Académique Documents
Professionnel Documents
Culture Documents
Kontrasepsi PDF
Transféré par
Triponia0 évaluation0% ont trouvé ce document utile (0 vote)
175 vues5 pagesCervical intraepithelial neoplasia (CIN) is initiated by human papillomavirus (HPV) infection. Sexual and reproductive behaviours, as well as hormone levels and hormone receptors, are known to afect the development of CIN. Use of condoms may reduce the risk of CIN among women highly susceptible to HPV infection.
Description originale:
Titre original
kontrasepsi.pdf
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentCervical intraepithelial neoplasia (CIN) is initiated by human papillomavirus (HPV) infection. Sexual and reproductive behaviours, as well as hormone levels and hormone receptors, are known to afect the development of CIN. Use of condoms may reduce the risk of CIN among women highly susceptible to HPV infection.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
175 vues5 pagesKontrasepsi PDF
Transféré par
TriponiaCervical intraepithelial neoplasia (CIN) is initiated by human papillomavirus (HPV) infection. Sexual and reproductive behaviours, as well as hormone levels and hormone receptors, are known to afect the development of CIN. Use of condoms may reduce the risk of CIN among women highly susceptible to HPV infection.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 5
INTRODUCTION
Cervical intraepithelial neoplasia (CIN) is initiated by human
papillomavirus (HPV) infection [1]. Sexual and reproductive
behaviours, as well as hormone levels and hormone receptors,
are known to afect the development of CIN [1]. Besides vac-
cination, use of condoms is an effective barrier against HPV
infection [2], and may reduce the risk of CIN among women
highly susceptible to HPV infection [3]. Its protective effect
needs to be ascertained on other women.
The transforming zone of the cervix, where HPV initiates CIN,
is sex-hormone dependent [1]. Steroid hormones including
progesterone, infuence HPV actions and indirectly contribute
to HPV-related CIN [1]. Despite the widespread use of oral
contraceptives and its protective effect against cancers
afecting female, such as endometrial cancer [4,5], there is no
consensus on the use of oral contraceptives and the health
of the cervix [6-8]. While a joint report by the World Cancer
Research Fund and the American Institute for Cancer Research
suggested a possible increased risk of cervical cancer [9], the
World Health Organization did not recommend discontinuing
the use of oral contraceptives as its use outweighed its risk [10].
Indeed, evidence is lacking on the relationship between oral
Condom and oral contraceptive use and risk of cervical
intraepithelial neoplasia in Australian women
Hui Jun Chih
1
, Andy H. Lee
1
, Linda Colville
1
, Daniel Xu
2
, Colin W. Binns
1
1
School of Public Health,
2
Department of Medical Education, Faculty of Health Sciences, Curtin University, Perth, Australia
Received Jul 26, 2013, Revised Aug 19, 2013, Accepted Aug 27, 2013
Correspondence to Hui Jun Chih
School of Public Health, Curtin University, GPO Box U1987, Perth, WA 6845,
Australia. E-mail: h.chih@curtin.edu.au
Copyright 2014. Asian Society of Gynecologic Oncology, Korean Society of Gynecologic Oncology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and
reproduction in any medium, provided the original work is properly cited.
www.ejgo.org
Objective: To assess the association between condom use and oral contraceptive consumption and the risk of cervical
intraepithelial neoplasia (CIN).
Methods: A cross-sectional study was conducted in Perth clinics. A total of 348 women responded to the structured
questionnaire. Information sought included demographic and lifestyle characteristics such as the use of condom for
contraception, consumption of oral contraceptive, and duration of oral contraceptive usage. Crude and adjusted odds ratio (OR)
and associated 95% confdence interval (CI) were calculated using unconditional logistic regression models and reported as
estimates of the relative risk.
Results: The prevalence of CIN was found to be 15.8%. The duration of oral contraceptive consumption among women
with abnormal Papanicolaou (Pap) smear result indicating CIN was significantly shorter than those without abnormal Pap
smear result (meanSD, 5.65.2 years vs. 8.27.6 years; p=0.002). Comparing to 3 years usage, prolonged consumption of
oral contraceptive for 10 years reduced the risk of CIN (p=0.012). However, use of condom for contraception might not be
associated with a reduced risk of CIN after accounting for the efects of confounding factors (adjusted OR, 0.52; 95% CI, 0.05 to
5.11; p=0.577).
Conclusion: Use of oral contraceptives, but not condoms, for contraception appeared to be inversely associated with CIN.
Prolonged use of oral contraceptive demonstrated its benefts of reducing the risk of CIN.
Keywords: Australia, Cervical intraepithelial neoplasia, Comparative study, Condom, Oral contraceptive
Original Article
J Gynecol Oncol Vol. 25, No. 3:183-187
http://dx.doi.org/10.3802/jgo.2014.25.3.183
pISSN 2005-0380eISSN 2005-0399
Hui Jun Chih, et al.
http://dx.doi.org/10.3802/jgo.2014.25.3.183 184www.ejgo.org
contraceptive consumption and the risk of CIN [11,12]. There-
fore, the present study aims to investigate whether the use
of non-clinical contraception, particularly condoms and oral
contraceptives, is associated with any risk of CIN in Australian
women.
MATERIALS AND METHODS
Community-dwelling adult women within metropolitan
Perth, Western Australia who had a Papanicolaou (Pap) smear
test at five medical centres and clinics (Parkwood Medical
Centre; Murdoch Health and Counselling Service; Fremantle
Womens Health; Womens Health Services, Northbridge;
Womens Health Service Incorporation, Gosnells) were ap-
proached by their general practitioners. Temporary residents,
women below 18 years of age, women who had a history
of breast, ovarian or endometrial cancer, and those with a
chronic debilitating disease, were excluded from this study.
