Académique Documents
Professionnel Documents
Culture Documents
Local Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MD
Transféré par
JohnBedaLatawanMalecdanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Local Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MD
Transféré par
JohnBedaLatawanMalecdanDroits d'auteur :
Formats disponibles
Lecture 64:
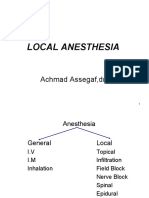
Local Anesthetics
Richard D. Minshall, PhD
Tobias Piegeler, MD
Departments of Anesthesiology and Pharmacology
February 28
th
, 2012
Outline
A. Pharmacologic aspects:
Basic structural characteristics
Mechanism of nerve conduction
Mechanisms of local anesthetic action
Characteristics of local anesthetic action
Metabolism
Why are vasoconstrictors often added to the local anesthetic preparations?
B. Clinical Aspects:
Problem-based learning with clinical vignettes
Chemical structure
Procaine
Lidocaine
Bupivacaine
Tetracaine
H
2
N C
O
CH
2
CH
2
N
C
2
H
5
C
2
H
5
O
HN C
O
CH
2
CH
2
N
CH
3
CH
3
O
C
4
H
9
C
O
N
CH
3
CH
3
NH
C
4
H
9
C
O
CH
3
CH
3
NH CH
2
N
C
2
H
5
C
2
H
5
Lipophilic group Linker Hydrophilic group
Ester-linked
Amide-linked
Local anesthetics
are drugs used to prevent or relieve pain
in specific regions of the body without
loss of consciousness
reversibly block pain sensation by
blocking nerve conduction
Definition
Neural transmission
Resting potential
Action potential
- - - - - - - ++++ + + + + + + + - - - - - -
Mechanism of action
Local anesthetics reversibly bind to the voltage-
gated Na
+
channel (VGSC)
block Na
+
influx and thus
block action potential and nerve conduction.
Local anesthetics
Propagation failure
VGSC(1)
I II III IV
Catterall WA, Neuron 2000; 26(1):13-25
LA
VGSC(2)
Pink:
Local anesthetic binding site
in the inner cavity of the pore
In Segment 6 of Domain IV
(IVS6-Helix)
Green:
Binding site for Tetrodrotoxin
Catterall WA, Neuron 2000; 26(1):13-25
- - - - - - - ++++ + + + +
Local anesthetics
+ + + - - - - - -
++++ + ++ ++ ++ + + + + + + + + + + + + + +
Propagation failure
Influence of fiber type
Local anesthetics more effectively block
small nerve fibers!
Different nerve fiber types
Use-dependent block
Nerves with higher firing frequency and
more positive membrane potential are more
sensitive to local anesthetic block!
Influence of pH
+
+
+
+
+
Low pH
High pH Normal pH
+
+
+
+
+
+
+
+
+
Reason for pH influence?
closed
BH
+
B + H
+
B
B BH
+
BH
+
open
inactivated
Na
+
extracellular
intracellular
H
+
+
Metabolism
1. Most ester-linked local anesthetics are quickly hydrolyzed
by plasma cholinesterase (exception: cocaine)
2. Amide-linked local anesthetics undergo oxidative
dealkylation/oxygenation by monooxygenases and
hydroxylation by carboxylesterase in the liver
3. Water-soluble metabolites are excreted in the urine.
Vasoconstrictor addition
1. Local anesthetics are removed from depot site mainly by
absorption into blood.
2. Addition of vasoconstrictor drugs (e.g. epinephrine)
reduces absorption of local anesthetics, thus prolonging
anesthetic effect and reducing systemic toxicity.
NOTE:
Do not use vasoconstrictors in areas with
(functional) end arteries
possible development of necrosis
due to prolonged hypoperfusion!!!
Whats the problem?
Too much local anesthetic!
Corning JL:
Spinal anaesthesia and local
medication of the cord.
New York State Med J 42:483 (1885)
Bier A:
Versuche ber Cocainisirung des Rckenmarkes.
Deutsche Zeitschrift fr Chirurgie 1899;51:361.
History
Today
Examples of local anesthetic use:
Infiltration
Field block
Nerve block
Intravenous regional block
Spinal anesthesia
Epidural nerve block
Topical anesthesia
Case 1
67 y.o. male with a histologically proven malignancy in the right sidewall of
his bladder presenting for a TUR-B.
