Académique Documents
Professionnel Documents
Culture Documents
Bedside Examination Vertigo PDF
Transféré par
Kenny Jap0 évaluation0% ont trouvé ce document utile (0 vote)
54 vues5 pagesDizziness, vertigo, and disequilibrium are common complaints in patients. Vertigo is an illusion of movement, usually rotation, although patients sometimes describe a sensation of linear displacement or tilt. Long-standing nonspecific vertigo more likely to have psychogenic origins.
Description originale:
Titre original
bedside examination vertigo.pdf
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDizziness, vertigo, and disequilibrium are common complaints in patients. Vertigo is an illusion of movement, usually rotation, although patients sometimes describe a sensation of linear displacement or tilt. Long-standing nonspecific vertigo more likely to have psychogenic origins.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
54 vues5 pagesBedside Examination Vertigo PDF
Transféré par
Kenny JapDizziness, vertigo, and disequilibrium are common complaints in patients. Vertigo is an illusion of movement, usually rotation, although patients sometimes describe a sensation of linear displacement or tilt. Long-standing nonspecific vertigo more likely to have psychogenic origins.
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 5
Abstract Dizzines and vertigo are common complaints in
patients referred for neurological evaluation. With a basic
understanding of vestibular physiology and proper examina-
tion techniques, a correct diagnosis can generally be made at
the bedside. This article reviews the most common peripher-
al and central vestibular syndromes as well as the key ele-
ments of the bedside vestibular system examination.
Key words Dizzines Vestibular Ocular motor Physical
examination Nystagmus
Introduction
Dizziness, vertigo, and disequilibrium are common com-
plaints in patients referred for neurological evaluation.
Because the results of a complete physical examination
and all diagnostic tests may be normal, the diagnosis
depends primarily on the history. Patients often have a
great deal of difficulty describing their symptoms. First,
an attempt should be made to elicit an exact description of
what the patient is experiencing. The most common com-
plaint is dizziness, a term that represents a wide range of
symptoms that may vary from true vertigo to more non-
specific symptoms characterized by unsteadiness or
imbalance, staggering, light-headedness, uncoordination,
or clumsiness.
Strictly defined, vertigo is an illusion of movement,
usually rotation, although patients occasionally describe a
sensation of linear displacement or tilt. Less than half of
the patients complaining of dizziness actually have verti-
go. The presence of true rotatory vertigo always indicates
an asymmetry of neural activity between the left and right
vestibular nuclei, whereas more nonspecific symptoms
suggest a whole series of other causes, including vasode-
pressor syncope, postural hypotension, cardiac dysrhyth-
mia, cerebellar dysfunction, peripheral neuropathy, hypo-
glycemia, and anxiety.
The history must define factors such as type of onset,
duration, number of episodes, and any associated audito-
ry and neurological signs. Vertigo is always temporary.
Even with a complete unilateral loss of vestibular func-
tion, vertigo always abates within a few days as central
compensation occurs. Long-standing nonspecific vertigo
is more likely to have psychogenic origins. Vertigo is
always made worse by head movements because they
accentuate any imbalance within the vestibular pathways.