Following consecutive referrals from the general practitioners,
and further screening and subsequent withdrawals, a total
of 348 women were eventually recruited and signed the
informed consent form. An appointment for interview was
made with each participant by the third author. These face-
to-face interviews were held at either the clinic of recruitment
or the participants residences. All participants were assured
of confidentiality but blinded to the research hypothesis.
The study protocol was approved by the Human Research
Ethics Committee at Curtin University (approval number HR
118/2006).
A structured questionnaire was used to collect information
on demographic and lifestyle characteristics. In relation
to contraception, information sought included the use of
condom for contraception (no, yes), consumption of oral
contraceptive (never, ever), and duration of oral contraceptive
usage (years). Specifcally, the participants were asked What
form of contraception, if any, do you use? The choices were:
I use condoms (categorized as 'yes'), I use another method
of contraception (categorized as 'no'), and None, I dont use
contraception (categorized as 'no'). For the consumption
of oral contraceptive, the participants were asked Are you
currently using, or have used, the oral contraceptive pill?
In the context of duration of oral contraceptive usage, the
participants were asked How many years in total have you
ever taken the oral contraceptive pill? Information about
other sexual history was not asked as it did not contribute
directly to CIN [13-15] and may cause embarrassment and
burden to the participants. The Pap smear test outcome was
classifed as normal or CIN based on the result reported by
the accredited St John of God Pathology, Murdoch, Western
Australia, Australia. The Pap smear status was defned accord-
ing to the Australian Modifed Bethesda System 2004 [16].
Descriptive statistics were frst used to summarize the char-
acteristics of the participants. Chi-square and independent
samples t-tests were then applied to compare the variables
between women with normal Pap smear status and with
abnormal Pap smear result indicating CIN. To assess the
effects of condom and oral contraceptive use on CIN risk,
including duration of oral contraceptive consumption, the
Pap smear test outcome was analysed by three separate
unconditional logistic regression models. Duration of cumula-
tive oral contraceptive consumption was categorized based
on the distribution of women with normal Pap smear status
into three increasing levels of exposure (3 years, 3.1 to 9.9
years, and 10 years). Each ftted multivariable model included
terms for age (years), age of frst pregnancy (years), smoking
duration (years), annual family income (<AUD $15,000, AUD
$15,000 to 60,000, >AUD $60,000), hormone replacement
therapy (never use, ever use), and number of pregnancies.
These confounding variables were plausible risk factors identi-
fed from the literature or from our univariate analyses. Crude
and adjusted odds ratio (OR) and associated 95% confdence
interval (CI) were reported as estimates of the relative risk. All
statistical analyses were performed using the IBM SPSS ver. 20
(IBM Co., Armonk, NY, USA).
RESULTS
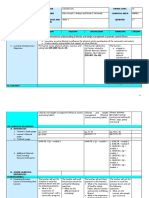
Table 1 presents characteristics of the 348 participants by
CIN status. The prevalence of CIN was found to be 15.8%
(55/348) in the present study. Most of the participants were
married (99%) and never smoked (62%). Women with CIN
(n=55) tended to be younger (p<0.001) and earned less
(p=0.019) than those without CIN (n=293). Body mass index,
lifestyle and reproductive characteristics were similar between
the two groups (p>0.05).
The duration of cumulative oral contraceptive consumption
among women without CIN was significantly longer than
those with CIN (meanSD, 8.27.6 years vs. 5.65.2 years;
p=0.002). Logistic regression results in Table 2 further showed
that long term consumption of oral contraceptive for at least
10 years was associated with a reduced risk; the adjusted OR
was 0.17 (95% CI, 0.04 to 0.69) when compared to 3 years or
less usage. However, use of condom for contraception might
not be associated with a reduced risk of CIN after accounting
for the efects of confounding factors (adjusted OR, 0.52; 95%
CI, 0.05 to 5.11).
Contraception and CIN risk in Australian women
J Gynecol Oncol Vol. 25, No. 3:183-187 www.ejgo.org185
Table 1. Characteristics of participants by CIN status
Variable Without CIN (n=293) With CIN (n=55) p-value*
Age (yr) 46.813.7 38.815.2 <0.001
Age of frst menarche (yr) 13.01.5 13.21.6 0.300
Age of frst pregnancy (yr) 25.25.3 24.55.5 0.435
No. of pregnancies 2.11.6 1.91.9 0.361
Body mass index (kg/m
2
)
26.15.42 25.15.0 0.223
Smoking duration (yr)
8.510.05 10.76.6 0.111
Smoking status 0.143
Never smoked 187 (63.8) 29 (52.7)
Current smoker 29 (9.9) 10 (18.2)
Ex-smoker 77 (26.3) 16 (29.1)
Marital status 0.119
Never married/de facto 2 (0.7) 2 (3.6)
Married 291 (99.3) 53 (96.4)
Nationality 0.149
Australia/New Zealand 189 (64.5) 41 (74.5)
Others 104 (35.5) 14 (25.5)
Annual family income (AUD $)
0.019
<15,000 14 (4.8) 7 (12.7)
15,000-60,000 135 (46.6) 30 (54.5)
>60,000 141 (48.6) 18 (32.7)
Hormone replacement therapy
0.290
Never use 213 (73.2) 44 (80.0)
Ever use 78 (26.8) 11 (20.0)
Values are presented as meanSD or number (%).
