Académique Documents
Professionnel Documents
Culture Documents
24 - 04 - 2014 - Overall Treatment Time Tongue Carcinoma
Transféré par
María José Sánchez LovellTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
24 - 04 - 2014 - Overall Treatment Time Tongue Carcinoma
Transféré par
María José Sánchez LovellDroits d'auteur :
Formats disponibles
Int. J. Radiation Oncology Biol. Phys., Vol. 57, No. 1, pp.
7178, 2003
Copyright 2003 Elsevier Inc.
Printed in the USA. All rights reserved
0360-3016/03/$see front matter
doi:10.1016/S0360-3016(03)00507-8
CLINICAL INVESTIGATION
Head and Neck
EFFECT OF TREATMENT TIME ON OUTCOME OF RADIOTHERAPY FOR
ORAL TONGUE CARCINOMA
YOICHIRO HOSOKAWA, D.D.S., PH.D.,* HIROKI SHIRATO, M.D., PH.D.,
TAKASHI NISHIOKA, M.D., PH.D., KAZUHIKO TSUCHIYA, M.D., PH.D., TA-CHEN CHANG, M.D.,
KENJI KAGEI, M.D., PH.D., KEIICHI OHOMORI, D.D.S., PH.D., KEN-ICHI OBINATA, D.D.S., PH.D.,
MASAYUKI KANEKO, D.D.S., PH.D.,* KAZUO MIYASAKA, M.D., PH.D., AND
MOTOYASU NAKAMURA, D.D.S., PH.D.
*Department of Dental Radiology, Health Sciences University of Hokkaido, Tobetsu, Japan; Department of Radiology, Hokkaido
University School of Medicine, Sapporo, Hokkaido, Japan; Department of Dental Radiology, Hokkaido University School of
Dentistry, Sapporo, Hokkaido, Japan
Purpose: To investigate the importance of total treatment time on the outcome of external beam radiotherapy
(EBRT) followed by internal brachytherapy for the treatment of oral tongue carcinoma.
Methods and Materials: Ninety-four patients with T1T2N0 squamous cell carcinoma of the oral tongue were
treated using 35 40 Gy EBRT followed by 35 40 Gy interstitial 137Cs brachytherapy between 1985 and 1995.
The interval between the end of EBRT and the start of interstitial treatment varied for numerous unavoidable
reasons, with a mean of 25.3 days and standard deviation of 3.5 days. The median follow-up period was 59.1
months (range 6 146).
Results: The actuarial survival rate of all cases was 78.4% at 5 years. The 5-year local control rate for those with
T1 and T2 was 92.8% and 62.7%, respectively (p < 0.05). The local control rate of the primary tumor in patients
with a total treatment time >43 days was statistically lower than that of patients with a total treatment time <43
days in all patients (p < 0.05) and in the subgroup of Stage T2 patients (p < 0.05). Multivariate analysis revealed
that the local control rates in all cases were significantly related to the T stage (T2 or not), total treatment time
(>43 days or not), and location of disease (posterior or not). Regression analysis for 5-year local control as a
function of treatment duration showed a 2% loss of local control per day of treatment extension >30 days (r
0.94, p < 0.01).
Conclusion: The total treatment time was associated with the local control rate in the RT of oral tongue
carcinoma. The loss in local control was estimated to be 2.0% per additional day in our series for oral tongue
carcinoma. 2003 Elsevier Inc.
Oral tongue carcinoma, Radiotherapy, Total treatment time.
INTRODUCTION
Accordingly, the aim of this study was to determine the
effect of total treatment time on local control of head-andneck cancer in combination treatment with EBRT and
brachytherapy.
The total treatment time is now recognized as an important
prognostic factor influencing local control of head-and-neck
carcinomas treated by external beam radiotherapy (EBRT)
(1 6). Increases in radiation time are reported to result in a
decrease in local control ranging from 1.5% to 1.7% per
additional day of treatment (6). In the case of combined
EBRT and brachytherapy, however, the influence of the
time factor on local control is less clear. That EBRT followed by brachytherapy is effective has been well established, but a period of several weeks without RT is often
required between the two treatments owing to cutaneous
and/or mucosal reactions after EBRT. Few studies have
evaluated the time factor in this treatment combination for
head-and-neck carcinomas (35).
