance on BSE 19 (6.6)
Discomfort/pain 11 (3.8)
are a few possible explanations for this. First, Korean doctors spend a small
amount of time examining each client and may not have enough time to
perform a CBE. Second, Korean women do not feel comfortable exposing
their breasts in an examination, especially to male doctors. A previous study
reported that Korean women feel shameful and humiliated during breast
cancer screening exams when the physician is male (Im, Park, Lee, & Yun,
2004). Thus, female clinicians should be made available to women who
are uncomfortable with male doctors. Clinician condence and comfort also
should be explored as potential barriers that prevent women from having a
CBE.
Although mammography is recommended for women aged 40 and
older, almost half of the participants in this age range had never had a
mammogram. This is far lower than the 60% screening rate proposed in the
Korea health plan 2010 (Korea National Institute of Health, 2005). Clinicians
should stress the importance of breast cancer screening and recommend
mammograms since they could have an important effect on whether women
initiate and maintain regular mammography screening (Hur, Kim, & Park,
2005; Rauscher, Hawley, & Earp, 2005). There were no signicant differences
in the con scores among age groups. Women between the ages of 30 and 34,
however, had the lowest pro scores. The benets of mammography should
be stressed when educating this age group.
As expected, women in the maintenance stage perceived fewer barriers
and more benets to mammography, and there was an association between
pros and cons and stage of change of mammography supporting previous
studies (Chamot et al., 2001; Lee, 2003; Otero-Sabogal et al., 2006). In
samples of Swiss women (Chamot et al., 2001), Korean women (Lee,
2003), and Filipino, Latino, African American, Chinese, and White women
(Otero-Sabogal et al., 2006), the pros were signicantly associated with stage
of adoption. In addition, positive mammography attitudes were strongly
associated with initiation of mammography among rural American women
(Rauscher et al., 2005), and perceived benets was one of the predictors of
stage of mammography adoption among rural Korean women (Hur, Kim, &
Park, 2005). Based on this study nding and those from previous studies, the
160 H. S. Kang et al.
pros of mammography appear to be a common factor associated with stage
of mammography adoption across cultures. These results show that one
strategy to increase mammography adoption is to improve attitudes toward
mammography, and women can benet from an education intervention to
raise awareness of benets of mammography.
Only the maintenance stage was differentiated from the precontem-
plation stage in this study, however, in contrast to ndings in previous
studies (Chamot et al., 2001). This may owe to differences in populations
or small samples. The proscons crossover was closer to the contemplation
stage, supporting a previous study of 909 Swiss women aged 40 to 80 years
(Chamot et al., 2001). But it was different from that of previous studies of
women in the United States, which showed crossover just before the action
stage (Prochaska, Velicer, et al., 1994). These discrepancies could be due to
differences in populations. This nding, however, supports that the crossover
always happened prior to the action stage (Prochaska, Velicer, et al., 1994).
More studies across various populations and a repeated study with Korean
women are needed.
Prochaska (1994) named approximately a 10 T-point (approximately
1.0 SD) increase in pros for progressing from the precontemplation stage
to the action stage as a strong principle and a 0.5-SD decrease in cons
for progressing from the precontemplation stage to the action stage as
a weak principle. Interestingly, the magnitude of the difference from
precontemplation to action in this study was 6.3 T points (0.63 SD) for
pros and 7.4 T points (0.74 SD) for cons. Results of this study partially
supported Prochaskas strong and weak principles of change. This result is
more consistent with the weak principle of change, although the magnitude
of decrease in cons is somewhat higher than predicted by the weak principal
of change. Further replication studies would be helpful.
Participants mentioned several barriers that prevented them from having
mammography exams. The most common reason was that they believed
that without any obvious signs or symptoms, a breast exam is not required.
This nding is consistent with previous reports that women who do not
experience breast symptoms are less likely to receive mammograms (Im et
al., 2004; Ogedegbe et al., 2005; Sabatino, Burns, Davis, Phillips, & McCarthy,
2006). It is important to educate women that the early stages of breast cancer
may preclude signs and symptoms and to emphasize that mammography can
detect cancer that is not yet palpable.