Neurol Sci (2004) 24:S16S19
DOI 10.1007/s10072-004-0210-y
S. Traccis G.F. Zoroddu M.T. Zecca T. Cau M.A. Solinas R. Masuri
Evaluating patients with vertigo: bedside examination
A C U T E V E RT I G O
S. Traccis () G.F. Zoroddu M.T. Zecca T. Cau
M.A. Solinas R. Masuri
U.O. Neurologia, Ospedale A. Segni, Ozieri (SS), Italy
e-mail: seb.tra@tiscalinet.it
S. Traccis et al.: Evaluating patients with vertigo S17
Peripheral causes of vertigo
Benign paroxysmal positioning vertigo
Benign paroxysmal positioning vertigo (BPPV) is the sin-
gle most common cause of vertigo, particularly in the
elderly. It has an almost certain pathogenesis, identifiable
in the detachment of otoliths and in their dislocation to the
semicircular canals. The term canalolithiasis refers to the
presence in the canal lumen of otoconial debris free to
move in the endolymph. The term cupulolithiasis is
reserved for the few cases of suspected adhesion of debris
to the cupula. Typically affected patients complain of
brief episodes of vertigo precipitated by rapid change of
head position relative to gravity. The so-called Dix-
Hallpike maneuver is the cornerstone of diagnosing the
common variety of posterior canal BPPV. The operator
turns the patients head 45 towards the right or left side
and brings the patient to a head-hanging position off the
bed. A typical response is characterized by a latent peri-
od of about 25 s, followed by vertigo, nausea, and a
mixed linear-rotatory nystagmus, with the fast phase beat-
ing toward the undermost ear or upward when gaze is
directed to the uppermost ear. The nystagmus gradually
recedes after 1040 s and ultimately abates even when the
precipitating head position is maintained. When the
patient returns to the seated position, the vertigo and nys-
tagmus may recur less violently in the opposite direction.
The horizontal canal variant of BPPV may produce hori-
zontal nystagmus when the patient is supine and the head
is quickly rolled to either side. If due to loose otoconia,
the nystagmus usually will be geotropic (beating toward
the ground). If otoconia are fixed to the cupula, the nys-
tagmus will be apogeotropic and persist. In most patients
with BPPV abnormal vestibular or auditory function can-
not be demonstrated. In a few it follows acute vestibular
neuritis or occurs during the course of a progressive inner
ear disease.
Vestibular neuritis
Acute unilateral vestibular paralysis is the third most com-
mon cause of peripheral vestibular vertigo. It is usually
ascribed to viral infection or to a parainfectious event. The
chief symptom is the acute onset of prolonged severe rota-
tory vertigo, associated with horizontal-torsional sponta-
neous nystagmus with the slow phases towards the affect-
ed ear, postural imbalance, and nausea without concomi-
tant auditory dysfunction. The nystagmus is always strict-
ly unidirectional. Bidirectional gaze-evoked nystagmus
excludes the diagnosis. The nystagmus is, to some extent,
always suppressed by visual fixation. The head impulse
test is invariably positive and shows absent lateral semi-
circular canal function on the affected side. In some
patients the disorder only affects the superior vestibular
nerve (horizontal semicircular canal paresis), which has a
separate path and its own ganglion, whereas the inferior
part (posterior semicircular canal) is spared. There is an
ocular tilt reaction characterized by ipsilateral head tilt and
an ocular skew deviation in which the eye ipsilateral to the
lesion is lower and extorted; the contralateral eye is high-
er and intorted. Patients often complain of vertical diplop-
ia but may also experience a tilt illusion of the visual
world. The condition gradually recovers naturally within
16 weeks.
Mnires disease
Mnires disease is characterized by attacks of severe
spontaneous vertigo with nausea and vomiting, a low fre-
quency tinnitus, fluctuating hearing loss, and a sense of
fullness or blockage in the affected ear. The vertigo attacks
usually last for a few hours, but the tinnitus and hearing
loss might continue for days. The tinnitus is typically
described as a roaring sound (the sound of the ocean or a
hollow seashell sound). Monosymptomatic cochlear or
vestibular manifestations are possible variants at the
beginning of the disease. Occasionally, the patients will
develop vestibular drop attacks. The most consistent
pathological finding in patients with Mnires disease is
an increase in the volume of endolymph associated with
distension of the entire endolymphatic system. Attacks of
Mnires disease must be distinguished by vestibular
migraine and vascular loop compression of the vestibular
nerve (vestibular paroxysmia).
Perilymph fistula
Perilymph fistula is associated with abnormal communica-
tion between the perilymph space and the middle ear
caused by traumatic pressure changes in either the cere-
brospinal fluid and/or the middle ear. Patients with fistula
may complain of imbalance, positional vertigo, and nys-
tagmus as well as a sudden hearing loss. Frequent triggers
are ambient pressure changes transferred to the inner ear,
certain head positions in space, head movements, or loco-
motion. In some patients perilymph fistula appears as a
sound-induced vestibular symptoms, known as the Tullio
phenomenon, either of the semicircular canal or of the
otolithic type. The disease is more often episodic than
chronic. Perilymph fistulas may resolve spontaneously, but
sometimes surgical repair is necessary.