METHODS AND MATERIALS
This retrospective study was carried out on all patients
with T1T2N0 oral tongue carcinoma who received EBRT
followed by brachytherapy to the primary tumor at Hokkaido University Medical Hospital between 1985 and 1995.
All patients had histopathologically proven squamous cell
carcinoma. They were previously untreated and did not have
distant metastasis as evaluated by clinical examination, laboratory tests, and chest radiography. Patients with 6
months of follow-up were excluded.
Reprint requests to: Yoichiro Hosokawa, D.D.S., Ph.D., Department of Dental Radiology, Health Sciences University of Hokkaido, Kanazawa 1757, Tobetsu, Hokkaido, Japan. Tel: 01332-3-
1211; Fax: 01332-3-1410; E-mail: hosokawa@hoku-iryo-u.ac.jp
Received Sep 6, 2002, and in revised form Apr 3, 2003. Accepted for publication Apr 7, 2003.
71
72
I. J. Radiation Oncology
Biology Physics
Between 1985 and 1995, 111 patients with T1T2 squamous cell carcinoma of the oral tongue according to the
1992 International Union Against Cancer TNM classification were treated radically with RT alone. Seven patients
were treated with brachytherapy alone and excluded from
this study. Four patients with regional lymph node metastasis were excluded and 6 patients were excluded because
they had a follow-up time of 6 months. The remaining 94
patients were entered as subjects of this study. Twenty-nine
tumors were Stage T1, and 65 were T2. Of the 94 patients,
58 were men and 36 women (average age 57.8 years, range
27 87). The medical records were reviewed in January
2003. The median follow-up period was 59.1 months (range
6 146).
After dental management, a fixation mask was made with
the patient in the supine position for EBRT. Before brachytherapy, EBRT in a daily dose of 2.5 Gy was applied to the
primary site four times weekly for 4 weeks, for a total dose
of 35 40 Gy. EBRT was performed using a Telecobalt unit.
Beam direction techniques were used with two fields and
wedge filtration. The homolateral node area of the supraclavicular and/or submandibular area was also irradiated,
giving 45 Gy in 18 fractions. The portal direction for the
neck area was AP for the middle and lower part. The
radiation field for the primary tumor and upper neck was
reduced in size at 35 40 Gy, so as to deliver 45 Gy in 18
fractions only to the upper neck lymphatic area. After EBRT
for the neck nodes, 137Cs needles were used for interstitial
brachytherapy to the primary site after administration of
local anesthesia. An intraoral protective spacer made individually for each patient was used instead of wet gauze
since 1988. The radioactive sources were implanted according to the Paterson-Parker method, using the tables of Paterson-Parker to calculate the irradiated dose. The prescribed
dose at the plane 5 mm from the plane of the radioactive
sources was adjusted to 35 40 Gy, with a dose rate of
10 12 Gy within 24 h in principle. In combination with the
external dose, the plane 5 mm from the plane of the radioactive sources received 75 Gy in total. Brachytherapy was
performed after the end of nodal EBRT of 45 Gy; thus, there
was an interval in which no radiation was given to the
primary site. No chemotherapy was given to 75 patients.
Nineteen patients, who were treated between 1990 and
1994, received carboplatin chemotherapy concomitant with
EBRT.
The actuarial survival, local control rate, and regional
lymph node control rate were measured using the KaplanMeier method. The duration of follow-up was calculated
from the date of the first treatment performed. Local recurrence was defined as pathologically confirmed relapse of
primary tumor with or without nodal or distant metastasis.
Regional recurrence was defined as neck node relapse or
residual disease with or without primary recurrence or distant failure. Statistical significance was analyzed by the
logrank test. The chi-square test was used to evaluate
differences among the patient subgroups. The primary site
of the tumor was classified as the anterior, middle, or
Volume 57, Number 1, 2003
posterior part of the tongue for the purpose of analysis.
Multivariate analysis was used to identify the prognostic
factors by logistic regression.
RESULTS
The average EBRT dose was 35.4 Gy (40 Gy in 12, 35
Gy in 81, and 20 Gy in 1). The average brachytherapy dose
was 39.7 Gy (60 Gy in 1, 55 Gy in 1, 50 Gy in 4, 45 Gy in
5, 40 Gy in 66, and 35 Gy in 21). The average dose rate at
5 mm from the radioactive source was 0.47 Gy/h (range
0.31 0.67).