PMH:
COPD w/ 90 py (and counting...), FEV1 = 65% VC, HTN,
no known CAD or CVD
Meds:
Tiotropium bromide inhaler
ACE-I
Previous surgeries/anesthesias:
Cystoscopy 01/2012 under GA PONV
Vitals:
HR 78/min, BP 135/78, RR 14/min, Pulse regular, SpO
2
91% at room air
Auscultation: S1, S2, no murmurs, rhythmic, lungs with discrete basal
expansion crackling rales on both sides
Proposed anesthesia?
Case 1
Spinal Anesthesia!
(Hyperbaric) Bupivacaine +/- opioid
Is that enough?
SPA: testing the effect
Try to establish the area where the
patient will recognize a cool pack as
a warm sensation or wont recognize it at all!
Spinal segments correlate with dermatomes!
T10 is sufficient for cystoscopy
NOTE:
1. Hypotension due to loss of
sympathetic tone (C fibers T5-L1!)
2. High spinal above T4
block of the Nn. accelerantes
= sympathetic cardiac accelerators
Obturator nerve
Obturator nerve block
General technique for a block with a nerve stimulator:
1. Stimulation started at e.g. 2 mA for 0.1 ms at 1 Hz
2. Advance the needle at the correct location until desired muscle twitching is visible
3. Current is gradually decreased to 0.2 mA to confirm proximity to the nerve
4. After confirmation of needle position, LA is injected
Case 2
You are on call. Its 3 am in the morning. You receive a call from the OB
resident requesting your service for a 27 y.o. female, gravida 1, para 0 in
the labor room, otherwise healthy.
She just needs a little pain relief, the resident tells you...
When you enter the room, you find a profusely sweating young woman in
serious distress and pain, who is yelling at an exhausted young male, who
seems to be her husband, as well as at the mid-wife, who tries to calm her
down.
Now she starts screaming at you
Procedure?
Case 2
Epidural Anesthesia!
Epidural Anesthesia(1)
Disinfection and
prepping
Skin and
subcutaneous
infiltration
Needle insertion
Epidural Anesthesia(2)
Needle advancement
with loss of resistance
technique
Catheter insertion
Then:
1. Test dose of LA with
epinephrine
Tachycardia?
2. Start of LA:
e.g. ropivacaine 0.1%
(walking epidural)
+/- low dose sufentanil
Case 2: Unforeseen
The epidural works fine, the mother stopped yelling and swears to name
her baby after you for taking her pain away and you get back to bed.
4 am: The OB resident tells you now, that they have to do a non-emergent
C-section on your patient due to unforeseen positioning of the baby.
And now?
General anesthesia with a high risk of aspiration and airway problems?
Solution: Change the ropivacaine from 0.1% to 0.33% and give a bolus.
Check the effect (dermatomes!) and repeat and/or raise continuous infusion
until effective analgesia is reached.
Case 3
A 37 y.o. male with a fracture of the distal radius after an accident with his
bicycle is scheduled for ambulant surgical repair of the fracture.
PMH: healthy
Meds: None
Past surgeries: None
Vitals: excellent
You decide to cover the patients needs with a axillary plexus block plus a
musculocutaneous nerve block.
Oh no
After an easy approach you inject the local anesthetic (bupivacaine),
remove the needle and are proud of yourself...
Seconds later the patient tells you, that his tongue and lips are getting
a little numb and you notice that he gets more and more aggitated and
anxious.
Right after that, the patient suffers from a generalized seizure, looses
consciousness, and stops breathing.
Your patient is dying unless YOU help him!
What would you do?
Lets save a life!
Working hypothesis: Local Anesthetic Systemic Toxicity (LAST)
1. Get help!
2. Initial Focus:
a. Airway management: ventilate with 100% oxygen
b. Seizure suppression: benzodiazepines preferred;
AVOID propofol in patients with cv instability
(vasodilation hypotension!)
Modified after ASRA Checklist for treatment of LAST, Reg Anesth Pain Med, 2012;37:16-18
You are able to establish a secure airway by intratracheal intubation after
induction of anesthesia with midazolam and fentanyl and succinylcholine as
the muscle relaxant.
Suddenly the ECG monitor makes some unfamiliar noises. It looks like this:
It gets worse
Further treatment
1. Management of Cardiac Arrhythmias
a. BLS and ACLS (adjustment of medication and prolonged effort
might be necessary
b. AVOID vasopressin, Ca2+ channel blockers, beta-blockers and
LA (lidocaine is an antiarrhythmic drug class 1B!)
