Académique Documents
Professionnel Documents
Culture Documents
13 Ashwinee Etal
Transféré par
editorijmrhsCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
13 Ashwinee Etal
Transféré par
editorijmrhsDroits d'auteur :
Formats disponibles
851
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
International Journal of Medical Research
&
Health Sciences
www.ijmrhs.com Volume 3 Issue 4 Coden: IJMRHS Copyright @2014 ISSN: 2319-5886
Received: 11
th
July 2014 Revised: 5
th
Aug 2014 Accepted: 31
st
Aug 2014
Research article
A STUDY OF BREASTFEEDING AND COMPLEMENTARY FEEDING PRACTICES WITH
EMPHASIS ON MISCONCEPTIONS AMONGST THE WOMEN WITH UNDER TWO YEAR
CHILDREN IN RURAL AREA
Rahalkar Ashwinee A
1
, *Phalke Deepak B
2
, Phalke Vaishali D
3
1
Student, Final MBBS, Rural Medical College, Pravara Institute of Medical Sciences, Loni, Maharashtra, India
2,3
Professor, Department of Community Medicine, Pravara Institute of Medical Sciences, Loni, Maharashtra
*Corresponding author email: deephalke@yahoo.co.in
ABSTRACT
Context: Breastfeeding is one of the most important determinants of child survival, birth spacing, and the
prevention of childhood infections. The beneficial effects of breastfeeding depend on its initiation, duration, and
the age at which the breastfed child is weaned. The complementary feeding pattern also plays a very important
role in the growth and development of the child. Aims & objectives: To study breastfeeding and complementary
feeding practices adopted by women of Loni area. To study the socio-cultural factors influencing breastfeeding
and complementary feeding practices. Settings and Design: Descriptive cross sectional study Methods and
Material: 150 women fulfilling eligibility criteria were taken up for the study for duration of two months. A
detailed questionnaire was given to the mothers and results were analysed later on. Statistical analysis used: Chi
square test Results: In 4.6% cases prelacteal food was given. Colostrum was given in 90% cases, while in 10% it
was not given. Only 50.6% babies were breastfed within 1 hour, Complementary feeding was started after 6
months in 84% babies, before 6 months in 4% and 12% did not know when to start weaning. Majority (58%) said
no to breastfeeding when mother was ill while 56.5% women had no change in their diet after delivery. Mothers
educational status was associated with proper breastfeeding practices while parity and socioeconomic factors had
no significant impact. Conclusions: Most of the women adopted appropriate practices regarding breastfeeding
and complementary feeding, but still misconceptions were noted. Thus more awareness should be created
regarding this topic.
Keywords: Breast feeding, Complementary feeding, Sociocultural practices
INTRODUCTION
For almost all infants, breast milk remains the
simplest, healthiest, and least expensive food, which
fulfils their requirement
1.
Breastfeeding is one of the
most important determinants of child survival, birth
spacing, and the prevention of childhood infections.
Under any circumstances, breast milk is the ideal
food for the infant. Proper implementation of
recommendations regarding breastfeeding and
complementary feeding will respectively prevent
13% and 6% (total=19%) deaths in under 5 age
group
2
. A great asset in India is that on an average
Indian mother, although poor in nutritional status, has
a remarkable ability to breastfeed her infant for
prolonged periods, sometimes extending up to nearly
2 years and beyond. Longitudinal and cross sectional
studies indicate that poor Indian women secrete as
much as 400-600 ml of milk per day during the first
year
3
It has been well documented that breastfeeding has
many beneficial effects on the baby as well as the
DOI: 10.5958/2319-5886.2014.00013.7
852
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
mother. It has been observed that infants between 0-5
months who have not been breastfed have a seven-
fold and five-fold increased risks of death due to
diarrhoea and pneumonia, respectively, than infants
who have been exclusively breastfed. Also, non-
exclusive rather than exclusive breastfeeding results
in more than twofold increased risk of dying due to
pneumonia and diarrhoea with higher risk in 6-11
month old infants
1
The complementary feeding pattern also plays a very
important role in the growth and development of the
child. Complementary feeding means gradual
withdrawal of the child from breast milk and giving
supplementary food. There is very little data available
on socio-cultural practices in rural areas, owing to
location of medical colleges mostly in urban areas.
Since present study is conducted in a tertiary care
hospital of rural area, it brings an interesting
perspective regarding problems of childrens nutrition
in rural community.
METHODS
It is a descriptive cross sectional study conducted
among 150 lactating mothers who attended Paediatrics
OPD and wards during the study period (May 2013 to
June 2013) in a Tertiary care hospital attached to
medical college in a rural area of western Maharashtra.
The institutional ethical committee clearance was
obtained before initiation of the study. Women having
children in the age group of 0-2 years were enrolled
for the study. While women suffering from infectious
diseases like HIV and those suffering from contagious
diseases in the area of the nipple were excluded.
Study design: - It is a descriptive cross sectional
study conducted in Tertiary care hospital. Women
fulfilling the eligibility criteria were enrolled. A
detailed questionnaire was made in consultation with
the research committee. The questionnaire was
translated into the local language (Marathi) and was
used to assess knowledge and practices related to
breastfeeding and complementary feeding after
obtaining verbal consent of the participants. Women
having children of any sex i.e. male or female were
included in the study.