The total treatment time varied from 29 to 69 days. The
average total treatment time for primary tumors was 43.3
5.9 days. The average duration from the start to the end of
EBRT in primary tumors was 25.3 3.5 days. The average
interval between EBRT and brachytherapy (measured from
the first day after EBRT to the beginning of brachytherapy)
in primary tumors was 14.6 5.5 days (Table 1). The
average duration of brachytherapy was 3.9 0.9 days.
To deliver EBRT to the primary tumors, 13 patients were
treated in 29 days, more than one standard deviation
greater than the mean duration of 25.1 days, and 81 patients
were treated within 29 days. The interval between the end
of EBRT and the start of brachytherapy varied because of
interruptions linked to public holidays or delays in the
availability of a room for brachytherapy (3 patients), poor
health status (1 patient), refusal of patients to undergo
implantation (1 patient), and severe reaction to EBRT (3
patients). Eight patients required 21 days, more than one
standard deviation greater than the mean of 14.6 days,
between EBRT and brachytherapy for primary tumors.
The actuarial survival rate for all patients was 78.4% at 5
years. The rate of local control for all patients was 72.4% at
5 years. Twenty-two patients experienced recurrence of the
primary tumor and 21 of them experienced recurrence
within 5 years. The patients without local failure had a
better survival rate at 5 years than did those with local
failure (p 0.05; Table 1). The regional control rate was
statistically worse in patients with local failure than in those
with local control (p 0.05; Fig. 1). At the time of analysis,
24 patients had died. No apparent difference in the cause of
death was demonstrated between patients with and without
local failure (Table 2).
The 5-year local control rate for those with T1 and T2
was 92.8% and 62.7%, respectively (p 0.05; Fig. 2).
Lesions located in the posterior portion of the tongue had a
significantly lower local control rate than those located in
the anterior or middle portion of the tongue (p 0.05; Fig.
3). Patient age, gender, treatment year, and use of chemotherapy did not have a significant effect on local control by
univariate analysis. The local control rate in the group with
a 14-day interval between EBRT and brachytherapy was
lower than that in the group with an interval of 14 days,
but the difference did not reach statistical significance (p
0.066; Fig. 4). The local control rate of the primary tumor in
patients with a total treatment time 43 days was statisti-
Effect of treatment time of RT for tongue carcinoma
Y. HOSOKAWA et al.
73
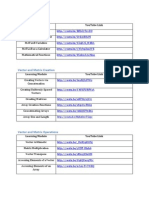
Table 1. Results of radiation dose and treatment time
Average EBRT dose (Gy)
Average brachytherapy dose (Gy)
Average dose rate at 5 mm from implant (Gy/h)
Total treatment time (d)
Average total treatment time (d)
Average duration from start to end of EBRT (d)
Average interval between EBRT and brachytherapy (d)
Average duration of brachytherapy (h)
Distribution of patients above and below mean duration (n)
Above (43 d)
Below (43 d)
Reasons for long interval* between EBRT and brachytherapy (n)
Public holidays
Availability of room for brachytherapy
Poor health status
Refusal of patient to undergo implantation
Severe reaction of external irradiation
5-year actuarial survival rate (%)
All (n 94)
Local recurrence (n 22)
No local recurrence (n 72)
35.4 (SD 2.61)
39.7 (SD 4.41)
0.43 (SD 0.08)
2969
43.3 (SD 5.92)
25.3 (SD 3.54)
14.6 (SD 5.49)
92.2 (SD 19.5)
41
53
2
1
1
1
3
78.4
66.2
81.5
* More than 1 SD greater than the mean (21 d).
Abbreviations: EBRT external beam radiotherapy; SD standard deviation.
cally lower than that of patients with a total treatment time
of 43 days (p 0.05; Fig. 5).
The T stage and the location of the primary tumor in each
group are shown in Table 3. Patients who had a total
treatment time 43 days had more T2 tumors than patients
who had a total treatment time of 43 days (p 0.05). The
results of the present examination of the actuarial local
control rate in 64 patients with T2 tumors indicated that this
rate was statistically lower in patients whose total treatment
time was 43 days (p 0.05; Fig. 6). No statistically
significant differences were found in the rate of lesions
located in the posterior portion of the tongue and in the
average total dose between these two groups.