2. Lipid emulsion (20%) therapy
a. Bolus 1.5 ml/kg iv over 1 min
b. Continuous infusion 0.25 ml/kg/min
c. Bolus repetition in case of persisting cv collapse
Modified after ASRA Checklist for treatment of LAST, Reg Anesth Pain Med, 2012;37:16-18
Case closed
After 2 boluses and a total 20 minutes of resuscitation, you are finally able
to re-establish a sufficient circulation in your patient and
transfer him to the ICU.
He leaves the hospital 10 days later without any residual damage
Systemic LA toxicity
Toxic effect
CV depression
Respiratory arrest
Coma
Convulsions Unconsciousness
Muscular twitching
Visual disturbance
Light headedness - Numbness of tongue
Tachycardia
F
r
e
e
L
A
c
o
n
c
e
n
t
r
a
t
i
o
n
i
n
p
l
a
s
m
a
Lipid solubility
Lidocaine 7.8 2.9 64 %
Mepivacaine 7.7 0.8 77 %
Bupivacaine
Levobupivacaine
Ropivacaine 8.1 14 94 %
pKa
8.1 27 95 %
Lipid
solubilty
Protein
binding
LipidRescue
Guy Weinberg, MD
Professor of Anesthesiology at UIC
How does it work?
We dont exactly know!
Lipid emulsion probably works as a scavenger,
that is able to absorb the LA from the
cardiac sodium channel and keep it in the vessel!
More information: www.lipidrescue.org
The End
Questions?
For feedback, questions or a request for a research internship in the Minshall lab:
rminsh@uic.edu
piegeler@uic.edu
Thank you very much for your attention!
Vous aimerez peut-être aussi
- Spinal & Epidural AnaesthesiaDocument31 pagesSpinal & Epidural AnaesthesiaKumar Gavali Suryanarayana0% (1)
- Local Anesthesia Exam TipsDocument9 pagesLocal Anesthesia Exam TipsshadapaaakPas encore d'évaluation
- Lecture Title: Acute Pain Management: Lecturer NameDocument51 pagesLecture Title: Acute Pain Management: Lecturer NameIndra KusumaPas encore d'évaluation
- Local Anaesthesia: Department of Anaesthesia University of Cape TownDocument0 pageLocal Anaesthesia: Department of Anaesthesia University of Cape TownjuniorebindaPas encore d'évaluation
- Pharmacology of Local Anesthetics IDocument93 pagesPharmacology of Local Anesthetics IAlshaimaa AhmedPas encore d'évaluation
- Oral & Maxillofacial Surgery Local Anesthesia PresentationDocument183 pagesOral & Maxillofacial Surgery Local Anesthesia Presentationhaneefmdf100% (2)
- Sub Arachnoid BlockDocument32 pagesSub Arachnoid Blockhendra_darmawan_4Pas encore d'évaluation
- Local AnaestheticsDocument31 pagesLocal AnaestheticsNodi NodiPas encore d'évaluation
- Spinal Epidural Anaesthesia 2Document29 pagesSpinal Epidural Anaesthesia 2ilham novesar0% (1)
- Regional Anesthesia for Hand Surgery: Bier Block LectureDocument28 pagesRegional Anesthesia for Hand Surgery: Bier Block LectureJessica CPas encore d'évaluation
- Local Anesthetics SabinDocument69 pagesLocal Anesthetics Sabinsabin7000Pas encore d'évaluation
- Anestesi LokalDocument12 pagesAnestesi LokalKurniatiKhasanahQhafisaQurratul'ainPas encore d'évaluation
- Local AnestheticsDocument30 pagesLocal AnestheticsmaurinmarceoiaPas encore d'évaluation
- Local Anesthetics2Document36 pagesLocal Anesthetics2sonapradhan14Pas encore d'évaluation
- Local Anaesthetic AgentsDocument21 pagesLocal Anaesthetic AgentsSuresh KumarPas encore d'évaluation
- 6 Regional AnaesthesiaDocument12 pages6 Regional AnaesthesiasaniaaPas encore d'évaluation
- Spinal AnesthesiaDocument4 pagesSpinal AnesthesiaIndah Permata Gaisar100% (2)
- Local Anesthetics2 / Orthodontic Courses by Indian Dental AcademyDocument38 pagesLocal Anesthetics2 / Orthodontic Courses by Indian Dental Academyindian dental academyPas encore d'évaluation
