Académique Documents
Professionnel Documents
Culture Documents
Lecture 22 Tissue Engineering
Transféré par
Grace Melissa ChoiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Lecture 22 Tissue Engineering
Transféré par
Grace Melissa ChoiDroits d'auteur :
Formats disponibles
1
3.051J/20.340J
Lecture 22
Tissue Engineering
Tissue Engineering: a field that seeks to replace, repair or enhance biological
function at the scale of a tissue or organ by manipulating cells via their extra-
cellular environment
Objectives:
1. Fulfill a biomechanical role (bone, cartilage)
2. Replace physiological function (liver, nerve)
3. Deliver secretory products (insulin)
4. A combination of the above
3 Main Approaches:
1. Extracorpeal/cell encapsulation (3)
2. In vitro synthesis (1-4)
3. In vivo synthesis (1-4)
2
3.051J/20.340J
1. Extracorpeal/Cell Encapsulation
Method:
1. Encapsulate cells of interest in semipermeable membrane
2. Implant encapsulated device or connect ex vivo
3. Cells secrete product therapy
4. Remove/disconnect device when therapy concluded
O
2
,
nutrients
T cells, B cells
CO
2
,
waste
Cells suspended
in gel
Semipermeable
membrane
Therapeutic
molecules
Immune system: Ab,
Advantages:
Natural theraputic response from living cells
Use of nonhost cellsimmunoisolation
Issues:
Potential for undesirable immune response from adsorption of
complement proteins (similar to blood filtration membranes)
Potential for thrombosis formation
(Anti-coagulants used during ex vivo treatment)
Potential for rupture of implanted devices
3
3.051J/20.340J
Applications Investigated:
Diabetes treatment*
Chronic pain*
Neurodegenerative diseases: ALS (Lou Gehrigs disease, neuromuscular),
Parkinsons, Alzheimers, Huntingtons disease (progressive brain death)
Dwarfism
Anemia/Hemophelia
Macular degeneration (blindness)
Cancer
Liver Failure* * = clinical trials
Device Examples
Encapsulated Islets (Islet Technology Inc., St Paul, MN)
CapCell: implantable membrane-encapsulated islets for glucose regulation
Cells: insulin-producing islets
Use: long-term treatment of diabetes
Device: alginate-based membrane confines islets
Treatment: islets transplanted into patients pancreas; patients
blood flows thru membrane; islets detect glucose level
variations & respond through insulin production
Status: preclinical trials (islet transplantation in clinical trials)
Islet cells
Alginate-based
membranes
Figure by MIT OCW.
4
3.051J/20.340J
Arbios Systems, Inc. (recently acquired from Circe Biomedical)
HepatAssist System: an extracorporeal, bioartificial liver support system
Cells: primary porcine hepatocytes (pig liver cells)
Use: temporary liver function for transplant candidates
Device: hollow fiber bioreactor, oxygenator, pump
Treatment: plasma circulated through bioreactor and
recombined with blood cells
Status: Phase I trials completed
Figure removed for copyright reasons.
5
3.051J/20.340J
2. In vitro Synthesis
Method:
1. Cells seeded in vitro on scaffold device
2. Cells maintained in culture to expand population &
develop tissue organization (in static culture or bioreactors)
3. Device implanted once cell colony is established
4. Device degrades, scaffold replaced by remodeled tissue
Figure by MIT OCW.
6
3.051J/20.340J
Advantages:
Natural theraputic response from living tissues
Permanent therapy
Allows control and quantification not easily obtained in vivo
Issues:
Cell sources
- possibility of rejection
- tumorogenicitycell lines
Full organ restoration challenges (e.g., skin)
Applications Investigated:
Vasculature (resorbable & nonresorbable)
Liver tissue
Nerve tissue
Cartilage*
Cornea*
Bladder*
Skin*
Bone
Ligament
Tendon
Muscle
Heart valve
Heart
Link to list of websites of tissue engineering companies:
http://www.cs.cmu.edu/~webwatch/text_only_industry.html
3.051J/20.340J
3. In vivo synthesis
Method:
1. Implant porous scaffold device
2. Cellular ingrowth in vivo
3. Scaffold replaced by remodeled tissue
Advantages:
Permanent therapy
No cell source problems
Issues:
Uncontrolled biological response to implanted scaffold
Applications Investigated:
Vasculature
Skin*
Bone*
Nerve
Ligament
Cartilage (Knee Meniscus)
7
Natural theraputic response from living tissues
Figure by MIT OCW.
