Académique Documents
Professionnel Documents
Culture Documents
SFMUN Medical Aid Backgrounder
Transféré par
AnnaLuxeCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
SFMUN Medical Aid Backgrounder
Transféré par
AnnaLuxeDroits d'auteur :
Formats disponibles
Introduction
The Social, Humanitarian and Cultural Committee (SOCHUM) is one of the most
important and contentious bodies within the United Nations. One of the founding
missions of the United Nations is the universal protection of human rights, and
SOCHUM is the committee of the General Assembly where discussions of human rights
issues take place. SOCHUMs mandate also covers a number of other social,
humanitarian, and cultural topics from discrimination to drug control. The range of
problems debated in the Social, Humanitarian and Cultural Committee ensures conflict
between UN member nations, but the success of the body has been in bridging these
differences to solve some of the worlds greatest challenges.
At SFMUN 2014, we as SOCHUM will be immersed in discussing the medical
conditions in low-income, low-resource global markets. Indeed, many of the medical
problems that have been already solved in first world countries are still the reason behind
the daily death of hundreds of people in other parts of the world. This is primarily
because low-income, low- resource markets cannot afford the production or sustainability
of advanced research and medical device design. With all the advancements that we have
accomplished during the past few decades, it is no longer acceptable to stay silent and
watch people die because of inadequate medical conditions. It is time to bring this topic
up to the attention of the international community. We will discuss direct and indirect
causes leading to these circumstances, as well as effective methods to approach them
internationally. This topic will force the committee to come up with creative solutions to
one of the worlds most pressing problems, and delegates in the Social, Humanitarian and
Cultural Committee of the General Assembly should address this humanitarian situation
and resolve it permanently!
Overview
As we enter 2014, we approach the Millennium Development Goals deadline of 2015.
The eight Millennium Development Goals (MDGs) which range from halving extreme
poverty to halting the spread of HIV/AIDS and providing universal primary education, by
the target date of 2015 form a blueprint agreed to by all the worlds countries and all
the worlds leading development institutions.
Two of the eight MDGs are strictly
concerned with healthcare: reducing child mortality and improving maternal health.
Notably, a lot has been done when it comes to these two specific areas, but looking at the
numbers of children dying upon birth or the conditions that mothers have to endure
during and after their pregnancy will prove shocking to any observer. Despite population
growth, the number of deaths in children under five worldwide declined from 12.4
million in 1990 to 6.9 million in 2011, which translates into about 14,000 fewer children
dying each day.
However, despite determined global progress in reducing child deaths, there is an
increasing proportion of child deaths in sub-Saharan Africa where one in nine children
die before the age of five and in Southern Asia where one in 16 die before age five.
Sadly, children born into poverty are almost twice as likely to die before the age of five
as those from wealthier families.
10
Similarly for maternal healthcare, maternal mortality
has nearly halved since 1990. An estimated 287,000 maternal deaths occurred in 2010
worldwide, a decline of 47 per cent from 1990. All regions have made progress but
accelerated interventions are required in order meet the target. Nonetheless, only half of
women in developing regions receive the recommended amount of healthcare they need.
Most of us are sheltered from this reality, allowing it to penetrate our daily lives through
momentary headline news briefs that we may bring up over coffee before we completely
forget about and move on to worry about more important things that are more relevant
to our daily lives such as filing our tax reports or studying for a history midterm.
However, many people have to worry about their lives and security every minute of every
day. Many mothers have to live with the risk of giving birth to a dead child whose
umbilical cord was wrapped around his/her neck and the closest primary health center
was 30 kilometers away, or having the baby choke from Meconium Aspiration, or losing
their child the morning following birth because of hypothermia. Many of us will live
without ever having to witness the birth of a dead baby straight from a mothers womb.
Many of us will never get closer to this reality than reading about it in the news.
However, when I saw a boy being born during summer 2013 in an overcrowded primary
health center in rural India, followed by seeing the mother and fathers happiness
immediately after birth, and then seeing them cry and scream as loud as they could a few
hours later upon the death of their son, I understood how sheltered from the truth I had
been.
