Académique Documents
Professionnel Documents
Culture Documents
Fitz
Transféré par
salamredDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Fitz
Transféré par
salamredDroits d'auteur :
Formats disponibles
Fitz-Hugh-Curtis Syndrome
Valerie Lewis MD, MPH
Nadja Peter MD
Basics
Description
Fitz-Hugh-Curtis (FHC) is the syndrome (FHCS) of perihepatitis, an
inflammation of the liver capsule, associated with PID in the reproductiveaged female.
Characterized laparoscopically by violin-string adhesions between the liver
capsule and abdominal wall.
Characterized clinically by acute or subacute onset of RUQ pain at the time of
genital tract infection (may be asymptomatic) with Chlamydia trachomatis or
Neisseria Gonorrhea.
RUQ pain can be persistent in the chronic phase of the disorder.
Age-Related Factors
Rates of FHCS are higher among adolescent females than adult women with
PID.
The higher rates among adolescents may be related to their immature cervical
ectropion (presence of columnar cells on the ectocervix), making them
biologically more susceptible to cervicitis.
Epidemiology
The incidence of FHCS (perihepatitis in presence of PID) is higher among adolescent
girls (27%) when compared to adult women (413.8%).
Risk Factors
Those factors which place an individual at risk for acquiring a genital infection with
Chlamydia or Gonorrhea resulting in pelvic inflammation:
Unprotected intercourse
Early sexual debut
Multiple sexual partners
In adult women, recent IUD placement may be a risk factor in the
development of PID.
Pathophysiology
The pathophysiology of this disorder is poorly understood, but the following
mechanisms have been proposed (some with conflicting or controversial
evidence, and maybe with different mechanisms in operation for Chlamydia
vs. Gonorrhea):
o Direct bacterial spread from the fallopian tubes to the liver via the
pericolic gutters:
Although it is possible that pelvic fluid can be tracked to the
RUQ, the causative bacteria has seldom been isolated from the
liver surface.
Hematogenous or lymphatic spread:
Some evidence for these mechanisms for Gonorrhea but very
little for Chlamydia.
Exaggerated immune response to C. trachomatis is the most likely
explanation, given what is known to date.
o
Higher anti-Chlamydial IgG titers have been found in those with both
perihepatitis and salpingitis than with salpingitis alone.
Antigenic proteins from Chlamydia may cross-react with host tissue
proteins, resulting in an exaggerated inflammatory response.
Associated Conditions
PID
Salpingitis
Diagnosis
Signs and Symptoms
History
The acute phase is characterized by:
o Sharp, pleuritic pain located in the RUQ of the abdomen, or pain
referred to the ipsilateral shoulder
o
Symptoms are usually associated with acute salpingitis, but signs or
symptoms of PID may be absent, especially with Chlamydia.
The chronic phase is characterized by persistent RUQ pain.
Pericapsular adhesions can occur in the absence of RUQ pain or salpingitis,
which can make the diagnosis challenging.
Review of Systems
May be associated with nausea, vomiting, hiccups, fever, chills, malaise, or signs of
salpingitis (lower abdominal pain and abnormal vaginal discharge)
Physical Exam
No pathognomonic exam findings, making FHCS a diagnosis of exclusion
Examination will demonstrate RUQ tenderness, or rarely a friction rub is
heard over the same area.
In patients with concurrent salpingitis, cervical motion or adnexal tenderness
may be present.
Tests
Laboratory tests and imaging studies are often nonspecific.
Labs
Liver enzyme levels: Typically, normal, but may be elevated. (Transaminase
elevations are more likely in the setting of gonococcal rather than Chlamydial
perihepatitis.)
ESR and/or C-reactive protein may be elevated.
WBC count may be normal or elevated.
Isolation of either Chlamydia and/or Gonorrhea from the cervix using a
variety of testing techniques including culture, direct immunofluorescent
smears, enzyme immunoassays, DNA probes, or nucleic acid amplification
tests.
Chlamydia-specific serology tests
If high clinical suspicion for STDs exists, samples should also be obtained
from the rectum, urethra, and pharynx.
Obtain studies to rule out other gastrointestinal or renal causes of RUQ pain:
Amylase, lipase, stool guaiac, and urinalysis/urine culture.
Imaging
Imaging studies are useful in ruling out or eliminating other potential causes of
RUQ pain.
Chest and abdominal radiographs to evaluate for pneumonia or
subdiaphragmatic free air:
o
US to evaluate the liver, the gallbladder for cholelithiasis or cholecystitis, or
the ovaries for a tubo-ovarian abscess or other signs of PID:
o
A right-sided hemidiaphragm elevation or small reactive pleural
effusion may be seen in FHCS.