The questionnaire covered the following parameters-
Mothers age, gravida, parity and educational status,
occupation of both parents, per capita income per
month, various practices related to breastfeeding like
an initiation of breastfeeding, giving colostrum,
giving pre-lacteal feed, period of exclusive
breastfeeding etc. knowledge regarding the
advantages of giving colostrum, continuing/
discontinued breastfeeding when a child is suffering
from diarrhoea, age of initiation of complementary
feeding type of supplementary food given, changes in
mothers diet after delivery. Pamphlets showing
appropriate breastfeeding position as per the Infant
and Young Child Feeding (IYCF) module was used
to ask the mothers if they breastfed their children in
the same manner. And later on, pamphlets were given
to the mothers to educate them. Once the
questionnaire was filled, doubts related to the same
were clarified.
Study Duration- May 2013 to December 2013
STATISTICAL ANALYSIS
The data was collected. Statistical analysis using Chi
square test was done to see the association between
socio cultural-factors and breastfeeding and
complementary feeding practices.
RESULTS
It was seen that 7/150 babies were given pre-lacteal
feed. Sugar water, cow milk, goat milk, jiggery and
honey were given as pre-lacteal feed.
Table 1: Education v/s knowledge and practices related to breastfeeding
Mothers educational status Nil/ Primary
education
Secondary
education
Graduation
Chi square
value
P values
Advantages of
colostrums
Yes 4/19 (21.0%) 40/114 (54.4%) 11/17(64.7%)
7.88
*P<0.05
No 15/19 (78.9%) 74/114 (45.6%) 6/17 (35.3%)
Colostrum given or
not
Yes 18/19 (94.7%) 110/114 (96.5%) 17/17 (100%)
0.082
P>0.05
No 1/19 (5.3%) 4/114 (3.5%) 0
* Statistically significant
It was seen that, mothers who were graduates or had
secondary level education knew that colostrum
protects the baby against infections, as compared to
those having a primary or nil education. Even then,
853
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
colostrum was given by majority of the women from
all three groups. Thus, education was positively
associated with awareness regarding advantages of
colostrum while no association was seen between
educational status and practice of giving colostrum.
Table 2: Initiation of breastfeeding
Initiation of
breastfeeding
Number of
women
%
Within 1 hour of birth
76/150 50.5
Within 2-5 hours of
birth
38/150 25.3
1 day-1 month after
birth
36/150 24.3
50% of mothers initiated breastfeeding within 1 hour
after birth. It was observed that in some cases
breastfeeding was initiated after a day up to 1 month
after birth.
Table 3: Parity versus complementary feeding
practices
Parameter Primipara Multipara
Complementary
feeding before 6
months
1/32
(3.1%)
2/67 (2.9%)
Complementary
feeding after 6
months
31/32
(96.9%)
65/67
(97.0%)
Chi square value 0.005
P value >0.05
99/150 babies were given supplementary food; while
in 51 exclusive breastfeeding was done.
No significant correlation was observed between
parity and complementary feeding practices. In primi
as well as multi para, complementary feeding was
done after 6 months in majority of the cases.
Table 4: Changes in mothers diet after delivery
Diet Number of women %
No change 83 56.6
Additional diet 35 23.4
Less diet 29 19.4
Liquid diet 1 0.6
Majority of the women made no changes in their diet
after delivery. A few, in fact, consumed less than
normal diet.
It was observed that per capita income per month had
no impact on the duration of exclusive breastfeeding.
Most of the women in both groups had done
exclusive breastfeeding up to 6 months of age.
Majority of the women were aware that feeding
should be continued even when the child is suffering
from diarrhoea. But still some said no to feed when
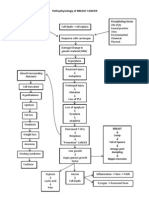
the child was suffering from diarrhoea (fig: 1)
Table 5: Association between economic status and
duration of exclusive breastfeeding
>Rs 900 per er
person per
month
<Rs 900 per
person per
month
Exclusive breastfeeding
for more than 6 months
86 38
Exclusive breastfeeding
for less than 6 months
6 1
Exclusive breastfeeding
for less than 6 months
17 2
Chi square value 3.95
P value >0.05
Fig 1- Should breast feeding be continued when child
is suffering from diarrhoea
DISCUSSION
As per IYCF guidelines pre-lacteal feed should not be
given to a baby. Even then, as per the traditional
practice, pre-lacteal feed was given to little babies.
Although in few women, this misconception of giving
pre-lacteal feed was observed.
Ideally breastfeeding should be initiated within one
hour after birth
2
. However, as per table 2, in this
study, it was found that only half of total number of
women initiated breastfeeding within first hour of
birth. While a quarter of them started it within 2-5
hours after birth i.e. total three quarter of mothers
initiated breastfeeding on the first day after birth.
Thus, the correct practice of initiation of
breastfeeding immediately after birth was not adopted
by all mothers showing another misconception in our
area. In contrast to this, only a quarter of women
started breastfeeding their babies on the first day of
birth in rural areas of Punjab
4
. While, higher number
of mothers initiated breastfeeding within first 2 hours
853
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
colostrum was given by majority of the women from
all three groups. Thus, education was positively
associated with awareness regarding advantages of
colostrum while no association was seen between
educational status and practice of giving colostrum.