The baby died simply because the nurse didnt check his temperature with a thermometer
when he was born, and hypothermia claimed his life shortly afterwards. A newborn baby
is homoeothermic, maintaining a constant and warm body temperature, but his ability to
stay warm may easily be overwhelmed by extremes of environmental temperatures. A
newborn is more prone to develop hypothermia because of large surface area per unit of
body weight. A low birth weight baby has decreased thermal insulation due to less
subcutaneous fat and reduced amount of brown fat. Brown fat is the site of heat
production. It is localized around the adrenal glands, kidneys, nape of neck and the inter-
scapular area and axillary region. Metabolism of brown fat results in heat production.
Blood flowing through the brown fat becomes warm and through circulation transfers
heat to other parts of the body. This mechanism of heat production is called non-
shivering thermogenesis.
12
Neonatal hypothermia often due to lack of attention by
healthcare providers continues to be a very important cause of neonatal deaths,
13
and this
was the reason behind the babys death.
Bear in mind that reducing child mortality and improving maternal health are two of the
eight MDGs, meaning that theyve been already getting a lot of attention from the
international community, and that the UN, state governments and NGOs have been
working on them really hard for the past 13 years. Still, what was just described still
happens. Now try to imagine other medical conditions that have not garnered the direct
attention of the international community because they are not recognized as MDGs at this
time. Think of malnutrition, eye care, cancer, dentistry and trauma. Think of a child
dying of polio because his vaccination records which essentially occupy the top half of
a paper while the bottom half comprises the vaccination record of a different child in a
massive folder which follows no system of archiving, not even alphabetical were lost
when the entire folder in which they were kept was misplaced, and it was assumed that he
had already gotten the polio vaccine to avoid paying for a second vaccine when he
originally never got one. Or think of a father getting bitten by a mosquito carrying dengue
virus and dying on the spot, leaving behind six children all under the age of 12 and a wife
to the streets. Think of a grandmother dying because the primary health center mixed up
her hypertension medication with macrolide antibiotics because of the lack of a proper
medication labeling system. Or think of a teenager dying because the insulin injections
that he is supposed to take were no longer active because he doesnt have a fridge to
refrigerate them and all he relies on is storing them in pottery kept in the shade and
cooled by running water. These are all cases I had only read about in newspapers or heard
of on TV. I unfortunately have to admit now that these cases are ones I personally
witnessed during summer 2013 while working in the field of medical healthcare in India.
It is time for the international community to wake up. It is time for us all to act. It doesnt
make sense that some people on Earth enjoy the perks of 3D printing, bullet trains and
outer space travel, while others living on the same planet die because of mosquito bites,
erroneous medication labeling, or the lack of a thermometer.
Relevant UN Actions
During the World Education Forum held in April 2000 in Dakar, UNESCO, UNICEF,
WHO, and the World Bank launched Focusing Resources on Effective School Health
(FRESH), an interagency initiative created in recognition of the need to improve holistic
rather than individual approaches to promote health and nutrition in schools. Instead
of implementing new programs and activities, FRESH seeks to accomplish this goal by
tailoring existing programs and activities so that they are more holistic. Specifically,
This interagency initiative has identified a core group of activities, each already
recommended by the participating agencies, that captures the best practices from program
experiences.
Though the ultimate goal of the initiative is to improve the quality and
equity of education worldwide, effective school health programs are essential to that end.
Proposed Solution
There can be no immediate solution to the medical problems of the developing countries.
Priorities are demanded, and it must be acknowledged that in allocation of medical
priorities certain compromises are required. It can be hoped that the least detrimental
compromises will be selected. Careful planning of health services and also of training
programs for various medical personnel must not rely on what exists in developed
countries, because those facilities and programs may be completely inappropriate to other
situation. At the same time as inroads are made into the preventable conditions that now
claim thousands of young lives, programs of birth control and improvement of
agricultural methods must be emphasized. The reduced morbidity including reporting
outcomes, budgets and supplies and mortality that results from immunization against
childhood infectious diseases, smallpox, and tuberculosis must be borne in mind in
overall planning for schools and general health services. Inexpensive and practical
programs that could be managed by medical personnel who are not highly trained should
be considered. As the benefits of technical development gradually reach the urbanizing
population living under poor social and hygienic conditions, changes in the disease
picture must be anticipated.