S18 S. Traccis et al.: Evaluating patients with vertigo
Central causes of vertigo
Cerebellar infarction
Central pathological causes of vertigo are less common than
peripheral causes. Severe vertigo, mimicking labyrinthine
disease, may be an early symptom of acute cerebellar infarc-
tion in the territory of either the anterior inferior cerebellar
artery or the posterior inferior cerebellar artery. The vertigo
can result from pontomedullary brainstem ischemia near the
vestibular nuclei. If the impulse test or the caloric irrigation
evoke bilateral normal responses, vertigo of central origin
should be suspected. Acute peripheral vestibulopathy usual-
ly causes unidirectional nystagmus, with the fast phase in
the opposite direction. The nystagmus increases during gaze
in the direction of the fast phase, is suppressed by visual fix-
ation, and remains horizontal on upward gaze. By contrast,
with a cerebellar infarction the nystagmus is in the direction
of gaze and most prominently ipsilateral to the lesion and
cannot be suppressed by visual fixation. Ocular motor find-
ings are often present in brainstem disease such as upbeat or
downbeat nystagmus or dysconjugate nystagmus. If vertigo
and lateropulsion are caused by an incomplete Wallenbergs
syndrome, ipsilateral ataxia and controlateral hypalgesia are
very helpful.
Cerebellopontine angle tumors
Most cerebellopontine angle tumors arise on the vestibular
portion of the eighth nerve in the internal auditory canal.
Initially, they present with gradually progressive hearing
loss and tinnitus due to cochlear nerve compression. The
tumor produces such a gradual reduction in vestibular
function that the central compensatory mechanisms have
the capability of preventing the vertigo. Compression of
the brainstem and the vestibulocerebellum causes Bruns
nystagmus. It is a combination of low-frequency, high-
amplitude horizontal nystagmus on looking ipsilaterally
due to defective gaze holding, and a high-frequency, low-
amplitude nystagmus on looking contralaterally, due to
vestibular imbalance.
Epileptic vertigo
Vestibular cortical function has been identified in humans
in the superior lip of the intraparietal sulcus, in the poste-
rior superior portions of the temporal lobe, and in the tem-
poroparietal border regions. Vestibular epilepsy can be
secondary to focal epileptic discharges in these areas. The
patient experiences rotational or linear vertigo and tinni-
tus, and paresthesia may precede or accompany the verti-
go. Vertigo can be the predominant symptom of a simple
or complex partial sensory seizure. A focus located in
either frontal or temporal cortex may lead to rotatory
seizures volvular epilepsy, circling epilepsy character-
ized by paroxysmal walking in small circles.
Bedside neuro-otological examination
A bedside neuro-otological examination should be per-
formed to determine if any static or dynamic vestibular
imbalance is present. Spontaneous nystagmus indicates a tone
imbalance of the vestibulo-ocular reflex, which may be cen-
tral or peripheral. When peripheral in origin, as in vestibular
neuritis, it is typically suppressed by visual fixation. There are
several simple methods for achieving the latter at the bedside.
Frenzel glasses have 10+ diopter lenses that prevent fixation,
allowing vestibular nystagmus to be seen. An ophthalmo-
scope can also be used to block fixation and bring out a spon-
taneous nystagmus. When the fundus of one eye is apparent,
the patient is asked to cover the other eye with one hand. The
direction of the nystagmus is reversed because the optic nerve
head is behind the center of rotation of the eye. Occasionally
nystagmus can be seen even through closed lids. The nystag-
mus is always rotatory-horizontal beating clockwise-left or
counterclockwise-right. Pure vertical, torsional, or linear nys-
tagmus cannot be explained by involvement of a single canal
or single labyrinth and implies a central etiology.