8
3.051J/20.340J
Scaffolds for Tissue Generation
Purpose: replace functions of extracellular matrix (ECM)
ECM functions:
1. cell anchorage
2. cell orientation
3. cell growth
4. mechanical integrity to neo-tissue
5. tissue microenvironment
6. cell differentiation
7. sequester, store & present soluble regulatory proteins
8. blueprint for tissue organization (e.g., biomineralized tissue)
ECM types:
Basal Lamina (basement membrane): directly underlying epithelial cells;
contains laminin, collagen, fibronectin, vitronectin
Stromal tissue (interstitial matrix): provides structural integrity; contains
matrix-secreting cells (fibroblasts, osteoblasts), collagen, elastin, fibrillin,
fibronectin, vitronectin, GAGs, glycoproteins, regulatory proteins
Basal lamina
Stromal tissue
9
3.051J/20.340J
Resorbable Tissue Engineering Scaffolds:
1. Collagen-matrix
e.g., artificial skin
drawback: immunogenic
2. Biodegradable polymers: PLA, PGA, PLGA
e.g., cartilage
drawback: no adhesion sites (can build in RGD)
3. Hydroxyapatite, Bioglass
e.g., bone regeneration
drawback: brittle, low strength
Processing of Tissue Engineering Devices
A. Design Issues
1. Cell density
must be sufficiently high to enable tissue formation, deliver therapy
2. Transport of nutrients/oxygen/waste
nutrients must reach cells within the scaffold/encapsulation device
10
3.051J/20.340J
Blood vessel Scaffold/encapsulation device
C
o
C
nut
x
Limiting distance from nutrients can be gauged from the Thiele modulus, S
(dimensionless ratio of consumption to supply)
D = nutrient diffusivity in device (cm
2
/sec)
S =
k x
2
C
o
= nutrient concentration at source (mol/cm
3
)
DC
k = cell nutrient uptake rate constant (mol/sec/cell)
o
x = distance from nutrient source (bloodstream) (cm)
= cell density in device (cells/cm
3
)
S>>1 cells consume more than can be delivered
S<<1 supply greater than demand
S = 1 supply balances demand; use as limit estimate for device design
A rule of thumb in designing tissue engineering devices: x
max
= 500 m.
11
3.051J/20.340J
3. Mechanical support
- Critical problem for hard tissue scaffolds
- Influenced by
materials choices
processing (orientation of polymers & composites)
4. Tissue organization blueprint
Cell migration guidance
chemical & morphology effects (chemo/hapto/durotaxis)
Cell Patterning
microcontact printing, microlithography
Spatial Organization of Muliple Cell Types
- most organs of more than one cell type
- pattern based on different ligands, ligand densities, ligand affinities
B. Scaffold Fabrication
Objective: Continuous, high-surface area scaffolds
1. Fabrics
Woven/nonwoven fibers
Mechanical interlocking pliable, 3D matrix
Porosity and pore size roughly controlled
12
3.051J/20.340J
2. Bonded fibers
PGA fibers dipped in PLLA/CH
2
Cl
2
solution
Heat treat fibers at T
g,PGA
< T < T
m,PLLA
to bond PGA to PGA
Dissolve away PLLA
Improved mechanical properties over fabrics; similar porosity
3. Freeze-dried Foams
Polymer solution immersed in liquid N
2
phase separation
Frozen solvent sublimates leaving porous scaffold
Pore size ~ of spinodal decomposition controlled pore structure
4. Salt-leached Foams
polymer solution mixed with uniform salt crystals
Solvent evaporates leaving solid polymer/salt composite
Immerse in H
2
O to leach out salt
Controlled porosities up to 93% (< 2 mm thick)
13
3.051J/20.340J
5. 3D Printing
Cast a bed of polymer powder (e.g., PLGA)
"Print" micron-sized droplets of solvent at desired points (chloroform)
Congealed powder solidifies as solvent evaporates
Repeat process, building up 3D structure
Shake out uncongealed powder
Precisely structured micron-porous polymer or ceramic scaffolds
C. Encapsulation Methods
1. Encapsulation Microspheres
Cells attach to surface of polymer microspheres
Cell-coated spheres suspended in weak polycation (polylysine NH
3
+
)
Add polyanion (e.g. sodium alginate, -COO
-
)
Polyelectrolytes form precipitated, porous complex around cells
(Complex coacervation)
Single microbeads contain a few hundred cells