Those involved with planning and training must understand various cultural influences so
that the transition period can be made as painless as possible. Certain seemingly attractive
Western procedures should be guarded against if they are not practical. For instance, a
common tendency is to build large modern hospitals throughout the land with disregard
for the fact that these hospitals cannot possibly be staffed, equipped, or maintained
because of shortages of trained people and available funds. This has been called an
edifice complex and is unfortunately found in many developing regions, stimulated
often by ill-considered advice from overseas experts. At the same time as medical
services are being improved, it is extremely important to document the improvements by
means of carefully recorded statistics. Guidance in necessary methods for documentation
should be sought early in the development of medical care. Obviously it is vital to
determine what and where the major medical problems are so that programs will be
designed to attack them. Once the problems are sorted out, available resources can be
allocated and preventive measures and health education can be aimed at specific aspects
of public health. Many general statements have been made to describe the medical
problems in the developing countries of the world. There is a need to particularize the
problems and approach the specific manifestations of disease with knowledge of local
conditions and resources. Traditional solutions no longer apply in the field, and the
ultimate solution may be along lines that are completely unique and nontraditional. To
break the usual rules may be the only practical means to solve the problem at hand, and
modified common sense must often replace modern technology. The practical variations
on the general theme described here make medical work in developing countries
interesting, exciting, and rewarding.
Community health should be tackled in an integrated manner, where a variety of players
and a variety of measures work together based on the particular characteristics of the
community in question. In addition, rather than as a particular fixed goal to be achieved,
community-based health is better seen as a dynamically changing process involving
constant trial and error, all the while aiming for greater well being in peoples lives.
Community-based health is by no means simply a problem solving method. Provided that
people in developing countries and their supporters work as partners with local residents
and see problems through their eyes, and scientific analysis lies at the basis of any
ongoing and steady progress, little by little the people in communities can be mutually
empowered through even the smallest of achievements. While the progress achieved will
be incremental, community-based health can indeed be regarded as a means for gradually
bringing people closer to achieving wellbeing in their lives.
Question that should be discussed
Current Situation
How are developed countries affecting medical conditions in developing countries?
What are multilateral and international laws, treaties, agreements, and organizations
currently in place to regulate medical conditions in low-resource, low-income markets?
What are currently the greatest challenges to improving medical conditions in low-
resource, low-income markets?
Potential Solutions
How can the international community best collaborate to ameliorate medical conditions
in low-resource, low-income markets?
How can the international community make the roots causes of poor medical
conditions in low-resource, low-income markets priorities in frameworks for long-
term solutions?
What should the role of developed nations be in the improvement of medical
conditions in developing nations?
How can the multitude of international and non-governmental organizations addressing
problems of medical conditions be incorporated into designing and implementing
lasting solutions?
Bloc Positions
The three sets of players that are most important for the future of medical conditions in
low-income, low-resource global markets are state governments, non-governmental
organizations (NGOs) and research groups. All three players must work together to
ensure that measures to spread medical awareness and implement proper medical
practices are successful. Without the support of the medical research community, for
example, it is impossible to reach new affordable healthcare devices and procedures.
Without the involvement of NGOs, fair and equitable documentation and implementation
plans will lack the expertise to be effective. Finally, without the backing of governments,
NGOs will lack the funding required to enact these programs and will be powerless
against prevailing discriminatory attitudes. It is important to note that the involvement of
governments of both developed and developing countries is essential for this
collaboration to be a flourishing one. Thus, any solution to the problem of inadequate
medical conditions must involve collaboration among these three players.
To determine your countrys policy, you must first identify the role of your government
regarding this matter. Are you a developed country that has been able to support other
countries with poor medical conditions, or has your government sought assistance from
the international community to improve its healthcare? Based on that, you would be able
to identify the NGOs that your government primarily works with, and you would be able
to determine the relationship between these players. It is also important to determine any
and all private and public medical research groups in your country in order to be able to
understand how your country has been able to contribute to solving this predicament or
benefit from the international community.
Further research
As a starting point, I would encourage you to do some research on the problem of
inadequate medical conditions in general. WHO has a good overview of the topic, and
there are many NGOs primarily involved with medical conditions in low-income, low-
resource global markets that would provide enough information for you understand the
general problems faced and the steps being taken to approach them.
Secondly, the best way to gain a sense of the severity of the problem and to better
understand the issues involved is to research a number of different geographic regions
with looming medical problems. Each delegation will be required to write one case study
on one of these geographic regions detailing the problem observed, the solutions
attempted, the degree of their success and a corresponding interpretation. This will be
further clarified in the Position Paper Requirements section of this study guide.