- Local Anesthesia: Achmad Assegaf, DR., SP - AnDocument48 pagesLocal Anesthesia: Achmad Assegaf, DR., SP - AnDesty ArianiPas encore d'évaluation
- Anesthesia 2024Document27 pagesAnesthesia 2024Dinesh Kumar MauryaPas encore d'évaluation
- Anestesi Pada Operasi Mata by PikalDocument60 pagesAnestesi Pada Operasi Mata by PikalSyahpikal SahanaPas encore d'évaluation
- AnesthesiaDocument6 pagesAnesthesiaSamyuktha NatarajanPas encore d'évaluation
- MalamedDocument8 pagesMalamedDr. DhDhPas encore d'évaluation
- Local Anesthesia & Analgesia: Mechanisms, Factors, and Clinical UseDocument18 pagesLocal Anesthesia & Analgesia: Mechanisms, Factors, and Clinical UseMirza HassanPas encore d'évaluation
- 14 Local Anesthesia 2006 BDocument18 pages14 Local Anesthesia 2006 BMansoor AhmadPas encore d'évaluation
- Ocular AnesthesiaDocument61 pagesOcular AnesthesiaAdarsh Keshari100% (1)
- Chapter 2 230327072253 9bf1fc09Document23 pagesChapter 2 230327072253 9bf1fc09parmarkeval1610Pas encore d'évaluation
- Basic Concept On NeuroanesthesiaDocument51 pagesBasic Concept On Neuroanesthesiabrojeem100% (1)
- ANAESTHESIADocument15 pagesANAESTHESIAshailendra.chauhan887Pas encore d'évaluation
- Local Anesthesia GuideDocument101 pagesLocal Anesthesia GuideDrIbrahimShaikhPas encore d'évaluation
- Local Anaesthetics Mechanism and Clinical UsesDocument33 pagesLocal Anaesthetics Mechanism and Clinical UsesYong MxPas encore d'évaluation
- Educational Material RA Handbook FinalDocument58 pagesEducational Material RA Handbook Finalอี๊ด โสภิต Pizzy100% (5)
- Local Anesthetics and Nerve Blocks HannanDocument57 pagesLocal Anesthetics and Nerve Blocks Hannanpriya_edwinPas encore d'évaluation
- Local Anesthetics and Nerve Blocks HannanDocument57 pagesLocal Anesthetics and Nerve Blocks Hannanpriya_edwinPas encore d'évaluation
- PHARM Yoshimura LocalAnesthetics PDFDocument32 pagesPHARM Yoshimura LocalAnesthetics PDFDhaif dhaifPas encore d'évaluation
- PRINCIPLES OF SURGICAL ANESTHESIADocument46 pagesPRINCIPLES OF SURGICAL ANESTHESIASisay FentaPas encore d'évaluation
- Anesthesia:: Perioperative Nursing ImplicationsDocument32 pagesAnesthesia:: Perioperative Nursing ImplicationsjamesbungoPas encore d'évaluation
- LOCAL ANESTHETICS: Local Anesthesia Is The Condition in Which Sensory TransmissionDocument7 pagesLOCAL ANESTHETICS: Local Anesthesia Is The Condition in Which Sensory TransmissionMuhammad Mustafa IjazPas encore d'évaluation
- THEME: General AnestheticsDocument5 pagesTHEME: General AnestheticsAmirah AzmanPas encore d'évaluation
- Local AnesthesiaDocument9 pagesLocal AnesthesiaSherry RamirezPas encore d'évaluation
- Local Anesthesia: Achmad Assegaf, DR., SP - AnDocument48 pagesLocal Anesthesia: Achmad Assegaf, DR., SP - AnDesty ArianiPas encore d'évaluation
- DR - Siddharth Dhanaraj Oral & Maxillofacial Surgeon: Composition Properties & Mechanism of Local AnestheticsDocument68 pagesDR - Siddharth Dhanaraj Oral & Maxillofacial Surgeon: Composition Properties & Mechanism of Local AnestheticsSiddharth DhanarajPas encore d'évaluation
- MRDocument11 pagesMRKireina Amanda NuriandariePas encore d'évaluation
- Local Anesthetic Systemic Toxicity (LAST)Document4 pagesLocal Anesthetic Systemic Toxicity (LAST)Abdelaziz ShokryPas encore d'évaluation
- Pendahuluan 1Document38 pagesPendahuluan 1Danema GrungePas encore d'évaluation
- LOCAL ANAESTHETICS: MECHANISM, USES AND COMPLICATIONSDocument32 pagesLOCAL ANAESTHETICS: MECHANISM, USES AND COMPLICATIONSSri LakshmiPas encore d'évaluation