AUD, Australian dollar; CIN, cervical intraepithelial neoplasia.
*Chi-square or t-test for diference between two groups.
Missing data present.
Table 2. Association between contraception use and risk of CIN in Australian women
Variable Without CIN (n=293) With CIN (n=55) Crude OR (95% CI) Adjusted* OR (95% CI) p-value
Duration of cumulative oral
contraceptive consumption (yr)
0.012
3 99 (33.8) 25 (45.5) 1.00 1.00
>3 and <10 83 (28.3) 18 (32.7) 0.859 (0.438-1.682) 0.339 (0.093-1.235)
10 111 (37.9) 12 (21.8) 0.428 (0.204-0.897) 0.169 (0.042-0.689)
Consumption of oral contraceptive 0.221
Never use 243 (82.9) 43 (78.2) 1.00 1.00
Ever use 50 (17.1) 12 (21.8) 1.356 (0.668-2.755) 0.256 (0.029-2.267)
Use of condom for contraception 0.577
No 261 (89.1) 50 (90.9) 1.00 1.00
Yes 32 (10.9) 5 (9.1) 0.816 (0.303-2.195) 0.523 (0.054-5.108)
Values are presented as number (%).
AUD, Australian dollar; CI, confdence interval; CIN, cervical intraepithelial neoplasia; OR, odds ratio.
*Adjusted for age (yr), age of frst pregnancy (yr), smoking duration (yr), annual family income (<AUD $15,000, AUD $15,000-60,000, >AUD
$60,000), hormone replacement therapy (never use, ever use), and number of pregnancies.
Hui Jun Chih, et al.
http://dx.doi.org/10.3802/jgo.2014.25.3.183 186www.ejgo.org
DISCUSSION
In this study, cumulative use of oral contraceptive was longer
amongst women with CIN. After controlling for plausible con-
founding factors, prolonged oral contraceptive consumption
was found to be inversely associated with the risk of CIN in
Australian women, consistent with a previous report of a de-
creased risk of CIN with use over 5 years [17]. The potentially
protective mechanism may be attributable to the hormonal
efect of oral contraceptive on HPV DNA expression and the
viscosity of the cervical mucus [18,19]. Estrogen can protect
the mucosal immune system against early HPV infection [17],
while the viscosity of the mucus affects the penetration of
foreign bodies including HPV [19]. The inverse association of
the risk of CIN with long term oral contraceptive consumption
could also be due to the relatively stable sexual relationships
among middle-aged women, who tended to prefer oral
contraception to the use of condoms [20]. Previous studies
have found the use of oral contraceptive to be not associated
with the risk of CIN [21-26], while some studies reported that
an increased risk was plausible for high grade CIN [27,28].
The association between use of condom for contraception
and risk of CIN was not signifcant. Nevertheless, the potential
benefcial efect of condom use against CIN has been demon-
strated in other studies [19,29]. Evidence showed that barrier
methods of contraception such as condom could increase the
clearance of HPV infection [30,31], thereby reducing the risk
of CIN [3]. The relatively small sample size of this study might
explain the apparent lack of association observed.
The strength of this study includes using standardized que-
stionnaire, classification of the Australian Modified Bethesda
System and the accredited pathology. The face-to-face inter-
views by a single investigator (third author) also eliminated
inter-interviewer bias. A major limitation is the small sample
cross-sectional retrospective design so that cause-effect
relationship cannot be established. Another limitation is the
one-of assessment of Pap smear status as HPV infection can
be transient and CIN may regress [32]. In addition, the types of
oral contraceptive used by the participants were not recorded.
Interaction between the estrogen and progesterone receptors
and the oral contraceptive can affect the physiology of the
cervical epithelium [33]. Similarly, ethnicity may play a role in
the disease etiology. Large-scale multiethnic longitudinal age-
matched studies including detailed information on sexual
history and behavior, together with periodical assessments of
Pap smear status, are recommended to confrm the associa-
tion of risk of CIN with various use of contraception for women
from various backgrounds. Both developed and developing
countries should be targeted for consideration. Despite these
limitations, the present study found that prolonged oral
contraceptive use was associated with a decreased risk of CIN.
As the protective benefts of oral contraceptives, and possibly
that of condom, outweighed the adverse effect, their use
should not be discontinued without consultation with general
practitioners.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was
reported.
ACKNOWLEDGMENTS
The authors are grateful for the in-kind support provided
by Curtin University and the participants for their voluntary
participation in this study.
REFERENCES
1. Monsonego J, Magdelenat H, Catalan F, Coscas Y, Zerat L, Sastre X.
Estrogen and progesterone receptors in cervical human papillo-
mavirus related lesions. Int J Cancer 1991;48:533-9.
2. Parazzini F, Negri E, La Vecchia C, Fedele L. Barrier methods of
contraception and the risk of cervical neoplasia. Contraception
1989;40:519-30.
3. Coker AL, Sanders LC, Bond SM, Gerasimova T, Pirisi L. Hormonal
and barrier methods of contraception, oncogenic human pa-
pillo maviruses, and cervical squamous intraepithelial lesion de-
velop ment. J Womens Health Gend Based Med 2001;10:441-9.
4. Grimbizis GF, Tarlatzis BC. The use of hormonal contraception
and its protective role against endometrial and ovarian cancer.
Best Pract Res Clin Obstet Gynaecol 2010;24:29-38.
5. Pasalich M, Su D, Binns CW, Lee AH. Reproductive factors for
ovarian cancer in southern Chinese women. J Gynecol Oncol
2013;24:135-40.