Table 2: Initiation of breastfeeding
Initiation of
breastfeeding
Number of
women
%
Within 1 hour of birth
76/150 50.5
Within 2-5 hours of
birth
38/150 25.3
1 day-1 month after
birth
36/150 24.3
50% of mothers initiated breastfeeding within 1 hour
after birth. It was observed that in some cases
breastfeeding was initiated after a day up to 1 month
after birth.
Table 3: Parity versus complementary feeding
practices
Parameter Primipara Multipara
Complementary
feeding before 6
months
1/32
(3.1%)
2/67 (2.9%)
Complementary
feeding after 6
months
31/32
(96.9%)
65/67
(97.0%)
Chi square value 0.005
P value >0.05
99/150 babies were given supplementary food; while
in 51 exclusive breastfeeding was done.
No significant correlation was observed between
parity and complementary feeding practices. In primi
as well as multi para, complementary feeding was
done after 6 months in majority of the cases.
Table 4: Changes in mothers diet after delivery
Diet Number of women %
No change 83 56.6
Additional diet 35 23.4
Less diet 29 19.4
Liquid diet 1 0.6
Majority of the women made no changes in their diet
after delivery. A few, in fact, consumed less than
normal diet.
It was observed that per capita income per month had
no impact on the duration of exclusive breastfeeding.
Most of the women in both groups had done
exclusive breastfeeding up to 6 months of age.
Majority of the women were aware that feeding
should be continued even when the child is suffering
from diarrhoea. But still some said no to feed when
the child was suffering from diarrhoea (fig: 1)
Table 5: Association between economic status and
duration of exclusive breastfeeding
>Rs 900 per er
person per
month
<Rs 900 per
person per
month
Exclusive breastfeeding
for more than 6 months
86 38
Exclusive breastfeeding
for less than 6 months
6 1
Exclusive breastfeeding
for less than 6 months
17 2
Chi square value 3.95
P value >0.05
Fig 1- Should breast feeding be continued when child
is suffering from diarrhoea
DISCUSSION
As per IYCF guidelines pre-lacteal feed should not be
given to a baby. Even then, as per the traditional
practice, pre-lacteal feed was given to little babies.
Although in few women, this misconception of giving
pre-lacteal feed was observed.
Ideally breastfeeding should be initiated within one
hour after birth
2
. However, as per table 2, in this
study, it was found that only half of total number of
women initiated breastfeeding within first hour of
birth. While a quarter of them started it within 2-5
hours after birth i.e. total three quarter of mothers
initiated breastfeeding on the first day after birth.
Thus, the correct practice of initiation of
breastfeeding immediately after birth was not adopted
by all mothers showing another misconception in our
area. In contrast to this, only a quarter of women
started breastfeeding their babies on the first day of
birth in rural areas of Punjab
4
. While, higher number
of mothers initiated breastfeeding within first 2 hours
76%
19.40% 4.60%
Should feeding be continued when
child is suffering from diarrhoea?
853
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
colostrum was given by majority of the women from
all three groups. Thus, education was positively
associated with awareness regarding advantages of
colostrum while no association was seen between
educational status and practice of giving colostrum.
Table 2: Initiation of breastfeeding
Initiation of
breastfeeding
Number of
women
%
Within 1 hour of birth
76/150 50.5
Within 2-5 hours of
birth
38/150 25.3
1 day-1 month after
birth
36/150 24.3
50% of mothers initiated breastfeeding within 1 hour
after birth. It was observed that in some cases
breastfeeding was initiated after a day up to 1 month
after birth.
Table 3: Parity versus complementary feeding
practices
Parameter Primipara Multipara
Complementary
feeding before 6
months
1/32
(3.1%)
2/67 (2.9%)
Complementary
feeding after 6
months
31/32
(96.9%)
65/67
(97.0%)
Chi square value 0.005
P value >0.05
99/150 babies were given supplementary food; while
in 51 exclusive breastfeeding was done.
No significant correlation was observed between
parity and complementary feeding practices. In primi
as well as multi para, complementary feeding was
done after 6 months in majority of the cases.
Table 4: Changes in mothers diet after delivery
Diet Number of women %
No change 83 56.6
Additional diet 35 23.4
Less diet 29 19.4
Liquid diet 1 0.6
Majority of the women made no changes in their diet
after delivery. A few, in fact, consumed less than
normal diet.
It was observed that per capita income per month had
no impact on the duration of exclusive breastfeeding.
Most of the women in both groups had done
exclusive breastfeeding up to 6 months of age.
Majority of the women were aware that feeding
should be continued even when the child is suffering
from diarrhoea. But still some said no to feed when
the child was suffering from diarrhoea (fig: 1)
Table 5: Association between economic status and
duration of exclusive breastfeeding
>Rs 900 per er
person per
month
<Rs 900 per
person per
month
Exclusive breastfeeding
for more than 6 months
86 38
Exclusive breastfeeding
for less than 6 months
6 1
Exclusive breastfeeding
for less than 6 months
17 2
Chi square value 3.95
P value >0.05
Fig 1- Should breast feeding be continued when child
is suffering from diarrhoea
DISCUSSION
As per IYCF guidelines pre-lacteal feed should not be
given to a baby. Even then, as per the traditional
practice, pre-lacteal feed was given to little babies.