Twenty-two patients had an adverse reaction to RT: 11
cases of transient tongue ulcer that healed within several
months, 5 cases of persistent tongue ulcer that did not elicit
severe complaints, 4 cases of severe tongue ulcer that required surgery, and 2 cases of osteoradionecrosis of the
mandible. No statistically significant differences were noted
in the rate of late adverse effects among any subgroups with
regard to age, gender, T stage, N stage, dose, total treatment
period, or treatment year (Table 3).
A correlation was found between the total treatment time
and the interval from the end of EBRT to the start of
brachytherapy (0.69, p 0.01) in the correlation analysis
(Table 4). Thus, the interval from the end of EBRT to the
start of brachytherapy was not included as an explanatory
variable in the multivariate analysis. The correlation analysis showed that the correlation coefficient between total
treatment time and T stage was not so great (0.2875).
Multivariate analysis revealed that, in all cases, the local
control rate was significantly related to T stage (T2 or not),
total treatment time, and location of disease (posterior or
not; Table 5).
Fig. 1. Regional control rates of patients with local failure and
those with local control.
74
I. J. Radiation Oncology
Biology Physics
Volume 57, Number 1, 2003
Table 2. Cause of death according to local control status
Local recurrence (n)
Cause
No
Yes
Local failure
Regional LN metastasis
Distant metastasis
Other disease
Unknown
Total
0
4
2
6
1
13 (n 72)
2
3
1
2
3
11 (n 22)
Figure 7 shows a plot of the 5-year local control rate as a
function of treatment duration for all patients. Patients were
grouped into subgroups according to total treatment time,
and the Kaplan-Meier 5-year local control rate was calculated for each group. A linear regression line was then fitted
to these data points. This line demonstrated a 2% loss of
local control per day of treatment extension 30 days. A
strong correlation was found between the total treatment
time and local control rate (r 0.94, p 0.01).
DISCUSSION
The management of carcinoma of the tongue in its early
stages by brachytherapy with or without EBRT has been
Fig. 3. Local control rates according to tumor location.
Fig. 2. Local control rates of T1 and T2.
used in many cancer centers (10 19). It was previously
suggested that local control correlated well with overall
survival (5, 14, 15). Our results were consistent with these
results, suggesting the importance of local control. The
patients with carcinoma at the posterior third of the oral
tongue in our series had lower local control rates. Hintz et
al. (20) concluded that patients showing involvement of the
base of the tongue were technically more demanding than
those with tumors of the oral tongue. Our results may have
been due to the technical difficulty of implantation in the
posterior location compared with that for tumors at the
anterior or middle part of the tongue.
The 5-year local control rate after RT for early tongue
carcinoma has been reported to be about 90% for T1 and
6592% for T2 (16 19). Our treatment results also showed
a significant difference in the local control rate between
patients with T1 and those with T2 lesions. Our multivariate
analysis indicated that prolongation of the overall treatment
time is also an independent significant factor for local
control. The correlation analysis showed that the correlation
coefficient between the total treatment time and the T stage
was not so great (0.2875). However, when we divided the
patients into two groups at 43 days, the proportion of those
with T2 was greater in the group with a total treatment time
Effect of treatment time of RT for tongue carcinoma
Fig. 4. Local control rates according to interval between EBRT and
brachytherapy.
43 days. This discrepancy can be explained by the limitation of deterministic grouping at a certain point into two
groups.
The prolongation of the overall treatment time has been
suggested to be an important factor contributing to local
failure of glottic cancer treatment by EBRT alone (15).
Burke et al. (1) reported that 67 patients who were treated
for 6 weeks had a 5-year local control rate of 93%, and
patients who were treated for 6 weeks had a 5-year local
control rate of 71%. In a report by van der Voet et al. (2),
the local control rate ranged from 95% for a treatment
duration of 2229 days to 79% for a treatment duration of
40 days. Robertson et al. (3) reviewed 303 patients radically treated with RT for T1 or T2 glottic cancer according
to one of six treatment schedules. The analysis of these data
revealed a marked decrease in local control associated with
a prolongation of treatment time within a range of biologically effective doses of 56.9 62 Gy. With respect to oropharyngeal carcinomas, Bataini et al. (21) evaluated 465
patients treated between 1978 and 1985 by EBRT alone and
showed a loss in tumor control of 17% weekly. This corresponds to a loss in treatment prolongation of 2.4% per day.