Cost was also one of the barriers identied by participants, supporting
previous ndings (Ko, Sadler, Ryujin, & Dong, 2003; McAlearney, Reeves,
Tatum, & Paskett, 2005; Sabatino et al., 2006). At the time the data for
this study were collected, women had to pay 50% of each mammography
exam. The cost for mammograms was lowered to a 30% copayment
in 2006, however, and cancer screening for low-income women is free.
Even so, health care providers cannot ignore the fact that cost may be
Korean Womens Attitudes Toward Mammography 161
a major barrier for some women. In addition, sonograms, recommended
when mammography results are ambiguous, are not covered by health
insurance. Sonograms are relatively common among young Oriental women
because their breast tissue is dense. Efforts to lower screening costs or to
expand health insurance coverage for breast cancer screening is needed
to lower the economic burden and promote participation in screening.
Several participants stated that lack of time and information were barriers to
mammography. Philippine women also considered lack of time as a barrier
(Ko et al., 2003). Many women work full time, and most Korean clinics
are open only during the week. Women who do not have time to make
an appointment during the week would benet from time made available
during lunch, evenings, or weekends.
Lack of knowledge is also a major barrier to breast cancer screening
(Guerra, Krumholz, & Shea, 2005; Ogedegbe et al., 2005). October is
national breast cancer awareness month in Korea, as well as in many
Western countries. Many free public educational programs are offered,
and events such as a fund-raising marathon, free mobile mammography
examinations, and pink ribbon festivals are held to raise breast cancer
awareness. Even though these campaigns are helpful, some women who
need regular screening are not being reached. Thus, more efforts are required
to disseminate information about the importance of early breast cancer
screening.
Previous studies have reported that many women are not comfortable
exposing their breasts to or being touched by male technicians during
mammography exams (Im, Lee, & Park, 2002; Ogedegbe et al., 2005; Poulos
& Llewellyn, 2005; Sharp et al., 2003). Arrangements should be made to
have more female technicians to support women who are reluctant to have
their mammography exams conducted by males. Discomfort and pain during
mammography also can prevent women from returning for follow-up or
future exams (Ogedegbe et al., 2005; Sabatino et al., 2006; Sharp et al., 2003).
It is important to train technicians to be gentle and sensitive to womens
feelings. Fear about x-ray and test results is another barrier identied in
the literature and supported by this studys results. Our ndings support
a previous study that found that women fear exposure to x-rays as well
as the chance of nding cancer (Thompson, Montano, Mahloch, Mullen, &
Taylor, 1997). When educating women, the effects of the x-rays used in
mammography should be clearly explained.
One limitation of this study is that it was restricted to a convenience
sample of a small number of women, and results do not necessarily apply
to women in the broader Korean population. We also did not differentiate
between high- and low-risk groups. In spite of these limitations, this study
provides useful information for developing strategies to provide appropriate
screening intervention, patient education, breast cancer screening behavior
counseling, and changes in Korean health policy.
162 H. S. Kang et al.
CONCLUSIONS
The majority of participants in this study did not receive regular breast cancer
screening, which supports the need to promote breast cancer awareness
among Korean women. Breast cancer screening can be encouraged by
emphasizing the benets of regular screening and decreasing the barriers.
The results of this study support the literature in regard to barriers
that prevent Korean women from following the recommended guidelines
for mammography. A salient issue regarding whether to have regular
mammograms is the value of early detection. Thus, it is important to
raise awareness of regular breast cancer screening, decrease the barriers
that prevent women from having mammograms, and reach out to women
who are in need of more education and assistance with payment for this
screening procedure. Disseminating information more assertively through
mass media, such as television, radio, newspapers, magazines, the Internet,
and mobile phones, is one way to raise awareness of important health
concerns. Lowering the cost of screening and using more women clinicians
or technicians also would be helpful to women who prefer them. Strategies to
promote screening would be more effective if cultural beliefs toward breast
cancer and screening were considered. Additional studies with larger samples
need to be conducted to explore barriers that prevent Korean women from
having CBE and mammography, particularly among women aged 40 years
and older.