Although in few women, this misconception of giving
pre-lacteal feed was observed.
Ideally breastfeeding should be initiated within one
hour after birth
2
. However, as per table 2, in this
study, it was found that only half of total number of
women initiated breastfeeding within first hour of
birth. While a quarter of them started it within 2-5
hours after birth i.e. total three quarter of mothers
initiated breastfeeding on the first day after birth.
Thus, the correct practice of initiation of
breastfeeding immediately after birth was not adopted
by all mothers showing another misconception in our
area. In contrast to this, only a quarter of women
started breastfeeding their babies on the first day of
birth in rural areas of Punjab
4
. While, higher number
of mothers initiated breastfeeding within first 2 hours
76%
Should feeding be continued when
child is suffering from diarrhoea?
Yes
No
Dont know
854
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
of birth in another study carried out in a rural area of
Maharashtra
5.
However, as per National family health
survey III (NFHS III) it was found that less than one
fourth (23%) of women in India
2
and more than half
(52%) women of Maharashtra initiated breastfeeding
early
2
. Thus, the results of our study were comparable
to that of the regional figure of Maharashtra but not
comparable to national figures. According to table I,
majority of the mothers gave colostrum to their
babies, but still one tenth discarded it. This is a
misconception that colostrum should not be given,
which was seen in some women. Even though
colostrum was given by most of the mothers,
awareness regarding its advantages was seen in very
few. Exclusive breastfeeding for 6 months has a
potential to reduce under 5 mortality rate by 13%.
Although most of the babies were exclusively
breastfed for more than 6 months, there were few
who started complementary feeding before 6 months
of age and some did not know till what age exclusive
breastfeeding should be done. Studies have shown
that sometimes exclusive breastfeeding is done much
beyond 6 months, which is insufficient to fulfil the
childs nutritional demand and thus should be
discouraged
7
and in our study also few such cases
were found where exclusive breastfeeding was done
much beyond 6 months. Hence, awareness regarding
the age of exclusive breastfeeding was seen in most
of the women, however not seen in all.
At the time of antenatal counseling, emphasis should
be placed on importance about the advantages of
breastfeeding thereby improves breastfeeding
practices
8
. Even then, only one-fifth of the women
were told about appropriate breastfeeding methods
and its advantages during antenatal counseling. So,
not all women were told about the method and
advantages of breastfeeding, antenatal counseling
should have been done ideally. Nutritional demand of
women increases during pregnancy and further
increases during lactation
9
. Thus, appropriate changes
in the diet should be done after delivery. As seen in
table 4, not even one fourth of the women had an
additional diet after delivery there by proving that
knowledge regarding changes in mothers diet after
delivery was poor. As per WHO guidelines, it is
recommended that breastfeeding should be continued
even when the child is suffering from diarrhoea. But
still, as per figure 1, almost more than one quarter of
women said no to breastfeeding when the child was
suffering from diarrhoea, showing that misconception
related to feeding practices when child was having
diarrhoea was present. In primi as well as multi para,
complementary feeding was done after 6 months in
most of the cases. As observed in table 3, no
association was seen between parity of the mother
and age of introduction of complementary feeding
Also according to table 5, no association was
observed between socioeconomic status and duration
of exclusive breastfeeding as it was done up to 6
months in most of the women belonging to different
socio-economic classes.
Thus, knowledge and practices regarding
breastfeeding and complementary feeding were
influenced by-mothers educational status. But no
significant variations were seen due to factors like-
parity of the mother and socioeconomic status.
CONCLUSION
Though majority of the women adopted appropriate
breastfeeding and complementary feeding practices,
there is still need of creating awareness regarding
breastfeeding and complementary feeding practices
as misconception of not giving colostrum, giving of
pre-lacteal feed and late initiation of breastfeeding
were existing. Also, some women did not know about
the age at which supplementary food should be
introduced. There were inadequate changes in
mothers diet after delivery and feeding was not done
when child was suffering from diarrhoea. Thus, there
is need of educating the women regarding
breastfeeding and complementary feeding practices.
LIMITATIONS
A larger sample size would yield better results for
generalization. This is a hospital based study thus the
results cannot be generalized. Recall bias of
participants is also a limitation.
RECOMMENDATIONS
The antenatal counselling regarding importance of
colostrums & breastfeeding practices should be
given. Doctors, nurses, postgraduates and interns
should help the mother for initiation of breastfeeding.
Drawbacks of bottle feeding must be emphasized.
Audio-visual aids like a television set showing proper
breastfeeding and weaning practices should be
provided in gynaecology and paediatrics OPD.
Removing misconceptions & misbelievers regarding
855
Ashwinee et al., Int J Med Res Health Sci. 2014; 3(4): 851-855
breastfeeding and complementary feeding during
ANC and PNC is necessary.