Several studies have evaluated the effects of treatment
duration and timing in combination treatment with EBRT
Y. HOSOKAWA et al.
75
Fig. 5. Local control rate according to total treatment time for all
patients.
and brachytherapy (7, 8, 22, 23). For cervical carcinoma and
breast tumors, the influence of treatment duration has been
shown to correlate with local control (22, 23). Dubray et al.
(22) showed an increasing probability of local failure with a
longer interval between EBRT and brachytherapy in breast
cancer. Fyles et al. (23) found that the treatment duration
had a significant effect on pelvic control in 830 patients with
cervical cancer treated by radical RT. In their review, patients treated for 30 days consistently showed a loss of
control of approximately 1% per day. With respect to headTable 3. T stage and primary tumor location according to total
treatment time
T1
T2
Anterior, middle
Posterior
Radiation injury
No
Yes
43 d
(n 41)
43 d
(n 53)
7
34
30
11
22
31
43
10
34
7
39
15
76
I. J. Radiation Oncology
Biology Physics
Volume 57, Number 1, 2003
Table 5. Results of multivariate analysis on possible prognostic
factors (Cox regression model)
Fig. 6. Local control rate according to total treatment time for
patients with T2 tumor.
and-neck carcinomas, it has been reported that the total
duration of RT and the delay between EBRT and brachytherapy were significant prognostic factors for local control
and overall survival of soft palate and tonsil carcinomas (7).
In our results for oral tongue carcinoma, the local control
rate for those with a total treatment time 43 days was
statistically lower than that for those with a total treatment
time of 43 days. This finding is consistent with the results
of Mendenhall et al. (8), who reported that local control was
achieved in 16 (76%) of 21 cases with a total treatment time
Factor
Relative
risk
T stage (T2 or not)
Disease location (posterior or not)
Total treatment time
Total dose
Treatment year
Age
Gender (male or not)
5.723
4.617
4.214
2.125
1.284
0.298
0.006
0.011
0.039
0.048
0.141
0.272
0.573
0.946
of 40 days and in 5 (36%) of 14 cases with a total
treatment time of 40 days. Our results for T2 tumors
suggest that the total treatment time of combined EBRT and
brachytherapy might be a biologically important factor for
local control in tongue carcinomas independent of tumor
size and tumor location. The loss in local control was
estimated to be 2.0% per additional day in our series for oral
tongue carcinoma. This rate is roughly in accordance with
the estimation of 1.51.7% by Hendry et al. (6) and that of
2.4% derived from the results of Bataini et al. (21) for
oropharyngeal carcinomas. Although these results were not
based on prospective randomized trials, the strong correlation between the total treatment time and local control rate
(r 0.94, p 0.01) suggests that total treatment time is one
of the most important prognostic factors. Accelerated repopulation of tumor cells may take place in patients with
oral tongue carcinoma as it does in those with head-andneck carcinoma (24).
We were unable to avoid a delay in the interval between
EBRT and brachytherapy. The strong correlation between
the overall treatment time and the interval between EBRT
and brachytherapy made it impossible to determine which
was the more important prognostic factor. The longer treatment time might have been the reason for the lower local
control rate of combined treatment compared with that of
brachytherapy alone in a past series (25). It would not be
profitable to add an EBRT dose to compensate for the delay
in the start of brachytherapy, because this would increase
late adverse reactions (19, 25). On the basis of these results
and those of previous studies, we are now treating T1-T2
Table 4. Partial correlation coefficients
T stage
Location
TTT
Total dose
Year
Age
Gender
Interval
T stage
Location
TTT
Total dose
Year
Age
Gender
Interval
1.0000
0.2488
0.2875
0.1356
0.0461
0.0021
0.1221
0.1918
0.2488
1.0000
0.0629
0.0622
0.1385
0.0816
0.2158
0.0622
0.2875
0.0629
1.0000
0.1395
0.2337
0.0924
0.0904
0.6944
0.1356
0.0622
0.1395
1.0000
0.1655
0.0357
0.0816
0.0003
0.0461
0.1385
0.2337
0.1655
1.0000
0.0404
0.2754
0.1538
0.0021
0.0816
0.0924
0.0357
0.0404
1.0000
0.0447
0.1929
0.1221
0.2158
0.0904
0.0816
0.2754
0.0447
1.0000
0.0340
0.1918
0.0622
0.6944
0.0003
0.1538
0.1929
0.0340
1.0000
Abbreviation: TTT total treatment time.