Finally, I would encourage you to know the ins and outs of your countrys healthcare
system. How has it changed over the past decades? What problems did it face, if any, and
how did it approach them? How has it been cooperating with the international society?
With other countries in its same geographic region facing the same problems? With more
developed or less developed countries? What are your governments policies towards
working with national, regional and international NGOs? These are some of the questions
that you would want to consider when evaluating the completeness of your research.
In doing your research, feel free to refer to the CIA World Factbook and State
Department Information form the Bureau of Public Affairs to find fundamental
information on any country. You should also explore the UN website, as well as the
SOCHUM and WHO websites, and the UN Documentation Research Guide. It would be
very helpful to understand the evolving nature of the issue and to regularly check World
News, CNN, BBC, Reuters, Agence France Press, The New York Times, Los Angeles
Times, and any other world renowned news agency.
You can also access United Nations Publications at the following:
United Nations Official Document System (ODS): online access to full text
parliamentary documentation and Official Records of the United Nations since 1993.
These include resolutions and documentation for organ meetings.
AccessUN: index of UN documents and publications; full text documents available.
The UN Bibliographic Information System (unbisnet.un.org) has meeting transcripts,
voting records, and other documents that might prove helpful during your research.
Bibliography
Social, Humanitarian & Cultural Third Committee, 13 September 2011
<http://www.un.org/en/ga/third/index. shtml>.
2
M. J. Peterson. <br />The General Assembly in World Politics<br />. Boston: Allen &
Unwin, 1986. Print.
3
M. J. Peterson. <br />The General Assembly in World Politics<br />. Boston: Allen &
Unwin, 1986. Print.
4
Evan Luard. <br />The United Nations: How It Works and What it does <br />. London:
Macmilliam, 1994. Print.
5
Evan Luard. <br />The United Nations: How It Works and What it does <br />. London:
Macmilliam, 1994. Print.
6
Sydney Bailey. <br />The General Assembly of the United Nations: A Study of Procedure and
Practice<br />. Westport: Greenwood Press, Inc., 1964. Print.
7
Arieh Eilan. <br />The General Assembly: Can It Be Salvaged? . Washington DC: The
Heritage Foundation, 1984. Print.
8
Millennium Development Goals and Beyond 2015 , UN Web Services Section, Department of
Public Information <http://www.un.org/millenniumgoals/>.
9
Goal 4: Reduce Child Mortality, UN Web Services Section, Department of Public Information
<http://www. un.org/millenniumgoals/childhealth.shtml>.
10
Goal 4: Reduce Child Mortality, UN Web Services Section, Department of Public Information
<http://www. un.org/millenniumgoals/childhealth.shtml>.
11
Goal 5: Improve Maternal Health, UN Web Services Section, Department of Public
Information <http://www. un.org/millenniumgoals/maternal.shtml>.
12
World Health Organization, Maternal and Newborn Health/Safe Motherhood. Thermal
Protection of The Newborn: A Practical Guide. WHO reference number: WS 420 97TH
(English) ed. Geneva: World Health Organization, UN, 1997. Print.
13
World Health Organization. Maternal Health and Safe Motherhood Programme Meeting of
Technical Working Group on Thermal Control of the Newborn. Thermal Control of The
Newborn : A Practical Guide. WHO/ FHE/MSM/93.2 ed. Geneva, Switzerland: World Health
Organization, UN, 1993. Print.
14
Atul Gawande. Slow Ideas. The New Yorker (Jul 29, 2013) Print.
15
Henry Jacob Bigelow. Insensibility During Surgical Operations Produced By Inhalation.
The Boston Medical and Surgical Journal XXXV.XXXIX (November 18, 1846) Print.
16
Henry Jacob Bigelow. Insensibility During Surgical Operations Produced By Inhalation.
The Boston Medical and Surgical Journal XXXV.XXXIX (November 18, 1846) Print.
17
Henry Jacob Bigelow. Insensibility During Surgical Operations Produced By Inhalation.
The Boston Medical and Surgical Journal XXXV.XXXIX (November 18, 1846) Print.
18
Francis Boott. Surgical Operations Performed During Insensibility Produced By The
Inhalation Of Sulfuric Ether. The Lancet: A Journal of British and Foreign Medical and
Chemical Science, Criticism, Literature and News Volume I.MDCCCXLVII (1846) Print.
19
Henry Jacob Bigelow. Surgical Anaethesia: Addresses and Other Papers . Boston: Boston:
Little, Brown, and Company, 1894. Print.