ACKNOWLEDGEMENT
Authors acknowledge support from Indian Council of
Medical Research, New Delhi for supporting this
research through an STS - program for year 2013-
2014; Ref ID 2013-00287
Conflict of Interest: Nil
REFERENCES
1. Umar AS, Oche MO. Breastfeeding and weaning
practices in an urban slum, north western Nigeria,
International Journal of tropical disease and
health 2013; 3(2):114-25
2. Infant and young child feeding module, prepared
by Maharashtra University of Health Sciences,
UNICEF, Breast Feeding Promotion Network of
India(Maharashtra State Branch), Rajmata Jijau
Mother Child Health & Nutrition Mission, Govt.
of Maharashtra, ICDS, DWCD, Dept. of Family
Welfare, Govt. of Maharashtra, 2005
3. Park K, Textbook of Preventive and Social
Medicine. 2013 22
nd
edition ; 497-99.
4. Bulletin of Breastfeeding Promotion Network of
India 2012; 35: 5
5. Deshpande JD, Giri PA, Phalke DB, Phalke VD,
Kalakoti P, Aarif MM. Socio-cultural practices in
relation to breastfeeding, weaning and child
rearing among Indian mothers and assessment of
nutritional status of children under five in rural
India. Australasian Medical Journal AMJ 2010;
3( 9) : 618-24
6. Ghai OP. Textbook of Essentials of Pediatrics,
2012 ;7
th
edition, 122
7. Khan ME. Breastfeeding and weaning practices
in India. Asia Pacific Population Journal 1990; 5:
7188
8. Mattar CN, Chong YS, Chan YS, Chew A, Tan
P, Chan YH, Rauff MH. Simple antenatal
preparation to improve breastfeeding practice: a
randomized controlled trial. Obstet Gynecol
2007; 109(1):73-80
9. Park K. Textbook of Preventive and Social
Medicine 2013; 22
nd
edition, 587
Vous aimerez peut-être aussi
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Jurnal Asi Ekslusif PDFDocument8 pagesJurnal Asi Ekslusif PDFDeep SleepPas encore d'évaluation
- The Venus of WillendorfDocument19 pagesThe Venus of Willendorfdbenit100% (1)
- Highschool DXD Dx1Document142 pagesHighschool DXD Dx1Gokul Krish100% (9)
- Perceptions and Practices Regarding Breastfeeding Among Postnatal Women at A District Tertiary Referral Government Hospital in Southern IndiaDocument7 pagesPerceptions and Practices Regarding Breastfeeding Among Postnatal Women at A District Tertiary Referral Government Hospital in Southern IndiaJamby VivasPas encore d'évaluation
- Nutrients: The Early Introduction of Complementary (Solid) Foods: A Prospective Cohort Study of Infants in Chengdu, ChinaDocument10 pagesNutrients: The Early Introduction of Complementary (Solid) Foods: A Prospective Cohort Study of Infants in Chengdu, ChinaCarlosPazPas encore d'évaluation
- 13 Sabharwal EtalDocument8 pages13 Sabharwal EtaleditorijmrhsPas encore d'évaluation
- EditDocument91 pagesEditShantaMohapatraPas encore d'évaluation
- Correlation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenDocument19 pagesCorrelation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenSherly Lebrina KerjapyPas encore d'évaluation
- JN 214346Document9 pagesJN 214346lada emmanuelPas encore d'évaluation
- Korn Ides 2013Document10 pagesKorn Ides 2013Nanda AlvionitaPas encore d'évaluation
- The Relationship Between Feeding Practices and Children Ages 0-24monthsDocument42 pagesThe Relationship Between Feeding Practices and Children Ages 0-24monthsGiovanni MartinPas encore d'évaluation
- 6.sick Child Feeding Practice and Associated Factors Among Mothers of Children Less Than 24 Months Old, in Burayu Tow, EthiopiaDocument8 pages6.sick Child Feeding Practice and Associated Factors Among Mothers of Children Less Than 24 Months Old, in Burayu Tow, EthiopiaTomas YeheisPas encore d'évaluation
- Advance Concept in NursingDocument17 pagesAdvance Concept in NursingAnita NakhshabPas encore d'évaluation
- Notes On Exclusive BreastfeedingDocument6 pagesNotes On Exclusive BreastfeedingNdem BasseyPas encore d'évaluation
- Jurnal 2Document5 pagesJurnal 2desianabsPas encore d'évaluation
- Assessment of Maternal Knowledge, Attitudes, and Practices Regarding Breastfeeding at Kampala International Teaching Hospital A Study Spanning May 2021 To July 2022Document15 pagesAssessment of Maternal Knowledge, Attitudes, and Practices Regarding Breastfeeding at Kampala International Teaching Hospital A Study Spanning May 2021 To July 2022KIU PUBLICATION AND EXTENSIONPas encore d'évaluation
- Frequency of Malnutrition Among Children Under 2 Years and Its Relationship With Inadequate Breast Feeding PracticeDocument3 pagesFrequency of Malnutrition Among Children Under 2 Years and Its Relationship With Inadequate Breast Feeding PracticeAndhika SatriyaPas encore d'évaluation
- Assess The Knowledge Attitude and Practice Regarding Breastfeeding Among Primi MothersDocument43 pagesAssess The Knowledge Attitude and Practice Regarding Breastfeeding Among Primi Mothersjuli_naz94% (33)