Effect of treatment time of RT for tongue carcinoma
Y. HOSOKAWA et al.
77
oral tongue carcinoma with brachytherapy alone, at 60 70
Gy in 1 week, to reduce the total treatment time for primary
tongue tumors. We are using low-dose-rate continuous RT
for T1 and small T2 tumors with single plane 137Cs implantation and starting high-dose-rate twice-daily RT with 129Ir
for larger T2 tumors to optimize the dose distribution in
space.
CONCLUSION
Fig. 7. Plot of 5-year local control rate as function of treatment
time for all patients. Data points grouped into 5-day intervals.
The local control rate of T1T2 oral tongue carcinoma
was better in cases of T1 than in T2 carcinoma; better in
cases of carcinoma located in the anterior or middle of
the tongue than in those located posteriorly; and better in
cases with shorter than in those with longer treatment
times. A treatment time of 43 days was associated with
a poor local control rate in patients with T2 primary
tumors. The results indicate that both the total treatment
time and the interval between EBRT and brachytherapy
are biologically important prognostic factors for local
control.
REFERENCES
1. Burke LS, Greven KM, McGuirt WT, et al. Definitive radiotherapy for early glottic carcinoma: Prognostic factors and
implications for treatment. Int J Radiat Oncol Biol Phys
1997;38:3742.
2. van der Voet JC, Keus RB, Hart AA, et al. The impact of
treatment time and smoking on local control and complications in T1 glottic cancer. Int J Radiat Oncol Biol Phys
1998;42:247255.
3. Robertson AG, Robertson C, Boyle P, et al. The effect of
differing radiotherapeutic schedules on the response of glottic
carcinoma of the larynx. Eur J Cancer 1993;29:501510.
4. Akine Y, Tokita N, Ogino T, et al. Radiotherapy of T1 glottic
cancer with 6 MeV X rays. Int J Radiat Oncol Biol Phys
1991;20:12151218.
5. Aref A, Dworkin J, Devi S, et al. Objective evaluation of the
quality of voice following radiation therapy for T1 glottic
cancer. Radiother Oncol 1997;45:149153.
6. Hendry JH, Bentzen SM, Dale RG, et al. A modelled comparison of the effects of using different ways to compensate
for missed treatment days in radiotherapy. Clin Oncol (R Coll
Radiol) 1996;8:297307.
7. Hoffstetter S, Marchal C, Peiffert D, et al. Treatment duration
as a prognostic factor for local control and survival in epidermoid carcinomas of the tonsillar region treated by combined
external beam irradiation and brachytherapy. Radiother Oncol
1997;45:141148.
8. Mendenhall WM, Parsons JT, Stringer SP, et al. T2 oral
tongue carcinoma treated with radiotherapy: Analysis of local
control and complications. Radiother Oncol 1989;16:275
281.
9. Bhattathiri VN. Cumulative interfraction interval analysis of
influence of time and interruptions on radiotherapy results in
oral cancers. Int J Radiat Oncol Biol Phys 2002;52:1251
1256.
10. Horiuchi J, Okuyama T, Shibuya H, et al. Results of brachytherapy for cancer of the tongue with special emphasis on
local prognosis. Int J Radiat Oncol Biol Phys 1982;8:829
835.
11. Pernot M, Hoffstetter S, Peiffert D, et al. Role of interstitial
brachytherapy in oral and oropharyngeal carcinoma: Reflection of a series of 1344 patients treated at the time of initial
presentation. Otolaryngol Head Neck Surg 1996;115:519
526.
12. Horwitz EM, Frazier AJ, Martinez AA, et al. Excellent functional outcome in patients with squamous cell carcinoma of
the base of tongue treated with external irradiation and interstitial iodine 125 boost. Cancer 1996;78:948957.
13. Mohanti BK, Swami K, Ganesh T, et al. Iridium-192 interstitial brachytherapy in carcinoma of the tongue. Acta Oncol
1997;36:165169.
14. Kirita T, Okabe S, Izumo T, et al. Risk factors for the
postoperative local recurrence of tongue carcinoma. J Oral
Maxillofacial Surg 1994;52:149154.