- Anestesi Lokal Pada Lesi Superfisial: Huntal NapoleonDocument12 pagesAnestesi Lokal Pada Lesi Superfisial: Huntal NapoleonshevinesaPas encore d'évaluation
- 2 LaDocument233 pages2 LaSudeep DkPas encore d'évaluation
- Anaesthesia 1Document26 pagesAnaesthesia 1Snehal SinghPas encore d'évaluation
- ITE Review 1.23.16Document4 pagesITE Review 1.23.16Diana HyltonPas encore d'évaluation
- Anesthetic SubstancesDocument12 pagesAnesthetic SubstancesNewPhoneWhoDisPas encore d'évaluation
- Anestesia 2Document7 pagesAnestesia 2Dani SPas encore d'évaluation
- Local Anesthesia - Material IndianDocument31 pagesLocal Anesthesia - Material IndianLidia SimionescuPas encore d'évaluation
- Understanding Local Anesthetics: Mechanisms, Properties, and UsesDocument33 pagesUnderstanding Local Anesthetics: Mechanisms, Properties, and UsesNOT ZUXPas encore d'évaluation
- Anesthesia Notes and DiscussionDocument58 pagesAnesthesia Notes and Discussionachyutsharma100% (1)
- (Anes) Regional AnesDocument2 pages(Anes) Regional Anesalmira.s.mercadoPas encore d'évaluation
- (ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Document3 pages(ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Ricky Justin NgoPas encore d'évaluation
- Bier Block (Intravenous Regional Anesthesia), Handout PDFDocument8 pagesBier Block (Intravenous Regional Anesthesia), Handout PDFjahangirealamPas encore d'évaluation
- Vascular Innervation and Receptor Mechanisms: New PerspectivesD'EverandVascular Innervation and Receptor Mechanisms: New PerspectivesRolf UddmanPas encore d'évaluation
- Questions and Answers in Small Animal AnesthesiaD'EverandQuestions and Answers in Small Animal AnesthesiaLesley J. SmithPas encore d'évaluation
- Groundbreaking ProgramDocument1 pageGroundbreaking ProgramJohnBedaLatawanMalecdanPas encore d'évaluation
- GNDocument3 pagesGNJohnBedaLatawanMalecdanPas encore d'évaluation
- How Did Rizal Develop His Nationalist AspirationsDocument3 pagesHow Did Rizal Develop His Nationalist AspirationsJohnBedaLatawanMalecdanPas encore d'évaluation
- Local Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MDDocument40 pagesLocal Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MDJohnBedaLatawanMalecdanPas encore d'évaluation
- Preterm Birth Post Term Growth Restriction Still BirthDocument12 pagesPreterm Birth Post Term Growth Restriction Still BirthJohnBedaLatawanMalecdanPas encore d'évaluation
- Pathophysiology of Burns: Dr. Shiara Ortiz-Pujols Burn Fellow NC Jaycee Burn CenterDocument75 pagesPathophysiology of Burns: Dr. Shiara Ortiz-Pujols Burn Fellow NC Jaycee Burn CenterJohnBedaLatawanMalecdanPas encore d'évaluation
- Ex2 Glucocorticoids: Study Online atDocument3 pagesEx2 Glucocorticoids: Study Online atJohnBedaLatawanMalecdanPas encore d'évaluation
- Pharmacology Eent - Derm PDFDocument2 pagesPharmacology Eent - Derm PDFJohnBedaLatawanMalecdanPas encore d'évaluation
- EENT - Lecture 4bDocument3 pagesEENT - Lecture 4bJohnBedaLatawanMalecdanPas encore d'évaluation
- EENT Outline 4ADocument2 pagesEENT Outline 4AJohnBedaLatawanMalecdanPas encore d'évaluation
- EENT - Nose - Mouth PDFDocument3 pagesEENT - Nose - Mouth PDFJohnBedaLatawanMalecdanPas encore d'évaluation
- ENT Lecture 1Document2 pagesENT Lecture 1JohnBedaLatawanMalecdan100% (1)
- Eent - Ear - LCCWDocument3 pagesEent - Ear - LCCWBeda MalecdanPas encore d'évaluation
- Scripta Medica 46 2 English PDFDocument62 pagesScripta Medica 46 2 English PDFSinisa RisticPas encore d'évaluation
- Critical Incident Reporting and Learning: Key PointsDocument7 pagesCritical Incident Reporting and Learning: Key PointsRavikiran SuryanarayanamurthyPas encore d'évaluation