- Research ProposalDocument6 pagesResearch Proposalgeorge100% (4)
- Breast-Feeding Performance Index - A Composite Index To Describe Overall Breast-Feeding Performance Among Infants Under 6 Months of AgeDocument9 pagesBreast-Feeding Performance Index - A Composite Index To Describe Overall Breast-Feeding Performance Among Infants Under 6 Months of AgeHuan VuongPas encore d'évaluation
- Effectiveness of Breast Feeding Protocol Among Caesarean Mothers Admitted in Narayana Medical College Hospital, NelloreDocument5 pagesEffectiveness of Breast Feeding Protocol Among Caesarean Mothers Admitted in Narayana Medical College Hospital, NelloreArti NegiPas encore d'évaluation
- Knowledge About Breast Feeding in Accordance With The National Policy Among DoctorsDocument12 pagesKnowledge About Breast Feeding in Accordance With The National Policy Among Doctorsmaylmutia100% (1)
- Analysis Breastfeeding Pattern and ECC, Susi PDFDocument10 pagesAnalysis Breastfeeding Pattern and ECC, Susi PDFSusi AbidinPas encore d'évaluation
- Knowledge Attitiude and Practice of BreaDocument8 pagesKnowledge Attitiude and Practice of BreaBesse Darmita Yuana PutriPas encore d'évaluation
- A Review Article: Myths, Beliefs and Malpractices Relating To Breastfeeding and Complementary Feeding PracticesDocument3 pagesA Review Article: Myths, Beliefs and Malpractices Relating To Breastfeeding and Complementary Feeding PracticesinventionjournalsPas encore d'évaluation
- Awareness and Practice of Breast Feeding Among Mothers at Kiryandongo District HospitalDocument12 pagesAwareness and Practice of Breast Feeding Among Mothers at Kiryandongo District HospitalKIU PUBLICATION AND EXTENSIONPas encore d'évaluation
- RESEARCH093016Document28 pagesRESEARCH093016Satra Sabbuh100% (1)
- Factors Influencing Breastfeeding Practices Among Mothers in Lafia LocalDocument13 pagesFactors Influencing Breastfeeding Practices Among Mothers in Lafia LocalCha Tozenity ChiePas encore d'évaluation
- Assess Theknowledge & Practice of Pregnant and Lactating Women Related To Nutrition DeficiencyDocument16 pagesAssess Theknowledge & Practice of Pregnant and Lactating Women Related To Nutrition DeficiencyZohrahLiaqatPas encore d'évaluation
- Literature Review On Knowledge Attitude and Practice of Exclusive BreastfeedingDocument7 pagesLiterature Review On Knowledge Attitude and Practice of Exclusive Breastfeedingfvg6kcwyPas encore d'évaluation
- Relationship Between Breastfeeding Practices and Nutritional Status Aged 0-24 Months KenyaDocument21 pagesRelationship Between Breastfeeding Practices and Nutritional Status Aged 0-24 Months KenyaderiPas encore d'évaluation
- Research Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in MauritiusDocument9 pagesResearch Article: An Assessment of The Breastfeeding Practices and Infant Feeding Pattern Among Mothers in MauritiusNurhikmah RnPas encore d'évaluation
- Title: Exploring The Various Infant Feeding Practice Among Mothers Attending Infant Welfare Clinic at Holy Trinity Ekona. Name: Neh Doreen No:1244Document5 pagesTitle: Exploring The Various Infant Feeding Practice Among Mothers Attending Infant Welfare Clinic at Holy Trinity Ekona. Name: Neh Doreen No:1244Lucien YemahPas encore d'évaluation
- Association PDFDocument4 pagesAssociation PDFLia RusmanPas encore d'évaluation
- Need To Optimise Infant Feeding CounsellingDocument30 pagesNeed To Optimise Infant Feeding CounsellingfadnesPas encore d'évaluation
- Correlation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenDocument5 pagesCorrelation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenAnonymous hETtEBkk7Pas encore d'évaluation
- Harry Potter and The Deathly Hallows (Russian)Document5 pagesHarry Potter and The Deathly Hallows (Russian)Te HineahuonePas encore d'évaluation
- Issues Related To Breastfeeding in The First Six Months of Life in An Urban Tertiary Care HospitalDocument7 pagesIssues Related To Breastfeeding in The First Six Months of Life in An Urban Tertiary Care HospitalVanyaPas encore d'évaluation
- Women Beliefs & Practices Regarding Food During Pregnancy - A Hospital Based Study"Document7 pagesWomen Beliefs & Practices Regarding Food During Pregnancy - A Hospital Based Study"ayrahma29Pas encore d'évaluation
- Factors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanDocument7 pagesFactors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanHilda HildaPas encore d'évaluation
- Factors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanDocument7 pagesFactors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanHilda HildaPas encore d'évaluation
