Académique Documents
Professionnel Documents
Culture Documents
Testing Hearing in Children (Boa)
Transféré par
Dian Rahma RidwansyahCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Testing Hearing in Children (Boa)
Transféré par
Dian Rahma RidwansyahDroits d'auteur :
Formats disponibles
Jane R.
Madell, PhD
Pediatric Audiology Consultant, Auditory Verbal Therapist
www.JaneMadell.com
TESTING HEARING IN CHILDREN
There are a number of different techniques used to test hearing in children. When
children are very young (less than 6 months of age), testing needs to be done without
requiring cooperation from the child. Testing is accomplished by using Auditory
Brainstem Response (ABR) testing and Behavioral Observation Audiometry (BOA)
observing changes in sucking. For children 6-36 months of age testing is accomplished
using Visual Reinforcement Audiometry (VRA) using a conditioned head turning
response. Once a child is about three years old, testing is best accomplished if we can
get the child to cooperate. The task is called Conditioned Play Audiometry. We teach the
child to use a Listen and Drop task making a motor response (such as putting a ring
on a ring stand, or dropping a block in a bucket) when he or she hears a sound.
BEHAVIORAL OBSERVATION AUDIOMETRY (BOA)
ABR testing is a critical protocol for use with infants because it provides information
about the auditory system without requiring cooperation from the baby. ABR measures
brainstem response and estimates hearing levels but, it is not a direct measure of
hearing. In addition we cannot use it to monitor how children are hearing with hearing
aids. BOA is an important test protocol because it tells us what the baby is hearing and
allows us to measure how they are hearing with hearing aids so we can be sure they are
hearing what they need to hear.
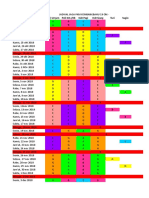
Table 1: ELECTROPHYSIOLOGICAL VS BEHAVIORAL TESTING
Electrophysiological testing
Does not require cooperation
Objective
Can easily be obtained in infants under
age 6 months
o Requires sedation over 6
months
o Newer equipment may not
require sedation
Not a measure of hearing
o A measure of brainstem activity
Cannot be used to monitor hearing
aids and cochlear implants
Behavioral testing
Requires some cooperation
A direct measure of hearing!!!
Can be easily obtained in infants!!!
Parents can easily observe and
understand test results
BOA test protocol
1. Baby resting comfortably in mothers arms or in infant seat
2. Begin nursing, feed baby bottle, or use pacifier.
3. Observe changes in sucking. A response can be either starting or stopping
sucking. Babies are consistent in how they respond. Some respond to the start of
the sound, and some to the stop.
4. Start at a loud level where you think the baby will hear. When you see a
response, make the sound softer. Keep making the sound softer until there are
no more responses. Then start making the sounds louder until you see the
response again
5. Responses should be observed 2-3 times before it is considered a response.
Jane R. Madell, PhD
Pediatric Audiology Consultant, Auditory Verbal Therapist
www.JaneMadell.com
6. Test low, mid and high frequencies.
The baby should be brought to the evaluation hungry so he will be ready to suck. Testing
will be most reliable if attention is paid to keeping the baby comfortable, not wiggling
around. If the baby becomes fussy, stop and comfort the baby before beginning testing
again. It is important that everyone in the test booth be careful not to respond to the
sounds so that it does not influence testing.
Testing can be performed with earphones, bone conduction, hearing aids, cochlear
implants, and FM systems to be sure the baby is hearing everything we want her to
hear.
VISUAL REINFORCEMENT AUDIOMETRY (VRA)
VRA uses a conditioned head turning response to measure response to sound. The
reinforcer can be as simple as a flashlight in a dark room or, even better, a movable toy.
The reinforcer should be off to the side so it is not directly in the babys line of site.
The child is seated comfortably on a parents lap, or in a highchair. A test assistant sits
in front of the child and keeps him focused in front holding toys or puppets to keep the
childs attention. Sounds are presented and paired with the toy or light. The child may
look up at the sound but she may not. After the sound has been on for a second or two,
the toy should be turned on. If the child does not look at the toy, the test assistant should
point to the toy to get the child to see it. After a few pairings of the sound and the toy, the
child should make the association and begin to look when she hears a sound. In this
way, thresholds can be obtained.
VRA test protocol
1. Seat the child comfortably on a lap, or in a highchair
2. Face the child forward, test assistant keeping the child focused forward
3. Pair the sound with the VRA toy to condition the child to respond
4. Start at a loud level where you think the baby will hear. When you get a
response, make the sound softer. Keep making the sound softer until there are
no more responses. Then start making the sounds louder until you see the
response again
5. Responses should be observed 2-3 times before it is considered a response.
6. Test low, mid and high frequencies.
7. Do not present sound too close together or the child will become bored with the
game and stop cooperating.