6. Schneider HP, Mueck AO, Kuhl H. IARC monographs program
on carcinogenicity of combined hormonal contraceptives and
menopausal therapy. Climacteric 2005;8:311-6.
7. Rieck G, Fiander A. The efect of lifestyle factors on gynaecological
cancer. Best Pract Res Clin Obstet Gynaecol 2006;20:227-51.
8. Webberley H, Mann M. Oral contraception. Curr Obstet Gynaecol
2003;13:21-9.
9. World Cancer Research Fund, American Institute for Cancer
Research. Food, nutrition, physical activity, and the prevention of
cancer: a global perspective. Washington DC: American Institute
for Cancer Research; 2007.
10. Gadducci A, Barsotti C, Cosio S, Domenici L, Riccardo Genazzani A.
Contraception and CIN risk in Australian women
J Gynecol Oncol Vol. 25, No. 3:183-187 www.ejgo.org187
Smoking habit, immune suppression, oral contraceptive use, and
hormone replacement therapy use and cervical carcinogenesis:
a review of the literature. Gynecol Endocrinol 2011;27:597-604.
11. Folger SG, Curtis KM, Tepper NK, Gaffield ME, Marchbanks PA.
Guidance on medical eligibility criteria for contraceptive use:
identifcation of research gaps. Contraception 2010;82:113-8.
12. Miller K, Blumenthal P, Blanchard K. Oral contraceptives and cervical
cancer: critique of a recent review. Contraception 2004;69:347-51.
13. Kjellberg L, Hallmans G, Ahren AM, Johansson R, Bergman F,
Wadell G, et al. Smoking, diet, pregnancy and oral contraceptive
use as risk factors for cervical intra-epithelial neoplasia in relation
to human papillomavirus infection. Br J Cancer 2000;82:1332-8.
14. Kim J, Kim BK, Lee CH, Seo SS, Park SY, Roh JW. Human papillo-
mavirus genotypes and cofactors causing cervical intraepithelial
neoplasia and cervical cancer in Korean women. Int J Gynecol
Cancer 2012;22:1570-6.
15. Ma LT, Campbell GA, Richardson G, Schnadig VJ. Should high-
risk adolescents have Papanicolaou tests? Cancer Cytopathol
2013;121:432-9.
16. National Health and Medical Research Council. Screening to
prevent cervical cancer: guidelines for the management of asy m-
ptomatic women with screen detected abnormalities. Canberra:
Commonwealth of Australia; 2005.
17. Schiff M, Miller J, Masuk M, van Asselt King L, Altobelli KK,
Wheeler CM, et al. Contraceptive and reproductive risk factors for
cervical intraepithelial neoplasia in American Indian women. Int J
Epidemiol 2000;29:983-90.
18. Guven S, Kart C, Guvendag Guven ES, Gunalp GS. The underlying
cause of cervical cancer in oral contraceptive users may be
related to cervical mucus changes. Med Hypotheses 2007;69:550-
2.
19. Schmeink CE, Massuger LF, Lenselink CH, Quint WG, Melchers
WJ, Bekkers RL. Effect of the menstrual cycle and hormonal
contraceptives on human papillomavirus detection in young,
unscreened women. Obstet Gynecol 2010;116:67-75.
20. Read C, Bateson D, Weisberg E, Estoesta J. Contraception and
pregnancy then and now: examining the experiences of a cohort
of mid-age Australian women. Aust N Z J Obstet Gynaecol
2009;49:429-33.
21. Kazerooni T, Mosalaee A. Does contraceptive method change
the Pap smear fnding? Contraception 2002;66:243-6.
22. Moscicki AB, Hills N, Shiboski S, Powell K, Jay N, Hanson E, et al.
Risks for incident human papillomavirus infection and low-grade
squamous intraepithelial lesion development in young females.
JAMA 2001;285:2995-3002.
23. Syrjanen K, Shabalova I, Petrovichev N, Kozachenko V, Zakharova
T, Pajanidi J, et al. Oral contraceptives are not an independent
risk factor for cervical intraepithelial neoplasia or high-risk human
papillomavirus infections. Anticancer Res 2006;26(6C):4729-40.
24. Harris TG, Miller L, Kulasingam SL, Feng Q, Kiviat NB, Schwartz
SM, et al. Depot-medroxyprogesterone acetate and combined
oral contraceptive use and cervical neoplasia among women
with oncogenic human papillomavirus infection. Am J Obstet
Gynecol 2009;200:489.e1-8.
25. Frega A, Scardamaglia P, Piazze J, Cerekja A, Pacchiarotti A, Verrico
M, et al. Oral contraceptives and clinical recurrence of human
papillomavirus lesions and cervical intraepithelial neoplasia
following treatment. Int J Gynaecol Obstet 2008;100:175-8.
26. Longatto-Filho A, Hammes LS, Sarian LO, Roteli-Martins C,
Derchain SF, Erzen M, et al. Hormonal contraceptives and the
length of their use are not independent risk factors for high-
risk HPV infections or high-grade CIN. Gynecol Obstet Invest
2011;71:93-103.
27. Moscicki AB, Ma Y, Wibbelsman C, Powers A, Darragh TM, Farhat
S, et al. Risks for cervical intraepithelial neoplasia 3 among
adolescents and young women with abnormal cytology. Obstet
Gynecol 2008;112:1335-42.
28. Samir R, Asplund A, Tot T, Pekar G, Hellberg D. Oral contraceptive
and progestin-only use correlates to tissue tumor marker ex-
pression in women with cervical intraepithelial neoplasia. Con-
traception 2012;85:288-93.