- Knowledge Attitude and Practice of ExcluDocument16 pagesKnowledge Attitude and Practice of ExclupblesynnPas encore d'évaluation
- Electronic Physician (ISSN: 2008-5842) HTTP://WWW - Ephysician.irDocument28 pagesElectronic Physician (ISSN: 2008-5842) HTTP://WWW - Ephysician.irRambu KudduPas encore d'évaluation
- Breastfeeding and The Use of Human Milk 2005Document13 pagesBreastfeeding and The Use of Human Milk 2005Juan Pablo Anabalón SaavedraPas encore d'évaluation
- The Effect of Education Lactation On Breastfeeding Behavior Infant 0-6 Months in Kendari IndonesiaDocument12 pagesThe Effect of Education Lactation On Breastfeeding Behavior Infant 0-6 Months in Kendari IndonesiaDessy WahyuniPas encore d'évaluation
- Pengaruh Status Gizi Ibu Menyusui Terhadap Eksklusivitas Asi Dan Pertumbuhan Bayi Di Rsud Prof. Dr. WZ Johannes Kupang-Ntt (Soi, Et All)Document17 pagesPengaruh Status Gizi Ibu Menyusui Terhadap Eksklusivitas Asi Dan Pertumbuhan Bayi Di Rsud Prof. Dr. WZ Johannes Kupang-Ntt (Soi, Et All)Alvin Brilian BudionoPas encore d'évaluation
- Fucile2018 Ver WordDocument8 pagesFucile2018 Ver WordAries CamiPas encore d'évaluation
- Anantha Lakshmi Satyavathi Devi Kommula PDFDocument3 pagesAnantha Lakshmi Satyavathi Devi Kommula PDFnjmdrPas encore d'évaluation
- L. Pengaruh Gizi Terhadap Produksi ASI (Jurnal) : Beatrix Soi, Madarina Julia, R. Dwi BudiningsariDocument8 pagesL. Pengaruh Gizi Terhadap Produksi ASI (Jurnal) : Beatrix Soi, Madarina Julia, R. Dwi BudiningsariAvc SubangPas encore d'évaluation
- Winly WenasDocument8 pagesWinly WenasFia PyooPas encore d'évaluation
- Timely-Initiation-Of-Complementary-Feeding-And-Associated-Factors-Amongchildren-Aged-6-To-12-Months-In-Addis-Ababa-Ethiopia-2015-2161-1165-1000272Document8 pagesTimely-Initiation-Of-Complementary-Feeding-And-Associated-Factors-Amongchildren-Aged-6-To-12-Months-In-Addis-Ababa-Ethiopia-2015-2161-1165-1000272Tomas YeheisPas encore d'évaluation
- Nursing Group Research PaperDocument16 pagesNursing Group Research Paperapi-368267454Pas encore d'évaluation
- Article 1Document10 pagesArticle 1nishaniindunilpeduruhewaPas encore d'évaluation
- Zainab ProjectDocument35 pagesZainab ProjectOpeyemi JamalPas encore d'évaluation
- Inter Tambunan 2021Document8 pagesInter Tambunan 2021yazmin arminabdullahPas encore d'évaluation
- Rume Chapter Five PDFDocument7 pagesRume Chapter Five PDFHarrison RumePas encore d'évaluation
- 434 652 1 SM PDFDocument7 pages434 652 1 SM PDFAngger Luhung Nur FadlilahPas encore d'évaluation
- Feeding Practices Among Children Under One Year of Age Admitted To A Public HospitalDocument11 pagesFeeding Practices Among Children Under One Year of Age Admitted To A Public HospitalAnonymous dRZNhhBFYPas encore d'évaluation
- Building Future Health and Well-Being of Thriving Toddlers and Young Children: 95th Nestlé Nutrition Institute Workshop, September 2020D'EverandBuilding Future Health and Well-Being of Thriving Toddlers and Young Children: 95th Nestlé Nutrition Institute Workshop, September 2020Pas encore d'évaluation
- Ijmrhs Vol 4 Issue 3Document263 pagesIjmrhs Vol 4 Issue 3editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 1 Issue 1Document257 pagesIjmrhs Vol 1 Issue 1editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 2Document281 pagesIjmrhs Vol 3 Issue 2editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 4Document294 pagesIjmrhs Vol 3 Issue 4editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 3Document271 pagesIjmrhs Vol 3 Issue 3editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 4 Issue 2Document219 pagesIjmrhs Vol 4 Issue 2editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 4 Issue 4Document193 pagesIjmrhs Vol 4 Issue 4editorijmrhs0% (1)
- Ijmrhs Vol 3 Issue 1Document228 pagesIjmrhs Vol 3 Issue 1editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 2Document197 pagesIjmrhs Vol 2 Issue 2editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 1 Issue 1Document257 pagesIjmrhs Vol 1 Issue 1editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 4Document321 pagesIjmrhs Vol 2 Issue 4editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 1Document110 pagesIjmrhs Vol 2 Issue 1editorijmrhs100% (1)
- Ijmrhs Vol 2 Issue 3Document399 pagesIjmrhs Vol 2 Issue 3editorijmrhs100% (1)
- 47serban Turliuc EtalDocument4 pages47serban Turliuc EtaleditorijmrhsPas encore d'évaluation
- 41anurag EtalDocument2 pages41anurag EtaleditorijmrhsPas encore d'évaluation
- 48 MakrandDocument2 pages48 MakrandeditorijmrhsPas encore d'évaluation
- 45mohit EtalDocument4 pages45mohit EtaleditorijmrhsPas encore d'évaluation