The results of this study provide additional support for constructs of
the transtheoretical model of behavior change as they apply to screening
mammography. The results of this study indicate that nurses should keep
in mind that there are various barriers to mammography screening when
promoting mammography and educating clients about its benets; the
educational material should include information on barriers. Findings also
indicate that efforts at different levels, both personal and intrapersonal,
should be made to promote breast cancer screening.
REFERENCES
Ahn, S., Yoo, K. Y., & Korean Breast Cancer Society, (2006). Chronological changes
of clinical characteristics in 31115 new breast cancer patients among Koreans
during 19962004. Breast Cancer Research and Treatment, 99(2), 209214.
American Cancer Society. (2001). Breast cancer facts & gures
20012002. Retrieved November 10, 2006, from http://www.cancer.org/
docroot/STT/content/STT 1x Breast Cancer Facts and Figures 20012002.asp
Bouchardy, C., Morabia, A., Verkooijen, H. M., Fioretta, G., Wespi, Y., & Schafer, P.
(2006). Remarkable change in age-specic breast cancer incidence in the Swiss
canton of Geneva and its possible relation with the use of hormone replacement
therapy. BMC Cancer, 6, 78.
Korean Womens Attitudes Toward Mammography 163
Chamot, E., Charvet, A. I., & Perneger, T. V. (2001). Predicting stages of adoption of
mammography screening in a general population. European Journal of Cancer,
37, 18691877.
Choi, J., Kim, Y. J., Shin, H. R., Noh, D. Y., & Yoo, K. Y. (2005). Long-term prediction
of female breast cancer mortality in Korea. Asian-Pacic Journal of Cancer
Prevention, 6(1), 1621.
Guerra, C. E., Krumholz, M., & Shea, J. A. (2005). Literacy and knowledge,
attitudes and behavior about mammography in Latinas. Journal Health Care
Poor Underserved, 16(1), 152166.
Hur, H. K., Kim, G. Y., & Park, S. M. (2005). Predictors of mammography participation
among rural Korean women age 40 and over. Taehan Kanho Hakhoe Chi, 35(8),
14431450.
Im, E., Lee, E. O., & Park, Y. S. (2002). Korean womens breast cancer experience.
Western Journal of Nursing Research, 24(7), 751771.
Im, E., Park, Y. S., Lee, E. O., & Yun, S. N. (2004). Korean womens attitudes toward
breast cancer screening tests. International Journal of Nursing Studies, 41(6),
583589.
Ko, C., Sadler, G., Ryujin, L., & Dong, A. (2003). Filipina American womens
breast cancer knowledge, attitudes, and screening behaviors. Public Health,
3(1), 2732.
Korea National Institute of Health. (2005). Health People 2010. Seoul: Authors.
Lee, Y. J. (2003). Predicting factors corresponding to the stage of adoption
for mammography based on transtheoretical model. Unpublished doctoral
dissertation, Yonsei University, Seoul, Korea.
Lee, E. E., Fogg, L. F., & Sadler, G. R. (2006). Factors of breast cancer screening
among Korean immigrants in the United States. J Immigr Minor Health, 8(3),
223233.
McAlearney, A. S., Reeves, K. W., Tatum, C., & Paskett, E. D. (2005). Perceptions
of insurance coverage for screening mammography among women in need of
screening. Cancer, 103(12), 24732480.
National Cancer Center. (2006). Cancer information (2nd ed.). Goyangsi: Korea
National Cancer Center.
Ogedegbe, G., Cassells, A. N., Robinson, C. M., Duhamel, K., Tobin, J. N., Sox, C.
H., et al. (2005). Perceptions of barriers and facilitators of cancer early detection
among low-income minority women in community health centers. Journal of
the National Medical Association, 97(2), 162170.
Otero-Sabogal, R., Stewart, S., Shema, S. J., & Pasick, R. J. (2006). Ethnic differences
in decisional balance and stages of mammography adoption. Health Education
& Behavior,. [Serial online]. August 4, 2006; doi:10.1177/1090198105277854
Poulos, A., & Llewellyn, G. (2005). Mammography discomfort: A holistic perspective
derived from womens experiences. Radiography, 11, 1725.
Prochaska, J. O. (1994). Strong and weak principles for progressing from precontem-
plation to action on the basis of twelve problem behaviors. Health Psychology,
13(1), 4751.