(thousands needed for therapy)
3.051J/20.340J
14
2. Encapsulation Membranes
Cast concentrated solution onto substrate (flat or tubular)
Substrate immersed into a nonsolvent bath
Coagulation of asymmetric membrane results
Cells suspended in gel within sealed membrane tube (length ~ 3 cm) or
disk (dia ~ 2-3 cm)
Semipermeable
membrane
Gel & cells
600-1200 m
~3 cm
Microporous substructure
(mechanical rigidity, high flux)
Dense surface layer (bath side)
(semi-permeable)
15
3.051J/20.340J
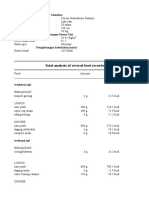
Membrane characteristics
- Molecular weight cutoff: typically ~30-70 kg/mol
(<100 nm dia. pores)
Note: Ab ~150 kg/mol
Molecule/Moiety Size
O
2
, H
2
O, salts 2-3
Lipids, glucose 10
Serum proteins, endotoxins 100
Viruses 1000
Bacteria 10
4
White blood cells, platelets 10
5
- Matrix examples: polysaccharides, alginate/chitosan coacervate,
collagen
- Body: PAN-PVC, PP, polycarbonate, cellulose nitrate, acrylic
- Shape & Size: disks vs. tubes
16
3.051J/20.340J
Disks Tubes
Mass transport Favored diameter
restrictions
Susceptibility to high surface area favored
clotting increases clot propensity
Cell # 50-100M 5M
Cell # required
Diabetes 10
9
Clotting factor 10
7
-10
8
CNS therapies 10
6
-10
7
D. Current Challenges
1. Micromechanical effects
Cell differentiation and growth (especially in load-bearing tissues) can be
affected by micromechanical stresses transmitted by the scaffold
2. Cell function deterioration
3. Cross-application to other areas (gene therapy, drug delivery)
4. Multicellular tissues and organs
- Complex, multicomponent structures (vascularized tissues)
- Regeneration-inducing factors (proteins) only known for blood & bone
17
3.051J/20.340J
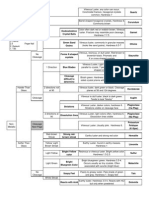
Basic Tissue Cell Types and Functions
Cell type Tissue Function Example
epithelial covers external (ex, skin) &
internal (ex, intestine, blood
vessel) organ surfaces
endothelial cells
connective supports other body tissues;
houses nerves & blood vessels
fibroblasts (ECM
generation),
cartilage, bone
muscle specialized for contraction; smooth, skeletal,
cardiac
nerve generate electrical signals &
secrete neurotransmitters
brain cells,
peripheral nerve
Figure by MIT OCW.
18
3.051J/20.340J
Cell Regeneration Capability
Category Normal Response to Examples
replic. rate injury
renewing/ High;
modest
skin, intenstinal
labile via stem cell mucosa, bone
differentiation marrow
Expanding/
stable
Low
large
endothelium,
fibroblasts,
hepatocytes,
osteoblasts
Static/ None No replication; heart muscle
permanent replaced by scar cells, nerve cells
tissue
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Lab Unit 4 - Cultural Evolution WorksheetDocument2 pagesLab Unit 4 - Cultural Evolution WorksheetGrace Melissa ChoiPas encore d'évaluation
- Classification of The PrimatesDocument1 pageClassification of The PrimatesGrace Melissa ChoiPas encore d'évaluation
- Osteological Identification ReferencesDocument1 pageOsteological Identification ReferencesGrace Melissa ChoiPas encore d'évaluation
- Glossary of Osteological TerminologyDocument1 pageGlossary of Osteological TerminologyGrace Melissa ChoiPas encore d'évaluation
- Unit 5 Primates and Primate Evolution Biology Lecture NotesDocument5 pagesUnit 5 Primates and Primate Evolution Biology Lecture NotesGrace Melissa ChoiPas encore d'évaluation
- Unit 6 Human Biology Biology Lecture NotesDocument6 pagesUnit 6 Human Biology Biology Lecture NotesGrace Melissa ChoiPas encore d'évaluation
- Biology II - Article Abstract 5Document4 pagesBiology II - Article Abstract 5Grace Melissa ChoiPas encore d'évaluation
- Voice: 602.243.0600: Biology I - Course Syllabus South Pointe High SchoolDocument3 pagesVoice: 602.243.0600: Biology I - Course Syllabus South Pointe High SchoolGrace Melissa ChoiPas encore d'évaluation
- Biology I - Course Outline: Unit # Title Subunits Lab PossibilitiesDocument1 pageBiology I - Course Outline: Unit # Title Subunits Lab PossibilitiesGrace Melissa ChoiPas encore d'évaluation