15. Yuen AP, Wei WI, Lam LK, et al. Results of surgical salvage
of locoregional recurrence of carcinoma of the tongue after
radiotherapy failure. Ann Otol Rhinol Laryngol 1997;106:
779782.
16. Mazeron JJ, Crook JM, Benck V, et al. Iridium 192 implantation of T1 and T2 carcinomas of the mobile tongue. Int J
Radiat Oncol Biol Phys 1990;19:13691376.
17. Pernot M, Malissard L, Hoffstetter S, et al. The study of
tumoral, radiobiological, and general health factors that influence results and complications in a series of 448 oral tongue
carcinomas treated exclusively by irradiation. Int J Radiat
Oncol Biol Phys 1994;29:673679.
18. Shibuya H, Hoshina M, Takeda M, et al. Brachytherapy for
stage I & II oral tongue cancer: An analysis of past cases
focusing on control and complications. Int J Radiat Oncol Biol
Phys 1993;26:5158.
19. Fujita M, Hirokawa Y, Kashiwado K, et al. Interstitial
brachytherapy for stage I and II squamous cell carcinoma of
the oral tongue: Factors influencing local control and soft
tissue complications. Int J Radiat Oncol Biol Phys 1999;
44:767775.
20. Hintz BL, Kagan R, Wollin M, et al. Treatment selection
78
I. J. Radiation Oncology
Biology Physics
for base of tongue carcinoma. J Surg Oncol 1989;41:165
171.
21. Bataini JP, Asselain B, Jaulerry C, et al. A multivariate
primary tumour control analysis in 465 patients treated by
radical radiotherapy for cancer of the tonsillar region: Clinical
and treatment parameters as prognostic factors. Radiother
Oncol 1989;14:265277.
22. Dubray B, Mazeron JJ, Simon JM, et al. Time factors in breast
carcinoma: Influence of delay between external irradiation and
brachytherapy. Radiother Oncol 1992;25:267272.
Volume 57, Number 1, 2003
23. Fyles A, Keane TJ, Barton M, et al. The effect of treatment
duration in the local control of cervix cancer. Radiother Oncol
1992;25:273279.
24. Kaanders JH, Bussink J, van der Kogel AJ. ARCON: A novel
biology-based approach in radiotherapy. Lancet Oncol 2002;
3:728737.
25. Pernot M, Malissard L, Aletti P, et al. Iridium-192 brachytherapy in the management of 147 T2N0 oral tongue carcinomas treated with irradiation alone: Comparison of two
treatment techniques. Radiother Oncol 1992;23:223228.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- National Radiotherapy Implementation Group Report IGRT Final PDFDocument93 pagesNational Radiotherapy Implementation Group Report IGRT Final PDFMaría José Sánchez LovellPas encore d'évaluation
- TG 218 Tolerance and Measurement Methods IMRTDocument9 pagesTG 218 Tolerance and Measurement Methods IMRTMaría José Sánchez LovellPas encore d'évaluation
- Review of Electron Beam Therapy PhysicsDocument36 pagesReview of Electron Beam Therapy PhysicsMaría José Sánchez LovellPas encore d'évaluation
- Links To Mathworks TutorialsDocument2 pagesLinks To Mathworks TutorialsMaría José Sánchez LovellPas encore d'évaluation
- Particle-Stabilized Emulsions Comprised of Solid DropletsDocument8 pagesParticle-Stabilized Emulsions Comprised of Solid DropletsMaría José Sánchez LovellPas encore d'évaluation
- Imaging Bio MarkersDocument4 pagesImaging Bio MarkersMaría José Sánchez LovellPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Fourth Quarter Examination in Arts 7Document3 pagesFourth Quarter Examination in Arts 7Jennifer Dapilmoto MandalPas encore d'évaluation
- The Excretory System-Biology-Unit 7 The Excretory SystemDocument6 pagesThe Excretory System-Biology-Unit 7 The Excretory SystemCamille ComasPas encore d'évaluation