29. Gavric-Lovrec V, Takac I. Use of various contraceptives and human
papillomavirus 16 and 18 infections in women with cervical
intraepithelial neoplasia. Int J STD AIDS 2010;21:424-7.
30. Richardson H, Abrahamowicz M, Tellier PP, Kelsall G, du Berger R,
Ferenczy A, et al. Modifable risk factors associated with clearance
of type-specific cervical human papillomavirus infections in a
cohort of university students. Cancer Epidemiol Biomarkers Prev
2005;14:1149-56.
31. Munk AC, Gudlaugsson E, Ovestad IT, Lovslett K, Fiane B, Hidle
Bv, et al. Interaction of epithelial biomarkers, local immune
response and condom use in cervical intraepithelial neoplasia
2-3 regression. Gynecol Oncol 2012;127:489-94.
32. Smith JS, Green J, Berrington de Gonzalez A, Appleby P, Peto
J, Plummer M, et al. Cervical cancer and use of hormonal
contraceptives: a systematic review. Lancet 2003;361:1159-67.
33. Green J, Berrington de Gonzalez A, Smith JS, Franceschi S,
Appleby P, Plummer M, et al. Human papillomavirus infection
and use of oral contraceptives. Br J Cancer 2003;88:1713-20.
Vous aimerez peut-être aussi
- Contraception for the Medically Challenging PatientD'EverandContraception for the Medically Challenging PatientRebecca H. AllenPas encore d'évaluation
- Intl Journal of Cancer - 2021 - Yang - Intrauterine Device Use and Risk of Ovarian Cancer Results From The New EnglandDocument9 pagesIntl Journal of Cancer - 2021 - Yang - Intrauterine Device Use and Risk of Ovarian Cancer Results From The New EnglandAnggie DiniayuningrumPas encore d'évaluation
- 43 FullDocument9 pages43 Fullnayeta levi syahdanaPas encore d'évaluation
- Urban2012 PDFDocument12 pagesUrban2012 PDFRemaja IslamPas encore d'évaluation
- Pi Is 0002937817301795Document9 pagesPi Is 0002937817301795trikurniati27Pas encore d'évaluation
- Am. J. Epidemiol.-2009-Rosenberg-473-9Document7 pagesAm. J. Epidemiol.-2009-Rosenberg-473-9reynomoralPas encore d'évaluation
- Cervical CA Proposal Jan152010Document21 pagesCervical CA Proposal Jan152010redblade_88100% (2)
- Effectiveness of Long-Acting Reversible Contraception: Original ArticleDocument10 pagesEffectiveness of Long-Acting Reversible Contraception: Original ArticleshabrundjamielPas encore d'évaluation
- Contra 2Document10 pagesContra 2Macy EarnestPas encore d'évaluation
- Oral Contraceptives and Cancer Risk: Questions and Answers: Key PointsDocument21 pagesOral Contraceptives and Cancer Risk: Questions and Answers: Key PointsTyan Caery QuePas encore d'évaluation
- Unintended Pregnancy Among HIV PDFDocument11 pagesUnintended Pregnancy Among HIV PDFTitin JuherniPas encore d'évaluation
- Oral Contraceptive Cancer RisksDocument3 pagesOral Contraceptive Cancer RisksJamie Paola SevillaPas encore d'évaluation
- Antidepressant Medication Use and Breast Cancer RiskDocument6 pagesAntidepressant Medication Use and Breast Cancer RiskinloesPas encore d'évaluation
- Manuscript 1 Promoting Family Planning: Contraceptive TechnologyDocument6 pagesManuscript 1 Promoting Family Planning: Contraceptive Technologyelfera09Pas encore d'évaluation
- research final draftDocument15 pagesresearch final draftapi-736869233Pas encore d'évaluation
- Mohllajee 2006Document12 pagesMohllajee 2006Rika Yulizah GobelPas encore d'évaluation
- Risiko Riwayat Keluarga Dan Penggunaan Alat Kontrasepsi Hormonal Terhadap Kanker Payudara Di RSD Dr. Soebandi Jember Nelyta OktavianisyaDocument7 pagesRisiko Riwayat Keluarga Dan Penggunaan Alat Kontrasepsi Hormonal Terhadap Kanker Payudara Di RSD Dr. Soebandi Jember Nelyta Oktavianisyasulas MiPas encore d'évaluation
- Jurnal ObgynDocument6 pagesJurnal ObgynHuuriyah 'Aathifah FaatinPas encore d'évaluation
- Aab OvariumDocument3 pagesAab OvariumAgustinus FatollaPas encore d'évaluation
- NIH Public Access: Recent Oral Contraceptive Use by Formulation and Breast Cancer Risk Among Women 20-49 Years of AgeDocument21 pagesNIH Public Access: Recent Oral Contraceptive Use by Formulation and Breast Cancer Risk Among Women 20-49 Years of AgeM Iqbal EffendiPas encore d'évaluation
- Ca Dan KontrasepsiDocument8 pagesCa Dan Kontrasepsidokter wawanPas encore d'évaluation
- ResearchDocument15 pagesResearchapi-736973985Pas encore d'évaluation
- Gyne - Obs-Relation Between OCPs and CancerDocument16 pagesGyne - Obs-Relation Between OCPs and CancerOstazPas encore d'évaluation
- A Comparative Analysis of ClassificationDocument12 pagesA Comparative Analysis of ClassificationSharmi BhatPas encore d'évaluation
- Finalpaper HealthchangeDocument8 pagesFinalpaper Healthchangeapi-500609372Pas encore d'évaluation
- Cancer Medicine: Pioglitazone and Bladder Cancer Risk: A Systematic Review and Meta-AnalysisDocument11 pagesCancer Medicine: Pioglitazone and Bladder Cancer Risk: A Systematic Review and Meta-AnalysisMaria MontoyaPas encore d'évaluation