Rarely, ascites in the hepatorenal space, loculated fluid in the pelvis or
abdomen or adhesions between the liver and abdominal wall may be
seen in FHCS.
CT occasionally demonstrates liver capsule enhancement.
Differential Diagnosis
FHCS can mimic other conditions making the diagnosis difficult.
Cholelithiasis/cholecystitis
Pneumonia
Pulmonary embolism
Rib fracture/abdominal trauma
Pyelonephritis
Hepatitis/Peritonitis
Nephrolithiasis
Subphrenic abscess
Pancreatitis
Appendicitis
Herpes zoster
Enteroviral epidemic pleurodynia (Burnhold disease)/pleurisy
Infection
C. trachomatis is more likely to be the etiologic agent than N. gonorrhea, although
both have been implicated in FHCS.
Treatment
General Measures
Antibiotic therapy is indicated in the management of FHCS.
The same agents directed against Chlamydia and Gonorrhea are used to treat
PID and FHCS.
One should not await confirmatory lab results to treat if clinical suspicion is
high.
Pain control can be achieved with NSAIDs or narcotic agents.
Sexual activity should be avoided until 1 week after both the patient and
partner(s) have completed treatment.
P.109
Medication (Drugs)
Treatment regimen as per CDC Guidelines for treatment of PID
Oral regimens:
Ceftriaxone 250 mg IM in a single dose PLUS doxycycline** 100 mg
PO b.i.d. for 14 days WITH OR WITHOUT Metronidazole 500 mg PO
b.i.d. for 14 days
Alternative: OR cefoxitin 2 g IM in a single dose and probenecid 1 g
PO administered concurrently in a single dose, OR other parenteral
3rd-generation cephalosporin PLUS doxycycline 100 mg PO b.i.d. for
14 days WITH OR WITHOUT metronidazole 500 mg PO b.i.d. for 14
days
Parenteral regimens:
o
Cefotetan 2 g IV q12h OR cefoxitin 2 g IV q6h PLUS doxycycline**
100 mg PO or IV q12h
Clindamycin 900 mg IV q8h PLUS gentamicin loading dose IV or IM
(2 mg/kg of body weight), followed by a maintenance dose (1.5
mg/kg) q8h. Single daily dosing may be substituted.
Alternative: OR ampicillin/sulbactam 3 g IV q6h PLUS doxycycline**
100 mg PO or IV q12h
Fluoroquinolones should only be used in persons with intolerance to
other aforementioned antibiotics and with low individual risk and low
community prevalence of Gonorrhea. If testing for Gonorrhea is
positive, the antibiotic should be changed or susceptibility testing
done.
Alert
Pediatric Considerations
Fluoroquinolones should be used sparingly in those younger than 18 years secondary
to concerns about interference with bone development.
Pregnancy Considerations
Fluoroquinolones and doxycycline should be avoided during pregnancy.
Surgery
Laparoscopic exploration can be used to assist in making the diagnosis of PID
and FHCS.
Surgical intervention is indicated only in the event that symptoms do not
resolve after antibiotic therapy:
o
Laparoscopy can be used to lyse perihepatic adhesions in the case of
chronic RUQ pain following an episode of FHCS.
Followup
Disposition
Hospital admission criteria for FHCS are similar to those for PID and include:
o Inability to rule out a surgical emergency
Inability to tolerate an oral regimen
The presence of a complication of PID such as tubo-ovarian abscess
Pregnancy
Discharge when the patient's symptoms of salpingitis have resolved.
Issues for Referral
Consider gynecologic surgical referral for lysis of perihepatic adhesions in individuals
with chronic RUQ pain.
Prognosis
Excellent
Patient Monitoring
Monitor for resolution of RUQ pain, as well as signs and symptoms of
salpingitis.
An association may exist between FHCS and fallopian tube dysfunction that
results in infertility. Severity of the tubal abnormality is determined by the
host's reactivity to Chlamydia.
Bibliography
Centers for Disease Control and Prevention, Updated recommended treatment
regimens for gonococcal infections and associated conditions United States, April
2007. http//www.cdc.gov/std/treatment/2006/updated-regimens.htm
Kobayashi Y, et al. Pathological study of Fitz-Hugh-Curtis syndrome evaluated from
fallopian tube damage. J Obstet Gynaecol. 2006;32(3):280285.
Litt IF, et al. Perihepatitis associated with salpingitis in adolescents. JAMA.
1978;240:12531254.