Testing can be performed with earphones, bone conduction, hearing aids, cochlear
implants, and FM systems to be sure the baby is hearing everything we want her to
hear.
VRA toy -
Jane R. Madell, PhD
Pediatric Audiology Consultant, Auditory Verbal Therapist
www.JaneMadell.com
CONDITIONED PLAY AUDIOMETRY (CPA)
CPA is a Listen and Drop game. We ask the child to listen for a sound, and then drop a
toy into a bucket, or put a ring on a ring stand when she hears the sound. CPA requires
cooperation from the child. If we use interesting toys we can easily keep a child
interested for long enough to get lots of testing accomplished. Blocks, puzzles, chips,
pebbles, all of which can be dropped into a bucket are good. Ring stands also work well.
It is important to have many toys available so when the child becomes tired of a toy you
can quickly change to another.
Some children will learn this task easily simply by being told what to do. We will say
Hold the toy near your ear and drop it in the bucket when you hear the sound. We may
then either make a noise or say Put it in. The first few times, the test assistant may
help the child by moving his or her hand from the ear towards the bucket. When the child
starts moving his hand towards the bucket by himself, the test assistant will drop her
hand.
When practicing, start by letting the child see your face if you are using a voice stimulus,
or see the toy that is making the noise if you are using a noise toy (bell, drum, pot and
spoon). The child will begin by using both visual and auditory cues. When he can do the
task by himself using both visual and auditory cues, drop the visual cue and try auditory
alone. The person making the noise should sit behind the child so he has no visual cues
and must rely on listening to know when to respond.
When the child seems to have the task, practice making the sounds softer, and try
different sounds. Be careful to change the rhythm of the presentation so you are not
presenting the sound every 50 to 60 seconds or the child may get into a time pattern and
not be responding to sound at all.
This should be a game for the child so find some interesting toys and make it a game.
Testing can be accomplished with earphones, bone conduction, hearing aids, cochlear
implants and FM systems.
Jane R. Madell, PhD
Pediatric Audiology Consultant and Auditory Verbal Therapist
www.JaneMadell.com
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Holistic Approach in Glaucoma and Dry Eye: ONLINE WEBINAR - SATURDAY JUNE 26 2021 - 14:00 - 16:00 PM (WIB)Document1 pageHolistic Approach in Glaucoma and Dry Eye: ONLINE WEBINAR - SATURDAY JUNE 26 2021 - 14:00 - 16:00 PM (WIB)Dian Rahma RidwansyahPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Secondary GlaucomaDocument19 pagesSecondary GlaucomaRakhmad TriharsadiPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Hari Tanggal Poli Umum Poli KIA /KB IGD Pagi IGD Siang Turi SugioDocument6 pagesHari Tanggal Poli Umum Poli KIA /KB IGD Pagi IGD Siang Turi SugioDian Rahma RidwansyahPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Bus Kartar Alisha TransDocument1 pageBus Kartar Alisha TransDian Rahma RidwansyahPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- JNC 8 Guideline Algorithm for Treating HypertensionDocument2 pagesJNC 8 Guideline Algorithm for Treating HypertensionTaradifaNurInsi0% (1)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- PTSDDocument38 pagesPTSDDian Rahma RidwansyahPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Poster EWS & CB Malang Agustus 2018Document2 pagesPoster EWS & CB Malang Agustus 2018Dian Rahma RidwansyahPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Parasitic Disease (Pheumoystis Jirovecii Pheomonia)Document15 pagesParasitic Disease (Pheumoystis Jirovecii Pheomonia)Brijesh Singh YadavPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- KOMPLIKASIDocument3 pagesKOMPLIKASIDian Rahma RidwansyahPas encore d'évaluation
- InesshhgDocument13 pagesInesshhgDian Rahma RidwansyahPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Phacomorphic Glaucoma: Case and Review: Joseph Sowka, O.DDocument4 pagesPhacomorphic Glaucoma: Case and Review: Joseph Sowka, O.DDian Rahma RidwansyahPas encore d'évaluation