- Hormonal Contraceptive Use Related To Breast Cancer Among Women in Indonesia: A Nationwide StudyDocument6 pagesHormonal Contraceptive Use Related To Breast Cancer Among Women in Indonesia: A Nationwide StudyIJPHSPas encore d'évaluation
- Winer2016 PDFDocument8 pagesWiner2016 PDFAlex AdamiteiPas encore d'évaluation
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsD'EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsÉvaluation : 5 sur 5 étoiles5/5 (9)
- Main PDFDocument10 pagesMain PDFBiaggi NugrahaaPas encore d'évaluation
- Prospektive Cohort Study of Risk Factors For Breast Cancer in Post Menopausal WomenDocument9 pagesProspektive Cohort Study of Risk Factors For Breast Cancer in Post Menopausal WomenAdi KaswadiPas encore d'évaluation
- Research Project 1Document9 pagesResearch Project 1Sangeeta SahaPas encore d'évaluation
- Hubungan Pemakaian Kontrasepsi Hormonal Dan PDFDocument7 pagesHubungan Pemakaian Kontrasepsi Hormonal Dan PDFAmhar Syukur Rizki100% (2)
- Clinical Oncology: World Journal ofDocument13 pagesClinical Oncology: World Journal ofMATEJ MAMICPas encore d'évaluation
- Benefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsD'EverandBenefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsPas encore d'évaluation
- Oral Contraceptive Use and Breast Cancer ADocument13 pagesOral Contraceptive Use and Breast Cancer AMuhammad MaulanaPas encore d'évaluation
- Fruits and Vegetables and Cervical Cancer: A Systematic Review and Meta-AnalysisDocument14 pagesFruits and Vegetables and Cervical Cancer: A Systematic Review and Meta-AnalysisSf AkhadiyatiPas encore d'évaluation
- Oup Accepted Manuscript 2018Document7 pagesOup Accepted Manuscript 2018FaidurrahmanPas encore d'évaluation
- Annotated BibDocument4 pagesAnnotated Bibapi-458216829Pas encore d'évaluation
- Correlation Between Age at First Menarche and Breast Cancer in Dr. Cipto Mangunkusumo National General Hospital Jakarta in 2010-2014Document6 pagesCorrelation Between Age at First Menarche and Breast Cancer in Dr. Cipto Mangunkusumo National General Hospital Jakarta in 2010-2014Irda Sudistiani PutriPas encore d'évaluation
- Research ArticleDocument14 pagesResearch ArticleShubhaDavalgiPas encore d'évaluation
- Knowledge, Attitudes, and Practices Regarding Cervical Cancer and Screening Among Women Visiting Primary Health Care Centres in BahrainDocument6 pagesKnowledge, Attitudes, and Practices Regarding Cervical Cancer and Screening Among Women Visiting Primary Health Care Centres in BahrainAnonymous N74eaOhdfkPas encore d'évaluation
- Phytoestrogen Consumption From Foods and Supplements and Epithelial Ovarian Cancer Risk: A Population-Based Case Control StudyDocument9 pagesPhytoestrogen Consumption From Foods and Supplements and Epithelial Ovarian Cancer Risk: A Population-Based Case Control StudyDiana LeonPas encore d'évaluation
- 38565-Article Text-106129-3-10-20200930Document5 pages38565-Article Text-106129-3-10-20200930kirito azumaPas encore d'évaluation
- Supportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachD'EverandSupportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachJames H. FeusnerPas encore d'évaluation
- Weight Gain and Menstrual Abnormalities Between Users of Depo-Provera and NoristeratDocument6 pagesWeight Gain and Menstrual Abnormalities Between Users of Depo-Provera and NoristeratMauricio Lopez MejiaPas encore d'évaluation
- Dietary Inflammatory Potential and Risk of Breast Cancer A Population Based Case Control Study in France Cecile StudyDocument25 pagesDietary Inflammatory Potential and Risk of Breast Cancer A Population Based Case Control Study in France Cecile Studymaria.panevayahoo.comPas encore d'évaluation
- Hormonal Contraception and Sexual DesireDocument19 pagesHormonal Contraception and Sexual Desirebustanul aswatPas encore d'évaluation
- Abel Man 2020Document6 pagesAbel Man 2020Redouane idrissiPas encore d'évaluation
- Cervical Cytology in Women With Abnormal Cervix.: Dr. Veena Rahatgaonkar, Dr. Savita MehendaleDocument4 pagesCervical Cytology in Women With Abnormal Cervix.: Dr. Veena Rahatgaonkar, Dr. Savita MehendaleIOSR Journal of PharmacyPas encore d'évaluation
- Active Surveillance for Localized Prostate Cancer: A New Paradigm for Clinical ManagementD'EverandActive Surveillance for Localized Prostate Cancer: A New Paradigm for Clinical ManagementPas encore d'évaluation
- Condom Use Promotes Regression of Cervical Intraepithelial Neoplasia and Clearance of Human Papillomavirus: A Randomized Clinical TrialDocument6 pagesCondom Use Promotes Regression of Cervical Intraepithelial Neoplasia and Clearance of Human Papillomavirus: A Randomized Clinical TrialAdi ParamarthaPas encore d'évaluation