Peter NG, et al. Fitz-Hugh-Curtis syndrome: A diagnosis to consider in women with
right upper quadrant pain. Cleve Clin J Med. 2004;71(3):233239.
Tsubuku M, et al. Fitz-Hugh-Curtis syndrome: Linear contrast enhancement of the
surface of the liver on CT. J Comput Assist Tomogr. 2002;26:456458.
Miscellaneous
Synonym(s)
Gonococcal perihepatitis
Perihepatitis syndrome
Clinical Pearls
C. trachomatis and N. gonorrhea are the main causative agents implicated in FHCS.
Among those with PID, FHCS occurs more commonly among adolescent females
(27%) than adult women (414%).
FHCS is usually a clinical diagnosis based on exclusion of other causes of RUQ pain
and isolation of the bacterial pathogen.
Treatment is with antibiotics directed against C. trachomatis and N. gonorrhea. Can
consider lysis of perihepatic adhesions if RUQ pain persists.
Abbreviations
FHCSFitz-Hugh Curtis syndrome
PIDPelvic inflammatory disease
RUQRight upper quadrant
STD/STISexually transmitted disease/infection
Codes
ICD9-CM
99.56 Perihepatitis
614.9 Pelvic inflammatory disease
Patient Teaching
Educate about safer sex practices including consistent condom use.
Encourage testing for other STIs, including HIV and syphilis.
Counsel about the importance of partner notification to prevent spread or
reinfection.
Frequent STI screening and testing among sexually active populations
Prevention
Reduction of high-risk sexual behaviors
Vous aimerez peut-être aussi
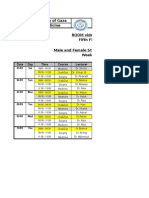
- Islamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1Document2 pagesIslamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1salamredPas encore d'évaluation
- MCQ On MenopauseDocument4 pagesMCQ On Menopausesalamred100% (3)
- Chronic DiarrheaDocument6 pagesChronic DiarrheasalamredPas encore d'évaluation
- ةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologyDocument14 pagesةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologysalamredPas encore d'évaluation
- Pelvis Types and Labor StagesDocument7 pagesPelvis Types and Labor Stagessalamred100% (1)
- HemoptysisDocument3 pagesHemoptysissalamredPas encore d'évaluation
- MCQ Net 3Document5 pagesMCQ Net 3salamredPas encore d'évaluation
- MCQs Psy Exam44 First GroupDocument7 pagesMCQs Psy Exam44 First Groupsalamred100% (3)
- Rectal bleeding causes and treatment optionsDocument21 pagesRectal bleeding causes and treatment optionslinaleen67% (3)
- Psychiatry Final Exam 2014Document2 pagesPsychiatry Final Exam 2014Ibrahem Y. NajjarPas encore d'évaluation
- Ortho OSCE 2008Document3 pagesOrtho OSCE 2008salamredPas encore d'évaluation
- امتحان الاشعة العملي النهائيDocument1 pageامتحان الاشعة العملي النهائيsalamredPas encore d'évaluation
- MCQs Psy Exam44 First GroupDocument7 pagesMCQs Psy Exam44 First Groupsalamred100% (3)
- MCQs on key psych topicsDocument17 pagesMCQs on key psych topicssalamredPas encore d'évaluation
- Solutions To The Test CasesDocument11 pagesSolutions To The Test CasessalamredPas encore d'évaluation
- MSQU Course MontadaDocument39 pagesMSQU Course MontadasalamredPas encore d'évaluation
- RadiologyDocument5 pagesRadiologysalamredPas encore d'évaluation
- اسبيرو طويل مهم جدا الثلاثاءDocument22 pagesاسبيرو طويل مهم جدا الثلاثاءsalamredPas encore d'évaluation
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 pagesChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredPas encore d'évaluation
- Longitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionDocument4 pagesLongitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionsalamredPas encore d'évaluation
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 pagesChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredPas encore d'évaluation
- A) Basic Surgical SciencesDocument27 pagesA) Basic Surgical SciencessalamredPas encore d'évaluation
- 333Document13 pages333salamredPas encore d'évaluation
- PMC Exam 2006Document27 pagesPMC Exam 2006salamredPas encore d'évaluation
- The Answer KeyDocument1 pageThe Answer KeysalamredPas encore d'évaluation
- Liver Surgery Procedures & ComplicationsDocument10 pagesLiver Surgery Procedures & ComplicationsIbrahem Y. NajjarPas encore d'évaluation