- FIQ - Proliferative Diabetic RetinopathyDocument35 pagesFIQ - Proliferative Diabetic RetinopathyHikban FiqhiPas encore d'évaluation
- Brain Cancer ThesisDocument7 pagesBrain Cancer ThesisKristen Flores100% (2)
- TULUA Lipoabdominoplasty Transversal Aponeurotic.12Document14 pagesTULUA Lipoabdominoplasty Transversal Aponeurotic.12Carolina Ormaza Giraldo100% (1)
- Spinocerebellar AtaxiaDocument3 pagesSpinocerebellar AtaxiaSeth LyhalimPas encore d'évaluation
- Pines City Colleges: College of NursingDocument2 pagesPines City Colleges: College of NursingmagisasamundoPas encore d'évaluation
- 9 - Clinical Management (STRATOG 2015 SBAs)Document12 pages9 - Clinical Management (STRATOG 2015 SBAs)w yPas encore d'évaluation
- Biomarkers-A General ReviewDocument17 pagesBiomarkers-A General ReviewKevin FossPas encore d'évaluation
- UELS NIH Research Plan CompressedDocument36 pagesUELS NIH Research Plan CompressedKunal JaisinghaniPas encore d'évaluation
- Use of Liquid ParaffinDocument7 pagesUse of Liquid ParaffinNada Milic - PavlicevicPas encore d'évaluation
- Common Anorectal Conditions - Evaluation and TreatmentDocument5 pagesCommon Anorectal Conditions - Evaluation and TreatmentNicolás CopaniPas encore d'évaluation
- Body As The Source of Threat and Fear of Death in Hypochondriasis and Panic DisorderDocument10 pagesBody As The Source of Threat and Fear of Death in Hypochondriasis and Panic DisorderAnđelka RakovićPas encore d'évaluation
- Assoc. Prof. Ma. Jennifer R. Tiburcio, MSMT Department of Med Tech UST Faculty of PharmacyDocument27 pagesAssoc. Prof. Ma. Jennifer R. Tiburcio, MSMT Department of Med Tech UST Faculty of PharmacyJaellah MatawaPas encore d'évaluation
- Jurnal NeuroDocument6 pagesJurnal NeuroSiti WahyuningsihPas encore d'évaluation
- Urethral InjuryDocument7 pagesUrethral InjuryIoannis ValioulisPas encore d'évaluation
- Case Ana-Hypothyroidism 2020Document7 pagesCase Ana-Hypothyroidism 2020Nicole cuencosPas encore d'évaluation
- Dengue Hemorrhagic ShitDocument28 pagesDengue Hemorrhagic ShitRebecca FabonPas encore d'évaluation
- Coordinators BibleDocument60 pagesCoordinators BibleSava SánchezPas encore d'évaluation
- Pediatric Care PlanDocument13 pagesPediatric Care PlanAlyssa Van VarkPas encore d'évaluation
- O&G Off-Tag Assesment Logbook: Traces-Pdf-248732173Document9 pagesO&G Off-Tag Assesment Logbook: Traces-Pdf-248732173niwasPas encore d'évaluation
- The Use of Warfarin in Prosthetic Heart Valves Patient Short VersionDocument27 pagesThe Use of Warfarin in Prosthetic Heart Valves Patient Short VersionStanley Santosa KamadjajaPas encore d'évaluation
- Sample Cpje 2019 BulletinDocument3 pagesSample Cpje 2019 BulletinLara Lai100% (3)
- Gynecological LaparosDocument32 pagesGynecological LaparosYosef Dwi Cahyadi Salan100% (1)
- NURS FPX 6614 Assessment 3 Disseminating The Evidence Scholarly Video Media SubmissionDocument7 pagesNURS FPX 6614 Assessment 3 Disseminating The Evidence Scholarly Video Media Submissionjoohnsmith070Pas encore d'évaluation
- Tpuc 501Document4 pagesTpuc 501hairiPas encore d'évaluation
- Standard Bill FormatDocument14 pagesStandard Bill FormatPrasanna Nammalwar100% (1)
- Lipoma of The Oral and Maxillofacial RegionDocument10 pagesLipoma of The Oral and Maxillofacial RegionLaila FortunatoPas encore d'évaluation
- Acute Liver Injury and FailureDocument14 pagesAcute Liver Injury and FailureWeslei ChaconPas encore d'évaluation
- Metals and Psychotherapy - Rudolf Treichler (AnthroMed)Document6 pagesMetals and Psychotherapy - Rudolf Treichler (AnthroMed)Alexandre Funcia100% (1)