- 503 837 1 PBDocument14 pages503 837 1 PB5m7m2c2kryPas encore d'évaluation
- Research Open AccessDocument8 pagesResearch Open AccessHafim RasydinPas encore d'évaluation
- Bacterial Vaginosis Draft Evidence ReviewDocument206 pagesBacterial Vaginosis Draft Evidence Reviewaisa mutiaraPas encore d'évaluation
- The Association Between Current Low-Dose Oral Contraceptive Pills and Periodontal Health: A Matched-Case-Control StudyDocument8 pagesThe Association Between Current Low-Dose Oral Contraceptive Pills and Periodontal Health: A Matched-Case-Control StudyAnna María RivasPas encore d'évaluation
- Knowledge Discovery From Breast Cancer DatabaseDocument5 pagesKnowledge Discovery From Breast Cancer DatabaseIOSRjournalPas encore d'évaluation
- Literature Review On Cervical Cancer ScreeningDocument4 pagesLiterature Review On Cervical Cancer Screeningbqvlqjugf100% (1)
- Risk Factors for Cervical Cancer StudyDocument7 pagesRisk Factors for Cervical Cancer StudyIntania RosatiPas encore d'évaluation
- Health Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central JavaDocument11 pagesHealth Belief Model On The Determinants of Human Papilloma Virus Vaccination in Women of Reproductive Age in Surakarta, Central Javaadilla kusumaPas encore d'évaluation
- Intraventricular HaemorrhageDocument9 pagesIntraventricular HaemorrhageTriponiaPas encore d'évaluation
- 00 B 4952850536271 A 0000000Document6 pages00 B 4952850536271 A 0000000TriponiaPas encore d'évaluation
- DyslipidemiaDocument87 pagesDyslipidemiaCarlos Arturo Paternina Cuello100% (1)
- Neonatal Vomiting: R. Shaoul N.L. JonesDocument2 pagesNeonatal Vomiting: R. Shaoul N.L. JonesTriponiaPas encore d'évaluation
- A JR CCM 183121715Document8 pagesA JR CCM 183121715TriponiaPas encore d'évaluation
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocument10 pagesIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaPas encore d'évaluation
- DiphtheriaDocument12 pagesDiphtheriajenconlu_11Pas encore d'évaluation
- MDCH Diphtheria Guidelines Revise 2014Document5 pagesMDCH Diphtheria Guidelines Revise 2014TriponiaPas encore d'évaluation
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocument10 pagesIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaPas encore d'évaluation
- Intracranial Hemorrhageinthe Preterm I Nfa NT: Under ST A Nding It, Preventing ItDocument26 pagesIntracranial Hemorrhageinthe Preterm I Nfa NT: Under ST A Nding It, Preventing ItTriponiaPas encore d'évaluation
- Risk Factors of Acquired Prothrombin Complex Deficiency Syndrome A Case-Control StudyDocument8 pagesRisk Factors of Acquired Prothrombin Complex Deficiency Syndrome A Case-Control StudyTriponiaPas encore d'évaluation
- 11chronic Lung Disease in Preterm InfantsDocument7 pages11chronic Lung Disease in Preterm InfantsTriponiaPas encore d'évaluation
- BLT 11 518Document10 pagesBLT 11 518TriponiaPas encore d'évaluation
- The Shapes of Head and Face in Normal Male Newborns in South-East of Caspian Sea (Iran-Gorgan)Document4 pagesThe Shapes of Head and Face in Normal Male Newborns in South-East of Caspian Sea (Iran-Gorgan)TriponiaPas encore d'évaluation
- Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksDocument4 pagesPrevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksTriponiaPas encore d'évaluation
- Australian Public Assessment Report For Human Prothrombin ComplexDocument51 pagesAustralian Public Assessment Report For Human Prothrombin ComplexTriponiaPas encore d'évaluation
- Hydrocortisone Treatment For Bronchopulmonary Dysplasia and Brain Volumes in Preterm InfantsDocument7 pagesHydrocortisone Treatment For Bronchopulmonary Dysplasia and Brain Volumes in Preterm InfantsTriponiaPas encore d'évaluation
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocument10 pagesIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaPas encore d'évaluation
- LDD 08 RDS BPDDocument6 pagesLDD 08 RDS BPDFaizan AbbasiPas encore d'évaluation
- Ventilation and Chronic Lung DiseaseDocument17 pagesVentilation and Chronic Lung DiseaseTriponiaPas encore d'évaluation
- 43 5 6 3 PDFDocument3 pages43 5 6 3 PDFTriponiaPas encore d'évaluation
- Journal Pone 0000192Document5 pagesJournal Pone 0000192TriponiaPas encore d'évaluation
- 00 B 4952850536271 A 0000000Document6 pages00 B 4952850536271 A 0000000TriponiaPas encore d'évaluation
- BPD Pathogen Es IsDocument10 pagesBPD Pathogen Es IsTriponiaPas encore d'évaluation
- 11chronic Lung Disease in Preterm InfantsDocument7 pages11chronic Lung Disease in Preterm InfantsTriponiaPas encore d'évaluation