A dynamic vestibular imbalance can be assessed by
determining the effect of head rotation on visual acuity,
observing the eye movements in response to low- and high-
frequency head rotations, and performing bedside caloric
testing. Dynamic visual acuity can be determined by pas-
sively rotating the patients head horizontally or vertically
at a frequency of about 2 Hz while reading a Snellen visu-
al acuity chart at the standard distance. A drop in acuity of
more than one line on the Snellen chart suggests an abnor-
mal VOR gain. The VOR can also be assessed with an oph-
thalmoscope by observing the stability of the optic nerve
head as the patient oscillates the head back and forth at
about 2 Hz while attempting to fix on an imagined distant
target. A normally functioning VOR will keep the optic
nerve head stable relative to the examiner. The high-fre-
quency VOR can be assessed by performing rapid head
rotations: head impulse test. The patient is asked to fix
upon a target while the examiner briskly turns the head hor-
izontally or vertically. The rotation should not be larger
than about 15, but should be of high acceleration. If the
VOR is working normally, gaze will be held steady; if not,
the patient has to perform a corrective catch-up saccade at
the end of the head movement to bring the image of the target
back to the fovea. Head-shaking nystagmus can also demon-
strate asymmetry of velocity storage that occurs as a result of
peripheral or central vestibular lesions. The patient is instruct-
ed to vigorously shake the head for 1015 s in the horizontal
S. Traccis et al.: Evaluating patients with vertigo S19
plane with the eyes closed. Upon stopping and opening the
eyes (preferably using Frenzel lenses), nystagmus usually
beats away from the side with the lesion. Bedside caloric test-
ing can be useful to determine the side of a peripheral vestibu-
lar lesion. The head of the patient is tilted 30 upward, so that
the orizontal semicircular canals are in the vertical plane, thus
allowing optimal caloric stimulation. Cool irrigation causes
nystagmus away from the ear and warm irrigation causes nys-
tagmus toward the ear. The nystagmus can be observed with
Frenzel lenses or occlusive ophthalmoscopy to eliminate fixa-
tion. Unilateral caloric hypo- or nonexcitability is found most
often in peripheral vestibular lesions, e.g., in vestibular neuri-
tis, acoustic neurinoma, or lesions of the labyrinths or vestibu-
lar nerve. Central vestibular disorders, however, may also
cause caloric hypoexcitability and mimic vestibular neuritis,
especially lesions at the root-entry zone of the vestibular nerve
(fascicular lesions) due to plaques in multiple sclerosis or
lacunar infarctions.
Suggested readings
Baloh RW, Honrubia V (1989) Clinical neurophysiology of the
vestibular system. Davis, Philadelphia
Brandt T (1998) Vertigo: its multisensory syndromes, 2nd edn.
Springer London
Leigh RJ, Zee DS (1999) The neurology of eye movements, 3rd
edn. Davis, Philadelphia
Traccis S (1992) Il nistagmo fisiologico e patologico. Patron,
Bologna
Traccis S, Rosati G (1995) Nervo Vestibolare. In: Bergonzi P,
Massaro AR (eds) Trattato Italiano di neurologia. Verducci,
Rome, pp 60.3760.44
Traccis S, Zambarbieri D (1992) I movimenti saccadici. Patron,
Bologna
Traccis S, Zambarbieri D (1994) I movimenti di inseguimento
lento. Patron, Bologna
Traccis S, Zambarbieri D (1996) Le interazioni visuo-vestibolari.