- Medicina Paliativa Walsh - Comprimido PDFDocument1 507 pagesMedicina Paliativa Walsh - Comprimido PDFMaría Isabel GarcíaPas encore d'évaluation
- A Comprehensive Introduction To Abdominal Acupuncture 1519537480Document5 pagesA Comprehensive Introduction To Abdominal Acupuncture 1519537480Marco GutzPas encore d'évaluation
- FDA narrative requirements for adverse event reportsDocument12 pagesFDA narrative requirements for adverse event reportskandulasatish100% (3)
- Lomitapide PDFDocument125 pagesLomitapide PDFAndrés Menéndez RojasPas encore d'évaluation
- Hepatopulmonary Syndrome (HPS)Document2 pagesHepatopulmonary Syndrome (HPS)Cristian urrutia castilloPas encore d'évaluation
- Paediatrica Indonesiana: Fereza Amelia, Muhammad Ali, Syahril PasaribuDocument5 pagesPaediatrica Indonesiana: Fereza Amelia, Muhammad Ali, Syahril PasaribuAnonymous rKbaHFEPas encore d'évaluation
- Anemia in Pregnancy by MahreeDocument53 pagesAnemia in Pregnancy by MahreesherzadmahreePas encore d'évaluation
- OET SPEAKING GUIDEDocument222 pagesOET SPEAKING GUIDERyu Tse100% (5)
- Proposal of Breast CancerDocument52 pagesProposal of Breast CancerOm Communication SatationeryPas encore d'évaluation
- Conservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesDocument4 pagesConservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Laser Courses, Laser ClassesDocument15 pagesLaser Courses, Laser Classessiya rajPas encore d'évaluation
- Notes Skin Eye Ears Infections MicrobioDocument18 pagesNotes Skin Eye Ears Infections MicrobioChristiel John MagtibayPas encore d'évaluation
- Autopsy Exam Reveals Cause of DeathDocument6 pagesAutopsy Exam Reveals Cause of DeathPRATAPPas encore d'évaluation
- Pcol 2 PrelimsDocument6 pagesPcol 2 PrelimsMa. Andrea Julie AcasoPas encore d'évaluation
- Patofisiologi HIV Dan AIDSDocument24 pagesPatofisiologi HIV Dan AIDSElidia dewiPas encore d'évaluation
- How To Write A Review Article PRISMA GuidelinesDocument5 pagesHow To Write A Review Article PRISMA GuidelinesPuneeth RaghavendraPas encore d'évaluation
- Medical CertificateDocument126 pagesMedical CertificateAnonymous mummYD0% (1)
- Case Hernia2Document19 pagesCase Hernia2ejkohPas encore d'évaluation
- Pictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-GoDocument32 pagesPictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-Go2012Pas encore d'évaluation
- Guidelines Motor Disorders Assessment and InterventionDocument322 pagesGuidelines Motor Disorders Assessment and InterventionWilhelm HeinleinPas encore d'évaluation
- Monograph GarlicDocument2 pagesMonograph GarlicJoann PortugalPas encore d'évaluation
- Vake's Proposal On HepatitisDocument26 pagesVake's Proposal On HepatitisVake MtongaPas encore d'évaluation
- CHD Indian GuidelinesDocument15 pagesCHD Indian GuidelinesDhiraj Kr GauravPas encore d'évaluation
- Heart Rate LabDocument6 pagesHeart Rate LabSteve RodriguesPas encore d'évaluation
- Therapeutic Index For The Doctors of Unani Medicine-2021Document29 pagesTherapeutic Index For The Doctors of Unani Medicine-2021dr Shariq Khan100% (1)
- Jfe Science Abstracts 2019Document31 pagesJfe Science Abstracts 2019api-308218624Pas encore d'évaluation
- Hb transports O2 & CO2; blood doping increases levelsDocument2 pagesHb transports O2 & CO2; blood doping increases levelsAmir BaPas encore d'évaluation
- VI - Members Guide (January 2022)Document22 pagesVI - Members Guide (January 2022)SalomeePas encore d'évaluation