- Review Article: Postnatal Corticosteroids For Prevention and Treatment of Chronic Lung Disease in The Preterm NewbornDocument13 pagesReview Article: Postnatal Corticosteroids For Prevention and Treatment of Chronic Lung Disease in The Preterm NewbornTriponiaPas encore d'évaluation
- Terobosan Baru Penanganan Krisis HipertensiDocument37 pagesTerobosan Baru Penanganan Krisis HipertensiTriponiaPas encore d'évaluation
- Nonsteroidal Anti-Inflammatory DrugsDocument21 pagesNonsteroidal Anti-Inflammatory DrugsTriponiaPas encore d'évaluation
- Triage Depkes APDocument23 pagesTriage Depkes APTriponiaPas encore d'évaluation
- Management Pain and Inflammation - Stand Alone Symp CLXDocument41 pagesManagement Pain and Inflammation - Stand Alone Symp CLXTriponiaPas encore d'évaluation
- STRATEGIC ANALYSIS OF BAYBAY RESTAURANTDocument7 pagesSTRATEGIC ANALYSIS OF BAYBAY RESTAURANTAngeline Maquiso SumaoyPas encore d'évaluation
- Menu Eval Plus: Fried Rice and EggDocument2 pagesMenu Eval Plus: Fried Rice and EggJasperl Niña MalabuyocPas encore d'évaluation
- Buletin Farmasi 11/2013Document10 pagesBuletin Farmasi 11/2013afiq83Pas encore d'évaluation
- Relaxationterhadap Kecemasan Dan Gula Darahpenderita: Pengaruh Spiritual Mindfulness Based On Benson DM Tipe 2Document11 pagesRelaxationterhadap Kecemasan Dan Gula Darahpenderita: Pengaruh Spiritual Mindfulness Based On Benson DM Tipe 2Akhsa NonnisaPas encore d'évaluation
- Ground Floor (Basement) : Lucile Packard Children's Hospital Stanford HospitalDocument1 pageGround Floor (Basement) : Lucile Packard Children's Hospital Stanford Hospitalsamawi ramudPas encore d'évaluation
- Auguste D and Alzheimer's Disease: Department of Medical HistoryDocument4 pagesAuguste D and Alzheimer's Disease: Department of Medical HistorySatyavrat WaglePas encore d'évaluation
- June Workout ScheduleDocument5 pagesJune Workout ScheduleJanePas encore d'évaluation
- Iris Cheng Cover LetterDocument1 pageIris Cheng Cover Letterapi-490669340Pas encore d'évaluation
- Neuropathic Pain SlidesDocument28 pagesNeuropathic Pain SlidesAndrias Oz100% (1)
- CCRH Research Strategic VisionDocument3 pagesCCRH Research Strategic VisionMeenu MinuPas encore d'évaluation
- Ipls & AptsDocument84 pagesIpls & AptsDesalegn TesfayePas encore d'évaluation
- Viral Exanthems and EnanthemsDocument2 pagesViral Exanthems and Enanthemsclark146Pas encore d'évaluation
- Draft 2Document84 pagesDraft 2John Gabriel SamsonPas encore d'évaluation
- Clinical Pharmacy Course CreditsDocument1 pageClinical Pharmacy Course Creditshadiatussalamah100% (2)
- Internal Medicine Review: Key Concepts and Practice QuestionsDocument26 pagesInternal Medicine Review: Key Concepts and Practice QuestionsDivine SangutanPas encore d'évaluation
- Daily Lesson Log on Lifestyle and Weight ManagementDocument8 pagesDaily Lesson Log on Lifestyle and Weight ManagementNoel Isaac Maximo100% (2)
- سندDocument82 pagesسندAshkan AbbasiPas encore d'évaluation
- Abrupta Placenta - 4 Pt presents with vaginal bleeding, ABDOMINAL PAIN, and uterine tendernessDocument211 pagesAbrupta Placenta - 4 Pt presents with vaginal bleeding, ABDOMINAL PAIN, and uterine tendernessroad2successPas encore d'évaluation
- Autoimmune Encephalitis Syndromes With Antibodies - UpToDateDocument1 pageAutoimmune Encephalitis Syndromes With Antibodies - UpToDateSamPas encore d'évaluation
- Case Report: Scleredema Diabeticorum in A Patient With Type 2 Diabetes MellitusDocument5 pagesCase Report: Scleredema Diabeticorum in A Patient With Type 2 Diabetes MellitusKerin ArdyPas encore d'évaluation
- Oral Pre Cancerous LesionsDocument49 pagesOral Pre Cancerous LesionsAmit MishraPas encore d'évaluation
- Transcript 137 Hashimotos The Root Cause With Dr. Izabella Wentz PDFDocument26 pagesTranscript 137 Hashimotos The Root Cause With Dr. Izabella Wentz PDFPopescu AndreeaPas encore d'évaluation
- H&S at Work act 1974 dutiesDocument44 pagesH&S at Work act 1974 dutiesSardar Majid80% (5)
- Pad Screening Draft Evidence ReviewDocument92 pagesPad Screening Draft Evidence ReviewHaryadi KurniawanPas encore d'évaluation
- 11 AustenDocument3 pages11 AustenCyprus Chad G. LausPas encore d'évaluation
- A Survey of Employee EngagementDocument31 pagesA Survey of Employee EngagementToni Krispin0% (1)
- PE 11 Modules For First Semester 1 1Document30 pagesPE 11 Modules For First Semester 1 1Joseph LapsoPas encore d'évaluation
- Spars Pandemic Scenario (1) (01 38)Document38 pagesSpars Pandemic Scenario (1) (01 38)YuliayAngel NavarroPas encore d'évaluation
- Shoulder Presentation Diagnosis and ManagementDocument20 pagesShoulder Presentation Diagnosis and ManagementCrevins NyarikiPas encore d'évaluation
- Materi 1 LUTS Bedah Dasar EDIT FIXDocument20 pagesMateri 1 LUTS Bedah Dasar EDIT FIXfienda feraniPas encore d'évaluation