Patron, Bologna
Reproducedwith permission of thecopyright owner. Further reproductionprohibited without permission.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Parasites Immunity and PathologyDocument389 pagesParasites Immunity and Pathologyrild278111Pas encore d'évaluation
- Principles of Endocrinology and Hormone PDFDocument794 pagesPrinciples of Endocrinology and Hormone PDFleogmail100% (4)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Come Thirsty Chapter1Document4 pagesCome Thirsty Chapter1Natalia Lupasco100% (1)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Unit 1, InvertebratesDocument4 pagesUnit 1, InvertebratesnatalescorPas encore d'évaluation
- What Are The Types of EndosDocument3 pagesWhat Are The Types of EndosSailu KatragaddaPas encore d'évaluation
- Top Knife - Cutted - Top PDFDocument238 pagesTop Knife - Cutted - Top PDFIvanKazaiev100% (1)
- H2S Training Slides ENGLISHDocument46 pagesH2S Training Slides ENGLISHf.B100% (1)
- Muscles of Mastication Functions and Clinical SignificanceDocument130 pagesMuscles of Mastication Functions and Clinical SignificanceDevanand GuptaPas encore d'évaluation
- Anatomy and Physiology TermsDocument8 pagesAnatomy and Physiology TermsDominic DinioPas encore d'évaluation
- The Pathophysiology of CholesteatomaDocument17 pagesThe Pathophysiology of Cholesteatomaapi-19500641Pas encore d'évaluation
- CONSUMER BEHAVIOUR UpdatedDocument66 pagesCONSUMER BEHAVIOUR UpdatedUmer AzizPas encore d'évaluation
- What Is The Best Way To Treat Tinea Cruris?: Clinical InquiriesDocument4 pagesWhat Is The Best Way To Treat Tinea Cruris?: Clinical InquiriesKenny JapPas encore d'évaluation
- Lactose Free As TX 4 Acute DiarrheaDocument5 pagesLactose Free As TX 4 Acute DiarrheaKenny JapPas encore d'évaluation
- The American Thoracic I DYSPNEUDocument31 pagesThe American Thoracic I DYSPNEUKenny JapPas encore d'évaluation
- Diagnosis and Management of Acute Otitis MediaDocument36 pagesDiagnosis and Management of Acute Otitis MediatheodorvalPas encore d'évaluation
- Bedside Examination Vertigo PDFDocument5 pagesBedside Examination Vertigo PDFKenny JapPas encore d'évaluation
- Anesthesia For High Risk PatientsDocument167 pagesAnesthesia For High Risk PatientsKenny Jap100% (1)
- 4 Coffee and HealthDocument24 pages4 Coffee and HealthKenny JapPas encore d'évaluation
- Laporan PBL 3 Lansia: Universitas Katolik Atma Jaya Fakultas Kedokteran 2010Document2 pagesLaporan PBL 3 Lansia: Universitas Katolik Atma Jaya Fakultas Kedokteran 2010Kenny JapPas encore d'évaluation
- Ais Iss Rts Ps TrissDocument12 pagesAis Iss Rts Ps TrissKenny JapPas encore d'évaluation
- AVM InfoDocument8 pagesAVM InfoKenny JapPas encore d'évaluation
- Acid Base BalanceDocument44 pagesAcid Base BalanceKenny JapPas encore d'évaluation
- Choice of Anesthesia TechniqueDocument7 pagesChoice of Anesthesia TechniqueKenny JapPas encore d'évaluation
- Ludwig's AnginaDocument7 pagesLudwig's AnginaKenny JapPas encore d'évaluation
- Bedside Examination Vertigo PDFDocument5 pagesBedside Examination Vertigo PDFKenny JapPas encore d'évaluation
- Efek Ekstra Piramidal EPSDocument3 pagesEfek Ekstra Piramidal EPSKenny JapPas encore d'évaluation
- Low Back PainDocument27 pagesLow Back PainKenny JapPas encore d'évaluation
- Kuliah Low Back Back PainDocument14 pagesKuliah Low Back Back PainAsri PrameswariPas encore d'évaluation
- Jurnal Back PainDocument23 pagesJurnal Back PainKenny JapPas encore d'évaluation