20
Henry Jacob Bigelow. Surgical Anaethesia: Addresses and Other Papers . Boston: Boston:
Little, Brown, and Company, 1894. Print.
21
Gawande.
22
Victor Robinson. The Story of Medicine. New York:
Kessinger Publishing, August 1943. Print.
23
John Bankston. Joseph Lister and the Story of Antiseptics (Uncharted, Unexplored, and
Unexplained). Mitchell Lane Publishers, 2004. Print.
24
Frederick Cartwright. Joseph Lister: the man who made surgery safe <br />. London:
Weidenfeld & Nicolson, 1963. Print.
25
Bankston.
26
Anne Crowther and Marguerite Dupree. Medical lives in the age of surgical revolution <br />.
Cambridge University Press, 2007. Print.
27
Fu Kuo-Tai Louis. Great Names in the History of Orthopaedics XIV: Joseph Lister (1827-
1912) Part 2. Journal of Orthopaedics, Traua and Rehabilitation 15 (2011) Print.
28
Cartwright.
29
Elie Metchnikoff. The Founders of Modern Medicine: Pasteur, Koch, Lister<br />. Freeport
(NY): Books for Libraries Press, 1939. Print.
30
Robinson.
31
J. M. T. Finney. A Surgeons Life: The Autobiography of J. M. T. Finney. New York: G.P.
Putnams Sons, 1940. Print.
32
Christopher Lawrence and Richard Dixey. Practising on principle: Joseph Lister and the germ
theories of disease <br />. Ed. Christopher Lawrence. London: Routledge, 1993. Print.
33
Atul Gawande. Better : A Surgeons Notes on Performance . New York: Metropolitan Books,
2007. Print.
Vous aimerez peut-être aussi
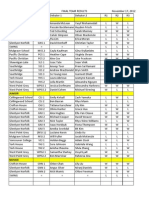
- Newman FISA ResultsDocument6 pagesNewman FISA ResultsAnnaLuxePas encore d'évaluation
- SH Tournament InviteDocument2 pagesSH Tournament InviteAnnaLuxePas encore d'évaluation
- UVIC 2013 Speaker ScoresDocument6 pagesUVIC 2013 Speaker ScoresAnnaLuxePas encore d'évaluation
- Basic CNDF GuideDocument2 pagesBasic CNDF GuideAnnaLuxePas encore d'évaluation
- Dsabc Tabs Individual Results Junior DivisionDocument8 pagesDsabc Tabs Individual Results Junior DivisionAnnaLuxePas encore d'évaluation
- UVIC Invitational Jr. TeamDocument3 pagesUVIC Invitational Jr. TeamAnnaLuxePas encore d'évaluation
- Mock Trial OutlineDocument10 pagesMock Trial OutlineAnnaLuxePas encore d'évaluation
- AP Exam Past Exam PaperDocument3 pagesAP Exam Past Exam PaperAnnaLuxePas encore d'évaluation
- AP Exam Past Exam PaperDocument3 pagesAP Exam Past Exam PaperAnnaLuxePas encore d'évaluation
- AP Exam Past Exam PaperDocument3 pagesAP Exam Past Exam PaperAnnaLuxePas encore d'évaluation
- IB English Commentary InstructionsDocument4 pagesIB English Commentary InstructionsAnnaLuxePas encore d'évaluation
- AP Exam Past Exam PaperDocument312 pagesAP Exam Past Exam PaperAnnaLuxe100% (3)
- AP Comparative Government FRQsDocument5 pagesAP Comparative Government FRQsAnnaLuxePas encore d'évaluation
- AP Comparative Government and Politics 2011 Free-Response QuestionsDocument3 pagesAP Comparative Government and Politics 2011 Free-Response QuestionsAnnaLuxePas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Neighborhood InvestigationDocument4 pagesNeighborhood Investigationapi-302394994Pas encore d'évaluation
- "Truth, Excellence, Service": Historical Review, 114 (2), 279-306Document5 pages"Truth, Excellence, Service": Historical Review, 114 (2), 279-306Chen Adrien Z. ThorPas encore d'évaluation
- 1Document54 pages1Maria Francessa AbatPas encore d'évaluation
- Appl TranscriptsDocument3 pagesAppl Transcriptssriram_parthaPas encore d'évaluation