Prochaska, J. O., Norcross, J. C., & DiClemente, C. C. (1994). Changing for good.
New York: William Morrow.
164 H. S. Kang et al.
Prochaska, J., Velicer, W., Rossi, J., Goldstein, M., Marcus, B., Rakowski, W., et
al. (1994). Stages of change and decisional balance for 12 problem behaviors.
Health Psychology, 13(1), 3946.
Rakowski, W., Clark, M. A., Pearlman, D. N., Ehrich, B., Rimer, B. K., Goldstein, M.
G., et al. (1997). Integrating pros and cons for mammography and Pap testing:
Extending the construct of decisional balance to two behaviors. Preventive
Medicine, 26(5), 664673.
Rauscher, G. H., Hawley, S. T., & Earp, J. L. (2005). Baseline predictors of initiation
vs. maintenance of regular mammography use among rural women. Preventive
Medicine, 40, 822830.
Sabatino, S., Burns, R., Davis, R., Phillips, R., & McCarthy, E. (2006). Breast cancer risk
and provider recommendation for mammography among recently unscreened
women in the United States. Journal of General Internal Medicine, 21, 285291.
Sharp, P., Michielutte, R., Freimanis, R., Cunningham, L., Spangler, J., & Burnette,
V. (2003). Reported pain following mammography screening. Archives Internal
Medicine, 163(7), 833836.
Smigal, C., Jemal, A., Ward, E., Cokkinides, V., Smith, R., Howe, H., et al. (2006).
Trends in breast cancer by race and ethnicity: Update 2006. CA: A Cancer
Journal of Clinicians, 56, 168183.
Smith, A. A., Saslow, D., Sawyer, K. A., Burke, A., Burke, W., Costanza, M. E., et al.
(2003). American Cancer Society guidelines for breast cancer screening: Update
2003. CA: A Cancer Journal of Clinicians, 53, 141169.
Spencer, L., Pagell, F., & Adams, T. (2005). Applying the transtheoretical model to
cancer screening behavior. Ame J Health Behavior, 29, 3656.
Sung, N., Park, E., Shin, H., & Choi, K. (2005). Participation rate and related socio-
demographic factors in the national cancer screening program. J Prev Med Public
Health, 38(1), 93100.
Thomas, E. C. (2004). African American womens breast memories, cancer beliefs,
and screening behaviors. Cancer Nursing, 27(4), 295302.
Thompson, B., Montano, D., Mahloch, J., Mullen, M., & Taylor, V. (1997). Attitudes
and beliefs toward mammography among women using an urban public
hospital. Journal of Health Care Poor Underserved, 8(2), 186201.
Tu, S., Yasui, Y., Kuniyuki, A., Schwartz, S., Jackson, J., & Taylor, V. (2002). Breast
cancer screening: Stages of adoption among Cambodian American women.
Cancer Detection and Prevention, 26, 3341.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Persistent Fear and Anxiety Can Affect Young Childrens Learning and Development PDFDocument16 pagesPersistent Fear and Anxiety Can Affect Young Childrens Learning and Development PDFCristina AlexeevPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Emergency Severity IndexDocument114 pagesEmergency Severity Indexpafin100% (3)
- Voice Production in Singing and SpeakingBased On Scientific Principles (Fourth Edition, Revised and Enlarged) by Mills, Wesley, 1847-1915Document165 pagesVoice Production in Singing and SpeakingBased On Scientific Principles (Fourth Edition, Revised and Enlarged) by Mills, Wesley, 1847-1915Gutenberg.org100% (3)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Manage Odontogenic Infections Stages Severity AntibioticsDocument50 pagesManage Odontogenic Infections Stages Severity AntibioticsBunga Erlita RosaliaPas encore d'évaluation
- Ongoing Pediatric Health Care For The Child Who Has Been MaltreatedDocument18 pagesOngoing Pediatric Health Care For The Child Who Has Been MaltreatedJesse M. MassiePas encore d'évaluation