- Jurnal Back PainDocument23 pagesJurnal Back PainKenny JapPas encore d'évaluation
- AnatomiDocument37 pagesAnatomiMuhammad HariyadiPas encore d'évaluation
- Divison and Characteristic Features of The Respiratory SystemDocument2 pagesDivison and Characteristic Features of The Respiratory SystemKenny JapPas encore d'évaluation
- SF-DCT INFORMATION FOR SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) CLAIMSDocument105 pagesSF-DCT INFORMATION FOR SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) CLAIMSKenny JapPas encore d'évaluation
- Lecture Pathology BMS IIIDocument44 pagesLecture Pathology BMS IIIKenny JapPas encore d'évaluation
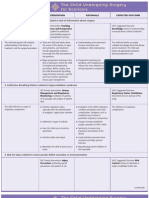
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverPas encore d'évaluation
- GIT Physio D&R AgamDocument67 pagesGIT Physio D&R Agamvisweswar030406Pas encore d'évaluation
- SGD Physiology Endocrine and MetabolismDocument7 pagesSGD Physiology Endocrine and MetabolismTinesh RajahPas encore d'évaluation
- The Third International Consensus Definitions For Sepsis and Septic Shock Sepsis-3 - JAMA 2016Document10 pagesThe Third International Consensus Definitions For Sepsis and Septic Shock Sepsis-3 - JAMA 2016Miguel Angel Quiroz CristobalPas encore d'évaluation
- POLYGRAPHY: THE SCIENTIFIC METHOD OF DETECTING DECEPTIONDocument15 pagesPOLYGRAPHY: THE SCIENTIFIC METHOD OF DETECTING DECEPTIONEino DuldulaoPas encore d'évaluation
- Template POMRDocument8 pagesTemplate POMRPPDS IPD ULMPas encore d'évaluation
- Shah Et Al-2016-Frontiers in Plant ScienceDocument28 pagesShah Et Al-2016-Frontiers in Plant ScienceJamie SamuelPas encore d'évaluation
- Electrolyte Imbalance 1Document3 pagesElectrolyte Imbalance 1Marius Clifford BilledoPas encore d'évaluation
- DLL - Science 6 - Q2Document7 pagesDLL - Science 6 - Q2Angelica GuillermoPas encore d'évaluation
- 10th BIOLOGY PPT CH. NO. 8Document13 pages10th BIOLOGY PPT CH. NO. 8Aastha BorhadePas encore d'évaluation
- Battle of BrainDocument7 pagesBattle of BrainKhalida Zia SiregarPas encore d'évaluation
- Nicotrol InhalerDocument19 pagesNicotrol InhalerdebysiskaPas encore d'évaluation
- USABO 17 Open Exam - Final.webDocument16 pagesUSABO 17 Open Exam - Final.webJ.Chang ChangPas encore d'évaluation
- A New Furileusaurian Abelisaurid From La Invernada Upper Cretaceous Santonian Bajo de La Carpa Formation Northern Patagonia ArgentinaDocument29 pagesA New Furileusaurian Abelisaurid From La Invernada Upper Cretaceous Santonian Bajo de La Carpa Formation Northern Patagonia ArgentinaStuff NewsroomPas encore d'évaluation
- Artificial Lung Design & Gas ExchangeDocument25 pagesArtificial Lung Design & Gas Exchangealoove66Pas encore d'évaluation
- Gastro-Intestinal System Diagnostic TestsDocument11 pagesGastro-Intestinal System Diagnostic TestsFev BanataoPas encore d'évaluation
- FORENSIC SEROLOGY AND BLOOD ANALYSISDocument16 pagesFORENSIC SEROLOGY AND BLOOD ANALYSISBARCELON, CHRISTOPHER JAMESPas encore d'évaluation
- Anatomy of A ClamDocument6 pagesAnatomy of A ClamRU VickPas encore d'évaluation
- Amino Acid Sequences Reveal Evolutionary RelationshipsDocument6 pagesAmino Acid Sequences Reveal Evolutionary RelationshipsAbby Gail DigalPas encore d'évaluation
- Neurotransmission, Measuring Chemical Events In: Advanced ArticleDocument12 pagesNeurotransmission, Measuring Chemical Events In: Advanced ArticleazzaassPas encore d'évaluation