- Method and Media Health EducationDocument10 pagesMethod and Media Health EducationAshok Mishra100% (2)
- Outline of Rizal's Life 2Document73 pagesOutline of Rizal's Life 2Reyji Edduba100% (1)
- BSC Comp SC - CBCSS Syllabus PDFDocument42 pagesBSC Comp SC - CBCSS Syllabus PDFSooraj krishnan v.sPas encore d'évaluation
- National Policy On Education (NPE 1986)Document11 pagesNational Policy On Education (NPE 1986)deepak kumarPas encore d'évaluation
- Edf1304 Assignment 1 Part 1 - Emily Greenberg - 26005123 1Document5 pagesEdf1304 Assignment 1 Part 1 - Emily Greenberg - 26005123 1api-285104874Pas encore d'évaluation
- Activity 1Document4 pagesActivity 1Joy Kimberly PaglinawanPas encore d'évaluation
- Predictors of Board Exam Performance of The Dhvtsu College of Education GraduatesDocument4 pagesPredictors of Board Exam Performance of The Dhvtsu College of Education Graduates15-0001Pas encore d'évaluation
- What Is Reflection and Reflective WritingDocument3 pagesWhat Is Reflection and Reflective WritingR-wah LarounettePas encore d'évaluation
- Betty Final Draft Assignment 2 - 04Document13 pagesBetty Final Draft Assignment 2 - 04Sei ChanPas encore d'évaluation
- Internship ReportDocument17 pagesInternship ReportDavidChenPas encore d'évaluation
- Neelima K VDocument3 pagesNeelima K Vneelima kommiPas encore d'évaluation
- 04 Expressing Satisfaction & Dissatisfaction - ExerciseDocument2 pages04 Expressing Satisfaction & Dissatisfaction - ExerciseMarcello AntonyPas encore d'évaluation
- Upside Down Art - MichelangeloDocument3 pagesUpside Down Art - Michelangeloapi-374986286100% (1)
- Strategic Negotiation and Deal MakingDocument7 pagesStrategic Negotiation and Deal MakingRohanPas encore d'évaluation
- CBM IndexDocument8 pagesCBM IndexSaili SarmalkarPas encore d'évaluation
- Australian Universities 2013Document25 pagesAustralian Universities 2013L Liew Tuck OnnPas encore d'évaluation
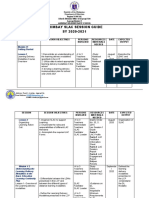
- Supervisory Plan: School ID: 501222 Poonbato IS 09455370326 501222pis@deped - Gov.phDocument2 pagesSupervisory Plan: School ID: 501222 Poonbato IS 09455370326 501222pis@deped - Gov.phBryan JesterPas encore d'évaluation
- Nursing Theory-Patient-Centered Approaches To Nurses.Document10 pagesNursing Theory-Patient-Centered Approaches To Nurses.Bheru LalPas encore d'évaluation
- SED 1FIL-10 Panimulang Linggwistika (FIL 102)Document10 pagesSED 1FIL-10 Panimulang Linggwistika (FIL 102)BUEN, WENCESLAO, JR. JASMINPas encore d'évaluation
- North East Frontier Railway Recruitment 2013 Group D Posts 1230 VacancyDocument3 pagesNorth East Frontier Railway Recruitment 2013 Group D Posts 1230 VacancymalaarunPas encore d'évaluation
- Appendix I Faculty Evaluation System General InformationDocument11 pagesAppendix I Faculty Evaluation System General InformationDani PhilipPas encore d'évaluation
- Arimbay Slac Session Guide SY 2020-2021Document6 pagesArimbay Slac Session Guide SY 2020-2021Jen ApinadoPas encore d'évaluation
- FS2 Le18Document1 pageFS2 Le18Jorebell W. QuiminoPas encore d'évaluation
- Handbook of Social MedicineDocument577 pagesHandbook of Social MedicineTaufiq AsrulPas encore d'évaluation
- James Cameron: Early LifeDocument7 pagesJames Cameron: Early Lifeproacad writersPas encore d'évaluation
- UT Dallas Syllabus For Stat1342.501.11s Taught by Yuly Koshevnik (Yxk055000)Document7 pagesUT Dallas Syllabus For Stat1342.501.11s Taught by Yuly Koshevnik (Yxk055000)UT Dallas Provost's Technology GroupPas encore d'évaluation