- Bacterial VaginosisDocument3 pagesBacterial VaginosisDian Rahma RidwansyahPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- IPA Assignment Analyzes New Public AdministrationDocument8 pagesIPA Assignment Analyzes New Public AdministrationKumaran ViswanathanPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- (Math 6 WK 5 L9) - Problems Involving Addition and or Subtraction of DecimalsDocument43 pages(Math 6 WK 5 L9) - Problems Involving Addition and or Subtraction of DecimalsRhea OcitePas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- A Sample of Directory or Instruction:: World Temperatures February 16Document1 pageA Sample of Directory or Instruction:: World Temperatures February 16eksaPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Investigation of Twilight Using Sky Quality Meter For Isha' Prayer TimeDocument1 pageInvestigation of Twilight Using Sky Quality Meter For Isha' Prayer Timeresurgam52Pas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Sulzer MC EquipmentDocument12 pagesSulzer MC EquipmentsnthmlgtPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
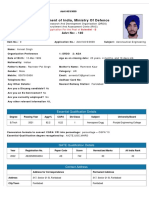
- DrdoDocument2 pagesDrdoAvneet SinghPas encore d'évaluation
- The Truth of Extinction: 7.1 Nietzsche's FableDocument2 pagesThe Truth of Extinction: 7.1 Nietzsche's FableGraciela Barón GuiñazúPas encore d'évaluation
- Designers' Guide To Eurocode 7 Geothechnical DesignDocument213 pagesDesigners' Guide To Eurocode 7 Geothechnical DesignJoão Gamboias100% (9)
- Manufacturing Processes (ME361) Lecture 13: Instructor: Shantanu BhattacharyaDocument28 pagesManufacturing Processes (ME361) Lecture 13: Instructor: Shantanu BhattacharyaSahil SundaPas encore d'évaluation
- CD1 ISO/IEC 17000 Conformity Assessment - Vocabulary and General PrinciplesDocument26 pagesCD1 ISO/IEC 17000 Conformity Assessment - Vocabulary and General PrinciplesMAC CONSULTORESPas encore d'évaluation
- Main Sulci & Fissures: Cerebral FissureDocument17 pagesMain Sulci & Fissures: Cerebral FissureNagbhushan BmPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- ECE Laws and Ethics NotesDocument29 pagesECE Laws and Ethics Notesmars100% (1)
- Reflecting on UPHSD's Mission, Vision, and Core ValuesDocument3 pagesReflecting on UPHSD's Mission, Vision, and Core ValuesBia N Cz100% (1)
- History of Computer AnimationDocument39 pagesHistory of Computer AnimationRanzelle UrsalPas encore d'évaluation
- 3.1-Pile Design Calculation For Boundary (p1 To p50)Document24 pages3.1-Pile Design Calculation For Boundary (p1 To p50)layaljamal2Pas encore d'évaluation
- Test Unit 7 m.2Document6 pagesTest Unit 7 m.2Petchara SridakunPas encore d'évaluation
- CROCI Focus Intellectual CapitalDocument35 pagesCROCI Focus Intellectual CapitalcarminatPas encore d'évaluation
- TM500 Design Overview (Complete ArchitectureDocument3 pagesTM500 Design Overview (Complete ArchitectureppghoshinPas encore d'évaluation
- Kuliah 1 - Konservasi GeologiDocument5 pagesKuliah 1 - Konservasi GeologiFerdianPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Inventory ManagementDocument60 pagesInventory Managementdrashti0% (1)
- Campbell Soup Case-StudyDocument3 pagesCampbell Soup Case-StudyraghudeepaPas encore d'évaluation
- Hackathon Statements V1Document10 pagesHackathon Statements V1AayushPas encore d'évaluation
- Proposed - TIA - 1392 - NFPA - 221Document2 pagesProposed - TIA - 1392 - NFPA - 221Junior TorrejónPas encore d'évaluation
- Penomoran Bantex - K64&COMPDocument8 pagesPenomoran Bantex - K64&COMPVigour Rizko MurdynePas encore d'évaluation
- CFLM1 Chapter 1Document24 pagesCFLM1 Chapter 1Jonathan TawagPas encore d'évaluation
- Exhaust Brake PDFDocument2 pagesExhaust Brake PDFFeliciaPas encore d'évaluation
- CA Module Franklin Gari RDocument28 pagesCA Module Franklin Gari RFranklin GariPas encore d'évaluation
- E Requisition SystemDocument8 pagesE Requisition SystemWaNi AbidPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Language Culture and ThoughtDocument24 pagesLanguage Culture and ThoughtLý Hiển NhiênPas encore d'évaluation
- Limits, Fits and Tolerances: Prof. S. S. PandeDocument31 pagesLimits, Fits and Tolerances: Prof. S. S. PandeM PankajPas encore d'évaluation