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDocument2 pagesRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsPas encore d'évaluation
- 38vaishnavi EtalDocument3 pages38vaishnavi EtaleditorijmrhsPas encore d'évaluation
- 43chaitali EtalDocument3 pages43chaitali EtaleditorijmrhsPas encore d'évaluation
- 40vedant EtalDocument4 pages40vedant EtaleditorijmrhsPas encore d'évaluation
- Williams-Campbell Syndrome-A Rare Entity of Congenital Bronchiectasis: A Case Report in AdultDocument3 pagesWilliams-Campbell Syndrome-A Rare Entity of Congenital Bronchiectasis: A Case Report in AdulteditorijmrhsPas encore d'évaluation
- Pernicious Anemia in Young: A Case Report With Review of LiteratureDocument5 pagesPernicious Anemia in Young: A Case Report With Review of LiteratureeditorijmrhsPas encore d'évaluation
- 35krishnasamy EtalDocument1 page35krishnasamy EtaleditorijmrhsPas encore d'évaluation
- 33 Prabu RamDocument5 pages33 Prabu RameditorijmrhsPas encore d'évaluation
- 36rashmipal EtalDocument6 pages36rashmipal EtaleditorijmrhsPas encore d'évaluation
- 37poflee EtalDocument3 pages37poflee EtaleditorijmrhsPas encore d'évaluation
- 34tupe EtalDocument5 pages34tupe EtaleditorijmrhsPas encore d'évaluation
- 32bheemprasad EtalDocument3 pages32bheemprasad EtaleditorijmrhsPas encore d'évaluation
- Partial Mastectomy ReconstructionDocument12 pagesPartial Mastectomy ReconstructionJose Mauricio Suarez BecerraPas encore d'évaluation
- MammographyDocument27 pagesMammographyRohmatullah Anas100% (1)
- ATR 026 Daddys Girl Se18e6Document61 pagesATR 026 Daddys Girl Se18e6Hannah CurranPas encore d'évaluation
- DR Show MeDocument6 pagesDR Show MesynuppsPas encore d'évaluation
- Maternal Physiological and Psychological Adaptations To PregnancyDocument62 pagesMaternal Physiological and Psychological Adaptations To PregnancySuad jakalatPas encore d'évaluation
- Garuda 653101Document5 pagesGaruda 653101Anti PraharaniPas encore d'évaluation
- Flipchart For ASHADocument68 pagesFlipchart For ASHA'minet Amores100% (1)
- The Breasts - Structure - Vasculature - TeachMeAnatomyDocument4 pagesThe Breasts - Structure - Vasculature - TeachMeAnatomywzt2001Pas encore d'évaluation
- Breast Cancer Risks RecommendationsDocument2 pagesBreast Cancer Risks RecommendationsYohannes GirmawPas encore d'évaluation
- Final - Health 8.4 Maternal Health Concerns, 4 LessonsDocument51 pagesFinal - Health 8.4 Maternal Health Concerns, 4 LessonsReggie SanguyoPas encore d'évaluation
- Breast Enlargement Exercise at Home For Getting Bigger Breasts NaturallyDocument8 pagesBreast Enlargement Exercise at Home For Getting Bigger Breasts NaturallyAT100% (1)
- Health7 - q1 - Mod4 - Health Appraisal and Screening Procedures - Final08032020Document26 pagesHealth7 - q1 - Mod4 - Health Appraisal and Screening Procedures - Final08032020Mark Anthony Telan Pitogo50% (2)
- Sally O'Driscoll ArticleDocument25 pagesSally O'Driscoll Articlep_kelleherPas encore d'évaluation
- VS Push UpDocument8 pagesVS Push UpmtandersongcPas encore d'évaluation
- Waiters Newborn Care PDFDocument1 pageWaiters Newborn Care PDFmp1757Pas encore d'évaluation
- Breast Pumps Flyer EN 1819-Single-Pages-A4Document6 pagesBreast Pumps Flyer EN 1819-Single-Pages-A4Rigoberto Leigue OrdoñezPas encore d'évaluation
- Community Health Nursing Sample TestDocument45 pagesCommunity Health Nursing Sample TestPaulo Tiangson MejiaPas encore d'évaluation
- Answers To Common Questions About Breast Screening and MammogramsDocument5 pagesAnswers To Common Questions About Breast Screening and MammogramsWatertown Daily TimesPas encore d'évaluation
- Temple RunDocument4 pagesTemple RunMitchPas encore d'évaluation
- Breastfeeding Protocols 1 To 21 Complete Manual 2013Document196 pagesBreastfeeding Protocols 1 To 21 Complete Manual 2013amandaguttPas encore d'évaluation
- Sailorio-The SanctuaryDocument73 pagesSailorio-The SanctuaryGar LewisPas encore d'évaluation
- Physical Assessment Table: Body Parts Assessed Technique Normal Findings Actual Findings Remarks General SurveyDocument11 pagesPhysical Assessment Table: Body Parts Assessed Technique Normal Findings Actual Findings Remarks General SurveyMia PascualPas encore d'évaluation
- Breast AssessmentDocument2 pagesBreast AssessmentHPas encore d'évaluation
- Breast ExaminationDocument40 pagesBreast ExaminationSanjay Kumar SanjuPas encore d'évaluation
- Breastfeeding Pamphlet - English ReformatDocument2 pagesBreastfeeding Pamphlet - English ReformatRisalouise LucasPas encore d'évaluation
- Seminar On FibroadenosisDocument23 pagesSeminar On FibroadenosisSk Saklin MustakPas encore d'évaluation
- Zinc in Human MilkDocument43 pagesZinc in Human MilkFajar YuniftiadiPas encore d'évaluation