- Metal Flame Tests InfographicDocument1 pageMetal Flame Tests InfographicGrace Melissa ChoiPas encore d'évaluation
- Problem Set 7Document4 pagesProblem Set 7Grace Melissa ChoiPas encore d'évaluation
- Mineral Flowchart RM 2013Document2 pagesMineral Flowchart RM 2013Grace Melissa ChoiPas encore d'évaluation
- Problem Set 4Document4 pagesProblem Set 4Grace Melissa ChoiPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Dearcán Ó Donnghaile: ProfileDocument2 pagesDearcán Ó Donnghaile: Profileapi-602752895Pas encore d'évaluation
- Republic Act No. 10070Document3 pagesRepublic Act No. 10070Ganiela MCPas encore d'évaluation
- CV Ilham AP 2022 CniDocument1 pageCV Ilham AP 2022 CniAzuan SyahrilPas encore d'évaluation
- EC Type-Examination Certificate: Reg.-No.: 01/205/5192.02/18Document11 pagesEC Type-Examination Certificate: Reg.-No.: 01/205/5192.02/18Orlando Ortiz VillegasPas encore d'évaluation
- Decision Trees QuestionsDocument2 pagesDecision Trees QuestionsSaeed Rahaman0% (1)
- Question Bank Chemistry (B.Tech.) : Solid StateDocument10 pagesQuestion Bank Chemistry (B.Tech.) : Solid StatenraiinPas encore d'évaluation
- Excerpts From Roe v. Wade Majority OpinionDocument2 pagesExcerpts From Roe v. Wade Majority OpinioncatherinewangcPas encore d'évaluation
- AD Oracle ManualDocument18 pagesAD Oracle ManualAlexandru Octavian Popîrțac100% (2)
- Performance Management and Strategic Planning:: Organization's Strategic PlanDocument7 pagesPerformance Management and Strategic Planning:: Organization's Strategic PlanSara AbidPas encore d'évaluation
- Air Conditioning Is Inoperative, Fault Code 91eb11 or 91eb15 Is StoredDocument5 pagesAir Conditioning Is Inoperative, Fault Code 91eb11 or 91eb15 Is Storedwasim AiniaPas encore d'évaluation
- Report On Marketing of ArecanutDocument22 pagesReport On Marketing of ArecanutsivakkmPas encore d'évaluation
- Exercise 6Document2 pagesExercise 6Satyajeet PawarPas encore d'évaluation
- SCL NotesDocument4 pagesSCL NotesmayaPas encore d'évaluation
- FRMUnit IDocument17 pagesFRMUnit IAnonPas encore d'évaluation
- Writing Workshop G7 PDFDocument12 pagesWriting Workshop G7 PDFJobell AguvidaPas encore d'évaluation
- Fire Safety: Good Servant But A Bad MasterDocument143 pagesFire Safety: Good Servant But A Bad MasterernmrajaPas encore d'évaluation
- 09B Mechanical Properties of CeramicsDocument13 pages09B Mechanical Properties of CeramicsAhmed AliPas encore d'évaluation
- Rekapan Belanja JKNDocument5 pagesRekapan Belanja JKNAPOTEK PUSKESMAS MALEBERPas encore d'évaluation
- Retrenchment in Malaysia Employers Right PDFDocument8 pagesRetrenchment in Malaysia Employers Right PDFJeifan-Ira DizonPas encore d'évaluation
- Akin To PityDocument356 pagesAkin To PityPaul StewartPas encore d'évaluation
- Annual Sustainability Report 2022-23 FinalDocument93 pagesAnnual Sustainability Report 2022-23 FinalLakshay JajuPas encore d'évaluation
- Industrial SpecialtiesDocument103 pagesIndustrial SpecialtiesRahul ThekkiniakathPas encore d'évaluation
- Tugas Gizi Caesar Nurhadiono RDocument2 pagesTugas Gizi Caesar Nurhadiono RCaesar 'nche' NurhadionoPas encore d'évaluation
- Urinary Tract Infection (UTI) - 4 Nursing Diagnosis InterventionsDocument4 pagesUrinary Tract Infection (UTI) - 4 Nursing Diagnosis InterventionsEricsonMitra0% (2)
- GEC PE 3 ModuleDocument72 pagesGEC PE 3 ModuleMercy Anne EcatPas encore d'évaluation
- 56.vocal Warmup Log For Belt Your FaceDocument5 pages56.vocal Warmup Log For Belt Your FaceAlinutza AlinaPas encore d'évaluation
- What Is A Solar Storm?Document2 pagesWhat Is A Solar Storm?Shawn SriramPas encore d'évaluation
- All Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationDocument7 pagesAll Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationRakesh KumarPas encore d'évaluation
- Water Quantity Estimation PDFDocument3 pagesWater Quantity Estimation PDFOladunni AfolabiPas encore d'évaluation
- Upper Gi f1 Survival GuideDocument1 pageUpper Gi f1 Survival GuideNathan Hovis JeffreysPas encore d'évaluation