- Antenatal & Postnatal Care: 1. General InformationDocument7 pagesAntenatal & Postnatal Care: 1. General InformationanishnithaPas encore d'évaluation
- Vroom Tips: Brain Building BasicsDocument7 pagesVroom Tips: Brain Building BasicsJesse M. MassiePas encore d'évaluation
- Fundamentals of Tooth Preparation Periodontal AspectsDocument74 pagesFundamentals of Tooth Preparation Periodontal AspectsVica Vitu100% (3)
- 3.mechanical VentilationDocument33 pages3.mechanical Ventilationisapatrick8126Pas encore d'évaluation
- Narrative Report On School Nursing - EditedDocument16 pagesNarrative Report On School Nursing - EditedAbby_Cacho_9151100% (2)
- Ozone Therapy in DentistryDocument16 pagesOzone Therapy in Dentistryshreya das100% (1)
- UrinalysisDocument43 pagesUrinalysisJames Knowell75% (4)
- Clinical Evoked PotentialsDocument13 pagesClinical Evoked PotentialsHerminaElenaPas encore d'évaluation
- Growth Chart IDocument1 pageGrowth Chart IJesse M. MassiePas encore d'évaluation
- Placement Changes and Emergency Department Visits in The First Year of Foster CareDocument9 pagesPlacement Changes and Emergency Department Visits in The First Year of Foster CareJesse M. MassiePas encore d'évaluation
- Effective Discipline To Raise Healthy Children: Policy StatementDocument12 pagesEffective Discipline To Raise Healthy Children: Policy StatementJesse M. MassiePas encore d'évaluation
- Status EpileticusDocument2 pagesStatus EpileticusJesse M. MassiePas encore d'évaluation
- Oral and Dental Aspects of Child Abuse and Neglect: Clinical ReportDocument10 pagesOral and Dental Aspects of Child Abuse and Neglect: Clinical ReportJesse M. MassiePas encore d'évaluation
- Identifying Child Abuse Fatalities During Infancy: Clinical ReportDocument11 pagesIdentifying Child Abuse Fatalities During Infancy: Clinical ReportJesse M. MassiePas encore d'évaluation
- Clinical Considerations Related To The Behavioral Manifestations of Child MaltreatmentDocument15 pagesClinical Considerations Related To The Behavioral Manifestations of Child MaltreatmentJesse M. MassiePas encore d'évaluation
- Making The Most of Mentors: A Guide For MenteesDocument5 pagesMaking The Most of Mentors: A Guide For MenteesJesse M. MassiePas encore d'évaluation
- IJMEDocument7 pagesIJMEJesse M. MassiePas encore d'évaluation
- Ckeck List Operacional - Usda Inst Saude e SegDocument3 pagesCkeck List Operacional - Usda Inst Saude e SegQualidade CooperalfaPas encore d'évaluation
- Difficult Patient Encounters: Assessing Pediatric Residents' Communication Skills Training NeedsDocument19 pagesDifficult Patient Encounters: Assessing Pediatric Residents' Communication Skills Training NeedsJesse M. MassiePas encore d'évaluation
- i-PASS OBSERVATION TOOLDocument1 pagei-PASS OBSERVATION TOOLJesse M. MassiePas encore d'évaluation
- Jpeds Aom 208Document3 pagesJpeds Aom 208Jesse M. MassiePas encore d'évaluation
- Cbig Cross-ReportingDocument25 pagesCbig Cross-ReportingJesse M. MassiePas encore d'évaluation
- Suidi Oklahoma ProviderDocument28 pagesSuidi Oklahoma ProviderJesse M. MassiePas encore d'évaluation
- SB773Document257 pagesSB773Jesse M. MassiePas encore d'évaluation
- What Is Child Abuse and Neglect? Recognizing The Signs and SymptomsDocument8 pagesWhat Is Child Abuse and Neglect? Recognizing The Signs and SymptomsJesse M. MassiePas encore d'évaluation
- Vroom Tips: Brain Building BasicsDocument16 pagesVroom Tips: Brain Building BasicsJesse M. MassiePas encore d'évaluation