- MCQDocument11 pagesMCQsalamredPas encore d'évaluation
- A) Basic Surgical SciencesDocument27 pagesA) Basic Surgical SciencessalamredPas encore d'évaluation
- breastطباعةDocument3 pagesbreastطباعةsalamredPas encore d'évaluation
- Dr:-Ashraf .I. ObaidDocument22 pagesDr:-Ashraf .I. ObaidsalamredPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Lubchanco Classification of Newborns-BoysgirlsDocument1 pageLubchanco Classification of Newborns-BoysgirlsAmanda JulianaPas encore d'évaluation
- Pregnant Mothers' KAP of Exercise During PregnancyDocument24 pagesPregnant Mothers' KAP of Exercise During PregnancyBEREKETPas encore d'évaluation
- Maternal Physiology: Metabolic Changes Hematological ChangesDocument33 pagesMaternal Physiology: Metabolic Changes Hematological ChangesironPas encore d'évaluation
- Activity-Based Costing Improves Healthcare ValueDocument1 pageActivity-Based Costing Improves Healthcare ValueKayle MatabalanPas encore d'évaluation
- Medical Assistant ThesisDocument5 pagesMedical Assistant Thesislindseycampbellerie100% (2)
- Kohl IntroDocument9 pagesKohl Introsankalp29Pas encore d'évaluation
- Patient Handover, Patient EndorsementDocument12 pagesPatient Handover, Patient Endorsementgladz25100% (2)
- Toxicology-Handbook PDFDocument2 pagesToxicology-Handbook PDFssb channelPas encore d'évaluation
- 1224 Visual Acuity FromDocument1 page1224 Visual Acuity Fromreza khakshouriPas encore d'évaluation
- Basic EKG 2: Dr. Wattana Wongtheptien M.D. Cardiologist Chiangrai Regional HospitalDocument79 pagesBasic EKG 2: Dr. Wattana Wongtheptien M.D. Cardiologist Chiangrai Regional HospitalVeerapong Vattanavanit0% (1)
- Pelvic Planes Dimensions and ContractionTITLEDocument12 pagesPelvic Planes Dimensions and ContractionTITLEDavid Eka PrasetyaPas encore d'évaluation
- PostnatalDocument99 pagesPostnatalPlain GerlPas encore d'évaluation
- Paediatric Intrathecal Antibiotic ProcedureDocument9 pagesPaediatric Intrathecal Antibiotic ProcedureAbu Azzam Al-HadiPas encore d'évaluation
- A Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)Document434 pagesA Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)AbdulraHman KhalEd100% (2)
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyMariana González DíazPas encore d'évaluation
- Disaster Management Action PlanDocument13 pagesDisaster Management Action Planpurunjay joshiPas encore d'évaluation
- Informatics Quiz 1 NAME: - DATE: - I. Multiple Choice. Choose The Best Answer. Encircle The Letter of The Correct AnswerDocument2 pagesInformatics Quiz 1 NAME: - DATE: - I. Multiple Choice. Choose The Best Answer. Encircle The Letter of The Correct Answerlouie roderosPas encore d'évaluation
- Preventionof HypothermiaDocument2 pagesPreventionof HypothermiarisnayektiPas encore d'évaluation
- Annexure K Provincial Administration: Free State Department of Health Closing Date NoteDocument14 pagesAnnexure K Provincial Administration: Free State Department of Health Closing Date NotedujdjsPas encore d'évaluation
- (CC) Malpresentation and DeliveryDocument6 pages(CC) Malpresentation and DeliveryDaryl Gay NanoPas encore d'évaluation
- Unit 13-Conversation by PhoneDocument10 pagesUnit 13-Conversation by Phonefransiska wijoyoPas encore d'évaluation
- Moxibustion Therapy by Debra BettsDocument2 pagesMoxibustion Therapy by Debra Bettsfloreslac100% (1)
- Clinical TeachingDocument21 pagesClinical Teachingtanmai nooluPas encore d'évaluation
- Dyspareunia: Physical Therapy Evaluation and ManagementDocument27 pagesDyspareunia: Physical Therapy Evaluation and ManagementJohayra AbbasPas encore d'évaluation
- Obgyn Protocol 2019Document341 pagesObgyn Protocol 2019fizii100% (1)
- CTU Insulin Sliding ScalesDocument2 pagesCTU Insulin Sliding ScalesnindylistyPas encore d'évaluation
- Aggravating Factors Precipitating Factors Predisposing FactorsDocument4 pagesAggravating Factors Precipitating Factors Predisposing FactorsJann ericka JaoPas encore d'évaluation
- OB SottoDocument2 pagesOB SottoSophia VeralloPas encore d'évaluation
- SoprolifeDocument15 pagesSoprolifeapi-365751897100% (1)