- dBA PROTECT YOUR HEARINGDocument4 pagesdBA PROTECT YOUR HEARINGJesse M. MassiePas encore d'évaluation
- 2018 OdhhsDocument124 pages2018 OdhhsJesse M. MassiePas encore d'évaluation
- Child Abuse Neglect Prevention OklahomaDocument44 pagesChild Abuse Neglect Prevention OklahomaJesse M. MassiePas encore d'évaluation
- Preventing Adverse Childhood Experiences (Aces) :: Leveraging The Best Available EvidenceDocument40 pagesPreventing Adverse Childhood Experiences (Aces) :: Leveraging The Best Available EvidenceJesse M. MassiePas encore d'évaluation
- Recommendations For Preventive Pediatric Health Care: Bright Futures/American Academy of PediatricsDocument2 pagesRecommendations For Preventive Pediatric Health Care: Bright Futures/American Academy of PediatricsJesse M. MassiePas encore d'évaluation
- Domestic Violence Oklahoma 2017Document44 pagesDomestic Violence Oklahoma 2017Jesse M. MassiePas encore d'évaluation
- COVID Positive/PUI: PAPR Prioritization MatrixDocument1 pageCOVID Positive/PUI: PAPR Prioritization MatrixJesse M. MassiePas encore d'évaluation
- Intimate Partner Violence, Sexual Violence, Stalking: Before The Age of 18Document1 pageIntimate Partner Violence, Sexual Violence, Stalking: Before The Age of 18Jesse M. MassiePas encore d'évaluation
- Life Calling Map Fillable FormDocument2 pagesLife Calling Map Fillable Formapi-300853489Pas encore d'évaluation
- Concrete MSDS 1 PDFDocument5 pagesConcrete MSDS 1 PDFmanil_5100% (1)
- Radial Club Hand TreatmentDocument4 pagesRadial Club Hand TreatmentAshu AshPas encore d'évaluation
- MMMM 3333Document0 pageMMMM 3333Rio ZianraPas encore d'évaluation
- Maxillofacial Privileges QGHDocument4 pagesMaxillofacial Privileges QGHSanam FaheemPas encore d'évaluation
- CapstoneDocument40 pagesCapstoneDevanshi GoswamiPas encore d'évaluation
- A Novel Visual Clue For The Diagnosis of Hypertrophic Lichen PlanusDocument1 pageA Novel Visual Clue For The Diagnosis of Hypertrophic Lichen Planus600WPMPOPas encore d'évaluation
- HouseflyDocument16 pagesHouseflyRitu Puri50% (2)
- Proctor Tobacco History Report Canadian Trial Rapport - Expert - ProctorDocument112 pagesProctor Tobacco History Report Canadian Trial Rapport - Expert - Proctorkirk_hartley_1Pas encore d'évaluation
- Reverse Optic Capture of The SingleDocument10 pagesReverse Optic Capture of The SingleIfaamaninaPas encore d'évaluation
- Bagian AwalDocument17 pagesBagian AwalCitra Monalisa LaoliPas encore d'évaluation
- Lecture 16-17 - Opioids AnalgesicsDocument20 pagesLecture 16-17 - Opioids AnalgesicsJedoPas encore d'évaluation
- Resume Massage Therapist NtewDocument2 pagesResume Massage Therapist NtewPartheebanPas encore d'évaluation
- MedAspectsBio PDFDocument633 pagesMedAspectsBio PDFDuy PhúcPas encore d'évaluation
- 2014 Windsor University Commencement Ceremony PROOFDocument28 pages2014 Windsor University Commencement Ceremony PROOFKeidren LewiPas encore d'évaluation
- WHO 1991 128 PagesDocument136 pagesWHO 1991 128 PagesLilmariusPas encore d'évaluation
- Bradford Assay To Detect Melamine ConcentrationsDocument3 pagesBradford Assay To Detect Melamine ConcentrationsVibhav SinghPas encore d'évaluation
- Dance BenefitsDocument9 pagesDance Benefitsapi-253454922Pas encore d'évaluation
- Patch ClampDocument4 pagesPatch ClampXael GarciaPas encore d'évaluation
- Dengulata KosamDocument3 pagesDengulata KosamChina SaidaPas encore d'évaluation
- Rangkuman by Yulia VionitaDocument21 pagesRangkuman by Yulia VionitaRizqi AkbarPas encore d'évaluation